Abstract
China is undergoing the nutrition transition that may explain partly the high prevalence of hypertension. We aimed to investigate the longitudinal association between dietary patterns and hypertension in Chinese adults over 28 years of follow-up. We used data collected in the China Health and Nutrition Survey from 1991 to 2018. Adults aged 18 years and above (n = 15,929) were included in the analysis, for whom questionnaires and anthropometric data were collected during at least two waves. Factor analysis was conducted to derive food patterns based on 18 foods or food groups. We constructed three-level mixed-effect linear regression models to estimate systolic blood pressure (SBP) and diastolic blood pressure (DBP) in relation to quartiles of dietary pattern score and performed three-level mixed-effect logistic regression models to assess the risk of hypertension. Participants in the top quartile of the modern pattern had a decrease in SBP (β = − 0.51; 95% CI −0.86, −0.16; P < 0.01) when adjusted for all potential confounders, whereas participants in the top quartile of the meat pattern had an increase in DBP (β = 0.31; 95% CI 0.08, 0.53; P < 0.01). Participants in the highest quartile of the meat pattern were more likely to have hypertension (OR = 1.14; 95% CI 1.03, 1.24; P < 0.01). Adherence to the modern pattern characterized by high intake of fruits and dairy products was inversely associated with SBP, whereas the meat pattern was positively associated with DBP and the risk of hypertension. These findings may well have important public health implications.

Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is the top leading cause of death in China, which accounted for about 44% and 47% of total deaths in urban and rural areas in 2019 respectively, according to the Annual Report on Cardiovascular Health and Diseases in China (2021) released by the National Center for Cardiovascular Diseases [1]. Among the many established risk factors for CVD, high blood pressure (BP) plays an important role and has a high prevalence of exposure [2,3,4]. China has experienced a growing burden of hypertension over the past decades, and the prevalence rate in adults was 27.5% in 2018 [5, 6]. The increase rate of deaths and mortality attributed to hypertension among Chinese residents were 112.72% and 77.04% respectively from 1990 to 2019 [7].
It has been recognized that unhealthy diet is an important risk factor affecting BP and dietary interventions can be effective as a strategy in the prevention and management of hypertension [8, 9]. Dietary pattern analysis has emerged as an alternative approach to provide more practical and meaningful diet information in nutritional epidemiology [10]. Several existing studies have identified various dietary patterns that are differently associated with BP and hypertension [11,12,13]. The Mediterranean diet (MED) and the Dietary Approaches to Stop Hypertension (DASH) diet that can have the protective effects against hypertension have been recommended and adopted as healthy dietary patterns by many countries [14,15,16,17,18]. However, most of the studies were performed in western communities and the results may not be capable to other populations because of the differing food culture and eating habit.
China is undergoing the nutrition transition from traditional dietary patterns to western dietary patterns, which may explain partly the high prevalence of hypertension [19, 20]. There is a need for public health professionals to provide dietary recommendation to persons who need to lower their BP or prevent development of hypertension. Previous studies have shown the association between dietary patterns and hypertension among Chinese population, which mostly were based either on cross-sectional surveys or on provincial data [21,22,23,24,25,26,27]. To add the substantial evidence, the current study aimed to investigate the longitudinal association between dietary patterns and hypertension in Chinese adults over 28 years of follow-up.
Methods
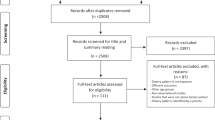
Study population
We used data collected in the China Health and Nutrition Survey (CHNS), an ongoing large-scale, longitudinal, household-based survey initiated in 1989 and continuing in 2018. The CHNS used a multistage random-cluster process to draw the sample from the original eight provinces to final fifteen provinces: Heilongjiang, Liaoning, Beijing, Henan, Jiangsu, Zhejiang, Shanghai, Shandong, Hubei, Hunan, Shaanxi, Yunnan, Chongqing, Guizhou, and Guangxi, which varied in demography, geography, economic development, and public resources. In each province, we selected 2 cities and 4 counties by income and randomly selected 4 communities in each city or county. We randomly selected 20 households in each community. All household members were interviewed from September to November and followed in next subsequent waves. The detailed design and sampling have been reported elsewhere [28, 29]. For this study we used ten waves of the survey conducted in 1991, 1993, 1997, 2000, 2004, 2006, 2009, 2011, 2015, and 2018. Adults aged 18 years and above (n = 20,439) were included in the present analysis, for whom questionnaires and anthropometric data were collected during at least two waves. We excluded pregnant or lactating women (n = 146), those being hypertensive at baseline (n = 4233), and those having implausible data (n = 131, < 800 kilocalories [kcal] per day or > 6000 kcal for men and < 600 kcal or > 4000 kcal for women). Finally, the total number of participants and observations were 15,929 and 64,016, respectively.
The CHNS was approved by the institutional review committees of the University of North Carolina at Chapel Hill and National Institute for Nutrition and Health, Chinese Center for Disease Control and Prevention. Participants provided their written, informed consent in the survey.
Dietary measurements
We collected diet data using weighing methods in combination with three consecutive 24 h dietary recalls (2 weekdays and 1 weekend day) in each wave of the CHNS. All condiments in the home inventory were carefully measured and recorded by trained interviewers. Standard forms was used to administer the 24 h dietary recalls in a face to face interview. The participants were asked to report the kinds and amount of the food and beverage items that they consume both at home and away from home during the previous 24 h. The average intake of the three recalls was used for each individual.
Blood pressure measurement
BP was measured by experienced physicians using standard mercury sphygmomanometers with regular adult cuffs. Participants were told to sit in comfortable position for about 5 min before measurement. Three measurements were obtained with a 30 s interval. BP was calculated from the average of the last 2 of the 3 measurements. We defined hypertension as having a mean systolic blood pressure (SBP) ≥ 140 mm Hg or a mean diastolic blood pressure (DBP) ≥ 90 mm Hg, currently undergoing treatment with antihypertensive medication, or previously diagnosed by a physician.
Other relevant variables
Each round of the CHNS has obtained identical questionnaires and anthropometric data with some adjustment from household members. We used a general questionnaire to collect individual and household information by face to face, including participant’s age, education, living area, smoking status, alcohol consumption, physical activity, annual household income per family member and so on. Well-trained health workers who followed a reference protocol recommended by the WHO took height, weight and other anthropometric measurements.
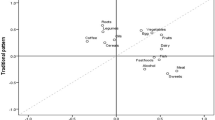
Statistical analysis
We derived dietary patterns using datasets of each year combined for 18 foods or food groups (Table S1) expressed as mean intake (g/d) according to the Chinese Food Composition Table. Factors were rotated by the varimax method to achieve a more simplistic structure with greater interpretability. Which set of factors to meaningfully describe distinct food patterns was based on the eigenvalues (> 1), the scree plots, and the interpretability of the factors. Factor loadings were calculated for each food group across the factors. A factor score was calculated for each subject for each of the factors, in which intakes of 18 food groups were weighted by their factor loadings and summed.
We categorized participants into quartiles across the score of each dietary pattern. We used chi-square tests (categorical variables) and analysis of variance (continuous variables) to compare the characteristics of participants across quartiles of dietary pattern score. We constructed three-level mixed-effect linear regression models (xtmixed in STATA) to estimate SBP and DBP in relation to quartiles of dietary pattern score and performed three-level mixed-effect logistic regression models (gllamm in STATA) to assess the risk of hypertension. We calculated regression coefficients (95% CIs) and odds ratios (ORs) (95% CIs), respectively.
All statistical tests were two-tailed, and we regarded differences as significant at P < 0.05. For all analyses, we used SAS (Version 9.4, SAS Institute Inc., Cary, NC, United States) and Stata/SE (STATA, Version 15, StataCorp, College Station, TX, United States).
Results
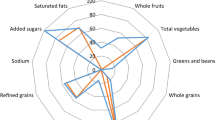
Dietary patterns
Factor analysis revealed three dietary patterns in Table 1. Factor 1 was characterized by the food items rice, vegetables, pork, was named the southern pattern because it represents a typical traditional diet in South China. Factor 2, had high loadings for fruits, dairy products, cakes, cookies, and pastries, was called the modern pattern. Factor 3, characterized by high intakes of poultry, organ meats and other livestock meat, was thus called the meat pattern.
The characteristics of the participants
The characteristics of the participants in 1991 by quartiles of dietary pattern score are given in Table 2. We observed significant differences in age, education level, living areas, energy intake, sodium intake, physical activity and individual income among quartiles of dietary pattern score. For the southern dietary pattern, participants in the top quartile had the youngest age, the highest energy intake, the lowest body mass index (BMI), and had the lowest proportion of females, high education level, and urban residents and the highest proportion of current smokers, current alcohol drinkers, and high physical activity. For the modern dietary pattern, participants in the top quartile had the highest energy intake, highest BMI, highest SBP and DBP, and had the highest proportion of high education level, urban residents, current smokers, current alcohol drinkers and high individual income, and had the lowest proportion of high physical activity. For the meat dietary pattern, participants in the top quartile tended to be the oldest, and had the highest proportion of high education level, urban residents and high individual income, and had the lowest proportion of high physical activity.
Dietary Patterns and BP/ Hypertension
Table 3 shows the longitudinal association of dietary patterns with SBP and DBP. Participants in the top quartile of the modern pattern had a decrease in SBP (β = −0.51; 95% CI −0.86, −0.16; P < 0.01) when adjusted for all potential confounders. The meat pattern was significantly associated with higher DBP (β = 0.31; 95% CI 0.08, 0.53; P < 0.01) when adjusted for all potential confounders.
Table 4 shows overall association between the dietary patterns and the risk of hypertension. After adjusting for all potential confounders, participants in the highest quartile of the meat pattern were more likely to have hypertension (OR = 1.14; 95% CI 1.03–1.24; P < 0.01). We observed no significant association between the traditional southern pattern and modern pattern and risk of hypertension.
Discussion
In this large-scale, 28-year follow-up study, we found that meat pattern was positively associated with DBP and the risk of hypertension among Chinese adults independent of potential confounding factors. Furthermore, participants with higher adherence to the modern pattern had significantly lower SBP. There was no significant association between the southern pattern and BP and hypertension. To the best of our knowledge, this is the longest cohort study to examine the longitudinal association between dietary patterns and BP as well as the risk of hypertension.
Over the last two decades, the meat pattern has become more prevalent in China [19]. The meat pattern also called animal pattern has been considered to be an unhealthy dietary pattern, which is most common and characterized by a high intake of red and processed meat in western countries [30]. The meat pattern in our study was a blend of healthy (poultry, fish and seafood) and unhealthy (red meat) constituents of dietary patterns. However, our findings were consistent with previous studies, which reported a significantly positive association between meat consumption and the risk of hypertension [31,32,33]. Moreover, we found meat pattern was positively associated with DBP, which was in agreement with previously reported findings of similar dietary patterns [34, 35]. This relationship was perhaps due to the fact that the fatty pork was the main component of meat intake among Chinese population [36]. There are several potential mechanisms through which the intake of meat could had adverse impact on blood pressure: the joint effect of multiple dietary components, such as saturated fat and cholesterol [32]; Millard reaction products in cooked meat through its inflammatory and oxidation pathways [31]; high concentrations of nitrite additives for food preservation in processed meat [33].
Our findings showed a negative association between the modern dietary pattern and SBP. Similar to our results, a cohort study of middle-aged and elderly men in Shanghai suggested that the ‘fruit and milk’ pattern was significantly associated with both lower SBP and DBP [34]. Besides, a community–based survey in Eastern China found that the fruit-dairy pattern was inversely associated with the risk of hypertension among the study participants [27]. The modern pattern in our study had high loadings for fruits, dairy products, eggs and nuts, all of which have been reported to have beneficial effects on BP [31]. This pattern also had high loadings for cakes, cookies and pastries, the deleterious effect of which may be counteracted by the protective effect of other food groups. However, synergistic effects of dietary patterns on BP are still unclear exactly.
The southern pattern that was the predominant dietary pattern in China, did not significantly affect BP and the risk of hypertension. This null association observed in our study was consistent with a previous report in a city of Eastern China [27]. Similarly, a traditional pattern with high loading of cereals and vegetables was not related to the risk of hypertension among Korean women aged 30–79 years [37]. Lack of association may be due to the interactions among different food groups. High intake of refined cereal and pork may exert opposite unfavorable effects on BP in spite of the high level of vegetable consumption. Our previous study found that the southern pattern was inversely associated with risk of overweight/obesity [38], which was considered as important risk for hypertension [20]. Thus, the southern pattern may have an indirectly beneficial role in the prevention of hypertension.
Asian perspectives
Some studies in Asia indicated that the healthy dietary patterns are associated with a decreased odds of hypertension [13]. However, further prospective studies are needed to better understand the influence of westernization of dietary patterns on BP among Asian populations.
There were some limitations in our study. First, the study subjects may not be representative of the whole Chinese population. Second, factor analysis involves a series of subjective decisions which may affect interpretation and it is difficult to compare results across studies because of differences in the dietary assessment methods, the number and type of food groupings. Third, the 24 h dietary recall method cannot reliably reflect usual dietary intake. However, the current study includes a relatively large sample size across a wide age range during a long time, and provides useful information to substantially support previous studies by examining the longitudinal relationship of dietary patterns with BP and the risk of hypertension.
In conclusion, adherence to the modern pattern characterized by high intake of fruits and dairy products was inversely associated with DBP, whereas the meat pattern was positively associated with SBP and the risk of hypertension. These findings may well have important implications for public health practice, not only for demonstrating the important roles of some specific food groups on BP and hypertension, but also for adding the evidence for the development of practical food-based dietary guidelines for different populations.
References
Liyuan MAZW, Jing FAN, Shengshou HU. An Essential introduction to the annual report on cardiovascular health and diseases in China (2021). Chin Gen Pract. 2022;25:3331–46.
Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension 2020;75:285–92.
Rehman S, Rehman E, Mumtaz A, Jianglin Z. Cardiovascular disease mortality and potential risk factor in China: A multi-dimensional assessment by a grey relational approach. Int J Public Health. 2022;67:1604599.
Li S, Liu Z, Joseph P, Hu B, Yin L, Tse LA, et al. Modifiable risk factors associated with cardiovascular disease and mortality in China: A PURE substudy. Eur Heart J. 2022;43:2852–63.
Yin R, Yin L, Li L, Silva-Nash J, Tan J, Pan Z, et al. Hypertension in China: burdens, guidelines and policy responses: a state-of-the-art review. J Hum Hypertens. 2022;36:126–34.
Zhang M, Wu J, Zhang X, Hu CH, Zhao ZP, Li C, et al. [Prevalence and control of hypertension in adults in China, 2018]. Zhonghua Liu Xing Bing Xue Za Zhi. 2021;42:1780–9.
Xu TZ M, Liu J, Wang L, Dong W. Death burden attributable to hypertension in 1990 and 2019 in China. Chin J Prev Contr Chron Dis. 2022;30:327–31.
Caligiuri SPB, Pierce GN. A review of the relative efficacy of dietary, nutritional supplements, lifestyle, and drug therapies in the management of hypertension. Crit Rev Food Sci Nutr. 2017;57:3508–27.
Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM, et al. Dietary approaches to prevent and treat hypertension: a scientific statement from the American Heart Association. Hypertension 2006;47:296–308.
Hu FB. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr Opin Lipido. 2002;13:3–9.
Sukhato K, Akksilp K, Dellow A, Vathesatogkit P, Anothaisintawee T. Efficacy of different dietary patterns on lowering of blood pressure level: An umbrella review. Am J Clin Nutr. 2020;112:1584–98.
Ndanuko RN, Tapsell LC, Charlton KE, Neale EP, Batterham MJ. Dietary patterns and blood pressure in adults: A systematic review and meta-analysis of randomized controlled trials. Adv Nutr. 2016;7:76–89.
Wang CJ, Shen YX, Liu Y. Empirically derived dietary patterns and hypertension likelihood: A meta-analysis. Kidney Blood Press Res. 2016;41:570–81.
Filippou CD, Thomopoulos CG, Kouremeti MM, Sotiropoulou LI, Nihoyannopoulos PI, Tousoulis DM, et al. Mediterranean diet and blood pressure reduction in adults with and without hypertension: A systematic review and meta-analysis of randomized controlled trials. Clin Nutr. 2021;40:3191–200.
Cowell OR, Mistry N, Deighton K, Matu J, Griffiths A, Minihane AM, et al. Effects of a Mediterranean diet on blood pressure: A systematic review and meta-analysis of randomized controlled trials and observational studies. J Hypertens. 2021;39:729–39.
Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N. Engl J Med. 1997;336:1117–24.
Harsha DW, Lin PH, Obarzanek E, Karanja NM, Moore TJ, Caballero B. Dietary Approaches to Stop Hypertension: A summary of study results. DASH Collaborative Research Group. J Am Diet Assoc. 1999;99:S35–39.
Filippou CD, Tsioufis CP, Thomopoulos CG, Mihas CC, Dimitriadis KS, Sotiropoulou LI, et al. Dietary Approaches to Stop Hypertension (DASH) Diet and Blood Pressure Reduction in Adults with and without Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Adv Nutr. 2020;11:1150–60.
Zhang J, Wang Z, Du W, Huang F, Jiang H, Bai J, et al. Twenty-Five-Year Trends in Dietary Patterns among Chinese Adults from 1991 to 2015. Nutrients. 2021;13:1327.
Shi Z, Sun X, Yan AF, Wang Y. Growing Burden of Hypertension in China: Causes, Challenges, and Opportunities. China CDC Wkly. 2020;2:776–9.
Zhao J, Guo W, Wang J, Wang T. Exploring the Association of dietary patterns with the risk of hypertension using principal balances analysis and principal component analysis. Public Health Nutr. 2023;26:160–70.
Zhang Y, Wang Y, Chen Y, Zhou J, Xu L, Xu K, et al. Associations of dietary patterns and risk of hypertension in southwest China: A prospective cohort study. Int J Environ Res Public Health. 2021;18.
Ye J, Lv Y, Li Z, Yao Y, Jin L. Associations of dietary patterns with hypertension among adults in Jilin Province, China: A structural equation modelling approach. Public Health Nutr. 2019;22:1048–55.
Ruan Y, Huang Y, Zhang Q, Qin S, Du X, Sun Y. Association between dietary patterns and hypertension among Han and multi-ethnic population in southwest China. BMC Public Health. 2018;18:1106.
Zheng PF, Shu L, Zhang XY, Si CJ, Yu XL, Gao W, et al. Association between Dietary Patterns and the Risk of Hypertension among Chinese: A Cross-Sectional Study. Nutrients 2016;8:239.
Wang D, He Y, Li Y, Luan D, Yang X, Zhai F, et al. Dietary patterns and hypertension among Chinese adults: a nationally representative cross-sectional study. BMC Public Health. 2011;11:925.
Wang C, Zheng Y, Zhang Y, Liu D, Guo L, Wang B, et al. Dietary Patterns in Association With Hypertension: A Community-Based Study in Eastern China. Front Nutr. 2022;9:926390.
Popkin BM, Du S, Zhai F, Zhang B. Cohort Profile: The China Health and Nutrition Survey–monitoring and understanding socio-economic and health change in China, 1989-2011. Int J Epidemiol. 2010;39:1435–40.
Zhang B, Zhai FY, Du SF, Popkin BM. The China Health and Nutrition Survey, 1989-2011. Obes Rev. 2014;15:2–7.
Jayedi A, Soltani S, Abdolshahi A, Shab-Bidar S. Healthy and unhealthy dietary patterns and the risk of chronic disease: an umbrella review of meta-analyses of prospective cohort studies. Br J Nutr. 2020;124:1133–44.
Schwingshackl L, Schwedhelm C, Hoffmann G, Knuppel S, Iqbal K, Andriolo V, et al. Food Groups and Risk of Hypertension: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Adv Nutr. 2017;8:793–803.
Zhang Y, Zhang DZ. Red meat, poultry, and egg consumption with the risk of hypertension: a meta-analysis of prospective cohort studies. J Hum Hypertens. 2018;32:507–17.
Allen TS, Bhatia HS, Wood AC, Momin SR, Allison MA. State-of-the-Art Review: Evidence on Red Meat Consumption and Hypertension Outcomes. Am J Hypertens. 2022;35:679–87.
Lee SA, Cai H, Yang G, Xu WH, Zheng W, Li H, et al. Dietary patterns and blood pressure among middle-aged and elderly Chinese men in Shanghai. Br J Nutr. 2010;104:265–75.
Shridhar K, Satija A, Dhillon PK, Agrawal S, Gupta R, Bowen L, et al. Association between empirically derived dietary patterns with blood lipids, fasting blood glucose and blood pressure in adults - the India migration study. Nutr J. 2018;17:15.
He Y, Yang X, Xia J, Zhao L, Yang Y. Consumption of meat and dairy products in China: a review. Proc Nutr Soc. 2016;75:385–91.
Cho YA, Kim J, Cho ER, Shin A. Dietary patterns and the prevalence of metabolic syndrome in Korean women. Nutr Metab Cardiovasc Dis. 2011;21:893–900.
Zhang J, Wang H, Wang Z, Huang F, Zhang X, Du W, et al. Trajectories of Dietary Patterns and Their Associations with Overweight/Obesity among Chinese Adults: China Health and Nutrition Survey 1991–2018. Nutrients. 2021;13:2835.
Acknowledgements
The authors are grateful to the participants for their involvement in the survey. The authors also thank the team at National Institute for Nutrition and Health, Chinese Center for Disease Control and Prevention, and Carolina Population Center, University of North Carolina at Chapel Hill.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, J., Du, W., Huang, F. et al. Longitudinal study of dietary patterns and hypertension in adults: China Health and Nutrition Survey 1991–2018. Hypertens Res 46, 2264–2271 (2023). https://doi.org/10.1038/s41440-023-01322-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01322-x
Keywords
This article is cited by
-
How do we tackle nighttime blood pressure?
Hypertension Research (2023)