Abstract
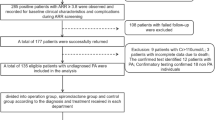
Low renin hypertension (LRH) is a common condition in hypertensive patients, and mainly includes primary aldosteronism (PA) and low renin essential hypertension. To investigate the distributions and clinical manifestations of the main LRH forms, we reviewed 1267 hypertensive patients who underwent assessment for plasma renin activity (PRA) and plasma aldosterone concentration (PAC) by standardized protocols in our specialized center. LRH was defined as PRA < 1.0 ng/mL/h. A saline infusion test (SIT) was performed when LRH patients showed positive screening results for PA. The main LRH forms were defined as follows: post-SIT PAC > 10 ng/dL as ‘overt PA’, post-SIT PAC 5–10 ng/dL as ‘mild PA’, and post-SIT PAC < 5 ng/dL or negative screening results as ‘non-PA’. Overall, 760 patients were defined as LRH, with 160 classified as overt PA, 268 as mild PA, and 332 as non-PA. The total proportion of PA amounted to 56.3% with 21.0% overt PA and 35.3% mild PA. Compared with the mild PA, patients with overt PA had higher systolic and diastolic blood pressures, lower serum potassium, higher urine potassium excretion, more frequent incidence of stage 3 hypertension, hypokalemia, diabetes mellitus, and classical unilateral adenoma on computerized tomography (P < 0.05). PA including overt and mild forms is indeed a major form of LRH. Clinical manifestations in mild PA are less severe than those in overt PA. Nevertheless, mild PA is more prevalent than overt PA in LRH and should be recognized.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Laragh JH. Vasoconstriction-volume analysis for understanding and treating hypertension: the use of renin and aldosterone profiles. Am J Med. 1973;55:261–74.
Ganguly A, Weinberger MH. Low renin hypertension: a current review of definitions and controversies. Am Heart J. 1979;98:642–52.
Gordon RD, Laragh JH, Funder JW. Low renin hypertensive states: perspectives, unsolved problems, future research. Trends Endocrinol Metab. 2005;16:108–13.
Monticone S, Burrello J, Tizzani D, Bertello C, Viola A, Buffolo F, et al. Prevalence and clinical manifestations of primary aldosteronism encountered in primary care practice. J Am Coll Cardiol. 2017;69:1811–20.
Hannemann A, Wallaschofski K. Prevalence of primary aldosteronism in patient cohort and in population-based studies: a review of the current literature. Horm Metabol Res. 2012;44:157–62.
Mulatero P, Verhovez A, Morello F, Veglio F. Diagnosis and treatment of low-renin hypertension. Clin Endocrinol. 2007;67:324–34.
Adlin EV, Braitman LE, Vasan RS. Bimodal aldosterone distribution in low-renin hypertension. Am J Hypertens. 2013;26:1076–85.
Baudrand R, Vaidya A. The low-renin hypertension phenotype: genetics and the role of the mineralocorticoid receptor. Int J Mol Sci. 2018;19:E546.
Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol. 2005;45:1243–8.
Mulatero P, Monticone S, Bertello C, Viola A, Tizzani D, Iannaccone A, et al. Long-term cardio- and cerebrovascular events in patients with primary aldosteronism. J Clin Endocrinol Metab. 2013;98:4826–33.
Ohno Y, Sone M, Inagaki N, Yamasaki T, Ogawa O, Takeda Y, et al. Prevalence of cardiovascular disease and its risk factors in primary aldosteronism: a multicenter study in Japan. Hypertension. 2018;71:530–7.
Giacchetti G, Mulatero P, Mantero F, Veglio F, Boscaro M, Fallo F. Primary aldosteronism, a major form of low renin hypertension: from screening to diagnosis. Trends Endocrinol Metab. 2008;19:104–8.
Baudrand R, Guarda FJ, Fardella C, Hundemer G, Brown J, Williams G, et al. Continuum of renin-independent aldosteronism in normotension. Hypertension. 2017;69:950–6.
Piaditis G, Markou A, Papanastasiou L, Androulakis II, Kaltsas G. Progress in aldosteronism: a review of the prevalence of primary aldosteronism in pre-hypertension and hypertension. Eur J Endocrinol. 2015;172:R191–203.
Douma S, Petidis K, Doumas M, Papaefthimiou P, Triantafyllou A, Kartali N, et al. Prevalence of primary hyperaldosteronism in resistant hypertension: a retrospective observational study. Lancet. 2008;371:1921–6.
Sywak M, Pasieka JL. Long-term follow-up and cost benefit of adrenalectomy in patients with primary hyperaldosteronism. Br J Surg. 2002;89:1587–93.
Wu VC, Wang SM, Chang CH, Hu YH, Lin LY, Lin YH, et al. Long term outcome of Aldosteronism after target treatments. Sci Rep. 2016;6:32103.
Stowasser M, Gordon RD. Primary aldosteronism–careful investigation is essential and rewarding. Mol Cell Endocrinol. 2004;217:33–9.
Mosso L, Carvajal C, Gonzalez A, Barraza A, Avila F, Montero J, et al. Primary aldosteronism and hypertensive disease. Hypertension. 2003;42:161–5.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2008;93:3266–81.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:1889–916.
Käyser SC, Dekkers T, Groenewoud HJ, van der Wilt GJ, Carel Bakx J, van der Wel MC, et al. Study heterogeneity and estimation of prevalence of primary aldosteronism: a systematic review and meta-regression analysis. J Clin Endocrinol Metab. 2016;101:2826–35.
Luo Q, Li NF, Yao XG, Zhang DL, Abulikemu SF, Chang GJ, et al. Potential effects of age on screening for primary aldosteronism. J Hum Hypertens. 2016;30:53–61.
Rossi GP, Auchus RJ, Brown M, Lenders JW, Naruse M, Plouin PF, et al. An expert consensus statement on use of adrenal vein sampling for the subtyping of primary aldosteronism. Hypertension. 2014;63:151–60.
The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med. 1997;157:2413–46.
Stowasser M, Ahmed AH, Cowley D, Wolley M, Guo Z, McWhinney BC, et al. Comparison of seated with recumbent saline suppression testing for the diagnosis of primary aldosteronism. J Clin Endocrinol Metab. 2018;103:4113–24.
Brown JM, Robinson-Cohen C, Luque-Fernandez MA, Allison MA, Baudrand R, Ix JH, et al. The spectrum of subclinical primary aldosteronism and incident hypertension: a Cohort Study. Ann Intern Med. 2017;167:630–41.
Markou A, Pappa T, Kaltsas G, Gouli A, Mitsakis K, Tsounas P, et al. Evidence of primary aldosteronism in a predominantly female cohort of normotensive individuals: a very high odds ratio for progression into arterial hypertension. J Clin Endocrinol Metab. 2013;98:1409–16.
Heinrich DA, Adolf C, Rump LC, Quack I, Quinkler M, Hahner S, et al. Primary aldosteronism: key characteristics at diagnosis: a trend toward milder forms. Eur J Endocrinol. 2018;178:605–11.
Omata K, Anand SK, Hovelson DH, Liu CJ, Yamazaki Y, Nakamura Y, et al. Aldosterone-producing cell clusters frequently harbor somatic mutations and accumulate with age in normal adrenals. J Endocr Soc. 2017;1:787–99.
Omata K, Tomlins SA, Rainey WE. Aldosterone-producing cell clusters in normal and pathological states. Horm Metab Res. 2017;49:951–6.
Weigel M, Riester A, Hanslik G, Lang K, Willenberg HS, Endres S, et al. Post-saline infusion test aldosterone levels indicate severity and outcome in primary aldosteronism. Eur J Endocrinol. 2015;172:443–50.
Hayashi R, Tamada D, Murata M, Mukai K, Kitamura T, Otsuki M, et al. Saline Infusion Test highly associated with the incidence of cardio-and cerebrovascular events in primary aldosteronism. Endocr J. 2017;64:507–13.
Ori Y, Chagnac A, Korzets A, Zingerman B, Herman-Edelstein M, Bergman M, et al. Regression of left ventricular hypertrophy in patients with primary aldosteronism/low-renin hypertension on low-dose spironolactone. Nephrol Dial Transpl. 2013;28:1787–93.
Murata M, Kitamura T, Tamada D, Mukai K, Kurebayashi S, Yamamoto T, et al. Plasma aldosterone level within the normal range is less associated with cardiovascular and cerebrovascular risk in primary aldosteronism. J Hypertens. 2017;35:1079–85.
Acknowledgements
This study was supported by Grant 81660139 from the National Natural Science Foundation of China and the non-profit Central Research Institute Fund of the Chinese Academy of Medical Sciences [2019PT330003]. No interventions were used in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human participants and/or animals
This study retrospectively analyzed data generated in a clinical process.
Informed consent
This was a retrospective data analysis that did not require informed consent from participants. The ethical committee of our hospital approved the study design and data analysis.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Luo, Q., Li, N., Wang, M. et al. Mild primary aldosteronism (PA) followed by overt PA are possibly the most common forms of low renin hypertension: a single-center retrospective study. J Hum Hypertens 34, 633–640 (2020). https://doi.org/10.1038/s41371-019-0291-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-019-0291-y