Abstract
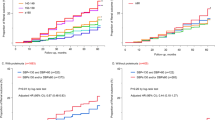
Predicting and preventing new-onset chronic kidney disease (CKD) through blood pressure (BP) measurements is worthwhile. This study assessed the risk of CKD, which was defined as proteinuria and/or an estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2, according to cross-classification by systolic and diastolic BP (SBP and DBP). This retrospective population-based cohort study analyzed data from 1,492,291 participants without CKD and without antihypertensive treatment in the JMDC database, which contains the annual health check-up data of Japanese aged <75 years. During a mean follow-up of 3.2 years, CKD incidence, proteinuria, and eGFR <60 mL/min/1.73 m2 occurred in 92,587, 67,021, and 28,858 participants, respectively. When the SBP/DBP <120/<80 mmHg group was set as a reference, both high SBP and DBP were significantly associated with an elevated CKD risk. DBP tended to be more strongly associated with CKD risk than SBP; the hazard ratio of CKD was 1.44–1.80 in the group with SBP/DBP of 130–139/≥90 mmHg and 1.23–1.47 in the group with SBP/DBP of ≥140/80–89 mmHg. A similar result was observed for developing proteinuria and eGFR <60 mL/min/1.73 m2. SBP/DBP ≥150/<80 mmHg was strongly associated with an elevated CKD risk due to the increased risk of eGFR decline. High BP, especially isolated high DBP levels, is a significant risk factor for CKD among individuals around middle age without kidney disease. Moreover, attention should be paid to kidney function, particularly eGFR decline, in the case of low DBP with extremely high SBP levels.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
All data and study materials will not be made available to other researchers in compliance with our contract with JMDC Inc.
References
Xie Y, Bowe B, Mokdad AH, Xian H, Yan Y, Li T, et al. Analysis of the Global Burden of Disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int. 2018;94:567–81.
Tohidi M, Hasheminia M, Mohebi R, Khalili D, Hosseinpanah F, Yazdani B, et al. Incidence of chronic kidney disease and its risk factors, results of over 10 year follow up in an Iranian cohort. PLoS ONE. 2012;7:e45304.
Lv JC, Zhang LX. Prevalence and Disease Burden of Chronic Kidney Disease. Adv Exp Med Biol. 2019;1165:3–15.
Satoh M, Hirose T, Nakayama S, Murakami T, Takabatake K, Asayama K, et al. Blood Pressure and Chronic Kidney Disease Stratified by Gender and the Use of Antihypertensive Drugs. J Am Heart Assoc. 2020;9:e015592.
Nitta K, Goto S, Masakane I, Hanafusa N, Taniguchi M, Hasegawa T, et al. Annual dialysis data report for 2018, JSDT Renal Data Registry: survey methods, facility data, incidence, prevalence, and mortality. Renal Replacement Ther. 2020;6:41.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269–324.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36:1953–2041.
Flint AC, Conell C, Ren X, Banki NM, Chan SL, Rao VA, et al. Effect of Systolic and Diastolic Blood Pressure on Cardiovascular Outcomes. N Engl J Med. 2019;381:243–51.
Bakris G, Ali W, Parati G. ACC/AHA Versus ESC/ESH on Hypertension Guidelines: JACC Guideline Comparison. J Am Coll Cardiol. 2019;73:3018–26.
Kanno A, Kikuya M, Ohkubo T, Hashimoto T, Satoh M, Hirose T, et al. Pre-hypertension as a significant predictor of chronic kidney disease in a general population: the Ohasama Study. Nephrol Dial Transplant. 2012;27:3218–23.
Schaeffner ES, Kurth T, Bowman TS, Gelber RP, Gaziano JM. Blood pressure measures and risk of chronic kidney disease in men. Nephrol Dial Transplant. 2008;23:1246–51.
Haroun MK, Jaar BG, Hoffman SC, Comstock GW, Klag MJ, Coresh J. Risk factors for chronic kidney disease: a prospective study of 23,534 men and women in Washington County, Maryland. J Am Soc Nephrol. 2003;14:2934–41.
Fox CS, Larson MG, Leip EP, Culleton B, Wilson PW, Levy D. Predictors of new-onset kidney disease in a community-based population. JAMA. 2004;291:844–50.
Yamagata K, Ishida K, Sairenchi T, Takahashi H, Ohba S, Shiigai T, et al. Risk factors for chronic kidney disease in a community-based population: a 10-year follow-up study. Kidney Int. 2007;71:159–66.
Yano Y, Fujimoto S, Sato Y, Konta T, Iseki K, Iseki C, et al. New-onset hypertension and risk for chronic kidney disease in the Japanese general population. J Hypertens. 2014;32:2371–7.
Obermayr RP, Temml C, Knechtelsdorfer M, Gutjahr G, Kletzmayr J, Heiss S, et al. Predictors of new-onset decline in kidney function in a general middle-european population. Nephrol Dial Transplant. 2008;23:1265–73.
Wan EYF, Yu EYT, Chin WY, Fong DYT, Choi EPH, Lam CLK. Association of Blood Pressure and Risk of Cardiovascular and Chronic Kidney Disease in Hong Kong Hypertensive Patients. Hypertension. 2019;74:331–40.
Yano Y, Fujimoto S, Sato Y, Konta T, Iseki K, Moriyama T, et al. Association between prehypertension and chronic kidney disease in the Japanese general population. Kidney Int. 2012;81:293–9.
Bae EH, Lim SY, Jung JH, Oh TR, Choi HS, Kim CS, et al. Chronic Kidney Disease Risk of Isolated Systolic or Diastolic Hypertension in Young Adults: A Nationwide Sample Based-Cohort Study. J Am Heart Assoc. 2021;10:e019764.
Yamada-Harada M, Fujihara K, Osawa T, Yamamoto M, Kaneko M, Kitazawa M, et al. Relationship Between Number of Multiple Risk Factors and Coronary Artery Disease Risk With and Without Diabetes Mellitus. J Clin Endocrinol Metab. 2019;104:5084–90.
Takeuchi M, Kawakami K. Association between Hemoglobin and Hemoglobin A1c: A Data-Driven Analysis of Health Checkup Data in Japan. J Clin Med. 2018;7:539.
Fukushima A, Khabtheni W, Guelfucci F, Onishi Y, Sugiyama D, Okamura T, et al. Impact of Hypertension on Hospitalizations for Cardiovascular Diseases in a Worksite Population: An Epidemiologic Study Using Claims Data for Workers. Am J Hypertens. 2019;32:298–307.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Nakayama S, Satoh M, Tatsumi Y, Murakami T, Muroya T, Hirose T, et al. Detailed association between serum uric acid levels and the incidence of chronic kidney disease stratified by sex in middle-aged adults. Atherosclerosis. 2021;330:107–13.
Nakayama S, Satoh M, Metoki H, Murakami T, Asayama K, Hara A, et al. Lifetime risk of stroke stratified by chronic kidney disease and hypertension in the general Asian population: the Ohasama study. Hypertens Res. 2021;44:866–73.
Terata S, Kikuya M, Satoh M, Ohkubo T, Hashimoto T, Hara A, et al. Plasma renin activity and the aldosterone-to-renin ratio are associated with the development of chronic kidney disease: the Ohasama Study. J Hypertens. 2012;30:1632–8.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Klag MJ, Whelton PK, Randall BL, Neaton JD, Brancati FL, Ford CE, et al. Blood pressure and end-stage renal disease in men. N Engl J Med. 1996;334:13–8.
Lee H, Yano Y, Cho SMJ, Park JH, Park S, Lloyd-Jones DM, et al. Cardiovascular Risk of Isolated Systolic or Diastolic Hypertension in Young Adults. Circulation. 2020;141:1778–86.
Arima H, Murakami Y, Lam TH, Kim HC, Ueshima H, Woo J, et al. Effects of prehypertension and hypertension subtype on cardiovascular disease in the Asia-Pacific Region. Hypertension. 2012;59:1118–23.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269–324.
Nakayama S, Satoh M, Metoki H, Murakami T, Asayama K, Hara A, et al. Lifetime risk of stroke stratified by chronic kidney disease and hypertension in the general Asian population: the Ohasama study. Hypertens Res. 2021;44:866–73.
Nakayama M, Metoki H, Terawaki H, Ohkubo T, Kikuya M, Sato T, et al. Kidney dysfunction as a risk factor for first symptomatic stroke events in a general Japanese population-the Ohasama study. Nephrol Dial Transplant. 2007;22:1910–5.
Zambon S, Maggi S, Zanoni S, Romanato G, Noale M, Corti MC, et al. Association of single measurement of estimated glomerular filtration rate and non-quantitative dipstick proteinuria with all-cause and cardiovascular mortality in the elderly. Results from the Progetto Veneto Anziani (Pro.V.A.) Study. Atherosclerosis. 2012;220:201–7.
Kanno A, Kikuya M, Asayama K, Satoh M, Inoue R, Hosaka M, et al. Night-time blood pressure is associated with the development of chronic kidney disease in a general population: the Ohasama Study. J Hypertens. 2013;31:2410–7.
Acknowledgements
The authors are grateful to all the staff at JMDC Inc. who advised us on the structure of the JMDC data used in the present study.
Funding
This study was supported by Grants for Scientific Research (17K15853 and 21K10478) from the Ministry of Education, Culture, Sports, Science, and Technology, Japan; research support from Bayer Yakuhin Co., Ltd.; the Health Care Science Institute Research Grant; a grant from the Foundation for Total Health Promotion; and the Medical Research Encouragement Prize from the Japan Medical Association.
Author information
Authors and Affiliations
Contributions
Research idea and study design TS, MS, TMurakami, TH, SN, TMori, TOhkubo, YI, and HM. Data acquisition MS, TObara, TOhkubo, YI, and HM. Data analysis/interpretation TS, MS, TMurakami, TH, TObara, SN, HH, MT, TMuroya, AK, TMori, TOhkubo, YI, and HM. Statistical analysis TS and MS. Supervision or mentorship MS, TMurakami, SN, and HM. Each author contributed important intellectual content during paper drafting or revision and agrees to be personally accountable for the individual’s contributions and to ensure that questions pertaining to the accuracy or integrity of any portion of the work, even one in which the author was not directly involved, are appropriately investigated and resolved, including with documentation in the literature, if appropriate.
Corresponding author
Ethics declarations
Conflict of interest
The Division of Public Health, Hygiene, and Epidemiology, Faculty of Medicine, and Tohoku Medical and Pharmaceutical University have received scholarship donations or research support from Pfizer Japan Inc.; Daiichi Sankyo Co., Ltd.; Astellas Pharma Inc.; Takeda Pharmaceutical Co., Ltd.; and Bayer Yakuhin Co., Ltd. in the past three years. T. Ohkubo, Y. Imai, and H. Metoki concurrently held the position of director at the Tohoku Institute for Management of Blood Pressure, which was supported by Omron Healthcare Co., Ltd.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Suenaga, T., Satoh, M., Murakami, T. et al. Cross-classification by systolic and diastolic blood pressure levels and chronic kidney disease, proteinuria, or kidney function decline. Hypertens Res 46, 1860–1869 (2023). https://doi.org/10.1038/s41440-023-01267-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01267-1
Keywords
This article is cited by
-
Triglyceride-glucose index predicts future chronic kidney disease development in all populations, including normotensive and isolated diastolic hypertension
Hypertension Research (2024)
-
Detailed cross-sectional association between traditional risk factors and high systolic blood pressure in a Japanese population
Hypertension Research (2024)
-
Don’t miss the isolated diastolic hypertension
Hypertension Research (2023)
-
Determinants and clinical implication of hypertension from childhood to old age in Asian subjects
Hypertension Research (2023)