Abstract
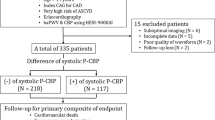
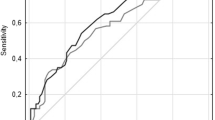
Various types of blood pressure (BP) variability have been recognized as risk factors for future cardiovascular events. However, the prognostic impact of in-hospital BP variability in patients with symptomatic peripheral arterial disease (PAD) has not yet been thoroughly investigated. A total of 386 patients with PAD who underwent endovascular therapy in two hospitals were retrospectively included. BP variability was assessed by the coefficient of variation (CV) of systolic BP measured during hospitalization by trained nurses. The primary endpoint was a composite of major adverse cardiovascular events (cardiovascular death, acute coronary syndrome, stroke, and hospitalization for heart failure) and major adverse limb events (major amputation, acute limb ischemia, and surgical limb revascularization). The mean systolic BP and the CV of systolic BP during hospitalization were 130.8 ± 15.7 mmHg and 11.2 ± 4.1%, respectively. During the median follow-up period of 22 months, 80 patients (21%) reached the primary endpoint. Receiver operating characteristic curve analysis showed that the CV of systolic BP significantly predicted major adverse cardiovascular and limb events (area under the curve 0.60, best cutoff value 9.8, P = 0.01). Using the best cutoff value, patients with high BP variability (n = 242) had a higher risk of clinical events than those with low BP variability (n = 144) (26% vs. 12%, P < 0.001). Multivariable analysis indicated that the CV of systolic BP, age, hemodialysis, and atrial fibrillation were associated with the primary endpoint. In conclusion, greater in-hospital systolic BP variability was associated with major adverse cardiovascular and limb events in patients with symptomatic PAD undergoing endovascular therapy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Fowkes FGR, Rudan D, Rudan I, Aboyans V, Denenberg JO, McDermott MM, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet. 2013;382:1329–40.
Reinecke H, Unrath M, Freisinger E, Bunzemeier H, Meyborg M, Lüders F, et al. Peripheral arterial disease and critical limb ischaemia: still poor outcomes and lack of guideline adherence. Eur Heart J. 2015;36:932–8.
Steg PG, Bhatt DL, Wilson PWF, D’Agostino R, Ohman EM, Röther J, et al. One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA. 2007;297:1197–206.
Feringa HHH, Bax JJ, Hoeks S, van Waning VH, Elhendy A, Karagiannis S, et al. A prognostic risk index for long-term mortality in patients with peripheral arterial disease. Arch Intern Med. 2007;167:2482–9.
Sprengers RW, Janssen KJM, Moll FL, Verhaar MC, van der Graaf Y. SMART Study Group. Prediction rule for cardiovascular events and mortality in peripheral arterial disease patients: data from the prospective Second Manifestations of ARTerial disease (SMART) cohort study. J Vasc Surg. 2009;50:1369–76.
Kumakura H, Kanai H, Aizaki M, Mitsui K, Araki Y, Kasama S, et al. The influence of the obesity paradox and chronic kidney disease on long-term survival in a Japanese cohort with peripheral arterial disease. J Vasc Surg. 2010;52:110–7.
Mueller T, Hinterreiter F, Luft C, Poelz W, Haltmayer M, Dieplinger B. Mortality rates and mortality predictors in patients with symptomatic peripheral artery disease stratified according to age and diabetes. J Vasc Surg. 2014;59:1291–9.
Rapsomaniki E, Timmis A, George J, Pujades-Rodriguez M, Shah AD, Denaxas S, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet. 2014;383:1899–911.
Stevens SL, Wood S, Koshiaris C, Law K, Glasziou P, Stevens RJ, et al. Blood pressure variability and cardiovascular disease: systematic review and meta-analysis. BMJ. 2016;354:i4098.
Parati G, Stergiou GS, Dolan E, Bilo G. Blood pressure variability: clinical relevance and application. J Clin Hypertens (Greenwich). 2018;20:1133–7.
Fukuda K, Kai H, Kamouchi M, Hata J, Ago T, Nakane H, et al. Day-by-Day Blood Pressure Variability and Functional Outcome After Acute Ischemic Stroke. Stroke. 2015;46:1832–9.
Hassan AKM, Rahman HA-E, Mohsen K, Dimitry SR. Impact of in-hospital blood pressure variability on cardiovascular outcomes in patients with acute coronary syndrome. J Clin Hypertens (Greenwich). 2017;19:1252–9.
Saito K, Saito Y, Kitahara H, Nakayama T, Fujimoto Y, Kobayashi Y. In-Hospital Blood Pressure Variability: A Novel Prognostic Marker of Renal Function Decline and Cardiovascular Events in Patients with Coronary Artery Disease. Kidney Blood Press Res. 2020;45:748–57.
Yanagiuchi T, Kato T, Hiroe T, Yabuta J, Hanabusa K, Ota Y, et al. A model for predicting the time of early symptomatic restenosis after infrapopliteal angioplasty in patients with critical limb ischemia. Cardiovasc Interv Ther. 2020. https://doi.org/10.1007/s12928-020-00691-1.
Shimada T, Habara S, Tanaka H, Kadota K. Plaque volume reduction after drug-coated balloon angioplasty for superficial femoral artery lesion. Cardiovasc Interv Ther. 2020. https://doi.org/10.1007/s12928-020-00672-4.
Higashitani M, Anzai H, Mizuno A, Utsunomiya M, Umemoto T, Yamanaka T, et al. One-year limb outcome and mortality in patients undergoing revascularization therapy for acute limb ischemia: short-term results of the Edo registry. Cardiovasc Interv Ther. 2020. https://doi.org/10.1007/s12928-020-00662-6.
Nakao M, Yamaguchi J, Otsuki H, Arashi H, Hagiwara N. Clinical outcomes of high-pressure balloon angioplasty for common femoral artery disease in contemporary practice. Cardiovasc Inter Ther. 2019;34:340–4.
Aboyans V, Ricco J-B, Bartelink M-LEL, Björck M, Brodmann M, Cohnert T, et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018;39:763–816.
Parati G, Ochoa JE, Lombardi C, Bilo G. Assessment and management of blood-pressure variability. Nat Rev Cardiol. 2013;10:143–55.
Garcia-Garcia HM, McFadden EP, Farb A, Mehran R, Stone GW, Spertus J, et al. Standardized end point definitions for coronary intervention trials: the Academic Research Consortium-2 consensus document. Circulation. 2018;137:2635–50.
Emdin CA, Anderson SG, Callender T, Conrad N, Salimi-Khorshidi G, Mohseni H, et al. Usual blood pressure, peripheral arterial disease, and vascular risk: cohort study of 4.2 million adults. BMJ. 2015;351:h4865.
Yeh C-H, Yu H-C, Huang T-Y, Huang P-F, Wang Y-C, Chen T-P, et al. High Systolic and Diastolic Blood Pressure Variability Is Correlated with the Occurrence of Peripheral Arterial Disease in the First Decade following a Diagnosis of Type 2 Diabetes Mellitus: a New Biomarker from Old Measurement. Biomed Res Int. 2016;2016:9872945.
Brennan MB, Guihan M, Budiman-Mak E, Kang H, Lobo JM, Sutherland BL, et al. Increasing SBP variability is associated with an increased risk of developing incident diabetic foot ulcers. J Hypertens. 2018;36:2177–84.
Rothwell PM, Howard SC, Dolan E, O’Brien E, Dobson JE, Dahlöf B, et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet. 2010;375:895–905.
Gosmanova EO, Mikkelsen MK, Molnar MZ, Lu JL, Yessayan LT, Kalantar-Zadeh K, et al. Association of Systolic Blood Pressure Variability with Mortality, Coronary Heart Disease, Stroke, and Renal Disease. J Am Coll Cardiol. 2016;68:1375–86.
Mancia G, Facchetti R, Parati G, Zanchetti A. Visit-to-visit blood pressure variability in the European Lacidipine Study on Atherosclerosis: methodological aspects and effects of antihypertensive treatment. J Hypertens. 2012;30:1241–51.
Rothwell PM, Howard SC, Dolan E, O’Brien E, Dobson JE, Dahlöf B,P, et al. Effects of β blockers and calcium-channel blockers on within-individual variability in blood pressure and risk of stroke. Lancet Neurol. 2010;9:469–80.
Muntner Paul ShimboDaichi, Tonelli Marcello ReynoldsKristi, Arnett Donna K, et al. The Relationship Between Visit-to-Visit Variability in Systolic Blood Pressure and All-Cause Mortality in the General Population. Hypertension. 2011;57:160–6.
Tsuchikura S, Shoji T, Kimoto E, Shinohara K, Hatsuda S, Koyama H, et al. Central versus peripheral arterial stiffness in association with coronary, cerebral and peripheral arterial disease. Atherosclerosis. 2010;211:480–5.
Zahner GJ, Gruendl MA, Spaulding KA, Schaller MS, Hills NK, Gasper WJ, et al. Association between arterial stiffness and peripheral artery disease as measured by radial artery tonometry. J Vasc Surg. 2017;66:1518–26.
Zhou Tan Lai, Henry Ronald MA, Stehouwer Coen DA, van Sloten Thomas T, Reesink Koen D, Kroon Abraham A. Blood Pressure Variability, Arterial Stiffness, and Arterial Remodeling. Hypertension. 2018;72:1002–10.
Alberts MJ, Bhatt DL, Mas J-L, Ohman EM, Hirsch AT, Röther J, et al. Three-year follow-up and event rates in the international REduction of Atherothrombosis for Continued Health Registry. Eur Heart J. 2009;30:2318–26.
Yang M, Pan X, Liang Z, Huang X, Duan M, Cai H, et al. Association between blood pressure variability and the short-term outcome in patients with acute spontaneous subarachnoid hemorrhage. Hypertens Res. 2019;42:1701–7.
Itoga NK, Tawfik DS, Lee CK, Maruyama S, Leeper NJ, Chang TI. Association of blood pressure measurements with peripheral arterial disease events: reanalysis of the ALLHAT data. Circulation. 2018;138:1805–14.
Lee SE, Lee H-Y, Cho H-J, Choe W-S, Kim H, Choi J-O, et al. Reverse J-Curve Relationship Between On-Treatment Blood Pressure and Mortality in Patients With Heart Failure. JACC Heart Fail. 2017;5:810–9.
Iida O, Takahara M, Soga Y, Suzuki K, Hirano K, Kawasaki D, et al. Shared and differential factors influencing restenosis following endovascular therapy between TASC (Trans-Atlantic Inter-Society Consensus) II class A to C and D lesions in the femoropopliteal artery. JACC Cardiovasc Inter. 2014;7:792–8.
Webb AJ, Rothwell PM. Effect of dose and combination of antihypertensives on interindividual blood pressure variability: a systematic review. Stroke. 2011;42:2860–5.
Lim HM, Chia YC, Ching SM, Chinna K. Number of blood pressure measurements needed to estimate long-term visit-to-visit systolic blood pressure variability for predicting cardiovascular risk: a 10-year retrospective cohort study in a primary care clinic in Malaysia. BMJ Open. 2019;9:e025322.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Suzuki, M., Saito, Y., Kitahara, H. et al. Impact of in-hospital blood pressure variability on clinical outcomes in patients with symptomatic peripheral arterial disease. Hypertens Res 44, 1002–1008 (2021). https://doi.org/10.1038/s41440-021-00648-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-021-00648-8