Abstract
The control rate of ambulatory blood pressure (BP) is unclear in Chinese hypertensive patients, and whether it would be associated with the ambulatory arterial stiffness indices is also unknown. From June 2018 until December 2022, 4408 treated hypertensive patients (52.8% men, average age 58.2 years) from 77 hospitals in China were registered. Ambulatory BPs were measured with validated monitors and analyzed with a web-based standardized Shuoyun system (www.shuoyun.com.cn). The BP control rate was the highest in the office (65.7%), moderate in the daytime (45.0%), low in the morning (34.1%), and the lowest in the nighttime (27.6%, P < 0.001). Only 21.0% had their 24 h BP perfectly controlled. The stepwise regression analyses identified that the factors associated with an imperfect 24 h BP control included male sex, smoking and drinking habits, a higher body mass index, serum total cholesterol and triglycerides, and the use of several specific types of antihypertensive drugs. After adjustment for the above-mentioned factors, the 24 h pulse pressure (PP) and its components, the elastic and stiffening PPs, were all significantly associated with an uncontrolled office and ambulatory BP status with the standardized odds ratios ranging from 1.09 to 4.68 (P < 0.05). The ambulatory arterial stiffness index (AASI) was only associated with an uncontrolled nighttime and 24 h BP status. In conclusion, the control rates of 24 h ambulatory BP, especially that in the nighttime and morning time windows, were low in Chinese hypertensive patients, which might be associated with arterial stiffness in addition to other common risk factors.

Similar content being viewed by others
Introduction
Hypertension is a major public health challenge. According to the Global Burden of Disease Study, there were 828 million adults with a systolic blood pressure (BP) >140 mm Hg in 2019 worldwide [1]. From 1990 to 2019, the total number of disability-adjusted life years due to high systolic BP increased from 154 million to 235 million [1]. In China, the prevalence of hypertension also rapidly increased from 11.3% in 1991 to 27.9% in 2012–2015 [2]. It is estimated that close to 250 million Chinese people had hypertension, and only 15.3% of the patients had their office BP controlled to the target of <140/90 mmHg [3].
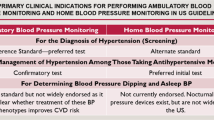
As recommended by most of the recent hypertension guidelines [4, 5], ambulatory BP monitoring has superiorities in hypertension management over office BP measurement. It allows the assessment of BP level and variation during daily activities and in different time windows throughout the day, e.g., in the daytime, nighttime and morning. A large number of prospective studies demonstrated that ambulatory BPs, especially the 24-h and nighttime BPs, were more closely associated with adverse outcomes than office BP [6, 7]. Therefore, ambulatory BP monitoring is considered as a standard method not only for the diagnosis of hypertension but also for evaluating effectiveness of antihypertensive regimens [8]. However, up to now it is unclear about the control rates of ambulatory BP in Chinese hypertensive patients.
Although the technique of the 24 h ambulatory BP monitoring has been applied in China for more than 20 years and is covered by medical insurance, it remains insufficiently used in real clinical practice. One of the barriers is the difficulty in the interpretation and use of the large amount of information provided by ambulatory BP monitoring for doctors, especially those at primary care settings. In addition, diverse reports generated by software from various manufacturers of BP monitors make the use of ambulatory BP monitoring more difficult. To cope with these difficulties, we developed a web-based Shuoyun system (https://www.shuoyun.com.cn), which can retrieve the data from various validated ambulatory BP monitors, and generate a standardized report [9]. In addition, it also paves a way for doctors at the specialized hypertension centres in secondary or tertiary hospitals to help doctors at the primary care centres to manage hypertension by giving advices in the report, no matter how far the geographical distance between hospitals is. From the year of 2018, we have been promoting the application of ambulatory BP monitoring with the use of the Shuoyun system in China, and initiated a registry study in treated hypertensive patients. Using the data of this nationwide registry, we would first analyze the control rates of the ambulatory BPs during the daytime, nighttime, morning and throughout the 24 h, and then to investigate factors associated with the control status of ambulatory BP. As arterial stiffness in terms of increased pulse wave velocity had been demonstrated as a significant predictor of poor response to antihypertensive treatment [10], and it can be indirectly assessed with the indices derived from ambulatory BP monitoring [11, 12], we also analyzed the associations between the ambulatory BP control status and the ambulatory arterial stiffness indices.
Methods
Study patients
The REgistry study on the “ACTION of controlling Ambulatory Blood Pressure to target in ten thousand patients” (REACTION-ABP) has been registered at www.ClinicalTrials.gov (identifier NCT03547856). It was designed as a prospective observational study from the year of 2018 to 2022 to compare cardiovascular outcomes between patients with or without controlled ambulatory blood pressure at baseline and to investigate the control rates of ambulatory blood pressure and the prevalence of white-coat and masked uncontrolled hypertension in Chinese patients with treated hypertension. The study was delayed due to the COVID-19 pandemic and is currently still ongoing in China. It was conducted in accordance with the Declaration of Helsinki. The study protocol was approved by the Ethics Committee of Ruijin Hospital Affiliated to Shanghai Jiaotong University School of Medicine (No. 2017–208) and also by the Ethics Committees of the participating hospitals as appropriate. All participating patients provided written informed consent.
Patients who attended the outpatient clinic in the participating hospitals were selected for inclusion, if they were men or women, aged 18–80 years, treated with antihypertensive medications, had performed the 24 h ambulatory blood pressure monitoring with validated devices, and were willing to provide information of medical history and results of blood biochemical examinations within the most recent 6 months per protocol. Patients who were untreated with antihypertensive drugs, or in hospitalization, or could not participate in the follow-up were excluded from the study.
From June 2018 to December 2022, 4254 patients from 77 hospitals in 25 provinces or municipalities were registered. We excluded 166 patients from the present analysis because the patients were not taking antihypertensive drugs (n = 22), or the ambulatory blood pressure recordings were missing (n = 2), or <70% of the readings that should be obtained according to the measurement settings (n = 19), or performed with the monitors which had not been validated nor listed at the www.stridebp.org (n = 123) [13]. In total, 4088 patients were included in the present analysis.
BP measurement
Ambulatory BP monitoring was performed with the monitors validated and available in each participating hospital. The supplemental Table S1 provides the detailed information about the monitors. Ambulatory BP was taken at 20–30 min intervals during 6:00–22:00 and at 30 min intervals during 22:00–6:00. The study participants were instructed to follow their usual daily activities, avoid vigorous exercise, and remain still during each blood pressure measurement. A brief diary was provided to report the time when they went to bed and arose, had meals, and took antihypertensive medication. After the completion of each 24 h recording, data was uploaded from the BP monitor at each centre to the web-based Shuoyun system (www.shuoyun.com.cn) and was analyzed and reported in a standardized manner according to the current ABPM guidelines [14, 15]. The analysis only included readings from the first 24 h of a recording. Daytime and nighttime were defined as the time awakening or asleep according to the diary. Morning was within the 2 h after getting up from bed. The ambulatory BPs during the 24 h, daytime, nighttime and morning intervals were respectively averaged for each patient. Doctors from the Shanghai Institute of Hypertension (Dr.s MXL, QFH, CSS, and YL) checked each recording and did minimal data editing if deemed necessary, and then issued the ABPM reports. A report sample is shown in the online only supplemental Fig. S1. In the present study, the thresholds for a controlled 24 h, daytime, nighttime and morning hypertension were BP means of <130/80, <135/85, <120/70 and <135/85 mmHg, respectively [14, 15]. A perfect ambulatory BP control was defined when the averages of the 24 h, daytime and nighttime means were all within the above-mentioned target levels.
Office BP measurement was requested to be performed preferably within 1 week of (either before or after) the ambulatory BP monitoring with the validated A&D 767 or 651BLE-W oscillometric monitors (A&D Medical, Kyoto, Japan). A cuff with an appropriately sized bladder was used. After the study participants had rested in the sitting position for at least 5 min, three consecutive BP readings were obtained at 1 min intervals, and immediately transmitted to the web-based Shuoyun System via a microphone or a customized wireless transmission module. These three office BP readings were averaged for analysis. Office BP control was an office BP mean of <140/90 mmHg [16].
Ambulatory arterial stiffness indices
The ambulatory arterial stiffness index (AASI) for each patient was calculated as one minus the regression slope of diastolic on systolic BPs in individual 24 h ABPM recordings [12]. Pulse pressure (PP) was the difference between systolic and diastolic BP. The PP components, that are the elastic PP (elPP) and stiffening PP (stPP), were calculated as previously proposed by Gavish et al [11]. In brief, elPP = PP*ln(K)/(K-1), and K is the ratio between the standard deviations (SD) of systolic and diastolic BP. The elPP was considered as the pressure change during the systole in response to the blood volume change, assuming the arterial stiffness was constant from diastole to systole. However, in real arteries, the artery “stiffens” for increased pressure (or volume). Therefore the stPP, calculated as PP minus elPP, expressed the extra pressure required during the systole to overcome the arterial stiffening from diastole to systole [11].
Other data collection
A standardized questionnaire was administered to collect information on medical history, intake of medications, cigarette smoking and alcohol intake. Body weight was measured with light indoor clothing and without shoes. Body height was measured to the nearest 0.5 cm. Body mass index was calculated as the body weight in kilograms divided by the body height in meters squared. Serum lipids, creatinine and uric acid, and fasting plasma glucose were measured with automatic biochemical analyzers in the participating hospitals. Chronic kidney disease was self-reported. Diabetes mellitus was defined as the current use of antidiabetic agents, or a diagnosis self-reported or documented in hospital records.
Statistical analysis
For database management and statistical analysis, we used SAS software (Version 9.4, SAS Institute Inc, USA). Continuous variables were expressed as mean ± standard deviation (SD) and compared using the unpaired Student’s t test or analyses of variance as appropriate. Categorical variables between independent groups were compared using the Chi-square test. The BP control rates in various time windows were compared with the McNemar test and the Bonferroni correction was performed for multiple pairwise comparisons. Using a stepwise multiple regression procedure with the P value for independent variables to enter and stay in the model set at 0.10, we identified factors associated with uncontrolled ambulatory hypertension. Multiple logistic regression was performed to determine the odds ratios and 95% confidence intervals (CI) associated with a 1-SD increase in the arterial stiffness indices. A two-sided P value of <0.05 was considered statistically significant.
Results
Characteristics of the registered patients
The 4088 participants included 2159 (52.8%) men, and had a mean (SD) age of 58.2 ± 11.8 years. Totally, 645 (15.8%) participants had diabetes mellitus, and 74 (1.8%) had chronic kidney disease. The mean (SD) number of antihypertensive drugs taken by the patients was 1.8 ± 0.9. Patients with perfectly controlled (n = 858) or uncontrolled 24 h ambulatory BP (n = 3230) differed in most of the demographic and clinical characteristics, except the presence of diabetes mellitus and chronic kidney disease, the level of fasting plasma glucose, and the number of antihypertensive drug classes (Table 1).
BP control status
The median (5–95th percentiles) number of the ambulatory BP readings for analyses were 59 (46–65) in the 24 h, 41 (29–49) in the daytime, 16 (11–21) in the nighttime, and 5 (2–6) in the morning. The corresponding mean BP levels were 130.8/79.4, 134.7/81.8, 122.2/73.9 and 137.6/84.1 mmHg, respectively. Among the total 4088 patients, 1915 (46.8%), 1378 (33.7%) and 795 (19.4%) patients used one, two, or three or more classes of antihypertensive drugs, respectively. With the increasing number of antihypertensive drugs, only morning and office systolic BPs were significantly higher (P ≤ 0.001, Table 2).
The BP control rate was the highest in the office (65.7%), moderate in the daytime (45.0%), low in the morning (35.5%) and the lowest in the nighttime (27.6%, P < 0.001, Fig. 1). Only 21.0% of patients had their 24 h BP perfectly controlled. The control rates did not differ among patients taking various number of antihypertensive drugs except that the control rates of office BP were lower in patients taking three or more drugs (Table 2). The stepwise regression analyses identified that the factors associated with an imperfect 24 h BP control included male sex, smoking and drinking habits, a higher body mass index, serum total cholesterol and triglycerides, and the use of angiotensin-receptor blockers, beta-blockers, calcium channel blockers, and the single pill combinations (Fig. 2).
Control rates of the ambulatory blood pressure in the 4088 patients registered in the REACTION-ABP study. For the definitions of daytime, nighttime and morning blood pressure (BP) control, please refer to the Methods. Perfect 24 h BP control means that the 24 h, daytime and nighttime BPs were all controlled. Pairwise comparisons of the rates were all statistically significant (P < 0.001)
Common clinical factors in relation to the perfect 24 h BP control status. Odds ratios and 95% confidence intervals were determined by stepwise regression with the P value for independent variables to enter and stay in the model set at 0.10. In addition to the variables shown in the figure, other factors in the model included age, fasting plasma glucose, serum creatinine, low-density lipoprotein cholesterol, the use of angiotensin-converting enzyme inhibitors, and the use of diuretics. BMI body mass index, ARB angiotensin receptor blockers, CCB calcium channel blockers, SPC single pill combination
BP control status in relation to arterial stiffness indices
In all participants, the 24 h PP and its components, the elastic and stiffening PP, averaged 51.4 mmHg, 41.8 mmHg and 9.6 mmHg, respectively. And the mean AASI was 0.54. The correlation coefficients with the elastic and stiffening PP were 0.888 and 0.653 for the 24 h PP, respectively, and 0.146 and 0.609 for the AASI (P < 0.001, Table S2). The 24-h PP and elastic PP (P ≤ 0.046), but not the stiffening PP or AASI (P ≥ 0.135), increased with the number of antihypertensive drugs (Table 2).
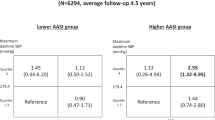
As shown in Fig. 3, the office and ambulatory BP control rates were largely lower (P < 0.05) in patients with a higher median of the PP, irrespective its components. While for AASI, only the control rates during the nighttime and throughout the 24 h differed significantly between the two median groups. After adjustment for age, sex, body mass index, and other significant covariates, the 1-SD increases in the 24 h, elastic and stiffening PP were all significantly associated with an uncontrolled office and the ambulatory BP status with odds ratios ranging from 1.09 to 4.68 (P < 0.05, Table 3). For AASI, the unadjusted and multivariate-adjusted standardized odds ratios were only significant (P < 0.001) for the nighttime BP control status (1.20 and 1.29) and the perfect 24 h BP control status (1.13 and 1.21, Table 3).
Discussion
Based on the data of a nationwide registry, the present study demonstrated that the control rates of ambulatory BPs were low in Chinese hypertensive patients. Only about one fifth of the patients had their ambulatory BP perfectly controlled throughout the whole day, and less than half (45%) had a controlled BP during the daytime, and only one third at the nighttime or in the morning. In addition to the commonly known risk factors for uncontrolled BP, such as male sex, obesity, smoking and alcohol drinking, and dyslipidemia, it was observed that the increased arterial stiffness in terms of a high 24 h PP and its components, and AASI were also related to the ambulatory BP control status.
In the China hypertension survey 2012–2015, the awareness, treatment and control rate of office hypertension in 451 755 adults (≥18 years) was 46.9%, 40.7% and 15.3%, respectively [3]. In those who took antihypertensive medication, the control rate of office BP was 37.6%. In the May Measurement Month (MMM) project carried out in China from the year of 2017 to 2019, more than 600,000 subjects participated in the opportunistic BP measurement [17,18,19]. The major measurement sites were hospital clinics. The BP control rate in hypertensive patients on medications was 64%, 62.7%, and 60.1% in the year of 2017, 2018 and 2019, respectively [17,18,19], which were very similar to the rate of office BP control observed in the present study. Our study firstly reported the control rates of ambulatory BP in Chinese patients with medicated hypertension, which seemed much lower than that in populations from other countries [20, 21]. The Home-Activity information and Communication Technology (ICT)-based Japan Ambulatory Blood Pressure Monitoring Prospective (HI-JAMP) study is also a nationwide registry study of medicated hypertensive patients began in 2017 in Japan [21]. The office, home and ambulatory BPs were measured with a single customized ICT-based multi-sensor ambulatory BP monitoring device. In the 2731 patients analyzed, the control rates of the 24 h, daytime and nighttime BP were 71.0%, 70.4% and 68.8%, respectively, for systolic, and 73.3%, 78.0%, and 57.9%, respectively, for diastolic [21]. The higher control rates in the Japanese than Chinese population might be due to more sufficient use of antihypertensive treatment in the former than the latter population. The median number of antihypertensive agents was 2.2 and the combination therapy was applied in 70.9% patients in the HI-JAMP, while in our study the corresponding values were 1.8 and 53.1%, respectively. A similar phenomenon observed in these two registry studies is the lower control rate of nighttime and morning BPs compared to that of daytime BPs. Therefore, both studies highlighted the importance of the application of out-of-office BP measurement in identifying nighttime and morning hypertension, and the use of long-acting drugs to control BP throughout the day and night in the Asian region [5, 22].
Similar to the MMM study in China [23], we found that in general men had a lower control rate than women and common barriers for blood pressure control in the Chinese population included cigarette smoking and alcohol drinking, a higher body mass index and serum cholesterol, and the under-use of combination therapy. Indeed, in the present study, the use of single pill combination antihypertensive therapy was favorably and independently associated with the 24 h BP control, but unfortunately only one fifth of the patients used such combination.
In addition to the common risk factors, our study also firstly investigated the ambulatory arterial stiffness indices and their relationship with the 24 h BP control. Both the 24 h PP and AASI indirectly reflect arterial elastic function and can be calculated from the data of ambulatory BP monitoring without the need of additional dedicated devices [11, 12]. Recently, the 24 h PP was proposed to be decomposed into two components: the elastic PP and the stiffening PP, associated with the stiffness at the diastole and the change of stiffness during systole, respectively [11]. As observed in the present study, both the elastic and stiffening PP were closely correlated with the 24 h PP with a correlation coefficient of 0.89 and 0.65, respectively. Longitudinal analyses showed that both of the PP components predicted cardiovascular morbidity and mortality but with some difference [24, 25]. In patients aged >60 years, the association of PP with clinical outcomes is mediated by the diastolic stiffness via elPP, while in patients aged <60 years, both components are associated with cause-specific clinical outcomes [25]. In the present study, we found that the 24 h PP and its components were all significantly associated with the ambulatory BP control status, which might be attributable to the fact that patients with stiff arteries would have poor BP control on one hand [10], and the 24 h PP and PP components were mathematically correlated with the ambulatory BP values on the other hand. Interestingly, the associations with the PPs seemed closer with the daytime than the nighttime BP control, and the opposite might be true for AASI. The differences between the ambulatory arterial stiffness indices is intriguing and warranted further investigation.
Our study should be interpreted within the context of its strengths and limitations. The ambulatory BP recordings were in high quality, and the data reporting was performed with a standardized web-based system [9]. The participating centres were almost across the whole country of China. However, as limited by the resources, in this study with a large sample size, we collected data only on common clinical risk factors associated with hypertension control, and missed many other important factors related to diurnal BP variations, such as stress, physical activity, sleep quality, and so on [26, 27]. The present study is cross-sectional and does not allow inferring any causal relationship. Some observed associations, such as the BP control status in relation to the number or specific class of antihypertensive drugs, can be a result of reverse causality, which should be interpreted with caution. In addition, considering the modest reproducibility of the BP phenotype, especially within short time intervals [28], repeated ambulatory BP measurement would be ideal for the assessment of BP control status.
Perspectives in Asia
The HOPE Asia network proposed seven-action approaches for the management of hypertension in Asia [5]. Among the seven actions, reducing morning home BP as the first target and nighttime BP as the second target for high-risk patients were recommended. Our study provides further support to this recommendation as a low control rate of nighttime and morning BP was observed in the real-world hypertensive patients.
Conclusion
The control rates of 24 h ambulatory BP, especially that in the nighttime and morning time windows, were low in Chinese hypertensive patients. More efforts will be needed to promote the control of 24 h ambulatory BP. Increased pulse pressure and ambulatory arterial stiffness were associated with lower ambulatory BP control rates. Future studies are warranted to illustrate the benefit of the 24 h BP control in patients with high versus low levels of arterial stiffness.
References
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 Study. J Am Coll Cardiol. 2020;76:2982–3021.
Wang JG, Zhang W, Li Y, Liu L. Hypertension in China: epidemiology and treatment initiatives. Nat Rev Cardiol. 2023 Jan. Epub ahead of print.
Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. China Hypertension Survey Investigators. Status of hypertension in China: Results from the China Hypertension Survey, 2012-2015. Circulation 2018;137:2344–56.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension global hypertension practice guidelines. J Hypertens. 2020;38:982–1004.
Kario K, Chia YC, Siddique S, Turana Y, Li Y, Chen CH, et al. Seven-action approaches for the management of hypertension in Asia - The HOPE Asia network. J Clin Hypertens (Greenwich). 2022;24:213–23.
Yang WY, Melgarejo JD, Thijs L, Zhang ZY, Boggia J, Wei FF, et al. International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes (IDACO) Investigators. Association of office and ambulatory blood pressure with mortality and cardiovascular outcomes. JAMA 2019;322:409–20.
Narita K, Hoshide S, Kario K. Association of home and ambulatory blood pressure with cardiovascular prognosis in practice hypertensive outpatients. Hypertension 2023;80:451–9.
Huang QF, Yang WY, Asayama K, Zhang ZY, Thijs L, Li Y, et al. Ambulatory blood pressure monitoring to diagnose and manage hypertension. Hypertension 2021;77:254–64.
Wang JG, Li Y, Chia YC, Cheng HM, Minh HV, Siddique S, et al. Hypertension Cardiovascular Outcome Prevention, Evidence (HOPE) Asia Network. Telemedicine in the management of hypertension: Evolving technological platforms for blood pressure telemonitoring. J Clin Hypertens (Greenwich). 2021;23:435–9.
Protogerou A, Blacher J, Stergiou GS, Achimastos A, Safar ME. Blood pressure response under chronic antihypertensive drug therapy: the role of aortic stiffness in the REASON (Preterax in Regression of Arterial Stiffness in a Controlled Double-Blind) study. J Am Coll Cardiol. 2009;53:445–51.
Gavish B, Bursztyn M. Ambulatory pulse pressure components: concept, determination and clinical relevance. J Hypertens. 2019;37:765–74.
Li Y, Wang JG, Dolan E, Gao PJ, Guo HF, Nawrot T, et al. Ambulatory arterial stiffness index derived from 24-hour ambulatory blood pressure monitoring. Hypertension 2006;47:359–64.
Stergiou GS, O’Brien E, Myers M, Palatini P, Parati G, STRIDE BP. Scientific Advisory Board. STRIDE BP: an international initiative for accurate blood pressure measurement. J Hypertens. 2020;38:395–9.
Kario K, Hoshide S, Chia YC, Buranakitjaroen P, Siddique S, Shin J, et al. Guidance on ambulatory blood pressure monitoring: A statement from the HOPE Asia Network. J Clin Hypertens (Greenwich). 2021;23:411–21.
Stergiou GS, Palatini P, Parati G, O’Brien E, Januszewicz A, Lurbe E, et al. European Society of Hypertension Council and the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. 2021 European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021;39:1293–302.
Joint Committee for Guideline Revision. 2018 Chinese guidelines for prevention and treatment of hypertension-A report of the Revision Committee of Chinese Guidelines for Prevention and Treatment of Hypertension. J Geriatr Cardiol. 2019;16:182–241.
Chen X, Xu SK, Li Y, Sheng CS, Guo QH, Yu W, et al. May Measurement Month 2017: an analysis of blood pressure screening results in China-East Asia. Eur Heart J Suppl. 2019;21:D37–39.
Chen X, Li Y, Hu Z, Liu M, Yu J, Wang HY, et al. May Measurement Month 2018: an analysis of blood pressure screening results from China. Eur Heart J Suppl. 2020;22:H40–H42.
Chen X, Liu CY, Xu LY, Wang HY, Liu M, Zhang YQ, Yin XH, Wang XL, Yu J, Li WH, Beaney T, Xia X, Poulter NR, Li Y, Wang JG. May Measurement Month 2019: an analysis of blood pressure screening results from China. Eur Heart J Suppl. 2021;23:B43–B45.
Omboni S, Mancinelli A, Rizzi F, Parati G. TEMPLAR (TEleMonitoring of blood Pressure in Local phARmacies) Project Group. Telemonitoring of 24-hour blood pressure in local pharmacies and blood pressure control in the community: The Templar Project. Am J Hypertens. 2019;32:629–39.
Kario K, Tomitani N, Nishizawa M, Harada N, Kanegae H, Hoshide S. Concept, study design, and baseline blood pressure control status of the nationwide prospective HI-JAMP study using multisensor ABPM. Hypertens Res. 2023;46:357–67.
Kario K, Wang JG, Chia YC, Wang TD, Li Y, Siddique S, et al. The HOPE Asia network 2022 update consensus statement on morning hypertension management. J Clin Hypertens (Greenwich). 2022;24:1112–20.
Chen X, Xu SK, Guo QH, Hu Z, Wang HY, Yu J, et al. Barriers to blood pressure control in China in a large opportunistic screening. J Clin Hypertens (Greenwich). 2020;22:835–41.
Bursztyn M, Kikuya M, Asayama K, Satoh M, Gavish B, Ohkubo T. Do estimated 24-h pulse pressure components affect outcome? Ohasama study J Hypertens 2020;38:1286–92.
Gavish B, Bursztyn M, Thijs L, Wei DM, Melgarejo JD, Zhang ZY, et al. International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcome Investigators. Predictive power of 24-h ambulatory pulse pressure and its components for mortality and cardiovascular outcomes in 11 848 participants recruited from 13 populations. J Hypertens. 2022;40:2245–55.
Parati G, Bilo G, Kollias A, Pengo M, Ochoa JE, Castiglioni P, et al. Blood pressure variability: methodological aspects, clinical relevance and practical indications for management - a European Society of Hypertension position paper. J Hypertens. 2023;41:527–44.
Narita K, Hoshide S, Kario K. Short- to long-term blood pressure variability: Current evidence and new evaluations. Hypertens Res. 2023;46:950–8.
Mancia G, Facchetti R, Vanoli J, Dolfini V, Grassi G. Reproducibility of blood pressure phenotypes identified by office and ambulatory blood pressure in treated hypertensive patients. Data from the PHYLLIS study. Hypertens Res. 2022;45:1599–608.
Acknowledgements
The authors thank all doctors and nurses of the participating centres for their excellent work, and all patients for their voluntary participation in the study.
Funding
The study is financially supported by Bayer (CN-OI-004-BPD) and A&D as an investigator-initiated research project in China. Dr YL is currently also supported by grants from the National Natural Science Foundation of China (grants 82070432 and 82270469) and from the Shanghai Commissions of Health (‘Leading Academics’ 2022LJ022), China.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
YL reports having received research grants from A&D, Bayer, Omron, Salubris, and Shyndec and lecture fees from A&D, Omron, Servier, Salubris and Shyndec. J-GW reports having received research grants, lecture and consulting fees from A&D, Bayer, Novartis, Omron, Servier and Viatris.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, MX., Zhang, DY., Tang, ST. et al. Control status of ambulatory blood pressure and its relationship with arterial stiffness in the China nationwide registry of treated hypertensive patients: the REACTION-ABP study. Hypertens Res 46, 2302–2311 (2023). https://doi.org/10.1038/s41440-023-01336-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01336-5
Keywords
This article is cited by
-
How do we tackle nighttime blood pressure?
Hypertension Research (2023)
-
Visualization of the interplay between arterial properties and 24-hour ambulatory blood pressure during daytime and nighttime, for different age ranges
Hypertension Research (2023)