Abstract
Hypertensive disorders of pregnancy increase the risk of adverse maternal and fetal outcomes. In 2018, the Japanese classification of hypertensive disorders of pregnancy was standardized with those of other countries, and a hypertensive disorder of pregnancy was considered to be present if hypertension existed during pregnancy and up to 12 weeks after delivery. Strategies for the prevention of hypertensive disorders of pregnancy have become much clearer, but further research is needed on appropriate subjects and methods of administration, and these have not been clarified in Japan. Although guidelines for the use of antihypertensive drugs are also being studied and standardized with those of other countries, the use of calcium antagonists before 20 weeks of gestation is still contraindicated in Japan because of the safety concerns that were raised regarding possible fetal anomalies associated with their use at the time of their market launch. Chronic hypertension is now included in the definition of hypertensive disorders of pregnancy, and blood pressure measurement is a fundamental component of the diagnosis of hypertensive disorders of pregnancy. Out-of-office blood pressure measurements, including ambulatory and home blood pressure measurements, are important for pregnant and nonpregnant women. Although conditions such as white-coat hypertension and masked hypertension have been reported, determining their occurrence in pregnancy is complicated by the gestational week. This narrative review focused on recent reports on hypertensive disorders of pregnancy, including those related to blood pressure measurement and classification.
Similar content being viewed by others
Introduction
In Japan, “pregnancy toxemia”, with three main features, “hypertension,” “proteinuria,” and “edema”, was defined and classified in 1982 [1] and then again in 1984 [2]. This term was widely used until 2005, when it was changed to “pregnancy-induced hypertension.” In 2018, the classification was standardized with those of other countries, and “hypertensive disorders of pregnancy (HDP)” were considered to be present if hypertension existed during pregnancy and up to 12 weeks after delivery [3]. High blood pressure before pregnancy (chronic hypertension) is now included in the definition of HDP. Among the various hypotheses explaining the etiology of HDP, the two-stage theory and angiogenesis imbalance are the most plausible. The two-stage theory of the etiology of HDP may have led to the novel possibility of treatment/prevention for HDP. Furthermore, assessing the circulating levels of angiogenic factors may have diverse clinical roles in preventing adverse outcomes in HDP [4]. This narrative review focused on recent reports on HDP, including those related to blood pressure measurement and classification.
Classification and definition of hypertensive disorders of pregnancy
HDP are classified into four types: preeclampsia, gestational hypertension, superimposed preeclampsia, and chronic hypertension [5]. Preeclampsia is defined as hypertension after 20 gestational weeks with proteinuria, organ damage, or uteroplacental dysfunction. Gestational hypertension is similar to preeclampsia; however, the condition is defined as hypertension alone after 20 gestational weeks. Based on the Japan Society for the Study of Hypertension in Pregnancy (JSSHP), superimposed preeclampsia is defined as hypertension accompanied by organ damage or proteinuria [3, 5].
In normal pregnancy, spiral artery remodeling occurs, where trophoblastic cells invade the decidua and replace the endothelial cells and vascular smooth muscle of the decidua spiral artery. As a result, the maternal blood vessels begin to perfuse into the interchorionic space, which increases the partial pressure of oxygen in the placenta and reduces systemic vascular resistance (Fig. 1A). Angiogenic factors, vascular endothelial growth factors (VEGFs), and placental growth factors (PlGFs) affect angiogenesis intracellularly through the receptor VEGFR-1 (Fig. 1B). Uterine natural killer (uNK) cells and regulatory T cells are essential for maintaining pregnancy and inhibiting allogeneic responses toward the fetus [6, 7]. Decidual uNK cells control trophoblast invasion by producing interleukin-8 and interferon-inducible protein-10 chemokines and secrete a series of angiogenic factors [8]. Early vascular changes resulting from desquamation, such as intimal vacuolation and disintegration, and thinning of the tunica media occur before trophoblastic cells are present near the spiral arteries of the uterus [9].
Schematic diagram of the two-stage theory of preeclampsia. In normal pregnancy, appropriate EVT invasion into the maternal endometrium (red arrow) leads to sufficient maternal blood flow from the spiral artery (A). PlGF, which is secreted from the placenta, activates VEGF and maintains a healthy endothelium (B). On the other hand, in preeclamptic pregnancy, incomplete invasion of the EVT (blue arrow) leads to insufficient maternal blood flow from the spiral artery and subsequent placental hypoxia (C). sFlt1 is then secreted from the placenta, which suppresses VEGF, resulting in systemic endothelial dysfunction and the appearance of various clinical symptoms (D). HELLP syn. hemolysis, elevated liver enzymes, low platelet count syndrome, FGR fetal growth restriction, NK cells natural killer cells, EVT extravillous trophoblast, PlGF placental growth factor, sFlt1 soluble fms-like tyrosine kinase-1, VEGF vascular endothelial growth factor
Preeclampsia
Preeclampsia is a complex medical disorder [10]. According to recent guidelines in Japan [5] and other countries [10,11,12,13,14], preeclampsia is characterized by hypertension with maternal acute kidney injury, liver dysfunction, neurological features, hemolysis or thrombocytopenia, or fetal growth restriction. Preeclampsia is thought to originate from the placenta because of the rapid improvement of clinical symptoms of preeclampsia after placenta delivery [15], while retained placenta leads to the development of preeclampsia; the removal of the placenta by intrauterine curettage results in disappearance of the symptoms [16].
Insufficient angiogenesis and remodeling cause an incomplete increase in the partial pressure of oxygen in the fetal placental circulation (Fig. 1C), resulting in placental ischemia and damage [17]. Stimulated soluble VEGFR-1 (sFlt-1) production in trophoblast cells inhibits PlGF production and soluble endoglin (sEng) production [18]. Inhibition of VEGF and PlGF by sFlt-1 suppresses the invasion of trophoblastic cells into the shed membrane and damages vascular endothelial cells (Fig. 1D). By binding and antagonizing TGF-β, sEng inhibits the invasion of cytotrophoblast cells [19]. The transition of these factors into maternal circulation causes the maternal symptoms of preeclampsia [20, 21]. Placental abnormalities in early pregnancy may cause chronic uteroplacental insufficiency, local ischemia, and the release of inflammatory cytokines, resulting in earlier maternal hypertension in early-onset preeclampsia [22,23,24]. In contrast, late-onset preeclampsia is more frequently based on placental dysfunction associated with chronic oxidative stress due to maternal metabolic abnormalities such as obesity and insulin resistance [22, 23, 25]. At the same time, there is much overlap in placental pathology and continuous features in desmoplastic vascular lesion pathology among the four HDP subtypes [26].
Superimposed preeclampsia
Superimposed preeclampsia is defined as chronic hypertension or kidney disease that progresses to preeclampsia [3]. It should be noted that in countries other than Japan, it basically refers only to superimposed chronic hypertension [10,11,12,13,14]. Vascular endothelial dysfunction is reported to predict the development of superimposed preeclampsia in chronic hypertension [27]. In preeclampsia following de novo gestational hypertension, early placental calcification and weight gain precede preeclampsia [28]. Pregnant women with IgA nephropathy [29] and chronic kidney disease [30] had 7.3- and 10.4-fold greater risks of preeclampsia than others, respectively.
Chronic hypertension in pregnancy
Blood pressure during early pregnancy seems important in pregnancies complicated by hypertension [31, 32]. A systolic blood pressure <130 mmHg within 14–15 weeks of gestation was reported to reduce the risk of early-onset superimposed preeclampsia in women with chronic hypertension [33]. As described in a later section on white-coat hypertension, it is essential to diagnose whether a patient has sustained or white-coat hypertension. Because chronic hypertension is a risk factor for perinatal mortality in both early and late gestation, a planned delivery at 37 to 38 weeks of gestation is reported to be a superior balance of risk [34].
Prognosis
Maternal outcomes
Regarding the risk of developing cardiovascular diseases later in life, although there are differences among HDP subtypes, Veerbeek et al. [35] reported that all types of HDP seem to be associated with high risks. Gestational hypertension is reported to be associated with a 4.2-fold higher risk for future chronic hypertension [36] and a greater risk of cardiovascular disease, coronary heart disease, and heart failure [37]. Preeclampsia is associated with a fourfold increased risk of future heart failure and a twofold increased risk of coronary heart disease, stroke, and death due to coronary heart or cardiovascular disease [38]. Women with HDP were reported to have a 6.3-fold higher risk for future hypertension within 2 years postpartum compared to controls [39] and a 4.9-fold higher risk of chronic kidney disease in later life [40].
Birth outcomes
Maternal cardiac output in early pregnancy has been associated with being small for gestational age (SGA) [41]. Maternal hypertension-related factors were associated with infant growth via placental factors based on the genome wide association study summary statistics of BioBank Japan data and compared with cohort data [42]. The Hokkaido study showed that women with HDP had 2.1-, 3.5-, and 3.6-fold higher risks of having SGA infants, preterm birth, and infants with low birth weight than those with normotensive pregnancy [43]. Home [44] and ambulatory [45] blood pressure measurements have been shown to be more associated with birth weight than clinic blood pressure; these are reviewed in subsequent sections. The trajectory of maternal blood pressure during pregnancy is also an indicator of infant birth weight [46,47,48].
Long-term outcomes of offspring
According to a meta-analysis of eight studies, HDP were associated with a 1.2-fold higher risk of asthma in offspring [49]. In a study, offspring exposed to HDP had a 1.4- and 1.3-fold higher risk for autism spectrum disorders and attention-deficit hyperactivity disorder, respectively [50]. The Helsinki Birth Cohort Study reported that offspring exposed to maternal gestational hypertension in utero had an increased risk of type 2 diabetes in late adulthood after adjustment for low birth weight or small for gestational age infants [51].
The results of studies in Japan on the long-term prognosis of pregnant women with HDP and their children exposed to HDP are now being reported. The TMM BirThree Cohort Study reported that women with superimposed preeclampsia had a 1.8-fold increased risk of having children with autistic behavior at 2 years old compared to normotensive women [52]. The Hokkaido Birth Cohort Study reported that male children exposed to HDP caught up with their growth and gained more weight by 7 years of age than male children who were not exposed to HDP [53]. According to observations in the Japan Environment and Children’s Study (JECS), HDP were not a risk factor for offspring regardless of the sensitivity analyses using possible mediating factors such as cesarean delivery, birth weight, and gestational age [54].
When examining the association between HDP and prognosis, there is no need to adjust for preterm birth and low birth weight because they are included in HDP outcomes and are mediators rather than confounders when considering their impact on the long-term prognosis of offspring [49, 50, 52, 53]. On the other hand, as mentioned earlier, several studies have performed sensitivity analyses considering the role of HDP as mediators [51, 54]. Based on the results of the ongoing mediator analysis and other studies, future studies need to examine possible intervention points for the association between HDP and child outcomes and develop better intervention methods.
Prediction, prevention, and treatment
Associated factors and prediction
The Fetal Medicine Foundation (FMF) first-trimester prediction model (the FMF triple test) has high detection rates of 90% and 75% for the prediction of early and preterm preeclampsia, respectively, with a 10% false-positive rate [55]. This FMF triple test consists of a combination of maternal factors and measurements of mean arterial pressure, the uterine artery pulsatility index, and serum placental growth factor. An Asia-wide study using an algorithm developed by the FMF in Asian people confirmed the validity of the FMF triple test with a detection rate of 64% for the prediction of preterm preeclampsia with a 10% false-positive rate [56].
In addition to the FMF triple test, several predictors have been reported in individual studies, and those presented in this study are listed in Table 1.
The JECS is a cohort study that started in 2011 to investigate the relationship between environmental exposure and child health. Several studies on HDP have been conducted with the JECS cohort. Higher levels of HbA1c at a nondiabetic level [57], both lower and higher Na intake before pregnancy [58], elevated serum IgE levels during the first trimester [59], higher caffeine intake [60], working a schedule of ≥36 h per week with night shifts [61], smoking [62], alcohol consumption [63], and becoming pregnant with in vitro fertilization and embryo transfer [64] were associated with the risk of hypertensive disorders of pregnancy. Moreover, coffee intake was associated with a decreased risk of HDP [60]. Although this is a large cohort study, some studies reported that no association between the exposures and outcomes can be found, such as calcium intake and HDP among primiparas [65]. The JECS involves a novel approach to adjunct studies. The peak areas of N-dimethylglycine and S-methylcysteine were significantly higher in the first-trimester serum of patients with early-onset HDP than in controls [66].
Sleep quality in early pregnancy may help predict elevated systolic blood pressure in the first trimester [67], and overnight oxygen saturation screening ~1 month before the due date may be useful in predicting late-onset gestational hypertension [68]. Unmodifiable factors include twin pregnancy [69, 70] and residing in a high-altitude area (>2500 m) [71, 72]. Blood pressure is known to be elevated in twin pregnancy [69], regardless of whether the pregnancy is a dichorionic or monochorionic diamniotic twin pregnancy [70]; therefore, pregnant women with unmodifiable factors should be followed up as high-risk pregnancies.
Several efforts to perform comprehensive metabolomic analysis in samples of pregnant women have been reported, such as the C-MATCH [73] and HELIX studies [74]. The metabolite profiles of women who developed HDP were comparable to those of women with normal pregnancies with longer gestation in the Maternity Log study, which is an adjunct to the BirThree cohort study [75].
Prevention
Aspirin administration has been described in various guidelines as effective in preventing the onset of preeclampsia. The ASPRE study showed that aspirin treatment for pregnant women at high risk for preeclampsia reduced the incidence of preeclampsia to 0.38 [76]. The NICE [11], ACOG [12], USPSTF [77], SOGC [13], SOMANZ [14], and ISSHP [10] guidelines state that aspirin should be administered to high-risk pregnant women. However, the Japanese guidelines from the JSSHP that were issued in 2015 state that aspirin should be given to a limited number of women [78], while those that were issued in 2021 state that aspirin should be considered for women with preeclampsia to prevent recurrence in subsequent pregnancy [5]. In Asian women, the dose-dependent efficacy of low-dose aspirin [79] and its efficacy in women with blood pressure of 130–139/80–89 mmHg, which is included in the American College of Cardiology/American Heart Association definition of Stage 1 hypertension or mild hypertension [80], have also been reported. However, a study reported that aspirin has poor efficacy when started at 12–20 weeks gestation [81]. The ADA guidelines also strongly recommended aspirin for women with diabetic pregnancies until 2020 [82]; moreover, the recommendations became weaker in the 2021 edition and later editions [83]. A recent study reported limited efficacy of aspirin in preventing preeclampsia among women with diabetic pregnancies [84]. Future studies are warranted on eligible subjects and administration methods.
Treatment
In principle, in Japan, inpatient management is recommended for HDP patients with blood pressure of 160/110 mmHg or higher, antihypertensive treatment should be given if a patient’s blood pressure is repeatedly found to be 160/110 mmHg or higher, and antihypertensive treatment is considered if a patient’s blood pressure is 140/90 mmHg or higher. Furthermore, if a patient has recurrent blood pressure of 160/110 mmHg or higher or has preeclamptic symptoms, magnesium sulfate should be administered to prevent eclampsia, and if management at the patient’s own facility is difficult, referral to a higher-level medical facility should be considered [5].
There are concerns that antihypertensive treatment during pregnancy may increase the risk of placental abruption and preterm delivery [85]. Data from Scotland showed a 2.3-fold increase in congenital defects with the use of antihypertensive drugs [86]. However, untreated hypertension, not antihypertensive medication, is a risk to the child [87]. The CHIPS study reported no significant group differences in the risk of pregnancy loss, high-level neonatal care, or overall maternal complications between less-tight (target office diastolic blood pressure of 100 mmHg) and tight (target office diastolic blood pressure of 85 mmHg) control of hypertension in pregnancy [88]. A recent meta-analysis showed that blood pressure-lowering treatment significantly prevented not only severe hypertension, preeclampsia, and severe preeclampsia but also placental abruption and preterm birth, while the risk of SGA was increased [89].
Currently, Japanese guidelines refer to methyldopa, hydralazine, and labetalol as oral antihypertensive drugs that can be used during pregnancy, while nifedipine can only be used after 20 weeks of pregnancy [5]. Guidelines for the use of different antihypertensive drugs have not been developed. There is a possibility of improved maternal prognosis with physiological nomogram-guided care and tailored pharmacological intervention [90]. In Japan, the use of calcium antagonists in early pregnancy is still not approved on the package label, and deviation from the guidelines is a concern [91]. However, in Japan, the most frequently prescribed oral antihypertensive drug during pregnancy is nifedipine, followed by methyldopa, hydralazine, and furosemide [92]. It has been reported that the risk of birth defects due to amlodipine use in the first trimester was not significantly different compared to the risk of the use of other antihypertensives in a case–control study in Japan [93]; more extensive observation is urgently needed.
Similar concerns have been raised regarding long-term prognosis. A comparison of the long-term prognosis of infants between treatment groups in a historical cohort study also reported the possibility of attention-deficit hyperactivity disorder and sleep disorders in infants whose mothers received drug interventions for gestational hypertension [94]. On the other hand, studies examining the effects of antihypertensive medications may not have examined baseline blood pressure levels [86], or baseline blood pressure levels may be obviously different [94]; hence, the risk of antihypertensive medication use must be carefully assessed. Such concerns are expected to be clarified by national-scale cohort studies.
Blood pressure measurement during pregnancy
There are several debates regarding how blood pressure should be measured during pregnancy [95]. Reports suggest that blood pressure values in pregnant women with preeclampsia vary depending on the measurement environment [96]. Hurrell et al. conducted a detailed review of blood pressure measurements in pregnant women [97]. A recent meta-analysis also confirmed that both systolic and diastolic blood pressure decrease by ~4 mmHg in the second trimester [98]; the results were very similar to those of a single cohort study investigating the use of home blood pressure [99].
Ambulatory blood pressure measurement
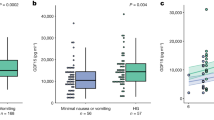
Ambulatory blood pressure measurement is valuable for diagnosing masked or white-coat hypertension (16) and assessing diurnal variations in blood pressure in pregnant women [100, 101]. Normal daytime values for ambulatory blood pressure monitoring in pregnant women have been reported to be less than 130/77 mmHg at ≤22 weeks, 133/81 mmHg at 26–30 weeks, and 135/86 mmHg after 30 weeks [102]. Diurnal variations in blood pressure during pregnancy have been reported to be nocturnal declines of 12–14%/18–19% in systolic/diastolic blood pressure [100]. It has also been reported that nocturnal declines in blood pressure are attenuated before gestational hypertension nephropathy becomes apparent [101]. Among 146 Japanese pregnant women with suspected HDP, ambulatory blood pressure monitoring was more strongly associated with SGA infants, with an odds ratio of 1.74 times for every 10 mmHg increase (95% CI: 1.28–2.38; P = 0.001) compared with office blood pressure measurement (OR: 1.40; 95% CI: 0.92–2.13; P = 0.11) [45].
Home blood pressure measurement
Home blood pressure measurement is suitable for detecting long-term and seasonal variations in blood pressure. In a 2008 statement on home blood pressure measurement, the American Heart Association noted that “Home blood pressure measurement is theoretically ideal for monitoring changes in blood pressure during pregnancy because it is the best technique for providing multiple readings recorded at the same time of day over prolonged periods of time.” [103]. Furthermore, a report from the consensus meeting of the European Council on Hypertension issued around the same time stated that “Home blood pressure monitoring, although at present not commonly practiced in this setting, has considerable potential in improving the management of pregnant women.” [104]. According to the Japanese Society of Hypertension guidelines, for general (nonpregnant) patients, if the results of office blood pressure and home blood pressure measurements are different, the home blood pressure result has priority for treatment [91]. In pregnancy, home blood pressure measurements may be taken by pregnant women before recommendations are made by health care providers. Using home blood pressure monitoring, seasonal blood pressure [99] and hemodynamic changes are well observed. In a study that simultaneously included both home and clinic blood pressure levels in early pregnancy, the adjusted odds ratios for having a baby that was 500 g smaller per standard deviation increase in mean and diastolic blood pressure were 1.29 (95% CI: 1.04–1.59) and 1.28 (95% CI: 1.04–1.58) for home blood pressure and 1.02 (95% CI: 0.83–1.24) and 1.06 (95% CI: 0.87–1.30) for clinic blood pressure, respectively, with only home blood pressure measurements having a significant association [44]. Furthermore, the maternal blood pressure trajectory during pregnancy was an indicator of infant birth weight [46]. However, no study has determined whether interventions based on home blood pressure measurements improve outcomes.
Several values have been proposed as the diagnostic threshold of home blood pressure based on population distribution and regression with office blood pressure values. Using the standard major axis method, the home blood pressure values reported to be equivalent to a clinical blood pressure of 140/90 mmHg were 120.8/83.5 mmHg, 126.0/85.2 mmHg, and 136.3/89.3 mmHg in the first, second, and third trimesters, respectively [105]. However, no consensus value has been established [106].
A meta-analysis reported in 2020 summarized nine studies and noted that the use of home blood pressure measurements in the antenatal period was associated with a reduced risk of induction of labor, hospitalization before delivery, and diagnosis of preeclampsia and that the number of prenatal visits was significantly lower in the home blood pressure group, but there was no significant difference in the combined maternal, fetal, or neonatal outcomes compared to conventional care [107].
Clinical significance of white-coat hypertension
White-coat hypertension is a condition in which a patient has high blood pressure in the office but normal blood pressure outside the office. Generally, 24-h ambulatory blood pressure monitoring or home blood pressure monitoring may be used to identify white-coat hypertension. Ishikuro et al. reported that among pregnant women who were normotensive, the white-coat effect during pregnancy was 4.1/3.8, 3.4/1.6, and 1.8/2.4 mmHg in early, mid-, and late pregnancy, respectively [108]. When the factors affecting the white-coat effect were examined in the same population, no significant differences were found for body mass in sex, age, or family history of hypertension. However, the effect was significantly greater in primiparas than in multiparas in early pregnancy for systolic blood pressure and in late pregnancy for diastolic blood pressure [109]. A meta-analysis of 16 studies on the white-coat effect showed that office blood pressure measurements were 4/3 (3–6/2–4) mmHg higher than home blood pressure measurements [106]. White-coat hypertension is prevalent in women with preexisting diabetes and may indicate an increased risk of developing pregnancy-induced hypertensive disorders later in life [110].
Based on ambulatory blood pressure monitoring in early pregnancy, it has been reported that 22% of pregnant women have sustained hypertension, and 8% of those with white-coat hypertension develop preeclampsia; thus, white-coat hypertension in pregnancy may have a relatively good prognosis [102]. It is essential to recognize that hypertension in the office may not necessarily require antihypertensive treatment if the blood pressure outside the office is normal. However, 42% of pregnant women with white-coat hypertension in early pregnancy showed hypertension both in the office and out of the office until delivery [102]; therefore, careful follow-up is necessary in such cases.
Clinical significance of masked hypertension
There are few studies on masked hypertension in pregnant women. Salazar et al. reported that masked hypertension is a prevalent and high-risk condition. An office blood pressure of ≥125/75 mmHg in the second half of gestation seems appropriate for indicating out-of-office measurements in women with high-risk pregnancies [111]. Pregnant women with masked hypertension had a 7.8 times higher risk of preeclampsia than those who were normotensive [112]. Unlike white-coat hypertension, masked hypertension cannot be detected unless all pregnant women who are at risk receive out-of-office blood pressure measurements. Therefore, further study is needed to determine which women should undergo blood pressure measurement outside the office.
Present blood pressure monitoring situations in clinical practice
According to a survey reported in 2021, 89.3% of obstetricians took blood pressure measurements in an outpatient setting only once per occasion if a woman’s blood pressure was normal. However, if the pregnant women had hypertension, 54.8% took a second measurement, and 40.3% repeated blood pressure measurements until a stable reading was obtained [113]. Furthermore, 62.8% of the obstetricians recorded the lowest value when they measured blood pressure twice, and 69.0% of the physicians recorded the last measurement when the blood pressure was measured until it stabilized [113]. Therefore, when conducting research based on databases, researchers need to recognize some variation in the measurements recorded on each measurement occasion. On the other hand, blood pressure measurements for research purposes at a venue different from that of the antenatal checkup was reported to be equivalent to home blood pressure measurements and significantly lower than those at antenatal checkups, and the possibility of a stressful environment during the antenatal checkup causing an increase in blood pressure should be considered [114].
A survey of family medicine and obstetrics/gynecology physicians providing prenatal care at a tertiary obstetrics hospital in Canada found that obstetricians were more likely to use home blood pressure monitoring. In contrast, family physicians were more likely to use 24 h ambulatory blood pressure monitoring as a diagnostic aid. While obstetricians were more likely than family physicians to use effective home blood pressure monitoring during pregnancy and monitor hypertension with home blood pressure monitoring, family physicians were significantly more likely than obstetricians to target “tight” blood pressure control [115].
In a survey of 128 patients conducted in the United States, postpartum women perceived a telehealth technology remote intervention as a safe and easy-to-use method, with an acceptable burden of care and an overall satisfactory method of monitoring blood pressure in the postpartum period [116]. A survey conducted in Belgium reported that 80% of midwives and 67% of obstetricians who used remote blood pressure monitoring in pregnancy perceived digital technologies as an important component of prenatal monitoring [117]. The results of an online survey of obstetricians in the United Kingdom showed that the percentage of obstetricians who thought that home blood pressure measurements and urinalysis were helpful indicators of clinical diagnosis rose from 88% before the COVID-19 pandemic to 96% after the pandemic. In addition, 47% of the obstetricians agreed that pregnant women would change their predetermined medications based on their measured blood pressure levels [118].
Novel attempt at blood pressure telemonitoring
In 2008, the transmission of home blood pressure measurements was discussed [119], but the explorations of remote monitoring are rapidly progressing during the COVID-19 pandemic. A study examined current practices and attitudes concerning home-based blood pressure and cardiotocography monitoring and telemonitoring in high-risk pregnancies requiring maternal and fetal monitoring and reported that home-based monitoring and telemonitoring were offered in 26% and 23% of hospitals, respectively, in the Netherlands [120]. In a retrospective comparison, the digital platform among high-risk pregnancies significantly reduced prenatal visits, ultrasounds, and hypertension-related hospitalizations compared to usual care without self-monitoring.
As mentioned earlier, the Maternity Log study [75] attempted to collect life logs, including home blood pressure measurements. There have been text-based attempts at blood pressure management in the postpartum period [121]. A study attempted to use a smartphone application to monitor home blood pressure in Belgium [122]. A prospective, randomized, controlled trial, called BP-PRESELF, using home blood pressure measurements is ongoing to assess whether home blood pressure monitoring in women with a history of preeclampsia/HELLP syndrome during pregnancy is a valuable tool for the early detection of chronic hypertension [123].
Conclusion
Blood pressure measurement during pregnancy is crucial in diagnosing HDP. The precise measurement and evaluation of blood pressure, including its variability, will continue to play an essential role in determining the prognosis and elucidating the pathogenesis of HDP.
References
Suzuki M, Ichijo M, Ichinoe K, Okada H, Kuji N, Kobori T, et al. Report of the Committee on Pregnancy Toxicosis. Acta Obst Gynaec Jpn. 1982;34:837–40.
Suzuki M, Ichijo M, Ichinoe K, Iwasaki H, Okada H, Kawabe S, et al. Report of the Committee on Pregnancy Toxicosis. Acta Obst Gynaec Jpn. 1984;36:983–9.
Watanabe K, Matsubara K, Nakamoto O, Ushijima J, Ohkuchi A, Koide K, et al. Outline of the new definition and classification of “Hypertensive Disorders of Pregnancy(HDP)”: a revised JSSHP statement of 2005. Hypertens Res Pregnancy. 2018;6:33–7.
Ngene NC, Moodley J. Role of angiogenic factors in the pathogenesis and management of pre-eclampsia. Int J Gynaecol Obstet. 2018;141:5–13.
Japan Society for the Stuy of HYPERTENSION IN PREGNANCY. Best Practise Guide 2021 for Care and Treatment of Hypertension in Pregnancy. Tokyo: Medical View Co., Ltd.; 2021.
Robertson SA, Guerin LR, Bromfield JJ, Branson KM, Ahlstrom AC, Care AS. Seminal fluid drives expansion of the CD4+CD25+ T regulatory cell pool and induces tolerance to paternal alloantigens in mice. Biol Reprod. 2009;80:1036–45.
Aluvihare VR, Kallikourdis M, Betz AG. Regulatory T cells mediate maternal tolerance to the fetus. Nat Immunol. 2004;5:266–71.
Hanna J, Goldman-Wohl D, Hamani Y, Avraham I, Greenfield C, Natanson-Yaron S, et al. Decidual NK cells regulate key developmental processes at the human fetal-maternal interface. Nat Med. 2006;12:1065–74.
Sava RI, March KL, Pepine CJ. Hypertension in pregnancy: taking cues from pathophysiology for clinical practice. Clin Cardiol. 2018;41:220–7.
Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S, et al. Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension. 2018;72:24–43.
Hypertension in pregnancy: diagnosis and management. London; 2019. https://www.nice.org.uk/guidance/ng133.
Gestational Hypertension and Preeclampsia: ACOG Practice Bulletin Summary, Number 222. Obstet Gynecol. 2020;135:1492–95.
Magee LA, Pels A, Helewa M, Rey E, von Dadelszen P, Canadian Hypertensive Disorders of Pregnancy Working G. Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy. Pregnancy Hypertens. 2014;4:105–45.
Lowe SA, Bowyer L, Lust K, McMahon LP, Morton MR, North RA, et al. The SOMANZ guidelines for the management of hypertensive disorders of pregnancy 2014. Aust NZ J Obstet Gynaecol. 2015;55:11–6.
Hunter CA Jr, Howard WF, Mc CC Jr. Amelioration of the hypertension of toxemia by postpartum curettage. Am J Obstet Gynecol. 1961;81:884–9.
Magann EF, Martin JN Jr., Isaacs JD, Perry KG Jr., Martin RW, Meydrech EF. Immediate postpartum curettage: accelerated recovery from severe preeclampsia. Obstet Gynecol. 1993;81:502–6.
Lyall F, Robson SC, Bulmer JN. Spiral artery remodeling and trophoblast invasion in preeclampsia and fetal growth restriction: relationship to clinical outcome. Hypertension. 2013;62:1046–54.
Gilbert JS, Gilbert SA, Arany M, Granger JP. Hypertension produced by placental ischemia in pregnant rats is associated with increased soluble endoglin expression. Hypertension. 2009;53:399–403.
Wang A, Rana S, Karumanchi SA. Preeclampsia: the role of angiogenic factors in its pathogenesis. Physiology. 2009;24:147–58.
Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Investig. 2003;111:649–58.
Venkatesha S, Toporsian M, Lam C, Hanai J, Mammoto T, Kim YM, et al. Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat Med. 2006;12:642–9.
Vatten LJ, Skjaerven R. Is pre-eclampsia more than one disease? BJOG. 2004;111:298–302.
Egbor M, Ansari T, Morris N, Green CJ, Sibbons PD. Morphometric placental villous and vascular abnormalities in early- and late-onset pre-eclampsia with and without fetal growth restriction. BJOG. 2006;113:580–9.
Moldenhauer JS, Stanek J, Warshak C, Khoury J, Sibai B. The frequency and severity of placental findings in women with preeclampsia are gestational age dependent. Am J Obstet Gynecol. 2003;189:1173–7.
Ness RB, Roberts JM. Heterogeneous causes constituting the single syndrome of preeclampsia: a hypothesis and its implications. Am J Obstet Gynecol. 1996;175:1365–70.
Stanek J. Placental pathology varies in hypertensive conditions of pregnancy. Virchows Arch. 2018;472:415–23.
Bramham K, Villa PM, Joslin JR, Laivuori H, Hamalainen E, Kajantie E, et al. Predisposition to superimposed preeclampsia in women with chronic hypertension: endothelial, renal, cardiac, and placental factors in a prospective longitudinal cohort. Hypertens Pregnancy. 2020;39:326–35.
Chen KH, Seow KM, Chen LR. Progression of gestational hypertension to pre-eclampsia: a cohort study of 20,103 pregnancies. Pregnancy Hypertens. 2017;10:230–7.
Liu Y, Ma X, Zheng J, Liu X, Yan T. A systematic review and meta-analysis of kidney and pregnancy outcomes in IgA nephropathy. Am J Nephrol. 2016;44:187–93.
Zhang JJ, Ma XX, Hao L, Liu LJ, Lv JC, Zhang H. A systematic review and meta-analysis of outcomes of pregnancy in CKD and CKD outcomes in pregnancy. Clin J Am Soc Nephrol. 2015;10:1964–78.
Nzelu D, Dumitrascu-Biris D, Nicolaides KH, Kametas NA. Chronic hypertension: first-trimester blood pressure control and likelihood of severe hypertension, preeclampsia, and small for gestational age. Am J Obstet Gynecol. 2018;218:e331–7.
Nzelu D, Dumitrascu-Biris D, Kay P, Nicolaides KH, Kametas NA. Severe hypertension, preeclampsia and small for gestational age in women with chronic hypertension diagnosed before and during pregnancy. Pregnancy Hypertens. 2018;14:200–4.
Ueda A, Hasegawa M, Matsumura N, Sato H, Kosaka K, Abiko K, et al. Lower systolic blood pressure levels in early pregnancy are associated with a decreased risk of early-onset superimposed preeclampsia in women with chronic hypertension: a multicenter retrospective study. Hypertens Res. 2022;45:135–45.
Grover S, Brandt JS, Reddy UM, Ananth CV. Chronic hypertension, perinatal mortality and the impact of preterm delivery: a population-based study. BJOG. 2022;129:572–9.
Veerbeek JH, Hermes W, Breimer AY, van Rijn BB, Koenen SV, Mol BW, et al. Cardiovascular disease risk factors after early-onset preeclampsia, late-onset preeclampsia, and pregnancy-induced hypertension. Hypertension. 2015;65:600–6.
Watanabe M, Sairenchi T, Nishida K, Uchiyama K, Haruyama Y, Satonaka H, et al. Gestational hypertension as risk factor of hypertension in middle-aged and older women. Int J Environ Res Public Health. 2020;17:4052.
Lo CCW, Lo ACQ, Leow SH, Fisher G, Corker B, Batho O, et al. Future cardiovascular disease risk for women with gestational hypertension: a systematic review and meta-analysis. J Am Heart Assoc. 2020;9:e013991.
Wu P, Haththotuwa R, Kwok CS, Babu A, Kotronias RA, Rushton C, et al. Preeclampsia and future cardiovascular health: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2017;10:e003497.
Giorgione V, Ridder A, Kalafat E, Khalil A, Thilaganathan B. Incidence of postpartum hypertension within 2 years of a pregnancy complicated by pre-eclampsia: a systematic review and meta-analysis. BJOG. 2021;128:495–503.
Oishi M, Iino K, Tanaka K, Ishihara K, Yokoyama Y, Takahashi I, et al. Hypertensive disorders of pregnancy increase the risk for chronic kidney disease: A population-based retrospective study. Clin Exp Hypertens. 2017;39:361–5.
De Paco C, Kametas N, Rencoret G, Strobl I, Nicolaides KH. Maternal cardiac output between 11 and 13 weeks of gestation in the prediction of preeclampsia and small for gestational age. Obstet Gynecol. 2008;111:292–300.
Sato N, Fudono A, Imai C, Takimoto H, Tarui I, Aoyama T, et al. Placenta mediates the effect of maternal hypertension polygenic score on offspring birth weight: a study of birth cohort with fetal growth velocity data. BMC Med. 2021;19:260.
Poudel K, Kobayashi S, Miyashita C, Ikeda-Araki A, Tamura N, Ait Bamai Y, et al. Hypertensive disorders during pregnancy (HDP), maternal characteristics, and birth outcomes among Japanese Women: a Hokkaido Study. Int J Environ Res Public Health. 2021;18:3342.
Iwama N, Metoki H, Ohkubo T, Ishikuro M, Obara T, Kikuya M, et al. Maternal clinic and home blood pressure measurements during pregnancy and infant birth weight: the BOSHI study. Hypertens Res. 2016;39:151–7.
Eguchi K, Ohmaru T, Ohkuchi A, Hirashima C, Takahashi K, Suzuki H, et al. Ambulatory BP monitoring and clinic BP in predicting small-for-gestational-age infants during pregnancy. J Hum Hypertens. 2016;30:62–7.
Iwama N, Oba MS, Satoh M, Ohkubo T, Ishikuro M, Obara T, et al. Association of maternal home blood pressure trajectory during pregnancy with infant birth weight: the BOSHI study. Hypertens Res. 2020;43:550–9.
Guo Q, Feng P, Yu Q, Zhu W, Hu H, Chen X, et al. Associations of systolic blood pressure trajectories during pregnancy and risk of adverse perinatal outcomes. Hypertens Res. 2020;43:227–34.
Teng H, Wang Y, Han B, Liu J, Cao Y, Wang J, et al. Gestational systolic blood pressure trajectories and risk of adverse maternal and perinatal outcomes in Chinese women. BMC Pregnancy Childbirth. 2021;21:155.
Li P, Xiong T, Hu Y. Hypertensive disorders in pregnancy and risk of asthma in offspring: a systematic review and meta-analysis. BMJ Open. 2021;11:e046769.
Maher GM, O’Keeffe GW, Kearney PM, Kenny LC, Dinan TG, Mattsson M, et al. Association of hypertensive disorders of pregnancy with risk of neurodevelopmental disorders in offspring: a systematic review and meta-analysis. JAMA Psychiatry. 2018;75:809–19.
Kajantie E, Osmond C, Eriksson JG. Gestational hypertension is associated with increased risk of type 2 diabetes in adult offspring: the Helsinki Birth Cohort Study. Am J Obstet Gynecol. 2017;216:e281–7.
Ishikuro M, Murakami K, Yokozeki F, Onuma T, Noda A, Ueno F, et al. Hypertension in pregnancy as a possible factor for child autistic behavior at two years old. Pregnancy Hypertens. 2021;25:88–90.
Poudel K, Kobayashi S, Miyashita C, Yamaguchi T, Tamura N, Ikeda-Araki A, et al. Hypertensive disorders during pregnancy and anthropometric measurement of children up to 7 Years of age: the Hokkaido Birth Cohort Study in Japan. Int J Environ Res Public Health. 2021;18:10951.
Yang L, Sato M, Saito-Abe M, Irahara M, Nishizato M, Sasaki H, et al. Hypertensive disorders of pregnancy and risk of allergic conditions in children: Findings from the Japan Environment and Children’s study (JECS). World Allergy Organ J. 2021;14:100581.
Chaemsaithong P, Sahota DS, Poon LC. First trimester preeclampsia screening and prediction. Am J Obstet Gynecol. 2022;226:S1071-S1097.e2. https://doi.org/10.1016/j.ajog.2020.07.020.
Chaemsaithong P, Pooh RK, Zheng M, Ma R, Chaiyasit N, Tokunaka M, et al. Prospective evaluation of screening performance of first-trimester prediction models for preterm preeclampsia in an Asian population. Am J Obstet Gynecol. 2019;221:650.e1–6.
Iwama N, Sugiyama T, Metoki H, Saito M, Hoshiai T, Watanabe Z, et al. Associations between glycosylated hemoglobin level at less than 24 weeks of gestation and adverse pregnancy outcomes in Japan: The Japan Environment and Children’s Study (JECS). Diabetes Res Clin Pract. 2020;169:108377.
Kyozuka H, Fukusda T, Murata T, Yamaguchi A, Kanno A, Yasuda S, et al. Impact of preconception sodium intake on hypertensive disorders of pregnancy: The Japan Environment and Children’s study. Pregnancy Hypertens. 2021;23:66–72.
Kyozuka H, Murata T, Fukuda T, Endo Y, Yamaguchi A, Yasuda S, et al. Immunoglobulin E levels and pregnancy-induced hypertension: Japan Environment and Children’s Study. Sci Rep. 2021;11:8664.
Kawanishi Y, Kakigano A, Kimura T, Ikehara S, Sato T, Tomimatsu T, et al. Hypertensive disorders of pregnancy in relation to coffee and tea consumption: the Japan Environment and Children’s Study. Nutrients. 2021;13:343.
Suzumori N, Ebara T, Matsuki T, Yamada Y, Kato S, Omori T, et al. Effects of long working hours and shift work during pregnancy on obstetric and perinatal outcomes: a large prospective cohort study-Japan Environment and Children’s Study. Birth. 2020;47:67–79.
Tanaka K, Nishigori H, Watanabe Z, Iwama N, Satoh M, Murakami T, et al. Higher prevalence of hypertensive disorders of pregnancy in women who smoke: the Japan environment and children’s study. Hypertens Res. 2019;42:558–66.
Iwama N, Metoki H, Nishigori H, Mizuno S, Takahashi F, Tanaka K, et al. Association between alcohol consumption during pregnancy and hypertensive disorders of pregnancy in Japan: the Japan Environment and Children’s Study. Hypertens Res. 2019;42:85–94.
Nagata C, Yang L, Yamamoto-Hanada K, Mezawa H, Ayabe T, Ishizuka K, et al. Complications and adverse outcomes in pregnancy and childbirth among women who conceived by assisted reproductive technologies: a nationwide birth cohort study of Japan environment and children’s study. BMC Pregnancy Childbirth. 2019;19:77.
Kyozuka H, Murata T, Fukuda T, Yamaguchi A, Kanno A, Yasuda S, et al. Association between pre-pregnancy calcium intake and hypertensive disorders during the first pregnancy: the Japan environment and children’s study. BMC Pregnancy Childbirth. 2020;20:424.
Kyozuka H, Fukuda T, Murata T, Endo Y, Kanno A, Yasuda S, et al. Comprehensive metabolomic analysis of first-trimester serum identifies biomarkers of early-onset hypertensive disorder of pregnancy. Sci Rep. 2020;10:13857.
Okada K, Saito I, Katada C, Tsujino T. Influence of quality of sleep in the first trimester on blood pressure in the third trimester in primipara women. Blood Press. 2019;28:345–55.
Watanabe M, Shinohara H, Kodama H. Nocturnal oxygen desaturation in the late third trimester of uncomplicated pregnancy for prediction of late-onset gestational hypertension. J Obstet Gynaecol Res. 2020;46:1735–43.
Mikami Y, Takai Y, Era S, Ono Y, Saitoh M, Baba K, et al. Differences in home blood pressure and pulse rates between singleton and twin pregnancies. J Int Med Res. 2018;46:1496–504.
Iwama N, Metoki H, Nishigori H, Mizuno S, Takahashi F, Tanaka K, et al. Blood pressure changes during twin pregnancies: the Japan Environment and Children’s Study. J Hypertens. 2019;37:206–15.
Grant ID, Giussani DA, Aiken CE. Blood pressure and hypertensive disorders of pregnancy at high altitude: a systematic review and meta-analysis. Am J Obstet Gynecol MFM. 2021;3:100400.
Bailey B, Euser AG, Bol KA, Julian CG, Moore LG. High-altitude residence alters blood-pressure course and increases hypertensive disorders of pregnancy. J Matern Fetal Neonatal Med. 2020. https://doi.org/10.1080/14767058.2020.1745181.
Sakurai K, Miyaso H, Eguchi A, Matsuno Y, Yamamoto M, Todaka E, et al. Chiba study of Mother and Children’s Health (C-MACH): cohort study with omics analyses. BMJ Open. 2016;6:e010531.
Maitre L, de Bont J, Casas M, Robinson O, Aasvang GM, Agier L, et al. Human Early Life Exposome (HELIX) study: a European population-based exposome cohort. BMJ Open. 2018;8:e021311.
Yamauchi T, Ochi D, Matsukawa N, Saigusa D, Ishikuro M, Obara T, et al. Machine learning approaches to predict gestational age in normal and complicated pregnancies via urinary metabolomics analysis. Sci Rep. 2021;11:17777.
Rolnik DL, Wright D, Poon LC, O’Gorman N, Syngelaki A, de Paco Matallana C, et al. Aspirin versus placebo in pregnancies at high risk for preterm preeclampsia. N Engl J Med. 2017;377:613–22.
Force USPST, Davidson KW, Barry MJ, Mangione CM, Cabana M, Caughey AB, et al. Aspirin use to prevent preeclampsia and related morbidity and mortality: US preventive services task force recommendation statement. JAMA. 2021;326:1186–191.
Japan Society for the Stuy of HYPERTENSION IN PREGNANCY. Best Practise Guide 2015 for Care and Treatment of Hypertension in Pregnancy. Tokyo: Medical View Co., Ltd.; 2015.
Gu W, Lin J, Hou YY, Lin N, Song MF, Zeng WJ, et al. Effects of low-dose aspirin on the prevention of preeclampsia and pregnancy outcomes: a randomized controlled trial from Shanghai, China. Eur J Obstet Gynecol Reprod Biol. 2020;248:156–63.
Huai J, Lin L, Juan J, Chen J, Li B, Zhu Y, et al. Preventive effect of aspirin on preeclampsia in high-risk pregnant women with stage 1 hypertension. J Clin Hypertens. 2021;23:1060–7.
Lin L, Huai J, Li B, Zhu Y, Juan J, Zhang M, et al. A randomized controlled trial of low-dose aspirin for the prevention of preeclampsia in women at high risk in China. Am J Obstet Gynecol. 2022;226:251.e251–12.
American Diabetes A. 14. Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl 1)1:S183–92.
American Diabetes Association Professional Practice C, American Diabetes Association Professional Practice C, Draznin B, Aroda VR, Bakris G, Benson G, et al. 15. Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes-2022. Diabetes Care. 2022;45(Suppl 1)1:S232–43.
Do NC, Vestgaard M, Asbjornsdottir B, Norgaard SK, Andersen LLT, Jensen DM, et al. Unchanged Prevalence of Preeclampsia After Implementation of Prophylactic Aspirin for All Pregnant Women With Preexisting Diabetes: A Prospective Cohort Study. Diabetes Care. 2021. https://doi.org/10.2337/dc21-1182.
Banhidy F, Acs N, Puho EH, Czeizel AE. The efficacy of antihypertensive treatment in pregnant women with chronic and gestational hypertension: a population-based study. Hypertens Res. 2010;33:460–6.
Fitton CA, Fleming M, Aucott L, Pell JP, Mackay DF, McLay JS. Congenital defects and early childhood outcomes following in-utero exposure to antihypertensive medication. J Hypertens. 2021;39:581–8.
Fitton CA, Fleming M, Steiner MFC, Aucott L, Pell JP, Mackay DF, et al. In utero antihypertensive medication exposure and neonatal outcomes: a Data Linkage Cohort Study. Hypertension. 2020;75:628–33.
Magee LA, von Dadelszen P, Rey E, Ross S, Asztalos E, Murphy KE, et al. Less-tight versus tight control of hypertension in pregnancy. N Engl J Med. 2015;372:407–17.
Abe M, Arima H, Yoshida Y, Fukami A, Sakima A, Metoki H, et al. Optimal blood pressure target to prevent severe hypertension in pregnancy: a systematic review and meta-analysis. Hypertens Res. 2022;45:887–99.
Mulder EG, Ghossein-Doha C, Cauffman E, Lopes van Balen VA, Schiffer V, Alers RJ, et al. Preventing recurrent preeclampsia by tailored treatment of nonphysiologic hemodynamic adjustments to pregnancy. Hypertension. 2021;77:2045–53.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Ishikawa T, Obara T, Nishigori H, Miyakoda K, Ishikuro M, Metoki H, et al. Antihypertensives prescribed for pregnant women in Japan: prevalence and timing determined from a database of health insurance claims. Pharmacoepidemiol Drug Saf. 2018;27:1325–34.
Mito A, Murashima A, Wada Y, Miyasato-Isoda M, Kamiya CA, Waguri M, et al. Safety of amlodipine in early pregnancy. J Am Heart Assoc. 2019;8:e012093.
Pasker-de Jong PC, Zielhuis GA, van Gelder MM, Pellegrino A, Gabreels FJ, Eskes TK. Antihypertensive treatment during pregnancy and functional development at primary school age in a historical cohort study. BJOG. 2010;117:1080–6.
Pickering TG. Reflections in hypertension. How should blood pressure be measured during pregnancy? J Clin Hypertens. 2005;7:46–9.
Rey E, Morin F, Boudreault J, Pilon F, Vincent D, Ouellet D. Blood pressure assessments in different subtypes of hypertensive pregnant women: office versus home patient- or nurse-measured blood pressure. Hypertens Pregnancy. 2009;28:168–77.
Hurrell A, Webster L, Chappell LC, Shennan AH. The assessment of blood pressure in pregnant women: pitfalls and novel approaches. Am J Obstet Gynecol. 2021. https://doi.org/10.1016/j.ajog.2020.10.026.
de Haas S, Mulder E, Schartmann N, Mohseni Z, Abo Hasson F, Alsadah F, et al. Blood pressure adjustments throughout healthy and hypertensive pregnancy: a systematic review and meta-analysis. Pregnancy Hypertens. 2022;27:51–8.
Metoki H, Ohkubo T, Watanabe Y, Nishimura M, Sato Y, Kawaguchi M, et al. Seasonal trends of blood pressure during pregnancy in Japan: the babies and their parents’ longitudinal observation in Suzuki Memorial Hospital in Intrauterine Period study. J Hypertens. 2008;26:2406–13.
Brown MA, Robinson A, Bowyer L, Buddle ML, Martin A, Hargood JL, et al. Ambulatory blood pressure monitoring in pregnancy: what is normal? Am J Obstet Gynecol. 1998;178:836–42.
Cugini P, Di Palma L, Battisti P, Leone G, Pachi A, Paesano R, et al. Describing and interpreting 24-hour blood pressure patterns in physiologic pregnancy. Am J Obstet Gynecol. 1992;166:54–60.
Brown MA, Mangos G, Davis G, Homer C. The natural history of white coat hypertension during pregnancy. BJOG. 2005;112:601–6.
Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D, et al. Call to action on use and reimbursement for home blood pressure monitoring: a joint scientific statement from the American Heart Association, American Society Of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension. 2008;52:10–29.
Parati G, Stergiou GS, Asmar R, Bilo G, de Leeuw P, Imai Y, et al. European Society of Hypertension guidelines for blood pressure monitoring at home: a summary report of the Second International Consensus Conference on Home Blood Pressure Monitoring. J Hypertens. 2008;26:1505–26.
Mikami Y, Takai Y, Era S, Ono Y, Saitoh M, Baba K, et al. Provisional criteria for the diagnosis of hypertension in pregnancy using home blood pressure measurements. Hypertens Res. 2017;40:679–84.
Tran K, Padwal R, Khan N, Wright MD, Chan WS. Home blood pressure monitoring in the diagnosis and treatment of hypertension in pregnancy: a systematic review and meta-analysis. CMAJ Open. 2021;9:E642–50.
Kalafat E, Benlioglu C, Thilaganathan B, Khalil A. Home blood pressure monitoring in the antenatal and postpartum period: A systematic review meta-analysis. Pregnancy Hypertens. 2020;19:44–51.
Ishikuro M, Obara T, Metoki H, Ohkubo T, Yamamoto M, Akutsu K, et al. Blood pressure measured in the clinic and at home during pregnancy among nulliparous and multiparous women: the BOSHI study. Am J Hypertens. 2013;26:141–8.
Ishikuro M, Obara T, Metoki H, Ohkubo T, Iwama N, Katagiri M, et al. Parity as a factor affecting the white-coat effect in pregnant women: the BOSHI study. Hypertens Res. 2015;38:770–5.
Vestgaard M, Asbjornsdottir B, Ringholm L, Andersen LLT, Jensen DM, Damm P, et al. White coat hypertension in early pregnancy in women with pre-existing diabetes: prevalence and pregnancy outcomes. Diabetologia. 2019;62:2188–99.
Salazar MR, Espeche WG, Balbin E, Leiva Sisnieguez CE, Leiva Sisnieguez BC, Stavile RN, et al. Office blood pressure values and the necessity of out-of-office measurements in high-risk pregnancies. J Hypertens. 2019;37:1838–44.
Salazar MR, Espeche WG, Leiva Sisnieguez BC, Balbin E, Leiva Sisnieguez CE, Stavile RN, et al. Significance of masked and nocturnal hypertension in normotensive women coursing a high-risk pregnancy. J Hypertens. 2016;34:2248–52.
Suzuki H, Takagi K, Tanaka K, Ichihara A, Seki H. A survey on the measurement of blood pressure in pregnant women and management of hypertensive disorders of pregnancy by the Japan Society for the Study of Hypertension in Pregnancy (JSSHP). Hypertens Res Pregnancy. 2021;9:30–9.
Usuzaki T, Ishikuro M, Metoki H, Murakami K, Noda A, Ueno F, et al. Comparison among research, home, and office blood pressure measurements for pregnant women: The TMM BirThree Cohort Study. J Clin Hypertens. 2020;22:2004–13.
Nash CM, Shetty N. Current state of affairs: a study regarding diagnosis, treatment and use of home blood pressure monitoring for hypertension in pregnancy. Pregnancy Hypertens. 2021;24:96–9.
Thomas NA, Drewry A, Racine Passmore S, Assad N, Hoppe KK. Patient perceptions, opinions and satisfaction of telehealth with remote blood pressure monitoring postpartum. BMC Pregnancy Childbirth. 2021;21:153.
Lanssens D, Vandenberk T, Lodewijckx J, Peeters T, Storms V, Thijs IM, et al. Midwives’, Obstetricians’, and recently delivered mothers’ perceptions of remote monitoring for prenatal care: retrospective survey. J Med Internet Res. 2019;21:e10887.
Fletcher B, Chappell LC, Lavallee L, Wilson HM, Stevens R, Mackillop L, et al. Changes to management of hypertension in pregnancy, and attitudes to self-management: an online survey of obstetricians, before and following the first wave of the COVID-19 pandemic. Pregnancy Hypertens. 2021;26:54–61.
Denolle T, Weber JL, Calvez C, Getin Y, Daniel JC, Lurton O, et al. Diagnosis of white coat hypertension in pregnant women with teletransmitted home blood pressure. Hypertens Pregnancy. 2008;27:305–13.
van den Heuvel JFM, Ayubi S, Franx A, Bekker MN. Home-based monitoring and telemonitoring of complicated pregnancies: Nationwide Cross-Sectional Survey of Current Practice in the Netherlands. JMIR Mhealth Uhealth. 2020;8:e18966.
Triebwasser JE, Janssen MK, Hirshberg A, Srinivas SK. Successful implementation of text-based blood pressure monitoring for postpartum hypertension. Pregnancy Hypertens. 2020;22:156–9.
Vandenberk T, Storms V, Lanssens D, De Canniere H, Smeets CJ, Thijs IM, et al. A vendor-independent mobile health monitoring platform for digital health studies: development and usability study. JMIR Mhealth Uhealth. 2019;7:e12586.
Muijsers HEC, van der Heijden OWH, de Boer K, van Bijsterveldt C, Buijs C, Pagels J, et al. Blood pressure after PREeclampsia/HELLP by SELF monitoring (BP-PRESELF): rationale and design of a multicenter randomized controlled trial. BMC Womens Health. 2020;20:41.
Acknowledgements
All authors have significantly contributed to and agree with the content of the manuscript. We would like to thank Editage (www.editage.com) for English language editing.
Funding
This study was supported by Grants for Scientific Research [16H05243, 19H03905, 10632242, 19K18659] from the Ministry of Education, Culture, Sports, Science, and Technology of Japan; the Japan Agency for Medical Research and Development (AMED) Birthday [grant number: JP21gk0110039]; and a Grant-in-Aid (19DA1001) from the Ministry of Health, Labor and Welfare, Health Research on Children, Youth and Families, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
HM concurrently holds the noncompensated subdirectorship at the Tohoku Institute for Management of Blood Pressure, which is supported by Omron Health Care Co. Ltd., and is involved in collaborative research with Omron Health Care in another study. HM has also received grants or scholarships from Academic Contributions from Pfizer Japan Inc., Astellas Research Support, Daiichi Sankyo Co. Ltd., Bayer Academic Support, Otsuka Pharmaceutical Co., Ltd, Takeda Research Support, Eli Lilly Japan K.K., Baxter Co., Ltd., Mitsubishi Tanabe Pharma Corporation, Chugai Pharmaceutical Co., Ltd., and Teijin Pharma Limited. These companies were not involved in this review article.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Metoki, H., Iwama, N., Hamada, H. et al. Hypertensive disorders of pregnancy: definition, management, and out-of-office blood pressure measurement. Hypertens Res 45, 1298–1309 (2022). https://doi.org/10.1038/s41440-022-00965-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-00965-6
Keywords
This article is cited by
-
Hypertensive disorders of pregnancy and the risk of dementia: a systematic review and meta-analysis of cohort studies
Hypertension Research (2024)
-
Self-management system for postpartum women with hypertension disorders: an eHealth application intervention study
BMC Pregnancy and Childbirth (2023)
-
Effective gestational weight gain advice to optimize infant birth weight in Japan based on quantile regression analysis
Scientific Reports (2023)
-
Preeclampsia up to date—What’s going on?
Hypertension Research (2023)
-
Association of hypertension in pregnancy with serum electrolyte disorders in late pregnancy among Cameroonian women
Scientific Reports (2023)