Abstract
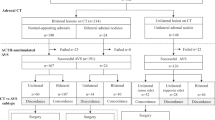
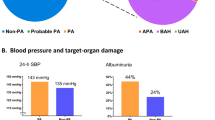
Primary aldosteronism (PA) is a common curable cause of hypertension. Adrenal venous sampling (AVS) is recommended for subtype diagnosis but is a difficult procedure. Recently, an increased prevalence of PA was reported, creating a greater demand for treatment of the condition in clinical facilities. The aim of the present study was to identify the historical changes over time and the differences between facilities in the success rate and subtype diagnosis of PA. The database of the PA registry developed by the Japan PA Study (JPAS) was used. A total of 2599 patients with PA who underwent AVS were evaluated. The overall success rate of AVS was 88%. The bilateral subtype was the dominant subtype, comprising 69% of cases. During the period 2004−2011 to 2011−2017, there were significant changes in the total number of AVS procedures (from 562 to 1732), ratio of ACTH administration with AVS (75 to 97%), success rate (79 to 90%), and proportion with bilateral subtype diagnosis (53 to 72%). There were also significant inter-facility differences in the number of AVS procedures (6 to 322), success rate (59 to 97%), and proportion with the bilateral subtype (44 to 86%). The principal enrolled department was Endocrinology (86%), and the ratio of unilateral PA was significantly higher in this department than in others (32% vs. 25%). In conclusion, the number of AVS procedures performed, the success rate, and the proportion with the bilateral subtype increased over time after normalizing the centre difference. Significant differences were observed between the centres.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Rossi GP, Bernini G, Caliumi C, Desideri G, Fabris B, Ferri C, et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol. 2006;48:2293–300.
Monticone S, Burrello J, Tizzani D, Bertello C, Viola A, Buffolo F, et al. Prevalence and clinical manifestations of primary aldosteronism encountered in primary care practice. J Am Coll Cardiol. 2017;69:1811–20.
Funder JW, Carey RM, Fardella C, Gomez-Sanchez CE, Mantero F, Stowasser M, et al. Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2008;93:3266–81.
Mulatero P, Stowasser M, Loh KC, Fardella CE, Gordon RD, Mosso L, et al. Increased diagnosis of primary aldosteronism, including surgically correctable forms, in centers from five continents. J Clin Endocrinol Metab. 2004;89:1045–50.
Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol. 2005;45:1243–8.
Savard S, Amar L, Plouin PF, Steichen O. Cardiovascular complications associated with primary aldosteronism: a controlled cross-sectional study. Hypertension. 2013;62:331–6.
Lim PO, Young WF, MacDonald TM. A review of the medical treatment of primary aldosteronism. J Hypertens. 2001;19:353–61.
Young WF Jr. Minireview: primary aldosteronism—changing concepts in diagnosis and treatment. Endocrinology. 2003;144:2208–13.
Catena C, Colussi G, Nadalini E, Chiuch A, Baroselli S, Lapenna R, et al. Cardiovascular outcomes in patients with primary aldosteronism after treatment. Arch Intern Med. 2008;168:80–5.
Rossi GP, Barisa M, Allolio B, Auchus RJ, Amar L, Cohen D, et al. The Adrenal Vein Sampling International Study (AVIS) for identifying the major subtypes of primary aldosteronism. J Clin Endocrinol Metab. 2012;97:1606–14.
Celen O, O’Brien MJ, Melby JC, Beazley RM. Factors influencing outcome of surgery for primary aldosteronism. Arch Surg. 1996;131:646–50.
Sukor N, Kogovsek C, Gordon RD, Robson D, Stowasser M. Improved quality of life, blood pressure, and biochemical status following laparoscopic adrenalectomy for unilateral primary aldosteronism. J Clin Endocrinol Metab. 2010;95:1360–4.
Gordon RD, Stowasser M, Tunny TJ, Klemm SA, Rutherford JC. High incidence of primary aldosteronism in 199 patients referred with hypertension. Clin Exp Pharmacol Physiol. 1994;21:315–8.
Umakoshi H, Naruse M, Wada N, Ichijo T, Kamemura K, Matsuda Y, et al. Adrenal venous sampling in patients with positive screening but negative confirmatory testing for primary aldosteronism. Hypertension. 2016;67:1014–9.
Umakoshi H, Wada N, Ichijo T, Kamemura K, Matsuda Y, Fuji Y, et al. Optimum position of left adrenal vein sampling for subtype diagnosis in primary aldosteronism. Clin Endocrinol. 2015;83:768–73.
Umakoshi H, Tanase-Nakao K, Wada N, Ichijo T, Sone M, Inagaki N, et al. Importance of contralateral aldosterone suppression during adrenal vein sampling in the subtype evaluation of primary aldosteronism. Clin Endocrinol. 2015;83(4):462–7.
Fujii Y, Umakoshi H, Wada N, Ichijo T, Kamemura K, Matsuda Y, et al. Subtype prediction of primary aldosteronism by combining aldosterone concentrations in the left adrenal vein and inferior vena cava: a multicenter collaborative study on adrenal venous sampling. J Hum Hypertens. 2017;32:12–19.
Nishikawa T, Omura M, Satoh F, Shibata H, Takahashi K, Tamura N, et al. Guidelines for the diagnosis and treatment of primary aldosteronism—the Japan Endocrine Society 2009. Endocr J. 2011;58:711–21.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Monticone S, Satoh F, Giacchetti G, Viola A, Morimoto R, Kudo M, et al. Effect of adrenocorticotropic hormone stimulation during adrenal vein sampling in primary aldosteronism. Hypertension. 2012;59:840–6.
Kayser SC, Dekkers T, Groenewoud HJ, van der Wilt GJ, Carel Bakx J, van der Wel MC, et al. Study heterogeneity and estimation of prevalence of primary aldosteronism: a systematic review and meta-regression analysis. J Clin Endocrinol Metab. 2016;101:2826–35.
Hannemann A, Wallaschofski H. Prevalence of primary aldosteronism in patient’s cohorts and in population-based studies—a review of the current literature. Horm Metab Res = Horm- und Stoffwechs = Horm et Metab. 2012;44:157–62.
Omura M, Sasano H, Saito J, Yamaguchi K, Kakuta Y, Nishikawa T. Clinical characteristics of aldosterone-producing microadenoma, macroadenoma, and idiopathic hyperaldosteronism in 93 patients with primary aldosteronism. Hypertens Res. 2006;29:883–9.
Nishikawa T, Saito J, Omura M. Prevalence of primary aldosteronism: should we screen for primary aldosteronism before treating hypertensive patients with medication? Endocr J. 2007;54:487–95.
Umakoshi H, Tsuiki M, Takeda Y, Kurihara I, Itoh H, Katabami T, et al. Significance of computed tomography and serum potassium in predicting subtype diagnosis of primary aldosteronism. J Clin Endocrinol Metab. 2018;103:900–8.
Young WF, Stanson AW, Thompson GB, Grant CS, Farley DR, van Heerden JA. Role for adrenal venous sampling in primary aldosteronism. Surgery. 2004;136:1227–35.
Plouin PF, Amar L, Chatellier G. Trends in the prevalence of primary aldosteronism, aldosterone-producing adenomas, and surgically correctable aldosterone-dependent hypertension. Nephrol, Dial, Transplant. 2004;19:774–7.
Young WF, Stanson AW. What are the keys to successful adrenal venous sampling (AVS) in patients with primary aldosteronism? Clin Endocrinol. 2009;70:14–7.
Rossi GP, Auchus RJ, Brown M, Lenders JW, Naruse M, Plouin PF, et al. An expert consensus statement on use of adrenal vein sampling for the subtyping of primary aldosteronism. Hypertension. 2014;63:151–60.
Acknowledgements
This study was conducted as a part of the JPAS and JRAS by a Research Grant from the Japan Agency for Medical Research and Development (AMED) under Grant Number JP17ek0109122,JP18ek0109352, and JP19ek0109352, andthe National Center for Global Health and Medicine, Japan (27-1402, 30-1008). We wish to thank Dr. Yukio Hirata at the Institute of Biomedical Research and Innovation Hospital and Dr. Kazuaki Shimamoto at Sapporo Medical University School of Medicine for interpreting the significance of the results of this study. We also wish to thank Dr. Masanobu Yamada at Gunma University, Tatsuya Kai at Saiseikai Tondabayashi Hospital, Ryuichi Sakamoto at Saiseikai Fukuoka Hospital for collecting the clinical data.
JPAS Study Group
Masanobu Yamada28, Hiromi Rakugi29, Takashi Kawamura30, Osamu Ogawa31, Toshinari Yamasaki31, Akiyo Tanabe32, Tomonobu Hasegawa33, Masanori Abe34, Ryuichi Sakamoto35, Takuro Shinbo36, Tatsuya Kai37, Tomikazu Fukuoka38, Masanori Murakami39, Shigeatsu Hashimoto40, Makito Tanabe41, Mitsuhiro Kometani42, Yuichirou Yoshikawa43, Youichi Oono44, Hisashi Fukuda45, Takashi Yoneda46, Touru Sugiyama47, Fumihiko Matsuda48, Takahisa Kawaguchi48
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the JPAS Study Group are listed at the end of the paper.
Supplementary information
Rights and permissions
About this article
Cite this article
Fujii, Y., Takeda, Y., Kurihara, I. et al. Historical changes and between-facility differences in adrenal venous sampling for primary aldosteronism in Japan. J Hum Hypertens 34, 34–42 (2020). https://doi.org/10.1038/s41371-019-0229-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-019-0229-4