Abstract
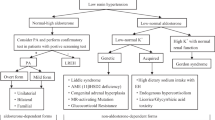
Primary aldosteronism (PA) is caused by excessive secretion of aldosterone from the adrenal glands, with subsequent changes in the renin-angiotensin system. In Japan, chemiluminescent enzyme immunoassay is currently performed for aldosterone assay rather than the earlier method of radioimmunoassay. This change in aldosterone measurement methods has resulted in faster and more accurate measurement of blood aldosterone levels. Since 2019, esaxerenone, a mineralocorticoid receptor antagonist (MRA) with a non-steroidal skeleton, has been available in Japan for the treatment of hypertension. Esaxerenone has been reported to have various effects, such as strong antihypertensive and anti-albuminuric/proteinuric effects. Treatment of PA with MRAs has been reported to improve the patient’s quality of life and to suppress the onset of cardiovascular events independent of their effects on blood pressure. Measuring renin levels is recommended for monitoring the extent of mineralocorticoid receptor blockade during MRA treatment. Patients receiving MRAs are prone to developing hyperkalemia, and combining MRAs with sodium/glucose cotransporter 2 inhibitors is expected to prevent severe hyperkalemia and provide additional cardiorenal protection. Mineralocorticoid receptor-associated hypertension is a broad concept of hypertension that includes not only PA, but also hypertension caused by borderline aldosteronism, obesity, diabetes, and sleep apnea syndrome.

New findings on primary aldosteronism, which is part of MR-associated hypertension. Aldosterone measurements have been changed to the CLEIA method. Treatment of primary aldosteronism with MRAs has a variety of positive effects. CT-guided radiofrequency ablation and transarterial embolization are alternatives to surgery for aldosterone-producing adenomas. BP blood pressure, CLEIA chemiluminescent enzyme immunoassay, CT computed tomography, K serum potassium, MR mineralocorticoid receptor, MRA mineralocorticoid receptor antagonist, QOL quality of life, SGLT2i sodium/glucose cotransporter 2 inhibitor.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Mulatero P, Stowasser M, Loh KC, Fardella CE, Gordon RD, Mosso L, et al. Increased diagnosis of primary aldosteronism, including surgically correctable forms, in centers from five continents. J Clin Endocrinol Metab. 2004;89:1045–50.
Rossi GP, Bernini G, Caliumi C, Desideri G, Fabris B, Ferri C, et al. A prospective study of the prevalence of primary aldosteronism in 1125 hypertensive patients. J Am Coll Cardiol. 2006;48:2293–300.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:1889–916.
Born-Frontsberg E, Reincke M, Rump LC, Hahner S, Diederich S, Lorenz R, et al. Cardiovascular and cerebrovascular comorbidities of hypokalemic and normokalemic primary aldosteronism: results of the German Conn’s Registry. J Clin Endocrinol Metab. 2009;94:1125–30.
Ohno Y, Sone M, Inagaki N, Yamasaki T, Ogawa O, Takeda Y, et al. Prevalence of cardiovascular disease and its risk factors in primary aldosteronism: a multicenter study in Japan. Hypertension. 2018;71:530–7.
Ozeki Y, Tanimura Y, Nagai S, Nomura T, Kinoshita M, Shibuta K, et al. Development of a new chemiluminescent enzyme immunoassay using a two-step sandwich method for measuring aldosterone concentrations. Diagnostics (Basel). 2021;11:433.
Teruyama K, Naruse M, Tsuiki M, Kobayashi H. Novel chemiluminescent immunoassay to measure plasma aldosterone and plasma active renin concentrations for the diagnosis of primary aldosteronism. J Hum Hypertens. 2022;36:77–85.
Nishikawa T, Satoh F, Takashi Y, Yanase T, Itoh H, Kurihara I, et al. Comparison and commutability study between standardized liquid chromatography-mass spectrometry/mass spectrometry (LC-MS/MS) and chemiluminescent enzyme immunoassay for aldosterone measurement in blood. Endocr J. 2022;69:45–54.
Ozeki Y, Kinoshita M, Miyamoto S, Yoshida Y, Okamoto M, Gotoh K, et al. Re-assessment of the oral salt loading test using a new chemiluminescent enzyme immunoassay based on a two-step sandwich method to measure 24-hour urine aldosterone excretion. Front Endocrinol (Lausanne). 2022;13:859347.
Naruse M, Katabami T, Shibata H, Sone M, Takahashi K, Tanabe A, et al. Japan Endocrine Society clinical practice guideline for the diagnosis and management of primary aldosteronism 2021. Endocr J. 2022;69:327–59.
Morimoto R, Ono Y, Tezuka Y, Kudo M, Yamamoto S, Arai T, et al. Rapid screening of primary aldosteronism by a novel chemiluminescent immunoassay. Hypertension. 2017;70:334–41.
Amar L, Baguet JP, Bardet S, Chaffanjon P, Chamontin B, Douillard C, et al. SFE/SFHTA/AFCE primary aldosteronism consensus: Introduction and handbook. Ann Endocrinol (Paris). 2016;77:179–86.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension guidelines for the management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Jeunemaitre X, Chatellier G, Kreft-Jais C, Charru A, DeVries C, Plouin PF, et al. Efficacy and tolerance of spironolactone in essential hypertension. Am J Cardiol. 1987;60:820–5.
Karagiannis A, Tziomalos K, Papageorgiou A, Kakafika AI, Pagourelias ED, Anagnostis P, et al. Spironolactone versus eplerenone for the treatment of idiopathic hyperaldosteronism. Expert Opin Pharmacother. 2008;9:509–15.
Karashima S, Yoneda T, Kometani M, Ohe M, Mori S, Sawamura T, et al. Comparison of eplerenone and spironolactone for the treatment of primary aldosteronism. Hypertens Res. 2016;39:133–7.
Parthasarathy HK, Ménard J, White WB, Young WF Jr, Williams GH, Williams B, et al. A double-blind, randomized study comparing the antihypertensive effect of eplerenone and spironolactone in patients with hypertension and evidence of primary aldosteronism. J Hypertens. 2011;29:980–90.
Rakugi H, Yamakawa S, Sugimoto K. Management of hyperkalemia during treatment with mineralocorticoid receptor blockers: findings from esaxerenone. Hypertens Res. 2021;44:371–85.
Arai K, Homma T, Morikawa Y, Ubukata N, Tsuruoka H, Aoki K, et al. Pharmacological profile of CS-3150, a novel, highly potent and selective non-steroidal mineralocorticoid receptor antagonist. Eur J Pharm. 2015;761:226–34.
Kario K, Ito S, Itoh H, Rakugi H, Okuda Y, Yamakawa S. Effect of esaxerenone on nocturnal blood pressure and natriuretic peptide in different dipping phenotypes. Hypertens Res. 2022;45:97–105.
Satoh F, Ito S, Itoh H, Rakugi H, Shibata H, Ichihara A, et al. Efficacy and safety of esaxerenone (CS-3150), a newly available nonsteroidal mineralocorticoid receptor blocker, in hypertensive patients with primary aldosteronism. Hypertens Res. 2021;44:464–72.
Ito S, Itoh H, Rakugi H, Okuda Y, Iijima S. Antihypertensive effects and safety of esaxerenone in patients with moderate kidney dysfunction. Hypertens Res. 2021;44:489–97.
Ichikawa S, Tsutsumi J, Sugimoto K, Yamakawa S. Antihypertensive effect of long-term monotherapy with esaxerenone in patients with essential hypertension: relationship between baseline urinary sodium excretion and its antihypertensive effect. Adv Ther. 2022;39:4779–91.
Ito S, Kashihara N, Shikata K, Nangaku M, Wada T, Okuda Y, et al. Esaxerenone (CS-3150) in patients with type 2 diabetes and microalbuminuria (ESAX-DN): phase 3 randomized controlled clinical trial. Clin J Am Soc Nephrol. 2020;15:1715–27.
Uchida HA, Nakajima H, Hashimoto M, Nakamura A, Nunoue T, Murakami K, et al. Efficacy and safety of esaxerenone in hypertensive patients with diabetic kidney disease: a multicenter, open-label, prospective study. Adv Ther. 2022;39:5158–75.
Bavuu O, Fukuda D, Ganbaatar B, Matsuura T, Ise T, Kusunose K, et al. Esaxerenone, a selective mineralocorticoid receptor blocker, improves insulin sensitivity in mice consuming high-fat diet. Eur J Pharm. 2022;931:175190.
Qiang P, Hao J, Yang F, Han Y, Chang Y, Xian Y, et al. Esaxerenone inhibits the macrophage-to-myofibroblast transition through mineralocorticoid receptor/TGF-β1 pathway in mice induced with aldosterone. Front Immunol. 2022;13:948658.
Yamamoto H, Yoshida N, Kihara S. Esaxerenone blocks vascular endothelial inflammation through SGK1. J Cardiovasc Pharm. 2022;80:583–91.
Bakris GL, Agarwal R, Anker SD, Pitt B, Ruilope LM, Rossing P, et al. Effect of finerenone on chronic kidney disease outcomes in type 2 diabetes. N. Engl J Med. 2020;383:2219–29.
Pitt B, Filippatos G, Agarwal R, Anker SD, Bakris GL, Rossing P, et al. Cardiovascular events with finerenone in kidney disease and type 2 diabetes. N. Engl J Med. 2021;385:2252–63.
Agarwal R, Filippatos G, Pitt B, Anker SD, Rossing P, Joseph A, et al. Cardiovascular and kidney outcomes with finerenone in patients with type 2 diabetes and chronic kidney disease: the FIDELITY pooled analysis. Eur Heart J. 2022;43:474–84.
Ahmed AH, Gordon RD, Sukor N, Pimenta E, Stowasser M. Quality of life in patients with bilateral primary aldosteronism before and during treatment with spironolactone and/or amiloride, including a comparison with our previously published results in those with unilateral disease treated surgically. J Clin Endocrinol Metab. 2011;96:2904–11.
Velema M, Dekkers T, Hermus A, Timmers H, Lenders J, Groenewoud H, et al. Quality of life in primary aldosteronism: a comparative effectiveness study of adrenalectomy and medical treatment. J Clin Endocrinol Metab. 2018;103:16–24.
Yoshida Y, Yoshida R, Shibuta K, Ozeki Y, Okamoto M, Gotoh K, et al. Quality of life of primary aldosteronism patients by mineralocorticoid receptor antagonists. J Endocr Soc. 2021;5:bvab020.
Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endocrinol. 2018;6:51–9.
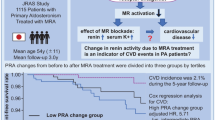
Yoshida Y, Fujiki R, Kinoshita M, Sada K, Miyamoto S, Ozeki Y, et al. Importance of dietary salt restriction for patients with primary aldosteronism during treatment with mineralocorticoid receptor antagonists: The potential importance of post-treatment plasma renin levels. Hypertens Res. 2023;46:100–7.
Nomura M, Kurihara I, Itoh H, Ichijo T, Katabami T, Tsuiki M, et al. Association of cardiovascular disease risk and changes in renin levels by mineralocorticoid receptor antagonists in patients with primary aldosteronism. Hypertens Res. 2022;45:1476–85.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:e240–327.
Epstein M, Calhoun DA. Aldosterone blockers (mineralocorticoid receptor antagonism) and potassium-sparing diuretics. J Clin Hypertens (Greenwich). 2011;13:644–8.
Shikata K, Ito S, Kashihara N, Nangaku M, Wada T, Okuda Y, et al. Reduction in the magnitude of serum potassium elevation in combination therapy with esaxerenone (CS-3150) and sodium-glucose cotransporter 2 inhibitor in patients with diabetic kidney disease: subanalysis of two phase III studies. J Diabetes Investig. 2022;13:1190–202.
Bohm M, Anker SD, Butler J, Filippatos G, Ferreira JP, Pocock SJ, et al. Empagliflozin improves cardiovascular and renal outcomes in heart failure irrespective of systolic blood pressure. J Am Coll Cardiol. 2021;78:1337–48.
Mogi M, Maruhashi T, Higashi Y, Masuda T, Nagata D, Nagai M, et al. Update on Hypertension Research in 2021. Hypertens Res. 2022;45:1276–97.
Tanaka A, Shibata H, Node K. Suspected borderline aldosteronism in hypertension: the next target? J Am Coll Cardiol. 2020;76:759–60.
Shibata H, Itoh H. Mineralocorticoid receptor-associated hypertension and its organ damage: clinical relevance for resistant hypertension. Am J Hypertens. 2012;25:514–23.
Shibata H. Exosomes and exosomal cargo in urinary extracellular vesicles: novel potential biomarkers for mineralocorticoid-receptor-associated hypertension. Hypertens Res. 2021;44:1668–70.
Burrello J, Burrello A, Pieroni J, Sconfienza E, Forestiero V, Rabbia P, et al. Development and validation of prediction models for subtype diagnosis of patients with primary aldosteronism. J Clin Endocrinol Metab. 2020;105:dgaa379.
Kaneko H, Umakoshi H, Ogata M, Wada N, Iwahashi N, Fukumoto T, et al. Machine learning based models for prediction of subtype diagnosis of primary aldosteronism using blood test. Sci Rep. 2021;11:9140.
Karashima S, Kawakami M, Nambo H, Kometani M, Kurihara I, Ichijo T, et al. A hyperaldosteronism subtypes predictive model using ensemble learning. Sci Rep. 2023;13:3043.
Chen Cardenas SM, Santhanam P. (11)C-metomidate PET in the diagnosis of adrenal masses and primary aldosteronism: a review of the literature. Endocrine. 2020;70:479–87.
Liu SY, Chu CM, Kong AP, Wong SK, Chiu PW, Chow FC, et al. Radiofrequency ablation compared with laparoscopic adrenalectomy for aldosterone-producing adenoma. Br J Surg. 2016;103:1476–86.
Sun F, Liu X, Zhang H, Zhou X, Zhao Z, He H, et al. Catheter-based adrenal ablation: an alternative therapy for patients with aldosterone-producing adenoma. Hypertens Res. 2023;46:91–9.
Williams TA, Gomez-Sanchez CE, Rainey WE, Giordano TJ, Lam AK, Marker A, et al. International histopathology consensus for unilateral primary aldosteronism. J Clin Endocrinol Metab. 2021;106:42–54.
Acknowledgements
We would like to thank Masaki Mogi, Tatsuo Shimosawa, Kazuomi Kario, and Hiroshi Itoh, members of the Japanese Society of Hypertension for providing us with the opportunity to write this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
HS has honorarium from Daiichi-Sankyo Company, Mochida Pharmaceuticals, Astrazeneca, Novartis Pharma, Bayer, and Astellas. HS also received scholarship from Chugai and Bayer.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yoshida, Y., Shibata, H. Recent progress in the diagnosis and treatment of primary aldosteronism. Hypertens Res 46, 1738–1744 (2023). https://doi.org/10.1038/s41440-023-01288-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01288-w