Abstract
The primary aldosteronism (PA) subtype is usually confirmed by CT and adrenal venous sampling (AVS). However, the subtype diagnosis by AVS is not necessarily consistent with the subtype diagnosis by CT. Patients with PA who show bilateral lesions (normal-appearing adrenals or bilateral adrenal nodules) on CT but unilateral disease on AVS are often found. The aim of this study was to evaluate whether patients with PA subtype discordance between CT and AVS obtain benefits from unilateral adrenalectomy. We retrospectively analyzed 362 consecutive patients with PA who underwent both CT and adrenocorticotropic hormone-unstimulated AVS at Kanazawa University Hospital. Surgical outcomes for unilateral PA were evaluated according to the criteria of the Primary Aldosteronism Surgical Outcome study. In our study, the success rate of AVS in patients with bilateral lesions on CT was 89% (191/214). Furthermore, the discordance rate between CT and AVS in patients with bilateral lesions on CT was 39% (74/191). After surgery, patients with bilateral lesions on CT but unilateral disease on AVS (n = 17) had a lower complete biochemical success rate than those with unilateral lesions on CT and ipsilateral disease on AVS (n = 30) (41% vs. 80%, p = 0.01), but clinical and biochemical benefits (the complete and partial success combined) were not significantly different between them (76% vs. 93% (p = 0.11) and 70% vs. 90% (p = 0.10), respectively). In conclusion, patients with bilateral lesions on CT but unilateral disease on AVS benefited from surgery, and AVS should be performed for patients who pursue surgical management when the CT findings suggest bilateral lesions.
Similar content being viewed by others
Introduction
Primary aldosteronism (PA) is a major form of secondary hypertension. PA should be diagnosed and treated appropriately because patients with PA have a higher incidence of cardiovascular complications than those with essential hypertension [1]. PA is classified into two subtypes: unilateral disease [aldosterone producing adenoma (APA), unilateral adrenal hyperplasia (UAH), and unilateral multiple adrenocortical micronodules (UMN)] and bilateral disease [idiopathic adrenal hyperplasia (IHA)]. Subtype classification is important for identifying patients with unilateral PA who can be cured by unilateral adrenalectomy. The PA subtype is usually confirmed by adrenal CT and adrenal venous sampling (AVS). CT is a minimally invasive procedure, but it does not always accurately diagnose PA subtype [1]. Indeed, some patients with a unilateral adrenal nodule on CT have bilateral disease on AVS. Other patients with bilateral lesions (normal-appearing adrenals or bilateral adrenal nodules) on CT demonstrate unilateral disease on AVS. Therefore, the clinical guidelines indicate that AVS, performed by an experienced radiologist, is the gold standard test to differentiate unilateral from bilateral PA [2]. Despite the risk of misclassification by CT, a recent prospective randomized study showed that there were no differences between CT vs. AVS-based treatment in the intensity of antihypertensive medication or clinical benefits for patients after one year of follow-up [3]. These findings highlighted a problem for the current guidelines and recommendations.
In our center, both CT and AVS have been performed for patients with PA who pursue surgical management. We often encounter cases in which CT findings suggest bilateral PA, but AVS results suggest unilateral PA. However, few studies have focused on patients with PA who undergo unilateral adrenalectomy, despite a discrepancy in CT vs. AVS subtype diagnosis. Therefore, we evaluated the pre- and postoperative clinical and biochemical features of patients with PA who showed bilateral lesions on CT but unilateral disease on AVS (CT vs. AVS discordant group) and assessed whether these patients obtain clinical benefits from surgery.
Methods
Patients
We retrospectively analyzed 362 consecutive patients with PA who underwent both adrenal CT and AVS between January 2005 and January 2016 at Kanazawa University Hospital (Fig. 1). First, the patients were divided into two groups (bilateral lesions or unilateral lesions) based on CT findings. Bilateral lesions on CT consisted of normal-appearing adrenals and bilateral adrenal nodules. Second, the patients were classified as having unilateral or bilateral disease based on bilateral adrenocorticotropic hormone (ACTH)-unstimulated AVS results. In addition, we examined concordance or discordance between PA subtypes based on CT vs. AVS results. The CT and AVS subtypes were judged to be concordant when the CT showed a unilateral adrenal nodule and AVS lateralized to the same side or when the CT showed either normal-appearing adrenals or bilateral adrenal nodules and AVS confirmed bilateral disease. Finally, the patients with PA who underwent unilateral adrenalectomy on the basis of AVS results were divided into the CT vs. AVS discordant group (bilateral lesions on CT but unilateral disease on AVS) and the CT vs. AVS concordant group (unilateral lesion on CT and ipsilateral disease on AVS). We then evaluated the pre- and postoperative clinical and biochemical characteristics of both groups.
Before screening, all patients were evaluated after discontinuing all antihypertensive drugs, except for calcium channel blockers and alpha adrenergic blockers, for 2 weeks, or for 6 weeks if using spironolactone and eplerenone. A plasma aldosterone concentration (pg/mL) to plasma renin activity (ng/mL/h) ratio > 200 was used to screen for PA. The diagnosis of PA was confirmed by the captopril challenge test, the furosemide plus upright test, and/or the saline infusion test according to the guidelines published by the Japanese Society of Hypertension (JSH) 2014 [4]. A dexamethasone suppression test was performed to exclude Cushing’s syndrome. Antihypertensive medications were converted to a standardized daily defined dose (DDD) according to the WHO ATC/DDD Index 2010. Preoperative blood pressure (BP) and antihypertensive medication intake were evaluated at the outpatient clinic before undergoing AVS. Clinical and biochemical outcomes were assessed at 6–12 months after surgery using the criteria of the Primary Aldosteronism Surgical Outcome (PASO) study [5]. The outcome categories are shown in Supplementary Table 1 (complete, partial, and absent success). Clinical and biochemical benefits were defined as the complete and partial success categories combined. Unilateral adrenalectomy was performed at Kanazawa University Hospital or Houju Memorial Hospital for patients with unilateral PA diagnosed by AVS.
Adrenal computed tomography
CT scans (Light Speed Ultra 16 or Light Speed VCT; General Electric Healthcare, Milwaukee, WI, USA) of the adrenal glands with contiguous 2.5 mm cuts were performed in all patients with PA before undergoing AVS. Radiological diagnosticians approved by the Japan Radiological Society confirmed the presence of adrenal nodules and categorized the imaging results as normal-appearing adrenals, bilateral adrenal nodules, or unilateral adrenal nodules.
Adrenal venous sampling technique and criteria
We performed ACTH-unstimulated simultaneous bilateral AVS in the morning. A semiquantitative quick cortisol assay was used to increase the AVS success rate between 2011 and 2014 as described previously [6]. The criterion for successful selective catheterization was the ratio of adrenal vein to inferior vena cava cortisol concentrations (i.e., selectivity index >2 [2]). Unilateral aldosterone overproduction was confirmed by calculating the ipsilateral adrenal vein aldosterone-to-cortisol concentration ratio divided by the contralateral aldosterone-to-cortisol ratio (i.e., lateralized index ≥2 [7, 8]). The contralateral ratio (defined as the ratio of plasma aldosterone to cortisol in the nondominant side to that in the inferior vena cava) was also evaluated.
Statistical analysis and ethics
Continuous variables were expressed as medians (25th-75th percentile) for parameters with a nonnormal distribution. Categorical variables are presented as numbers and percentages. Comparisons between two independent groups were performed using the Mann–Whitney U-test, and comparisons between two related groups were performed using the Wilcoxon signed-rank test for continuous variables. Comparisons between two independent groups were performed using Fisher’s exact probability test for categorical variables. A P value <0.05 was considered significant. All statistical analyses were performed using Excel 2016 (Microsoft, Seattle, WA, USA) with the add-in software Statcel4 (OMS, Tokyo, Japan). This clinical study was approved by the ethics committees of Kanazawa University (no.2015121) and Houju Memorial Hospital (no.18–12).
Results
CT versus AVS discordant group
Of the 362 patients with PA, 214 had bilateral lesions (i.e., 190 with normal-appearing adrenals and 24 with bilateral adrenal nodules) and 148 had unilateral lesions on CT (Fig. 1). ACTH-unstimulated AVS was successfully performed in 167/190 (88%) patients with normal-appearing adrenals, 24/24 (100%) patients with bilateral adrenal nodules, and 126/148 (85%) patients with unilateral adrenal nodules on CT. Unilateral disease was observed on AVS in 60/167 (36%) patients with normal-appearing adrenals and 14/24 (17%) patients with bilateral adrenal nodules on CT (CT vs. AVS discordant group), whereas 52/126 (41%) patients with a unilateral adrenal nodule on CT demonstrated ipsilateral disease on AVS (CT vs. AVS concordant group). On the basis of the AVS results, unilateral adrenalectomy was performed in 14/60 patients with normal-appearing adrenals on CT but unilateral disease on AVS, 4/14 patients with bilateral adrenal nodules on CT but unilateral disease on AVS (CT vs. AVS discordant group undergoing surgery), and 32/52 patients with unilateral disease on CT and ipsilateral disease on AVS (CT vs. AVS concordant group undergoing surgery).
Proportion of adrenal CT results concordant or discordant with the AVS results
ACTH-unstimulated AVS was successfully performed in 191 patients with bilateral and 126 patients with unilateral lesions on CT (Fig. 1). The rates of concordance between CT and AVS in the former and the latter group were 61% (117/191) and 41% (52/126), respectively (Supplementary Fig. 1). In total, the PA subtype concordance rate between CT and AVS was 53% (169/317).
Baseline characteristics of the CT versus AVS discordant group
Among the patients with bilateral lesions on CT, we examined differences in baseline clinical and biochemical characteristics between those with unilateral disease on AVS (CT vs. AVS discordant group) and those with bilateral disease on AVS. The former and the latter groups consisted of 74 patients (60 with normal-appearing adrenals and 14 with bilateral adrenal nodules on CT) and 117 patients (107 with normal-appearing adrenals and 10 with bilateral adrenal nodules on CT), respectively (Fig. 1). Patients with unilateral disease on AVS had significantly higher plasma aldosterone concentrations than those with bilateral disease on AVS (p = 0.04) (Table 1).
We next divided the group with bilateral lesions on CT into the normal-appearing adrenal group and the bilateral adrenal nodule group and conducted a similar analysis in the respective groups (Supplementary Table 2). In the group with normal-appearing adrenals on CT, there were no differences between patients with unilateral disease (n = 60) and those with bilateral disease (n = 107) on AVS. In the group with bilateral adrenal nodules on CT, patients with unilateral disease on AVS (n = 14) had a higher body mass index (p = 0.01) and lower serum potassium (p = 0.04) than those with bilateral disease (n = 10).
Pre- and postoperative evaluation of the CT versus AVS discordant group undergoing surgery
We compared the pre- and postoperative clinical and biochemical characteristics of the patients in the CT vs. AVS discordant group undergoing surgery with those in the CT vs. AVS concordant group undergoing surgery (Fig. 2). As shown in Fig. 1, the CT vs. AVS discordant group undergoing surgery and the CT vs. AVS concordant group undergoing surgery consisted of 18 patients (14 with normal-appearing adrenals and 4 with bilateral adrenal nodules on CT) and 32 patients, respectively. Of these patients, 1/18 (1/3 bilateral adrenal nodules on CT) and 2/32 were excluded from this analysis. One patient underwent surgery at an outside hospital, and postoperative clinical information was unavailable for the other two patients. Therefore, the CT vs. AVS discordant group undergoing surgery consisted of 17 patients, and the CT vs. AVS concordant group undergoing surgery consisted of 30 patients. On preoperative evaluation, the systolic and diastolic blood pressure, number of antihypertensive medications, plasma renin activity, and aldosterone-to-renin ratio did not differ between the two groups. However, the CT vs. AVS concordant group undergoing surgery had significantly higher plasma aldosterone concentrations (p = 0.02) and lower serum potassium levels (p = 0.02) than those of the CT vs. AVS discordant group undergoing surgery. On postoperative evaluation, the systolic and diastolic blood pressure, plasma aldosterone concentration, plasma renin activity, aldosterone-to-renin ratio, and serum potassium levels were significantly improved in both groups. However, the CT vs. AVS discordant group undergoing surgery had a significantly higher aldosterone-to-renin ratio than that of the CT vs. AVS concordant group undergoing surgery (p = 0.03).
Pre- and postoperative evaluation of the CT vs. AVS discordant group undergoing surgery. Discordant, CT vs. AVS discordant group undergoing surgery. Concordant, CT vs. AVS concordant group undergoing surgery; pre, preoperation; post, postoperation. a SBP, Systolic blood pressure. b DBP, Diastolic blood pressure. c Number of anti-hypertension medications. d PAC, Plasma aldosterone concentration. e PRA, Plasma renin activity. f ARR, Aldosterone-to-renin ratio. g Serum potassium. The data are shown as box plots, were analyzed using the Wilcoxon signed-rank test before and after surgery and were compared between the two groups using the Mann–Whitney U-test. *p < 0.05, †p < 0.01, ‡p < 0.001 compared with preoperation. p < 0.05 vs. the CT vs. AVS concordant group undergoing surgery
In the CT vs. AVS discordant group undergoing surgery, we focused on 14 patients with PA who had normal-appearing adrenals on CT but unilateral disease on AVS and underwent unilaterally adrenalectomy (CT-normal and AVS-unilateral group undergoing surgery). The small number of patients with PA who showed bilateral adrenal nodules on CT and unilateral disease on AVS and underwent surgery (n = 3) could not be analyzed statistically. We compared the pre- and postoperative clinical and biochemical characteristics of the CT-normal and AVS-unilateral group undergoing surgery with those of the CT vs. AVS concordant group undergoing surgery (Supplementary Fig. 2). On preoperative evaluation, the systolic blood pressure, number of antihypertensive medications, plasma renin activity, and aldosterone-to-renin ratio did not differ between the two groups. However, the CT vs. AVS concordant group undergoing surgery had significantly higher diastolic blood pressure (p = 0.03) and plasma aldosterone concentration (p = 0.04) and lower serum potassium levels (p = 0.02) than those of the CT-normal and AVS-unilateral group undergoing surgery. On postoperative evaluation, the systolic and diastolic blood pressure, plasma aldosterone concentration, plasma renin activity, aldosterone-to-renin ratio, and serum potassium levels were significantly improved in the CT-normal and AVS-unilateral group undergoing surgery. However, the CT-normal and AVS-unilateral group undergoing surgery had a significantly higher aldosterone-to-renin ratio than the CT vs. AVS concordant group undergoing surgery (p = 0.03).
Remission rates for clinical and biochemical outcomes in the CT versus AVS discordant group according to the criteria of the PASO study
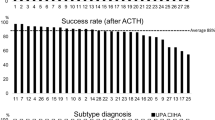
Remission rates for clinical and biochemical outcomes in the CT vs. AVS discordant and concordant groups were evaluated according to the criteria of the PASO study (Fig. 3). Complete clinical success was achieved in 35% (6/17) of the discordant group and 50% (15/30) of the concordant group, and partial clinical success was achieved in 41% (7/17) of the discordant group and 43% (13/30) of the concordant group. There were no differences in the complete clinical success rates (35% vs. 50%, p = 0.25) and the complete and partial clinical success rates combined (clinical benefit) between the two groups (76% vs. 93%, p = 0.11). Complete biochemical success was achieved in 41% (7/17) of the discordant group and 80% (24/30) of the concordant group, and partial clinical success was achieved in 29% (5/17) of the discordant group and 10% (3/30) of the concordant group. The discordant group had a lower complete biochemical success rate than that of the concordant group (41% vs. 80%, p = 0.01), but there were no differences in complete and partial biochemical success rates combined (biochemical benefit) between the two groups (71% vs. 90%, p = 0.10).
Remission rates for clinical and biochemical outcomes in the CT vs. AVS discordant group according to the criteria of the Primary Aldosteronism Surgical Outcome (PASO) study. The data were compared between the two groups using Fisher’s exact probability test. *p < 0.05 compared with the CT vs. AVS concordant group undergoing surgery
We next divided the CT vs. AVS discordant group into patients with normal-appearing adrenals vs. those with bilateral adrenal nodules on CT and evaluated the remission rates for clinical and biochemical outcomes, respectively (Supplementary Fig. 3). Patients with normal-appearing adrenals on CT and unilateral disease on AVS (CT-normal and AVS-unilateral group) showed similar findings to the CT vs. AVS discordant group.
Discussion
Our study showed that patients with bilateral lesions on CT but unilateral disease on AVS (CT vs. AVS discordant group) were different in preoperative characteristics from those with bilateral lesions on CT and bilateral disease on AVS and those with unilateral disease on CT and ipsilateral disease on AVS (CT vs. AVS concordant group). Moreover, we demonstrated that the CT vs. AVS discordant group undergoing surgery had a lower complete biochemical success rate than the CT vs. AVS concordant group undergoing surgery, but there were no significant differences in clinical and biochemical benefits (complete and partial success categories combined) between the two groups according to the criteria of the PASO study. To our knowledge, this study is the first to evaluate the pre- and postoperative features of the CT vs. AVS discordant group. The findings of the current study may be useful for deciding to perform AVS when clinicians encounter patients with bilateral PA on CT.
AVS was initially used to determine PA subtype classification in the 1960s [9]. Subsequently, CT was adopted as the primary method for distinguishing unilateral from bilateral adrenal abnormalities. However, CT is often inaccurate for PA subtype diagnosis. The sensitivity and specificity of CT for unilateral disease (78 and 75%, respectively) are inferior to those of AVS (95 and 100%, respectively) [10, 11]. Several retrospective studies have reported that the rate of concordance between CT and AVS is 31% [1], 53% [10], 54% [11], and 51% [12]. In the present study, the rate of concordance between CT and AVS was 53% (169/317) (Supplementary Fig. 1), which was in agreement with prior studies [1, 10,11,12]. If we determined the PA subtype based on only CT findings, 74 patients with bilateral lesions on CT but unilateral disease on AVS would have been excluded as candidates for surgery, and 74 patients with unilateral lesion on CT but contralateral or bilateral disease on AVS would have had inappropriate surgery (Supplementary Fig. 1). Although younger patients (<age 35 years) with hypokalemia, marked aldosterone excess, and unilateral adrenal lesions on adrenal CT may not need AVS before surgery [13], relying on CT alone can generally lead to misdiagnoses of the PA subtype.
Despite the risk of misclassification by CT, a randomized controlled trial was recently performed to compare the outcome of CT-based treatment with AVS-based treatment for ~200 patients with PA [3]. Although the rate of subtype concordance between CT and AVS was 50%, there were no differences in the intensity of antihypertensive medication after 1 year of follow-up between the 92 patients with CT-based treatment (46 patients underwent unilateral adrenalectomy and 46 received a mineralocorticoid receptor antagonist) and the 92 patients who received AVS-based treatment (46 patients underwent unilateral adrenalectomy and 46 received a mineralocorticoid receptor antagonist) [3]. More persistent PA was observed in the CT-diagnosed group than in the AVS-diagnosed group (20% vs. 10%, respectively) after surgery, but the difference was not statistically significant [3]. These findings highlighted a problem for the current recommendations. However, the rate of hypokalemia in this study was higher than that in previous epidemiological studies (68% vs. 9–37%) [14], causing a possible selection bias. In addition, surgery might be beneficial to some patients with unilateral lesions on CT and bilateral disease on AVS. Hypertension was cured in 6 out of 40 (15%) patients diagnosed with bilateral PA on AVS and underwent unilaterally adrenalectomy, and hypertension was improved in 8 out of 40 (20%) patients at final follow-up 12–144 (median, 56.4) months after surgery [15].
In the CT vs. AVS discordant group, we focused on patients with normal-appearing adrenals on CT but unilateral disease on AVS (CT-normal and AVS-unilateral group). A previous study reported that patients with PA who showed bilateral normal adrenals with normokalemia were weakly recommended to perform AVS because of the low rate of unilateral disease on AVS [16]. In our study, the prevalence of unilateral lesion on AVS was as follows: bilateral normal adrenals on CT with normokalemia, 36% (55/153); unilateral lesion on AVS, 36% (5/14); unilateral disease on CT with normokalemia, 29% (26/90); and unilateral disease on CT with hypokalemia, 72% (26/36) (Supplementary Fig. 4). Therefore, patients with bilateral normal adrenal on CT and normokalemia had a similar prevalence for unilateral disease on AVS as those with unilateral disease on CT and normokalemia and those with unilateral disease on CT and normokalemia. Generally, PA with normal-appearing adrenals on CT but unilateral disease on AVS includes aldosterone-producing microadenoma (APmicroA) [17, 18], UAH [19], and UMN [20]. Several studies have evaluated pre- and postoperative clinical characteristics for patients with APmicroA, whereas similar evaluations have not been performed for the small number of patients with UAH or UMN. Preoperative clinical findings for patients with APmicroA were significantly similar to those for patients with IHA but not to those for patients with aldosterone-producing macroadenoma (APmacroA) detected by CT [18]. In our study, there were no significant differences in baseline characteristics between the CT-normal and AVS-unilateral group (e.g., APmicroA) and normal-appearing adrenals on CT and bilateral disease on AVS (e.g., IHA) (Supplementary Table 2), but the CT-normal and AVS-unilateral group undergoing surgery had lower diastolic blood pressure and plasma aldosterone concentration and higher serum-potassium levels than the CT vs. AVS concordant group undergoing surgery (e.g., APmacroA) (Supplementary Fig. 2). Furthermore, patients with APmicroA had as great an improvement in blood pressure, plasma aldosterone concentration, and plasma renin activity as those with APmacroA after unilateral adrenalectomy [17, 18]. In a few patients with UAH [19] and UMN [20], surgery cured their hypertension and hyporeninemic hyperaldosteronism. On the other hand, the CT-normal and AVS-unilateral group undergoing surgery had a significantly higher aldosterone-to-renin ratio than the CT vs. AVS concordant group undergoing surgery (Supplementary Table 2), and the former had significantly lower complete biochemical success rates than the latter after surgery, although the former had complete clinical outcome success rates as high as those of the latter (Supplementary Fig. 3). Compared with the biochemical complete success rate of 83–100% in the PASO study [5], the biochemical complete success rate was quite low in the CT-normal and AVS-unilateral groups undergoing surgery. Therefore, the postoperative results in our study differed from the results of previous studies [17,18,19,20].
The reasons for lower complete biochemical success rates in the CT-normal and AVS-unilateral groups might be found in the criteria for lateralization and the use of ACTH in AVS. First, different criteria for the lateralization of AVS between institutions may cause a difference in subtype diagnosis. We used a lateralization index (LI) ≥2 in this study because it provided the best compromise between the sensitivity and false positive rates for the lateralization of PA [7, 8]. However, a lateralized index > 4 [21], a contralateral ratio <1 and an ipsilateral ratio (defined as aldosterone to cortisol ratio on the dominant side/aldosterone to cortisol on the inferior vena cava) >2 [22] have also been used as criteria for lateralization in ACTH-unstimulated AVS. Therefore, we analyzed the biochemical outcomes in the CT-normal and AVS-unilateral groups using these criteria (Supplementary Fig. 5). The CT-normal and AVS-unilateral group had a lower complete biochemical success rate than the CT vs. AVS concordant group using a lateralized index >4 (43% vs. 85%, p = 0.04), but there were no significant differences in the complete biochemical success rate between the two groups using a contralateral ratio <1 and an ipsilateral ratio >2 (57% vs. 90%, p = 0.08). Furthermore, it was difficult to compare the PASO study results with our results because both the LI < 4 and LI ≥ 4 groups in the PASO study included cases diagnosed with ACTH-unstimulated and ACTH-stimulated AVS. Second, ACTH stimulation might affect the lateralization in AVS. We previously reported that 75/158 (47%) patients with PA who underwent successful ACTH-unstimulated and stimulated AVS had diagnostic discrepancies between ACTH-unstimulated and stimulated AVS results, 70/75 (93%) patients changed from unilateral PA to bilateral PA after ACTH stimulation, and both the number and calculated area of aldosterone-producing cell clusters (APCCs) in APAs were significantly smaller in patients with unilateral PA on both ACTH-unstimulated and ACTH-stimulated AVS than in those who changed from unilateral to bilateral disease after ACTH stimulation [23]. Although we determined AVS lateralization based on ACTH-unstimulated AVS results in the present study, 5/14 patients with normal-appearing adrenals on CT but unilateral disease on ACTH-unstimulated AVS underwent not only ACTH-unstimulated AVS but also ACTH-stimulated AVS. Three out of five patients changed from unilateral to bilateral PA after ACTH stimulation when we used a lateralized index ≥4 as criteria for lateralization in ACTH-stimulated AVS. Therefore, patients with unilateral disease on unstimulated AVS who did not undergo ACTH-stimulated AVS might also show bilateral disease on ACTH-stimulated AVS and have a large number and calculated area of APCCs. The criteria for lateralization and diagnostic discrepancies by using ACTH needs to be further discussed.
The limitations of our study include the retrospective nature of the analysis and relatively small numbers of patients with bilateral lesions on CT but unilateral disease on AVS who received unilateral adrenalectomy (i.e., 14/60 in the normal-appearing adrenals group and 4/14 in the bilateral adrenal nodules group). First, 30/60 patients in the normal-appearing adrenal group underwent ACTH-stimulated AVS. After ACTH stimulation, 28/30 changed from unilateral to bilateral disease, and 2/30 showed ipsilateral disease. Twenty-six patients with subtype discrepancy before and after ACTH stimulation were treated with medication, while two patients with subtype discrepancy and two patients with subtype concordance underwent surgery. Of 30 patients in the normal-appearing adrenals group who underwent only ACTH-unstimulated AVS, 10 underwent surgery and 20 intended to take medication after AVS. Second, 6/14 patients in the bilateral adrenal nodule group underwent not only ACTH-unstimulated AVS but also ACTH-stimulated AVS. After ACTH stimulation, 4 and 1 patients changed from unilateral to bilateral disease and contra-unilateral disease, respectively. The other two patients showed ipsilateral disease. Five patients with subtype discrepancy were treated with medication and 2 patients with subtype concordance underwent surgery. Of the 8 patients in the bilateral adrenal nodules group who underwent only ACTH-unstimulated AVS, 2 underwent surgery, but 6 selected medications because they were worried about the risk of residual adrenal tumor enlargement after surgery. Finally, immunohistochemical staining and somatic gene mutation analysis have been developed for APA, UMN, and UAH [24]. Therefore, immunohistochemical staining and gene analyses need to be performed, particularly in the CT-normal and AVS-unilateral group.
In conclusion, the CT vs. AVS discordant group benefited from unilateral adrenalectomy. Therefore, AVS should be performed in patients with bilateral PA on CT who pursue surgical management.
References
Takeda Y, Karashima S, Yoneda T. Primary aldosteronism, diagnosis and treatment in Japan. Rev Endocr Metab Disord. 2011;12:21–25.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:1889–916.
Dekkers T, Prejbisz A, Kool LJS, Groenewoud HJMM, Velema M, Spiering W, et al. SPARTACUS Investigators. Adrenal vein sampling versus CT scan to determine treatment in primary aldosteronism: an outcome-based randomized diagnostic trial. Lancet Diabetes Endocrinol. 2016;4:739–46.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. Japanese Society of Hypertension Guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Williams TA, Lenders JWM, Mulatero P, Burrello J, Rottenkolber M, Adolf C, et al. Primary Aldosteronism Surgery Outcome (PASO) investigators. Outcomes after adrenalectomy for unilateral primary aldosteronism: an international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol. 2017;5:689–99.
Yoneda T, Karashima S, Kometani M, Usukura M, Demura M, Sanada J, et al. Impact of new quick gold nanoparticle-based cortisol assay during adrenal vein sampling for primary aldosteronism. J Clin Endocrinol Metab. 2016;101:2554–61.
Rossi GianPaolo, Sacchetto Alfredo, Chiesura-Corona Matteo, Toni RenzoDe, Gallina Michele, Feltrin GianPietro, et al. Identification of the etiology of primary aldosteronism with adrenal vein sampling in patients with equivocal computed tomography and magnetic resonance findings: results in 104 consecutive cases. J Clin Endocrinol Metab. 2001;86:1083–90.
Rossi GP, Auchus RJ, Brown M, Lenders JW, Naruse M, Plouin PF, et al. An expert consensus statement on use of adrenal vein sampling for the subtyping of primary aldosteronism. Hypertension. 2014;63:151–60.
Melby JC, Spark RF, Dale SL, Egdahl RH, Kahn PC. Diagnosis and localization of aldosterone-producing adenomas by adrenal-vein catheterization. N Engl J Med. 1967;277:1050–6.
Young WilliamF Jr, Stanson AnthonyW, Thompson GeoffreyB, Grant CliveS, Farley DavidR, van Heerden JonA. Role for adrenal venous sampling in primary aldosteronism. Surgery. 2004;136:1227–35.
Nwariaku FE, Miller BS, Auchus R, Holt S, Watumul L, Nesbitt S, et al. Primary hyperaldosteronism: effect of adrenal vein sampling on surgical outcome. Surgery. 2006;141:497–502.
Nanba AyaT, Nanba Kazutaka, Byrd JamesB, Shields JamesJ, Giordano ThomasJ, Miller BarbaraS, et al. Discordance between imaging and immunohistochemistry in unilateral primary aldosteronism. Clin Endocrinol. 2017;87:665–72.
Funder JohnW, Carey RobertM, Mantero Franco, Murad MHassan, Reincke Martin, Shibata Hirotaka, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101:1889–916.
Mulatero P, Stowasser M, Loh KC, Fardella CE, Gordon RD, Mosso L, et al. Increased diagnosis of primary aldosteronism, including surgically correctable forms, in centers from five continents. J Clin Endocrinol Metab. 2004;89:1045–50.
Sukor Norlela, Gordon RichardD, Ku YeeKim, Jones Mark, Stowasser Michael. Role of unilateral adrenalectomy in bilateral primary aldosteronism: A 22-year single center experience. J Clin Endocrinol Metab. 2009;94:2437–45.
Umakoshi Hironobu, Tsuiki Mika, Takeda Yoshiyu, Kurihara Isao, Itoh Hiroshi, Katabami Takuyuki, et al. Significance of computed tomography and serum potassium in predicting subtype diagnosis of primary aldosteronism. J Clin Endocrinol Metab. 2018;103:900–8. JPAS Study Group
Karashima Shigehiro, Takeda Yoshiyu, Cheng Yuan, Yoneda Takashi, Demura Masashi, Kometani Mitsuhiro, et al. Clinical characteristics of primary hyperaldosteronism due to adrenal microadenoma. Steroids. 2011;76:1363–6.
Omura Masao, Sasano Hironobu, Saito Jun, Yamaguchi Kunio, Kakuta Yukio, Nishikawa Tetsuo. Clinical characteristics of aldosterone-producing microadenoma, macroadenoma, and idiopathic hyperaldosteronism in 93 patients with primary aldosteronism. Hypertens Res. 2006;29:883–9.
Iacobone M, Citton M, Viel G, Boetto R, Bonadio I, Tropea S, et al. Unilateral adrenal hyperplasia: a novel cause of surgically correctable primary hyperaldosteronism. Surgery. 2012;152:1248–55.
Omura M, Sasano H, Fujiwara T, Yamaguchi K, Nishikawa T. Unique case of unilateral hyperaldosteronemia due to multiple adrenocortical micronodules, which can only be detected by selective adrenal venous sampling. Metabolism. 2002;51:350–5.
Monticone S, Satoh F, Viola A, Fischer E, Vonend O, Bernini G, et al. Aldosterone suppression on contralateral adrenal during adrenal vein sampling does not predict blood pressure response after adrenalectomy. J Clin Endocrinol Metab. 2014 Nov;99:4158–66.
Stowasser Michael, Gordon RichardD, Rutherford JohnC, Nikwan NikZ, Daunt Nicholas, Slater GregoryJ. Diagnosis and management of primary aldosteronism. J Renin Angiotensin Aldosterone Syst. 2001;2:156–69.
Kometani M, Yoneda T, Aono D, Karashima S, Demura M, Nishimoto K, et al. Impact of aldosterone-producing cell clusters on diagnostic discrepancies in primary aldosteronism. Oncotarget. 2018;9:26007–18.
Yamazaki Yuto, Nakamura Yasuhiro, Omata Kei, Ise Kazue, Tezuka Yuta, Ono Yoshikiyo, et al. Histopathological Classification of Cross-Sectional Image–Negative Hyperaldosteronism. J Clin Endocrinol Metab. 2017;102:1182–92.
Acknowledgements
We would like to thank Drs. Ayako Wakayama and Yohei Toyoda (Houju Memorial Hospital) for providing pre- and postoperative data.
Funding
This study was supported by the Japan Society for the Promotion of Science Grant (Grant Number 25461244 to Y.T.) and Health Labor Sciences Research Grant (Number 201324012B to Y.T.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aono, D., Kometani, M., Karashima, S. et al. Primary aldosteronism subtype discordance between computed tomography and adrenal venous sampling. Hypertens Res 42, 1942–1950 (2019). https://doi.org/10.1038/s41440-019-0310-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0310-y
Keywords
This article is cited by
-
Diagnostic performance of the adrenal vein to inferior vena cava aldosterone ratio in classifying the subtype of primary aldosteronism
Hypertension Research (2023)
-
Diagnosis and management of primary hyperaldosteronism in patients with hypertension: a practical approach endorsed by the British and Irish Hypertension Society
Journal of Human Hypertension (2023)
-
Advances in the molecular imaging of primary aldosteronism
Annals of Nuclear Medicine (2023)
-
Key to the Treatment of Primary Aldosteronism in Secondary Hypertension: Subtype Diagnosis
Current Hypertension Reports (2023)
-
Left adrenal aldosteronism coexisting with left paraaortic paraganglioma presenting as bilateral adrenal and left paraaortic tumors– comprehensive adrenal evaluation aiding perfect management: a case report
BMC Endocrine Disorders (2022)