Abstract
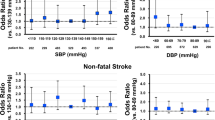
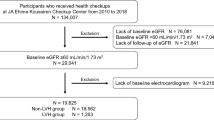
A higher resting heart rate (RHR) is associated with an increased risk of cardiovascular events in patients with type 2 diabetes mellitus (T2DM) and cardiovascular diseases. The aim of this study was to investigate the association between RHR and cardiovascular events in T2DM patients with diabetic retinopathy and without known cardiovascular disease. We analyzed the association between RHR and cardiovascular events, including coronary, cerebral, renal and vascular events or cardiovascular death in T2DM patients with retinopathy and hyperlipidemia without prior cardiovascular events who were enrolled in the EMPATHY study. Data from 4746 patients were analyzed. The median RHR was 76 bpm. Patients were divided into four groups based on their baseline RHR ( < 60, 60–69, 70–79, and ≥80 bpm). Patients with a higher RHR were more likely to be younger and had a higher body mass index, blood pressure value, HbA1c value, and estimated glomerular filtration rate and a lower B-type natriuretic peptide value; they also had a higher proportion of current smoking status, neuropathy, and nephropathy. After adjusting for confounders, including the aforementioned risk factors, a RHR of 70–79 bpm and a RHR ≥ 80 bpm were significantly associated with cardiovascular events (hazard ratio 1.50, 95% CI 1.03–2.20; and hazard ratio 1.62, 95% CI 1.11–2.36; respectively) compared to a RHR of 60–69 bpm. The analysis using restricted cubic splines indicated that the cardiovascular risk seemed to be similarly high when the RHR range was ≥70 bpm. In conclusion, in T2DM patients with diabetic retinopathy and without known cardiovascular disease, a high RHR, particularly ≥70 bpm, was associated with the risk of cardiovascular events compared to a RHR of 60–69 bpm.

High resting heart rate (RHR), particularly ≥70 bpm, was associated with the risk of cardiovascular events compared to RHR 60-69 bpm in patients with type 2 diabetes mellitus (T2DM), diabetic retinopathy, and hyperlipidemia, but without known cardiovascular disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Diaz A, Bourassa MG, Guertin MC, Tardif JC. Long-term prognostic value of resting heart rate in patients with suspected or proven coronary artery disease. Eur Heart J. 2005;26:967–74.
Kotecha D, Flather MD, Altman DG, Holmes J, Rosano G, Wikstrand J, et al. Heart rate and rhythm and the benefit of beta-blockers in patients with heart failure. J Am Coll Cardiol. 2017;69:2885–96.
Fox K, Borer JS, Camm AJ, Danchin N, Ferrari R, Lopez Sendon JL, et al. Resting heart rate in cardiovascular disease. J Am Coll Cardiol. 2007;50:823–30.
Courand P-Y, Lantelme P. Significance, prognostic value and management of heart rate in hypertension. Arch Cardiovasc Dis. 2014;107:48–57.
Alhalabi L, Singleton MJ, Oseni AO, Shah AJ, Zhang ZM, Soliman EZ. Relation of higher resting heart rate to risk of cardiovascular versus noncardiovascular death. Am J Cardiol. 2017;119:1003–7.
Aune D, Hartaigh O, Vatten LJ. Resting heart rate and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Nutr Metab Cardiovasc Dis. 2015;25:526–34.
Vinik AI, Ziegler D. Diabetic cardiovascular autonomic neuropathy. Circulation. 2007;115:387–97.
Iyngkaran P, Anavekar N, Majoni W, Thomas MC. The role and management of sympathetic overactivity in cardiovascular and renal complications of diabetes. Diabetes Metab. 2013;39:290–8.
Kuehl M, Stevens MJ. Cardiovascular autonomic neuropathies as complications of diabetes mellitus. Nat Rev Endocrinol. 2012;8:405–16.
Böhm M, Schumacher H, Teo KK, Lonn EM, Mahfoud F, Ukena C, et al. Resting heart rate and cardiovascular outcomes in diabetic and non-diabetic individuals at high cardiovascular risk analysis from the ONTARGET/TRANSCEND trials. Eur Heart J. 2020;41:231–8.
Hillis GS, Woodward M, Rodgers A, Chow CK, Li Q, Zoungas S, et al. Resting heart rate and the risk of death and cardiovascular complications in patients with type 2 diabetes mellitus. Diabetologia. 2012;55:1283–90.
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2016;37:2315–81.
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41:255–323.
Imai Y, Hirata T, Saitoh S, Ninomiya T, Miyamoto Y, Ohnishi H, et al. Impact of hypertension stratified by diabetes on the lifetime risk of cardiovascular disease mortality in Japan: a pooled analysis of data from the evidence for cardiovascular prevention from observational cohorts in Japan study. Hypertens Res. 2020;43:1437–44.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2019;74:e177–e232.
Itoh H, Komuro I, Takeuchi M, Akasaka T, Daida H, Egashira Y, et al. Intensive treat-to-target statin therapy in high-risk Japanese patients with hypercholesterolemia and diabetic retinopathy: Report of a randomized study. Diabetes Care. 2018;41:1275–84.
Ueshima K, Itoh H, Kanazawa N, Komuro I, Nagai R, Takeuchi M, et al. Rationale and design of the standard versus intensive statin therapy for hypercholesterolemic patients with diabetic retinopathy (EMPATHY) study: A randomized controlled trial. J Atheroscler Thromb. 2016;23:976–90.
Harrell FE. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis. Springer Series in Statistics. Springer, New York, NY. https://doi.org/10.1007/978-1-4757-3462-1_5.
Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR, et al. 2018 ACC/AHA/HRS Guideline on the evaluation and management of patients with bradycardia and cardiac conduction delay: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Rhythm Society. Circulation. 2019;140:e382–e482.
Kossmann CE. The normal electrocardiogram. Circulation. 1953;8:920–36.
Palatini P. Heart rate and the cardiometabolic risk. Curr Hypertens Rep. 2013;15:253–9.
Ikeda S, Shinohara K, Enzan N, Matsushima S, Tohyama T, Funakoshi K, et al. Serial measurement of B-type natriuretic peptide and future cardiovascular events in patients with type 2 diabetes mellitus without known cardiovascular disease. Int J Cardiol. 2022;356:98–104.
White DW, Raven PB. Autonomic neural control of heart rate during dynamic exercise: Revisited. J Physiol. 2014;592:2491–2500.
Vinik AI, Maser RE, Mitchell BD, Freeman R. Diabetic autonomic neuropathy. Diabetes Care. 2003;26:1553–79.
Palatini P, Julius S. The physiological determinants and risk correlations of elevated heart rate. Am J Hypertens. 1999;12:3S–8S.
Grassi G, Arenare F, Quarti-Trevano F, Seravalle G, Mancia G. Heart rate, sympathetic cardiovascular influences, and the metabolic syndrome. Prog Cardiovasc Dis. 2009;52:31–37.
Giannoglou GD, Chatzizisis YS, Zamboulis C, Parcharidis GE, Mikhailidis DP, Louridas GE. Elevated heart rate and atherosclerosis: An overview of the pathogenetic mechanisms. Int J Cardiol. 2008;126:302–12.
Liao D, Carnethon M, Evans GW, Cascio WE, Heiss G. Lower heart rate variability is associated with the development of coronary heart disease in individuals. Diabetes. 2002;51:3524–31.
Ko SH, Song KH, Park SA, Kim SR, Cha BY, Son HY, et al. Cardiovascular autonomic dysfunction predicts acute ischaemic stroke in patients with type 2 diabetes mellitus: A 7-year follow-up study. Diabet Med. 2008;25:1171–7.
Dimitropoulos G, Tahrani AA, Stevens MJ. Cardiac autonomic neuropathy in patients with diabetes mellitus. World J Diabetes. 2014;5:17–39.
Ko SH, Park SA, Cho JH, Song KH, Yoon KH, Cha BY, et al. Progression of cardiovascular autonomic dysfunction in patients with type 2 diabetes. A 7-year follow-up study. Diabetes Care. 2008;31:1832–6.
Falk E, Shah PK, Fuster V. Coronary plaque disruption. Circulation. 1995;92:657–71.
Beere PA, Glagov S, Zarins CK. Experimental atherosclerosis at the carotid bifurcation of the cynomolgus monkey. Localization, compensatory enlargement, and the sparing effect of lowered heart rate. Arterioscler Thromb. 1992;12:1245–53.
Beere PA, Glagov S, Zarins CK. Retarding effect of lowered heart rate on coronary atherosclerosis. Science. 1984;226:180–2.
Custodis F, Baumhäkel M, Schlimmer N, List F, Gensch C, Böhm M, et al. Heart rate reduction by ivabradine reduces oxidative stress, improves endothelial function, and prevents atherosclerosis in apolipoprotein E-deficient mice. Circulation. 2008;117:2377–87.
Custodis F, Fries P, Mller A, Stamm C, Grube M, Kroemer HK, et al. Heart rate reduction by ivabradine improves aortic compliance in apolipoprotein E-deficient mice. J Vasc Res. 2012;49:432–40.
Hohneck AL, Fries P, Ströder J, Schneider G, Wagenpfeil S, Schirmer SH, et al. Effects of heart rate reductionwith ivabradine on vascular stiffness and endothelial function in chronic stable coronary artery disease. J Hypertens. 2019;37:1023–31.
Miot A, Ragot S, Hammi W, Saulnier P-J, Sosner P, Piguel X, et al. Prognostic value of resting heart rate on cardiovascular and renal outcomes in type 2 diabetic patients: A competing risk analysis in a prospective cohort. Diabetes Care. 2012;35:2069–75.
Tsujimoto T, Sugiyama T, Shapiro MF, Noda M, Kajio H. Risk of cardiovascular events in patients with diabetes mellitus on β-blockers. Hypertension. 2017;70:103–10.
Fortuin-de Smidt MC, Sewe MO, Lassale C, Weiderpass E, Andersson J, Huerta JM, et al. Physical activity attenuates but does not eliminate coronary heart disease risk amongst adults with risk factors: EPIC-CVD case-cohort study. Eur J Prev Cardiol. 2022;29:1618–29.
Francois ME, Pistawka KJ, Halperin FA, Little JP. Cardiovascular benefits of combined interval training and post-exercise nutrition in type 2 diabetes. J Diabetes Complications. 2018;32:226–33.
Sardeli AV, Griffth GJ, dos Santos MVMA, Ito MSR, Chacon-Mikahil MPT. The effects of exercise training on hypertensive older adults: an umbrella meta-analysis. Hypertens Res. 2021;44:1434–43.
Sakamoto S. Prescription of exercise training for hypertensives. Hypertens Res. 2020;43:155–61.
Bathula R, Francis DP, Hughes A, Chaturvedi N. Ethnic differences in heart rate: can these be explained by conventional cardiovascular risk factors? Clin Auton Res. 2008;18:90–95.
Farrell MC, Giza RJ, Shibao CA. Race and sex differences in cardiovascular autonomic regulation. Clin Auton Res. 2020;30:371–9.
Sloan RP, Huang MH, McCreath H, Sidney S, Liu K, Williams OD, et al. Cardiac autonomic control and the effects of age, race, and sex: The CARDIA study. Auton Neurosci. 2008;139:78–85.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
KS reports grants from Daiichi Sankyo, Nippon Boehringer Ingelheim, and Otsuka Medical Devices. HI reports personal fees from SBI Pharmaceuticals, Wakunaga Pharmaceutical, NIPRO, Meiji, Taisho Pharmaceutical, Ono Pharmaceutical, Kowa, Takeda Pharmaceutical, Daiichi Sankyo, and Novartis Pharma. IK reports grants and/or personal fees from Idorsia Pharmaceuticals Japan, Daiichi Sankyo, Takeda Pharmaceutical, Mitsubishi Tanabe Pharma, Teijin Pharma, AstraZeneca, Kowa, MSD, Otsuka Pharmaceutical, Ono Pharmaceutical, Nippon Boehringer Ingelheim, Novartis Pharma, and Bayer Yakuhin. HT reports grants and/or personal fees from Daiichi Sankyo, Novartis Pharma, Otsuka Pharmaceutical, Pfizer Japan, Mitsubishi Tanabe Pharma, Teijin Pharma, Nippon Boehringer Ingelheim, AstraZeneca, Ono Pharmaceutical, Kowa, IQVIA Service Japan, MEDINET, Medical Innovation Kyushu, Bayer Yakuhin, Johnson & Johnson, NEC, Nippon Rinsho and Japanese Heart Failure Society. Other authors report no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors received no financial support for the research or publication of this article.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ikeda, S., Shinohara, K., Enzan, N. et al. A higher resting heart rate is associated with cardiovascular event risk in patients with type 2 diabetes mellitus without known cardiovascular disease. Hypertens Res 46, 1090–1099 (2023). https://doi.org/10.1038/s41440-023-01178-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01178-1
Keywords
This article is cited by
-
Preface–Metabolic aspects of hypertension in Asia
Hypertension Research (2023)
-
Resting heart rate as a possible biomarker and target to prevent future cardiovascular disease in type 2 diabetes patients (HTR-2023-0066.R2)
Hypertension Research (2023)