Abstract
Primary aldosteronism (PA) is a major cause of secondary hypertension and presents a higher risk for cardio-cerebrovascular (CCV) events compared with essential hypertension. To diagnose PA after a positive screening test, at least one of three available confirmatory tests [the saline infusion test (SIT), the captopril challenge test (CCT) or the furosemide upright test (FUT)] should be performed. The aim of our study was to investigate the relationship between the number of positive confirmatory tests using SIT and CCT and the clinical presentation and prevalence of CCV events in 398 PA patients. The number of PA patients doubled when PA diagnosis was defined by positive results on either the SIT or CCT confirmatory tests (single positive) compared to positive results on both the SIT and CCT confirmatory tests (double positive). We also found a more typical clinical presentation of PA, such as the use of more antihypertensive drugs to control blood pressure and a higher incidence of hypokalemia, in PA patients with double positive confirmatory tests than in those with a single positive confirmatory test. The incidence of CCV events in PA patients with double positive confirmatory tests was significantly higher than that in those with a single positive confirmatory test. Our results demonstrated that the number of PA patients was doubled by the use of PA diagnostic criteria using a single positive confirmatory test compared to the use of double positive confirmatory tests. PA patients with double positive confirmatory tests were associated with a more typical clinical presentation and a higher incidence of CCV events than those with a single positive confirmatory test.
Similar content being viewed by others
Introduction
Primary aldosteronism (PA) is a major cause of secondary hypertension. PA is caused by autonomous and excess secretion of aldosterone and accounts for 5~13% of hypertensive patients [1, 2]. Aldosterone excess causes not only hypertension but also direct myocardial and vascular damage. PA patients have a higher risk of cardiovascular and cerebrovascular (CCV) events compared with essential hypertension patients [3, 4]. Therefore, mineralocorticoid receptor antagonist treatment or adrenalectomy should be considered and initiated to reduce the risk of CCV events in patients with PA [5].
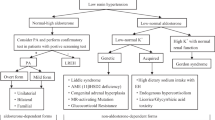
The plasma aldosterone concentration (ng/dL) (PAC)/plasma renin activity (ng/mL/hr) (PRA) ratio (ARR) has been used for PA screening. Patients with positive ARR should undergo one or more confirmatory tests to diagnose PA. The “Guidelines for the diagnosis and treatment of primary aldosteronism” published by the Japan Endocrine Society in 2009 recommend performing at least two of three confirmatory tests [the saline infusion test (SIT), the captopril challenge test (CCT) and the furosemide upright test (FUT)] to diagnose PA [6]. However, the Endocrine Society [7] and Japan Hypertension Society [8] indicate that one confirmatory test is enough to diagnose PA. In 2016, the Japan Endocrine Society published the consensus statement on PA diagnosis and defined PA as the presence of at least one positive confirmatory test, as the other societies above have recommended [9].
We reported that SIT and CCT were useful not only for the diagnosis of PA but also for the evaluation of the risk of CCV events [10]. SIT-positive PA patients had a significantly higher risk of CCV events than SIT-negative PA patients. In addition, post-SIT PAC and post-CCT ARR levels are correlated with the risk of CCV events. However, it remains unclear whether the number of positive confirmatory tests reflects the risk of a CCV event. Moreover, no study has assessed the clinical significance of performing two confirmatory tests.
The aim of our cross-sectional study was to investigate the relationship between the number of positive confirmatory tests (SIT and CCT) and the clinical presentation and prevalence of CCV events in 398 PA patients.
Methods
Subjects
The participants in this study included 398 PA patients (males 162/ females 236) who were diagnosed with SIT and CCT at our hospital between January 2004 and December 2017 (Table 1).
The study protocol was approved by the Human Ethics Committee of Osaka University (no. 16136) and conformed to the Declaration of Helsinki.
Diagnosis of PA
PA was diagnosed by a positive result on either the SIT or the CCT based on the cut-off value for each confirmatory test presented in the guidelines of the Japan Endocrine Society [6]. To exclude the effects of antihypertensive agents on PRA and PAC levels, all hypertensive treatment with angiotensin II receptor blockers, angiotensin-converting enzyme (ACE) inhibitors, β-blockers was discontinued for 14 days and diuretics were discontinued for 4 weeks before the diagnostic tests were performed, as recommended in The Endocrine Society guidelines on PA [7]. We measured the PAC (ng/dL) and PRA (ng/mL/hr) and calculated the ARR. When the ARR was more than 20, we performed the SIT and CCT to confirm the diagnosis of PA. Although the FUT is performed to evaluate renin suppression in Japan, the area under the ROC curve for the post-FUT PRA was smaller than that of the ARR [11], and neither positive nor negative FUT results were associated with CCV events in PA patients [10]. For this reason, two confirmatory tests (SIT and CCT) were investigated in this study. The tests were considered positive using the following cut-off levels: postinfusion PAC > 6 ng/dL (SIT) and ARR at 60 or 90 min after captopril challenge > 20 (CCT). The diagnosis of PA was established when one of these tests was positive. We excluded patients who were under 18 years of age, had end-stage kidney disease (eGFR < 15 (mL/min/1.73 m2), did not undergo the SIT or CCT, or were clinically diagnosed with PA without confirmatory tests. We defined both confirmatory tests positive as double positive group, either test positive as single positive group.
CCV events
We defined CCV events as cardiovascular disease (CVD) (nonfatal myocardial infarction or angina diagnosed by coronary angiography); atrial fibrillation (Af); or heart failure (HF) requiring hospitalization, defined as a history of admission to the hospital for HF treatment; symptomatic cerebral hemorrhage (CH) and cerebral infarction (CI). All patients were assessed for a history of CCV events at the time of PA diagnosis.
Laboratory tests
Blood samples were taken in the early morning after fasting, with the patient in a recumbent position. PAC was measured using an aldosterone radioimmunoassay (RIA) kit II (YAMASA Corporation, Tokyo, reference range: 2–13 ng/dL, intra and interassay CV: ≤ 15%, before 31 January 2007; Spac S Aldosterone Kit (TFB Corporation, Tokyo, reference range: 2.99–15.88 ng/dL, intra and interassay CV of ≤20%, from 1 February 2007 to 12 February 2017; or Accuraseed Aldosterone (Fuji Film Wako Corporation, Tokyo, reference range: 2.99–15.9 ng/dL, intra and interassay CV of ≤20%, after 13 February 2017)). The measured values were adjusted using a correlation formula estimated by the linear regression model of the aldosterone RIA Kit II (A) or Accuraseed Aldosterone (B) and Spac S Aldosterone Kit (C). PAC levels (A) were converted to PAC values (C) using the formula C (ng/dL) = 0.767 × A (ng/dL)−0.67. Similarly, PAC levels (B) were converted to PAC values (C) using the formula C (ng/dL) = [B (ng/dL) + 2.19]/0.89. The correlation coefficients of the regression models were 0.97 and 0.90, respectively.
PRA was measured by radioimmunoassay (YAMASA renin RIA beads, YAMASA Corporation, Tokyo), with a reference range of 0.2–2.7 ng/mL/hr and an intra and interassay CV of <15%.
Statistical analysis
Variables were expressed as median values (first and third quartiles) or mean ± SD. The 95% confidence interval (CI) for the proportion is based on the Clopper-Pearson method. The parameters of the two groups were compared using the Wilcoxon test for continuous variables and the chi-square test or Fisher’s exact test for categorical variables. Relationships were evaluated by the Pearson correlation coefficient. Two-sided p < 0.05 was considered to indicate the presence of a statistically significant difference. Statistical analyses were performed using the JMP Pro software for Windows (ver. 12, SAS Institute, Cary, NC).
Results
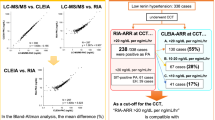
Relationship between the SIT and CCT results in PA patients
The relationship between the SIT and CCT results in the PA patients is shown in Fig. 1. Three hundred four PA patients were SIT positive, and 318 PA patients were CCT positive. PA patients who were positive on both the SIT and CCT (the double-positive group) accounted for 56.3% (224 patients). PA patients with positive results on either the SIT or CCA (the single-positive group) accounted for 43.7% (174 patients); the SIT-positive group comprised 80 patients (20.1%), and the CCT-positive group comprised 94 patients (23.6%).
Comparison of clinical presentation and incidence of CCV events between the double-positive group and the single-positive group
The clinical presentation of the 398 PA patients is shown in Table 1. The median age of these patients was 58 years (range: 47–67), and the median body mass index (BMI) was 23.9 kg/m2 (range: 21.7–27.1). The median systolic blood pressure (SBP) was 136 mmHg (range: 125–150)/median diastolic blood pressure (DBP) was 82 mmHg (range: 75–93), and the patients took 1.4 ± 1.1 numbers of antihypertensive classes. The median ARR was 55.5 (range: 30.1–108.6), eGFR was 76.6 mL/min/1.73 m2 (range: 66.2–87.3), serum potassium was 3.8 mEq/L (range: 3.6–4.1) and the rate of hypokalemia at diagnosis was 28.0%. The incidence of all CCV events was 6.0% [CVD 1.0% (4 patients), Af 1.5% (6 patients), HF 0.5% (2 patients), CH 0.8% (3 patients) and CI 2.8% (11 patients)] (Table 1). There was no difference in the incidence of CCV events between the SIT-positive PA patients and the CCT-positive PA patients (7.2 vs. 6.9%, p = 0.88).
The clinical presentations of the double-positive group and the single-positive group are shown in Table 2. The proportion of female patients in the single-positive group was higher than that of the double-positive group (54.0% vs. 66.1%, p = 0.015). Compared with the single-positive group, the double-positive group was taking more antihypertensive drugs (1.5 = 1.1 vs. 1.2 ± 1.0, p = 0.003) and had a higher PAC (19.9 vs. 12.0 ng/dL, p < 0.001), lower PRA (0.3 vs. 0.4 ng/mL/hr, p < 0.001), higher ARR [77.2 (ng/dL)/(ng/mL/hr) vs. 30.7 (ng/dL)/(ng/mL/hr), p < 0.001], lower serum potassium (3.8 vs. 3.9 mEq/L, p = 0.001) and a higher incidence of hypokalemia (39.0 vs. 13.8%, p < 0.001). There were no significant differences in eGFR, urinary sodium-to-creatinine ratio, urinary potassium-to-creatinine ratio, rate of ever smoking, diabetes mellitus or hyperlipidemia.
The incidence of CCV events in the double-positive group was significantly higher than in the single positive group [8.9% (20/224) vs. 2.3% (4/174), respectively, p = 0.006] (Fig. 2).
Comparison of the incidence of CCV events according to double-positive results (both the SIT and CCT are positive) or single-positive results (either the SIT or CCT is positive). The data on each bar represent the percentage of patients who developed CCV events. SIT saline infusion test, CCT captopril challenge test
In the present study, 100 patients underwent adrenal venous sampling successfully, 34 patients were diagnosed with unilateral PA, and 66 patients were diagnosed with bilateral PA. The proportion of unilateral PA in the double-positive group was higher than in the single-positive group (40.7 vs. 5.3%, p = 0.003). Thirty-nine PA patients underwent adrenalectomy and were diagnosed with adrenal cortical adenoma. The proportion of adrenal cortical adenoma in the double-positive group was higher than in the single-positive group (92.7 vs. 33.3%, p = 0.030).
Comparison of clinical presentations between the SIT-positive and CCT-positive subgroups of the single-positive group
The single-positive group was divided into two subgroups: the SIT-positive subgroup and the CCT-positive subgroup. The clinical presentations of the two subgroups are shown in Table 3. Patients in the SIT-positive subgroup were characterized by a higher proportion of males (51.3 vs. 19.1%, p < 0.001), younger age (47 years vs. 66 years, p < 0.001), higher systolic blood pressure (141 vs. 135 mmHg, p = 0.026), higher diastolic blood pressure (90 vs. 78 mmHg, p < 0.001), higher PAC (14.8 vs. 10.2 ng/dL, p < 0.001), higher PRA (0.9 vs. 0.2 ng/mL/h, p < 0.001) and lower ARR [18.5 (ng/dL)/(ng/mL/h) vs. 49.8 (ng/dL)/(ng/mL/h), p < 0.001). There were no significant differences in the duration of hypertension, the number of antihypertensive drugs used and the rate of hypokalemia.
Discussion
The present study showed that the double-positive group had a more typical clinical presentation of PA; they took more antihypertensive drugs to control blood pressure and had a higher PAC, lower PRA, higher ARR, lower serum potassium, higher rate of hypokalemia, higher incidence of CCV events, higher proportion of unilateral PA and higher proportion of adrenal cortical adenoma than the single-positive group. These results suggest that the double-positive group had a higher capacity for autonomous aldosterone secretion and a greater likelihood of having a unilateral adrenocortical adenoma compared with the single-positive group.
Regarding the diagnosis of PA, the CCT results confirm the failure of ACE inhibition to decrease ARR, and the SIT results confirm the failure to suppress aldosterone secretion after volume expansion with isotonic saline. Thus, these tests examine different parts of the renin-angiotensin-aldosterone system (RAAS) to evaluate autonomous aldosterone secretion. Kim et al. reported that the results of the CCT are not always in agreement with those of the SIT regarding PA diagnosis [12]. In fact, there were different clinical characteristics in the SIT-positive and CCT-positive subgroups in the present study. The SIT-positive subgroup included a significantly higher proportion of young males and higher PAC and PRA levels than the CCT-positive subgroup. RAAS is affected by sex and age. Estrogen decreases PAC levels, while testosterone increases PAC levels [13]. with increased age, PRA tends to decrease, and ARR tends to increase because salt sensitivity increases [14]. Based on these reports, young males tend to be more likely to show higher PAC levels and be positive on the SIT compared with the elderly, and postmenopausal females tend to be more likely to have positive CCT results. Regarding ARR in the CCT, the possibility of unreliable and misleading diagnosis as a result of suppressed PRA in cases of low-renin hypertension should be considered. Therefore, other PAC diagnostic criteria post-CCT [12] might lead to different results and conclusions.
The treatment goal for PA is to prevent CCV events and control hypertension and hypokalemia [15]. The clinical severity and CCV event risk of PA patients ranges from mild to severe and from low to high, respectively. Therefore, we suggest that PA patients be treated based on their clinical severity and CCV event risk. The point is how PA patients evaluate their clinical severity and risk of CCV events. As previously described, we reported that SIT-positive PA patients had a significantly higher risk of CCV events than SIT-negative patients, and the post-SIT PAC and post-CCT ARR levels correlated with the risk of CCV events [10]. The present study also showed that SIT-positive patients had a higher risk of CCV events than SIT-negative patients (7.2% vs. 2.1%, Fisher’s exact test, p = 0.083) and had higher post-SIT PAC levels and post-CCT ARR (Cochran-Armitage tendency, p = 0.059 and p = 0.016, respectively). In addition, patients with SIT and CCT positivity had a significantly higher risk of CCV events compared to patients with SIT positivity and CCT negativity (odds ratio 3.82, p = 0.033, data not shown). Our previous study did not investigate the CCT results in SIT-positive PA patients because some of them underwent only one CCT and SIT. However, the present study elucidated that PA patients with CCT positivity had a higher risk of CCV events than CCT negative PA patients with SIT positivity because we recruited PA patents who had undergone both the SIT and the CCT. Thus, the use of both the SIT and CCT confirmatory tests may be more beneficial than the use of each test alone for elucidating the clinical severity and CCV event risk in PA patients. In terms of the incidence of specific CCV events in the double-positive group and the single-positive group, the double-positive group had a higher incidence of Af (2.7 vs. 0%), HF (0.9 vs. 0%), CH (1.4 vs. 0%) and CI (4.0 vs. 1.2%) than the single-positive group, but its incidence of CVD was not higher (0.9 vs. 1.2%). The reason that the incidence of CVD events was not different between these groups was not elucidated because the small number of CVD cases might be affected. Thus, performing both SIT and CCT confirmatory tests may be more useful for elucidating the clinical severity and CCV event risk in PA patients compared to the use of either test alone.
As a limitation, our study was cross-sectional. Further prospective studies are needed to show whether the use of both the SIT and CCT tests predicts the clinical severity and the CCV event risk of PA patients.
In conclusion, the number of PA patients was doubled when PA diagnostic criteria requiring a single positive confirmatory test was used compared to when double positive confirmatory tests were required. PA patients with double positive confirmatory tests had a more typical clinical presentation of PA and a higher incidence of CCV events than those with a single positive confirmatory test.
References
Nishikawa T, Omura M. Clinical characteristics of primary aldosteronism: its prevalence and comparative studies on various causes of primary aldosteronism in Yokohama Rosai Hospital. Biomed Pharmacother. 2000;54(Suppl 1):83s–85s.
Young WF Jr. Minireview: primary aldosteronism—changing concepts in diagnosis and treatment. Endocrinology. 2003;144:2208–13.
Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol. 2005;45:1243–8.
Mulatero P, Monticone S, Bertello C, Viola A, Tizzani D, Iannaccone A, et al. Long-term cardio and cerebrovascular events in patients with primary aldosteronism. J Clin Endocrinol Metab. 2013;98:4826–33.
Catena C, Colussi G, Nadalini E, Chiuch A, Baroselli S, Lapenna R, et al. Cardiovascular outcomes in patients with primary aldosteronism after treatment. Arch Intern Med. 2008;168:80–85.
Nishikawa T, Omura M, Satoh F, Shibata H, Takahashi K, Tamura N, et al. Task Force Committee on Primary Aldosteronism TJES. Guidelines for the diagnosis and treatment of primary aldosteronism—the Japan Endocrine Society 2009. Endocr J. 2011;58:711–21.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:jc20154061.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Naruse M, Nishikawa T, Yanase T, Shibata H. Task Force members of the Committee of Primary Aldosteronism of Japan Endocrine Society. Consensus statement of diagnosis and treatment of primary aldosteronism in Japan. Folia Endocrinologica Japonica. 2016;92:20.
Hayashi R, Tamada D, Murata M, Mukai K, Kitamura T, Otsuki M, et al. Saline Infusion Test highly associated with the incidence of cardio and cerebrovascular events in primary aldosteronism. Endocr J. 2017;64:507–13.
Hirohara D, Nomura K, Okamoto T, Ujihara M, Takano K. Performance of the basal aldosterone to renin ratio and of the renin stimulation test by furosemide and upright posture in screening for aldosterone-producing adenoma in low renin hypertensives. J Clin Endocrinol Metab. 2001;86:4292–8.
Kim JH, Park KS, Hong AR, Shin CS, Kim SY, Kim SW. Diagnostic role of captopril challenge test in Korean subjects with high aldosterone-to-renin ratios. Endocrinol Metab. 2016;31:277–83.
Komukai K, Mochizuki S, Yoshimura M. Gender and the renin-angiotensin-aldosterone system. Fundam Clin Pharmacol. 2010;24:687–98.
Nakama C, Kamide K, Kawai T, Hongyo K, Ito N, Onishi M, et al. The influence of aging on the diagnosis of primary aldosteronism. Hypertens Res. 2014;37:1062–7.
Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. 1999;341:709–17.
Acknowledgements
This study was supported by a Health Labour Sciences Research Grant [Nanchitou (Nan)—Ippan—046] from the Ministry of Health, Labor and Welfare, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Saiki, A., Tamada, D., Hayashi, R. et al. The number of positive confirmatory tests is associated with the clinical presentation and incidence of cardiovascular and cerebrovascular events in primary aldosteronism. Hypertens Res 42, 1186–1191 (2019). https://doi.org/10.1038/s41440-019-0247-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0247-1
Keywords
This article is cited by
-
Comparison of the shortened and standard saline infusion tests for primary aldosteronism diagnostics
Hypertension Research (2020)