Abstract
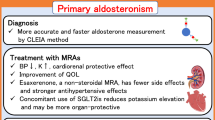
Patients with primary aldosteronism (PA) have a higher risk of cardiovascular disease (CVD) than essential hypertension due to underlying hyperaldosteronism. However, the association between high plasma aldosterone concentrations (PACs) and diurnal blood pressure (BP) variation has not been fully elucidated. Because abnormal ambulatory blood pressure monitoring (ABPM) profiles are associated with increased CVD risk, we investigated the association between PACs and the ABPM profile in 36 patients with PA diagnosed by confirmatory tests who underwent adrenal venous sampling (AVS). The clinical parameters were measured during hospitalization for AVS. The dietary salt intake of hospitalized patients was controlled at 6 g/day. During AVS, blood samples were collected from the inferior vena cava before and 1 h after adrenocorticotropic hormone (ACTH) stimulation to measure the PACs. The post-stimulation PAC had a significant negative correlation with nocturnal BP dipping rates (R = −0.387, p = 0.020), whereas pre-stimulation PAC did not (R = −0.217, p = 0.204). The nocturnal BP dipping rates were significantly lower in the high PAC group (PAC higher than the median) than low PAC group (PAC lower than the median) (p = 0.009). Multiple regression analysis revealed that high PAC was an independent factor contributing to low nocturnal BP dipping rates (β = −0.316, p = 0.038). In conclusion, in patients with PA, hyperaldosteronism is associated with nocturnal hypertension, which is an important risk factor for CVD. Additionally, ACTH stimulation may improve the sensitivity of PACs as a clinical indicator of nocturnal hypertension.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
All relevant data are included within the paper. The datasets are available from the corresponding authors upon reasonable request.
References
Käyser SC, Dekkers T, Groenewoud HJ, van der Wilt GJ, Carel Bakx J, van der Wel MC, et al. Study heterogeneity and estimation of prevalence of primary aldosteronism: A systematic review and meta-regression analysis. J Clin Endocrinol Metab. 2016;101:2826–35.
Burrello J, Monticone S, Losano I, Cavaglià G, Buffolo F, Tetti M, et al. Prevalence of hypokalemia and primary aldosteronism in 5100 patients referred to a tertiary hypertension unit. Hypertension 2020;75:1025–33.
Ohno Y, Sone M, Inagaki N, Yamasaki T, Ogawa O, Takeda Y, et al. Prevalence of cardiovascular disease and its risk factors in primary aldosteronism: A multicenter study in Japan. Hypertension 2018;71:530–7.
Kawashima A, Sone M, Inagaki N, Takeda Y, Itoh H, Kurihara I, et al. Renal impairment is closely associated with plasma aldosterone concentration in patients with primary aldosteronism. Eur J Endocrinol. 2019;181:339–50.
Buffolo F, Tetti M, Mulatero P, Monticone S. Aldosterone as a mediator of cardiovascular damage. Hypertension 2022;79:1899–911.
Murata M, Kitamura T, Tamada D, Mukai K, Kurebayashi S, Yamamoto T, et al. Plasma aldosterone level within the normal range is less associated with cardiovascular and cerebrovascular risk in primary aldosteronism. J Hypertens. 2017;35:1079–85.
Kario K, Shin J, Chen CH, Buranakitjaroen P, Chia YC, Divinagracia R, et al. Expert panel consensus recommendations for ambulatory blood pressure monitoring in Asia: The HOPE Asia Network. J Clin Hypertens (Greenwich). 2019;21:1250–83.
Shintani Y, Kikuya M, Hara A, Ohkubo T, Metoki H, Asayama K, et al. Ambulatory blood pressure, blood pressure variability and the prevalence of carotid artery alteration: the Ohasama study. J Hypertens. 2007;25:1704–10.
Tatasciore A, Renda G, Zimarino M, Soccio M, Bilo G, Parati G, et al. Awake systolic blood pressure variability correlates with target-organ damage in hypertensive subjects. Hypertension 2007;50:325–32.
Kario K. Nocturnal Hypertension: New Technology and Evidence. Hypertension 2018;71:997–1009.
Boggia J, Li Y, Thijs L, Hansen TW, Kikuya M, Björklund-Bodegård K, et al. Prognostic accuracy of day versus night ambulatory blood pressure: A cohort study. Lancet 2007;370:1219–29.
Kario K, Matsuo T, Kobayashi H, Imiya M, Matsuo M, Shimada K. Nocturnal fall of blood pressure and silent cerebrovascular damage in elderly hypertensive patients. Advanced silent cerebrovascular damage in extreme dippers. Hypertension. 1996;27:130–5.
Yano Y, Inokuchi T, Hoshide S, Kanemaru Y, Shimada K, Kario K. Association of poor physical function and cognitive dysfunction with high nocturnal blood pressure level in treated elderly hypertensive patients. Am J Hypertens. 2011;24:285–91.
Yano Y, Ning H, Muntner P, Reis JP, Calhoun DA, Viera AJ, et al. Nocturnal blood pressure in young adults and cognitive function in Midlife: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Hypertens. 2015;28:1240–7.
Hoshide S, Kario K, Hoshide Y, Umeda Y, Hashimoto T, Kunii O, et al. Associations between nondipping of nocturnal blood pressure decrease and cardiovascular target organ damage in strictly selected community-dwelling normotensives. Am J Hypertens. 2003;16:434–8.
Kario K, Hoshide S, Mizuno H, Kabutoya T, Nishizawa M, Yoshida T, et al. Nighttime blood pressure phenotype and cardiovascular prognosis: Practitioner-based nationwide JAMP study. Circulation 2020;142:1810–20.
Middeke M, Schrader J. Nocturnal blood pressure in normotensive subjects and those with white coat, primary, and secondary hypertension. Bmj 1994;308:630–2.
Ceruti M, Petramala L, Cotesta D, Cerci S, Serra V, Caliumi C, et al. Ambulatory blood pressure monitoring in secondary arterial hypertension due to adrenal diseases. J Clin Hypertens (Greenwich). 2006;8:642–8.
Middeke M, Klüglich M, Holzgreve H. Circadian blood pressure rhythm in primary and secondary hypertension. Chronobiol Int. 1991;8:451–9.
Wu Q, Hong M, Xu J, Tang X, Zhu L, Gao P, et al. Diurnal blood pressure pattern and cardiac damage in hypertensive patients with primary aldosteronism. Endocrine 2021;72:835–43.
Penzo M, Palatini P, Rossi GP, Zanin L, Pessina AC. In primary aldosteronism the circadian blood pressure rhythm is similar to that in primary hypertension. Clin Exp Hypertens. 1994;16:659–73.
Mansoor GA, White WB. Circadian blood pressure variation in hypertensive patients with primary hyperaldosteronism. Hypertension 1998;31:843–7.
Libianto R, Menezes S, Kaur A, Gwini SM, Shen J, Narayan O, et al. Comparison of ambulatory blood pressure between patients with primary aldosteronism and other forms of hypertension. Clin Endocrinol (Oxf). 2021;94:353–60.
Azushima K, Tamura K, Haku S, Wakui H, Kanaoka T, Ohsawa M, et al. Effects of the oriental herbal medicine Bofu-tsusho-san in obesity hypertension: A multicenter, randomized, parallel-group controlled trial (ATH-D-14-01021.R2). Atherosclerosis 2015;240:297–304.
Yanagi M, Tamura K, Fujikawa T, Wakui H, Kanaoka T, Ohsawa M, et al. The angiotensin II type 1 receptor blocker olmesartan preferentially improves nocturnal hypertension and proteinuria in chronic kidney disease. Hypertens Res. 2013;36:262–9.
Tamura K, Tsurumi Y, Sakai M, Tanaka Y, Okano Y, Yamauchi J, et al. A possible relationship of nocturnal blood pressure variability with coronary artery disease in diabetic nephropathy. Clin Exp Hypertens. 2007;29:31–42.
Azushima K, Wakui H, Uneda K, Haku S, Kobayashi R, Ohki K, et al. Within-visit blood pressure variability and cardiovascular risk factors in hypertensive patients with non-dialysis chronic kidney disease. Clin Exp Hypertens. 2017;39:665–71.
Mitsuhashi H, Tamura K, Yamauchi J, Ozawa M, Yanagi M, Dejima T, et al. Effect of losartan on ambulatory short-term blood pressure variability and cardiovascular remodeling in hypertensive patients on hemodialysis. Atherosclerosis 2009;207:186–90.
Masuda S, Tamura K, Wakui H, Kanaoka T, Ohsawa M, Maeda A, et al. Effects of angiotensin II type 1 receptor blocker on ambulatory blood pressure variability in hypertensive patients with overt diabetic nephropathy. Hypertens Res. 2009;32:950–5.
Yanase T, Oki Y, Katabami T, Otsuki M, Kageyama K, Tanaka T, et al. New diagnostic criteria of adrenal subclinical Cushing’s syndrome: Opinion from the Japan Endocrine Society. Endocr J. 2018;65:383–93.
Naruse M, Katabami T, Shibata H, Sone M, Takahashi K, Tanabe A, et al. Japan Endocrine Society clinical practice guideline for the diagnosis and management of primary aldosteronism 2021. Endocr J. 2022;69:327–59.
Nanba AT, Nanba K, Byrd JB, Shields JJ, Giordano TJ, Miller BS, et al. Discordance between imaging and immunohistochemistry in unilateral primary aldosteronism. Clin Endocrinol (Oxf). 2017;87:665–72.
Young WF Jr. Diagnosis and treatment of primary aldosteronism: practical clinical perspectives. J Intern Med. 2019;285:126–48.
Zelinka T, Widimský J. Twenty-Four hour blood pressure profile in subjects with different subtypes of primary aldosteronism. Physiol Res. 2001;50:51–57.
Takakuwa H, Shimizu K, Izumiya Y, Kato T, Nakaya I, Yokoyama H, et al. Dietary sodium restriction restores nocturnal reduction of blood pressure in patients with primary aldosteronism. Hypertens Res. 2002;25:737–42.
Bollag WB. Regulation of aldosterone synthesis and secretion. Compr Physiol. 2014;4:1017–55.
Kem DC, Weinberger MH, Higgins JR, Kramer NJ, Gomez-Sanchez C, Holland OB. Plasma aldosterone response to ACTH in primary aldosteronism and in patients with low renin hypertension. J Clin Endocrinol Metab. 1978;46:552–60.
Saruta T, Okuno T, Eguchi T, Nakamura R, Saito I, Kondo K, et al. Responses of aldosterone-producing adenomas to ACTH and angiotensins. Acta Endocrinol (Copenh). 1979;92:702–9.
Rossi GP, Barisa M, Allolio B, Auchus RJ, Amar L, Cohen D, et al. The Adrenal Vein Sampling International Study (AVIS) for identifying the major subtypes of primary aldosteronism. J Clin Endocrinol Metab. 2012;97:1606–14.
Weinberger MH, Grim CE, Hollifield JW, Kem DC, Ganguly A, Kramer NJ, et al. Primary aldosteronism: diagnosis, localization, and treatment. Ann Intern Med. 1979;90:386–95.
Uzu T, Ishikawa K, Fujii T, Nakamura S, Inenaga T, Kimura G. Sodium restriction shifts circadian rhythm of blood pressure from nondipper to dipper in essential hypertension. Circulation 1997;96:1859–62.
Kimura G. Kidney and circadian blood pressure rhythm. Hypertension 2008;51:827–8.
Hannemann A, Wallaschofski H, Lüdemann J, Völzke H, Markus MR, Rettig R, et al. Plasma aldosterone levels and aldosterone-to-renin ratios are associated with endothelial dysfunction in young to middle-aged subjects. Atherosclerosis 2011;219:875–9.
Gkaliagkousi E, Anyfanti P, Triantafyllou A, Gavriilaki E, Nikolaidou B, Lazaridis A, et al. Aldosterone as a mediator of microvascular and macrovascular damage in a population of normotensive to early-stage hypertensive individuals. J Am Soc Hypertens. 2018;12:50–57.
Park S, Kim JB, Shim CY, Ko YG, Choi D, Jang Y, et al. The influence of serum aldosterone and the aldosterone-renin ratio on pulse wave velocity in hypertensive patients. J Hypertens. 2007;25:1279–83.
Satoh M, Kikuya M, Hara A, Ohkubo T, Mori T, Metoki H, et al. Aldosterone-to-renin ratio and home blood pressure in subjects with higher and lower sodium intake: the Ohasama study. Hypertens Res. 2011;34:361–6.
Schweda F. Salt feedback on the renin-angiotensin-aldosterone system. Pflug Arch. 2015;467:565–76.
Fallo F, Castellano I, Gomez-Sanchez CE, Rhayem Y, Pilon C, Vicennati V, et al. Histopathological and genetic characterization of aldosterone-producing adenomas with concurrent subclinical cortisol hypersecretion: a case series. Endocrine 2017;58:503–12.
Mulatero P, Monticone S, Deinum J, Amar L, Prejbisz A, Zennaro MC, et al. Genetics, prevalence, screening and confirmation of primary aldosteronism: A position statement and consensus of the Working Group on Endocrine Hypertension of The European Society of Hypertension. J Hypertens. 2020;38:1919–28.
Alnazer RM, Veldhuizen GP, Kroon AA, de Leeuw PW. The effect of medication on the aldosterone-to-renin ratio. A critical review of the literature. J Clin Hypertens (Greenwich). 2021;23:208–14.
Acknowledgements
We thank Textcheck for editing and reviewing the English in this manuscript.
Funding
This work was supported by grants from the Yokohama Foundation for Advancement of Medical Science; Uehara Memorial Foundation; Japan Society for the Promotion of Science; Japan Kidney Association-Nippon Boehringer Ingelheim Joint Research Program; Japanese Association of Dialysis Physicians; Salt Science Research Foundation; Strategic Research Project of Yokohama City University; Japan Agency for Medical Research and Development (AMED); Translational Research Program; Strategic Promotion for Practical Application of Innovative Medical Technology (TR-SPRINT) from AMED; Moriya Scholarship Foundation; Bayer Scholarship for Cardiovascular Research; and Mochida Memorial Foundation for Medical and Pharmaceutical Research.
Author information
Authors and Affiliations
Contributions
KA designed and conducted the research. KA, RM, TH, KK, HW, and KT wrote the manuscript. KA, RM, SS, RK, SK, TK, YT, and HW performed the research. KA, RM, SS, and TH analyzed the data. KT supervised the research. All authors approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morita, R., Azushima, K., Sunohara, S. et al. High plasma aldosterone concentration is associated with worse 24-h ambulatory blood pressure profile in patients with primary aldosteronism. Hypertens Res 46, 1995–2004 (2023). https://doi.org/10.1038/s41440-023-01325-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01325-8
Keywords
This article is cited by
-
The potential of a new nomogram for the diagnosis of primary aldosteronism
Hypertension Research (2023)
-
Importance of plasma aldosterone concentrations as a clinical indicator of nocturnal hypertension in primary aldosteronism
Hypertension Research (2023)