Abstract
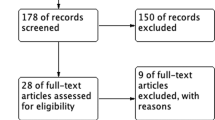
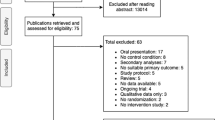
Sexual-wellbeing is recognized as an important aspect of quality-of-life. Yet, no overview exists of which aspects of sexual-wellbeing have been assessed in trans individuals seeking or undergoing medical treatment, nor is it clear what tools are used to evaluate the effect of medical treatment on sexual-wellbeing. First, to identify which topics pertaining to sexual-wellbeing have been assessed in transgender individuals in a medical context. Second, to determine which tools have been used for measuring aspects of sexual-wellbeing. A conceptual framework of sexual-wellbeing, was used as reference. A literature search (in PubMed, Embase, Cochrane Library) was performed up to March 10th, 2020. Studies that assessed aspects of sexual-wellbeing in transgender individuals’ medical context were included in this review. Specific sexual topics addressed in each study were extracted by two independent reviewers. Thematic analysis was performed to identify sexual themes. Additionally, tools used to measure topics related to sexuality in transgender individuals were identified. In 172 papers, a total of 178 topics related to sexual-wellbeing were identified. Ten overarching themes were identified; sexuality, enacted sexual script, sexual activities, sexual relations, sexual response cycle, genital function, sexual function, sexual pleasure, sexual satisfaction, and quality-of-sex-life. Functional aspects of sexuality are assessed most frequently. A variety of methods was used to evaluate aspects related to sexual-wellbeing in trans individuals and over 50 different tools were identified. Self-developed questionnaires were used most frequently (n = 80), followed by chart reviews (n = 50), self-developed structured interviews (n = 37) and physical examination (n = 13). 23 previously developed questionnaires were used, all of which were developed for a cisgender population. Many studies in trans individuals touch on topics related to sexual-wellbeing, however, a comprehensive conceptualisation of (10 themes of) sexual-wellbeing is still lacking. Still, no valid tool exists for assessing sexual-wellbeing in the trans population, but is much needed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
This can be found in supplement 1.
References
van de Grift TC, Elfering L, Greijdanus M, Smit JM, Bouman MB, Klassen AF, et al. Subcutaneous mastectomy improves satisfaction with body and psychosocial function in trans men: Findings of a cross-sectional study using the BODY-Q chest module. Plast Reconstr Surg. 2018;142:1125–32.
Woloski-Wruble AC, Oliel Y, Leefsma M, Hochner-Celnikier D. Sexual activities, sexual and life satisfaction, and successful aging in women. J Sex Med. 2010;7:2401–10.
Klein C, Gorzalka BB. Sexual functioning in transsexuals following hormone therapy and genital surgery: a review. J Sex Med. 2009;6:2922–39. quiz 40-1
Holmberg M, Arver S, Dhejne C. Supporting sexuality and improving sexual function in transgender persons. Nat Rev Urol. 2019;16:121–39.
Thurston MD, Allan S. Sexuality and sexual experiences during gender transition: a thematic synthesis. Clin Psychol Rev. 2018;66:39–50.
Stephenson R, Riley E, Rogers E, Suarez N, Metheny N, Senda J, et al. The sexual health of transgender men: a scoping review. J Sex Res. 2017;54:424–45.
Bettocchi C, Ralph DJ, Pryor JP. Pedicled pubic phalloplasty in females with gender dysphoria. BJU Int. 2005;95:120–4.
Kim SK, Park JW, Lim KR, Lee KC. Is rectosigmoid vaginoplasty still useful? Arch Plast Surg. 2017;44:48–52.
Krege S, Bex A, Lummen G, Rubben H. Male-to-female transsexualism: a technique, results and long-term follow-up in 66 patients. BJU Int. 2001;88:396–402.
Mukai Y, Watanabe T, Sugimoto M, Kimata Y, Namba Y. Vaginoplasty with a pudendal-groin flap in male-to-female transsexuals. Acta Med Okayama. 2017;71:399–405.
Stanojevic DS, Djordjevic ML, Milosevic A, Sansalone S, Slavkovic Z, Ducic S, et al. Sacrospinous ligament fixation for neovaginal prolapse prevention in male-to-female surgery. Urology 2007;70:767–71.
Takamatsu A, Harashina T. Labial ring flap: a new flap for metaidoioplasty in female-to-male transsexuals. J Plast, Reconstructive Aesthetic Surg. 2009;62:318–25.
Vesely J, Hyza P, Ranno R, Cigna E, Monni N, Stupka I, et al. New technique of total phalloplasty with reinnervated latissimus dorsi myocutaneous free flap in female-to-male transsexuals. Ann Plast Surg. 2007;58:544–50.
Papadopulos NA, Schaff J, Biemer E. Usefulness of free sensate osteofasciocutaneous forearm and fibula flaps for neophallus construction. J Reconstr Microsurg. 2001;17:407–12.
Papadopulos NA, Zavlin D, Lelle JD, Herschbach P, Henrich G, Kovacs L, et al. Combined vaginoplasty technique for male-to-female sex reassignment surgery: operative approach and outcomes. J Plast, Reconstr Aesthetic Surg. 2017;70:1483–92.
van de Grift TC, Pigot GLS, Kreukels BPC, Bouman MB, Mullender MG. Transmen’s experienced sexuality and genital gender-affirming surgery: findings from a clinical follow-up study. J Sex Marital Ther. 2019;45:201–5.
Kerckhof ME, Kreukels BPC, Nieder TO, Becker-Hebly I, van de Grift TC, Staphorsius AS, et al. Prevalence of sexual dysfunctions in transgender persons: results from the ENIGI follow-up study. J Sex Med. 2019;16:2018–29.
Nikkelen SWC, Kreukels BPC. Sexual experiences in transgender people: the role of desire for gender-confirming interventions, psychological well-being, and body satisfaction. J Sex Marital Ther. 2018;44:370–81.
Nobili A, Glazebrook C, Arcelus J. Quality of life of treatment-seeking transgender adults: a systematic review and meta-analysis. Rev Endocr Metab Disord. 2018;19:199–220.
Byers SR, U. Sexual well-being. APA handbook of sexuality and psychology. Washington, D.C.: American Psychological Association; 2014.
Moher D, Liberati A, Tetzlaff J, Altman DG. The PG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Innovation VH. Covidence systematic review software.
OCEBM Levels of Evidence Working Group: Jeremy Howick ICJLL, Paul Glasziou, Trish Greenhalgh, Carl Heneghan, Alessandro Liberati, Ivan Moschetti, et al.. The Oxford 2011 Levels of Evidence. 2011.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
Djordjevic ML. Novel surgical techniques in female to male gender-confirming surgery. Transl Androl Urol. 2018;7:628–38.
Djordjevic ML, Bizic MR. Comparison of two different methods for urethral lengthening in female to male (metoidioplasty) surgery. J Sex Med. 2013;10:1431–8.
Djordjevic ML, Stanojevic D, Bizic M, Kojovic V, Majstorovic M, Vujovic S, et al. Metoidioplasty as a single stage sex reassignment surgery in female transsexuals: Belgrade experience. J Sex Med. 2009;6:1306–13.
Smith YL, van Goozen SH, Cohen-Kettenis PT. Adolescents with gender identity disorder who were accepted or rejected for sex reassignment surgery: a prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 2001;40:472–81.
Smith YL, van Goozen SH, Kuiper AJ, Cohen-Kettenis PT. Transsexual subtypes: clinical and theoretical significance. Psychiatry Res. 2005;137:151–60.
Stojanovic B, Bizic M, Bencic M, Kojovic V, Majstorovic M, Jeftovic M, et al. One-stage gender-confirmation surgery as a viable surgical procedure for female-to-male transsexuals. J Sex Med. 2017;14:741–6.
van de Grift TC, Pigot GLS, Boudhan S, Elfering L, Kreukels BPC, Gijs L, et al. A longitudinal study of motivations before and psychosexual outcomes after genital gender-confirming surgery in transmen. J Sex Med. 2017;14:1621–8.
Al-Tamimi M, Pigot GL, van der Sluis WB, van de Grift TC, Mullender MG, Groenman F, et al. Colpectomy significantly reduces the risk of urethral fistula formation after urethral lengthening in transgender men undergoing genital gender affirming surgery. J Urol. 2018;200:1315–22.
Ranno R, Hyza P, Vesely J, Dessy LA, Kadanka Z. An objective evaluation of contraction power of neo-phallus reconstructed with free re-innervated LD in female-to-male transsexuals. Acta Chirurgiae Plasticae. 2007;49:8–12.
Ranno R, Vesely J, Hyza P, Stupka I, Justan I, Dvorak Z, et al. Neo-phalloplasty with re-innervated latissimus dorsi free flap: a functional study of a novel technique. Acta Chirurgiae Plasticae. 2007;49:3–7.
Vukadinovic V, Stojanovic B, Majstorovic M, Milosevic A. The role of clitoral anatomy in female to male sex reassignment surgery. Sci World J. 2014;2014:437378.
Bouman MB, van der Sluis WB, van Woudenberg Hamstra LE, Buncamper ME, Kreukels BPC, Meijerink W, et al. Patient-reported esthetic and functional outcomes of primary total laparoscopic intestinal vaginoplasty in transgender women with penoscrotal hypoplasia. J Sex Med. 2016;13:1438–44.
Buncamper ME, Honselaar JS, Bouman MB, Ozer M, Kreukels BP, Mullender MG. Aesthetic and functional outcomes of neovaginoplasty using penile skin in male-to-female transsexuals. J Sex Med. 2015;12:1626–34.
Buncamper ME, van der Sluis WB, de Vries M, Witte BI, Bouman MB, Mullender MG. Penile inversion vaginoplasty with or without additional full-thickness skin graft: to graft or not to graft? Plast Reconstr Surg. 2017;139:649e–56e.
Lawrence AA. Factors associated with satisfaction or regret following male-to-female sex reassignment surgery. Arch Sex Behav. 2003;32:299–315.
Lawrence AA. Sexuality before and after male-to-female sex reassignment surgery. Arch Sex Behav. 2005;34:147–66.
Lawrence AA. Patient-reported complications and functional outcomes of male-to-female sex reassignment surgery. Arch Sex Behav. 2006;35:717–27.
Lindemalm G, Korlin D, Uddenberg N. Long-term follow-up of “sex change” in 13 male-to-female transsexuals. Arch Sex Behav. 1986;15:187–210.
Lindemalm G, Korlin D, Uddenberg N. Prognostic factors vs. outcome in male-to-female transsexualism. A follow-up study of 13 cases. Acta Psychiatr Scand. 1987;75:268–74.
Elaut E, Bogaert V, De Cuypere G, Weyers S, Gijs L, Kaufman JM, et al. Contribution of androgen receptor sensitivity to the relation between testosterone and sexual desire: an exploration in male-to-female transsexuals. J Endocr Investig. 2010;33:37–41.
Elaut E, De Cuypere G, De Sutter P, Gijs L, Van Trotsenburg M, Heylens G, et al. Hypoactive sexual desire in transsexual women: prevalence and association with testosterone levels. Eur J Endocrinol. 2008;158:393–9.
Papadopulos NA, Lelle JD, Zavlin D, Herschbach P, Henrich G, Kovacs L, et al. Psychological pathologies and sexual orientation in transgender women undergoing gender confirming treatment. Ann Plast Surg. 2020;84:312–6.
Rehman J, Lazer S, Benet AE, Schaefer LC, Melman A. The reported sex and surgery satisfactions of 28 postoperative male-to-female transsexual patients. Arch Sex Behav. 1999;28:71–89.
Rehman J, Melman A. Formation of neoclitoris from glans penis by reduction glansplasty with preservation of neurovascular bundle in male-to-female gender surgery: functional and cosmetic outcome. J Urol. 1999;161:200–6.
van der Sluis WB, Bouman MB, de Boer NK, Buncamper ME, van Bodegraven AA, Neefjes-Borst EA, et al. Long-term follow-up of transgender women after secondary intestinal vaginoplasty. J Sex Med. 2016;13:702–10.
van der Sluis WB, Neefjes-Borst EA, Bouman MB, Meijerink WJ, De Boer NK, Mullender MG, et al. Morphological spectrum of neovaginitis in autologous sigmoid transplant patients. Histopathology. 2016;68:1004–12.
Zavlin D, Schaff J, Lelle JD, Jubbal KT, Herschbach P, Henrich G, et al. Male-to-female sex reassignment surgery using the combined vaginoplasty technique: Satisfaction of transgender patients with aesthetic, functional, and sexual outcomes. Aesthetic Plast Surg. 2018;42:178–87.
Zavlin D, Wassersug RJ, Chegireddy V, Schaff J, Papadopulos NA. Age-related differences for male-to-female transgender patients undergoing gender-affirming surgery. Sex Med. 2019;7:86–93.
Smith YL, Van Goozen SH, Kuiper AJ, Cohen-Kettenis PT. Sex reassignment: outcomes and predictors of treatment for adolescent and adult transsexuals. Psychol Med. 2005;35:89–99.
Dunford C, Bell K, Rashid T. Genital reconstructive surgery in male to female transgender patients: a systematic review of primary surgical techniques, complication profiles, and functional outcomes from 1950 to present day. Eur Urol Focus. 2020;7:464–71.
Harden KP. A sex-positive framework for research on adolescent sexuality. Perspect Psychol Sci. 2014;9:455–69.
ETM Laan VK, MA Werner, HW van Lunsen, E Janssen. In pursuit of pleasure: a biopsychosocial perspective on sexual pleasure and gender. Int J Sex Health. 2021:1–21.
LeBreton M, Courtois F, Journel NM, Beaulieu-Prevost D, Belanger M, Ruffion A, et al. Genital sensory detection thresholds and patient satisfaction with vaginoplasty in male-to-female transgender women. J Sex Med. 2017;14:274–81.
Ristori J, Cocchetti C, Castellini G, Pierdominici M, Cipriani A, Testi D, et al. Hormonal treatment effect on sexual distress in transgender persons: 2-year follow-up data. J Sex Med. 2020;17:142–51.
Staples JM, Bird ER, Gregg JJ, George W. Improving the gender-affirmation process for transgender and gender-nonconforming individuals: associations among time since transition began, body satisfaction, and sexual distress. J Sex Res. 2020;57:375–83.
Lawrance K-A, Byers ES. Sexual satisfaction in long-term heterosexual relationships: the interpersonal exchange model of sexual satisfaction. Personal Relatsh. 1995;2:267–85.
Martin KM, Woodgate RL. Concept analysis: the holistic nature of sexual well-being. Sex Relatsh Ther. 2020;35:15–29.
Acknowledgements
The literature search was done in collaboration with, Ralph de Vries, a medical information specialist at Amsterdam University Medical Center.
Author information
Authors and Affiliations
Contributions
Müjde Özer: methodology, conceptualisation, investigation, writing—original draft Sahaand Poor Toulabi: methodology, conceptualisation, investigation, writing, visualisation Luk Gijs: writing—review, editing and supervision Baudewijntje Kreukels: writing—review, editing and supervision Margriet Mullender: review, editing, and supervision.
Corresponding author
Ethics declarations
Competing interests
All authors have seen and agree on the submitted version. We declare that the material is original and has not been published elsewhere.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Özer, M., Poor Toulabi, S., Gijs, L. et al. The assessment of sexual wellbeing in treatment-seeking transgender individuals: a systematic review of the medical literature. Int J Impot Res 35, 121–131 (2023). https://doi.org/10.1038/s41443-022-00529-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-022-00529-9
This article is cited by
-
Measuring Sexual Function in Gender Minority Individuals: A Critical Review
Current Sexual Health Reports (2024)