Abstract
Purpose
To evaluate the clinical features of developmental cysts of the orbit.
Patients and methods
Retrospective study of patients who had excision of cysts between 1992 and 2020.
Results
Three hundred and 58 patients (189 male; 53%) with orbital developmental cysts were identified, all being unilateral. Age at surgery varied from birth to 77 years (mean 17, median 18 years) and the average symptom duration was 5 years (median 18 months; range 1 day-50 years). The commonest presenting features were a peribulbar lump or upper lid swelling, followed by proptosis, pain, diplopia and reduced vision. Most patients (82%) had a palpable mass, with epidermoids, sebaceous dermoids and keratinised dermoids commonly affecting the superotemporal quadrant, and conjunctiva-containing cysts usually being biased to a medial location.
Cysts were lined by keratinised epithelium with dermal structures (224/358; 63%), non-keratinised epithelium with dermal structures (69/358; 19%), epidermis without identifiable dermal structures (19/358 ‘epidermoids’; 5%), conjunctiva (12/358; 3%), respiratory epithelium (4/358; 1%), or mixed dermal and conjunctival epithelia (30/358 ‘dermo-conjunctival’ cysts; 8%). Overall, two-thirds (242/358; 66%) had histological evidence of chronic intramural inflammation, and a half of cysts showed granuloma formation (178/358 cysts). Chronic inflammation was less common with conjunctival cysts (54%, 7/12 patients) and none showed granuloma formation.
Conclusion
Developmental cysts of the orbit vary from the relatively common dermoid cysts to the extremely rare respiratory epithelial-lined cysts. Respiratory cysts, being deeper, may present late in life and cysts containing conjunctival epithelium tend to be less inflamed and typically favour the superonasal quadrant.
Similar content being viewed by others
Introduction
Congenital cysts are the commonest orbital mass in childhood, derived by sequestration of surface ectoderm along suture lines that close during embryonic development [1]. According to the epithelial phenotype, the presence of dermal appendages, keratinisation, or goblet cells, these cysts may be termed ‘epidermoid’, ‘sebaceous (non-keratinised) dermoid’, ‘keratinised dermoid’, ‘congenital conjunctival cyst’, ‘congenital respiratory cyst’ or ‘dermo-conjunctival cyst’ [2].
Although possibly some overlapping features, there appear to be fundamental clinical, pathological and embryonic distinctions between these types of cysts, and we compare the modes of presentation for a large series of such patients.
Patients and methods
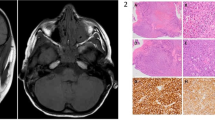
Patients who, between 1992 and 2020, underwent surgical excision of developmental cysts of the orbit at Moorfields Eye Hospital were identified from the orbital database. Based on surface epithelial phenotype and the presence of keratin, intradermal appendages and/or goblet cells, the cysts were classified into one of six categories—namely, keratinised dermoid (Fig. 1A), (ii) sebaceous (non-keratinised) dermoid, (iii) epidermoid (Fig. 1B), (iv) congenital conjunctival cyst (Fig. 1C) (v) congenital respiratory cyst (Fig. 1D), or (vi) dermo-conjunctival cyst (Fig. 1E) [2]. The clinical records for these patients were reviewed for gender, symptoms and duration, laterality, age at surgery and position within the orbit.
A Dermoid cyst with keratinised squamous epithelium, free keratin in the cavity (arrow) and intramural sebaceous glands (arrow-head). B Epidermoid cyst with free keratin (arrow) inside a cavity lined by keratinised squamous epithelium, but without any intramural dermal appendages. C Conjunctival cyst with goblet cells within the epithelium (arrow-heads). D Respiratory cyst lined with ciliated (arrow-head) pseudo-columnar epithelium. E A dermo-conjunctival cyst with both goblet cell-containing epithelium (arrow) and non-keratinised stratified squamous epithelium (arrow-head). All stained with haematoxylin and eosin and x10 objective, except “D” (with x40).
The study was approved by the Institutional Review Board (MEH #367) and adhered to the tenets of the Declaration of Helsinki.
Results
Three hundred and 58 patients (189 male; 53%) had complete histopathological records, with 224 (63%) keratinised dermoids, 69 (19%) sebaceous dermoids, 30 (8%) dermo-conjunctival cysts, 19 (5%) epidermoids, 12 (3%) conjunctival cysts, and 4 (1%) respiratory cysts.
The overall mean age at presentation was 17 years (median 18; range 0–77), with keratinised or sebaceous dermoids typically presenting in the first two decades, earlier than other groups (p < 0.001) (Table 1). The duration of symptoms was extremely varied with all types of cyst (from 1 day to ~50 years), the average duration being 5 years and median duration 18 months. The commonest symptoms were a peribulbar lump or upper eyelid swelling (Table 1). Overall, a palpable mass was evident in 82% (294/358) and proptosis in 22% (77/358), although a higher proportion of patients with epidermoids and respiratory cysts had proptosis (9/19 [47%] and 3/4 [75%], respectively) (p = 0.002) (Table 1). Although non-axial displacement was noted in 16% (58/358) patients overall, it was seen with 37% epidermoids, 50% respiratory cysts and 47% dermo-conjunctival cysts (p < 0.001). Impaired ocular motility was rare with keratinised and sebaceous dermoids, and absent with conjunctival cysts, but occurred more commonly with epidermoids (26%), respiratory cysts (50%) or dermo-conjunctival cysts (20%) (p < 0.001) (Table 1).
The location of a cyst was known accurately in 304/358 (85%) patients and most (207/304; 68%) were preseptal or parabulbar, although 50% epidermoids and 59% dermo-conjunctival cysts were retrobulbar (Table 2). Dermoids and epidermoids were the only lesions recorded as having a “dumbbell” configuration through the lateral orbital wall, and only sebaceous or keratinised dermoids occurred in the temporalis fossa. Of 160 superotemporal lesions, 121/160 (76%) were keratinised dermoids and 32 (20%) sebaceous, whereas conjunctival and dermo-conjunctival cysts were not found in this location. Most (75%) conjunctival cysts were located superonasally or superiorly and 84% dermo-conjunctival cysts were nasally-biased (Table 2).
Chronic intramural inflammation was present in 66% (242/358) cysts and granulomatous inflammation in a half (178/358). Conjunctival cysts were associated with somewhat less chronic inflammation (7/12 cysts; 54%) and with no granuloma formation (Table 3).
Discussion
Keratinised dermoids were the commonest developmental cysts in this series, followed by non-keratinised ‘sebaceous’ dermoids—with the former containing a thick, greasy keratin ‘paste’ and the latter having translucent sebaceous oil: both have a predilection for the superotemporal quadrant [3, 4] and, in this series, are the only types found within the temporalis fossa (Table 2). Dermoid cysts presented at the youngest median age (Table 1), although deep orbital dermoids present later and often with inflammation due to leakage of lipid [3, 5]. Consistent with previous studies [6,7,8], chronic intramural inflammation was seen in two-thirds of our dermoid cysts; the lower proportion with inflammation amongst conjunctival cysts (Table 3) suggests that leakage of the lipid content from dermoids is a potent inflammatory trigger.
Epidermoid cysts are lined by keratinised squamous epithelium and lack dermal appendages, although some dermoids may be regarded as ‘epidermoid’ if—due to histological sampling variation—sparse dermal appendages are missed. Although clinically similar to dermoids, epidermoids often presenting 1–2 decades later as a higher proportion of them involve the deeper parts of the orbit, with a superotemporal predilection. A deep orbital epidermoid with possible intracranial extension has been described[9].
Congenital respiratory cysts are extremely rare (1% of cases in this series) and with less than 20 cases in the literature [10,11,12,13,14,15,16,17,18]. Whilst most orbital respiratory cysts occur with paranasal sinus disease or trauma[10, 11], congenital respiratory cysts probably arise from epithelium sequestered during the development of the paranasal sinuses [12]. The four patients in this series had no history of sinus disease or trauma, presented in later adulthood, and three of the four cysts were retrobulbar—the latter causing non-axial proptosis and impaired ocular motility (Table 1) [7,10,11,12,16,17,18].
Developmental conjunctival cysts usually present with a soft, fluctuant and uninflamed mass in the anterior superonasal quadrant, without visual impairment, diplopia or globe displacement (Tables 1–3). The 3% prevalence in our series is comparable to previous reports [19, 20], as is the superonasal location [21, 22]. Although less likely to have intramural inflammation (Table 3) [2, 20], the slow expansion of these thin-walled cysts can cause pain and tenderness [21]. Dermo-conjunctival cysts (with both conjunctival and cutaneous epithelia) are almost exclusively sited medially [2, 5, 20], this location suggesting that they may arise from sequestered embryonic caruncular tissue [2]. They accounted for 8% of our cases, comparable to the 5% reported by Shields et al. [6].
In summary, this large series highlights the clinical and pathological differences between various congenital orbital cysts. Due to their more anterior location, keratinised and sebaceous dermoids are usually detected at a younger age than other types of developmental cyst. The large or deep orbital lesion may cause significant globe displacement and reduced motility. Intramural or perilesional inflammation can be identified in two-thirds of the cysts, especially those with dermal appendages that secrete pro-inflammatory lipids, such as keratin and sebaceous oil.
Summary Table
What was known before
-
Most periorbital developmental cysts are lined by an epidermal or dermal epithelium, with contents derived from such surface epithelium.
-
Periorbital dermoids favour a superotemporal location within the orbit and usually present in childhood as a palpable mass.
What this study adds
-
The largest study of patients undergoing excision of periorbital developmental cysts, with a logical classification into six subgroups, based upon the type of epithelial lining.
-
A broad age range for the presentation of these cysts, with rarer types (such as those containing solely respiratory or conjunctival epithelium) often remaining asymptomatic for many decades.
-
In contrast to dermoids and epidermoids, developmental cysts lined by conjunctival epithelium (with or without an admixture of stratified squamous epithelium) arise almost exclusively in the medial half of the orbit.
-
Chronic intramural inflammation is common, but less frequent with conjunctival cysts (in which granulomatous inflammation was not seen). This difference suggests that leakage of lipid debris from dermal or epidermal cysts might be a more potent trigger for intramural inflammation.
References
Shields JA, Bakewell B, Ausburger JJ, Donoso LA, Bernardino V. Space-occupying orbital masses in children. Ophthalmology. 1986;93:379–84.
Vahdani K, Thaung C, Tay E, Rose G. Developmental cysts of the orbit with mixed conjunctival and cutaneous epithelial phenotypes. Ophthalmic Plast Reconstr Surg. 2021. https://doi.org/10.1097/IOP.0000000000001976
Bonavolontà G, Tranfa F, de Conciliis C, Strianese D. Dermoid cysts: 16-year survey. Ophthalmic Plast Reconstr Surg. 1995;11:187–92.
Bartlett SP, Lin KY, Grossman R, Katowitz J. The surgical management of orbitofacial dermoids in the pediatric patient. Plast Reconstr Surg. 1993;91:1208–15.
Vahdani K, Rose GE. Presentation and treatment of deep orbital dermoid cysts. Ophthalmology. 2020;127:1276–8.
Shields JA, Kaden IH, Eagle RC Jr, Shields CL. Orbital dermoid cysts: clinicopathologic correlations, classification, and management. The 1997 Josephine E. Schueler lecture. Ophthalmic Plast Reconstr Surg. 1997;13:265–76.
Abou-Rayyah Y, Rose GE, Konrad H, Chawla SJ, Moseley IF. Clinical, radiological and pathological examination of periocular dermoid cysts: evidence of inflammation from an early age. Eye. 2002;16:507–12.
Pushker N, Meel R, Kumar A, Kashyap S, Sen S, Bajaj MS. Orbital and periorbital dermoid/ epidermoid cyst: a series of 280 cases and a brief review. Can J Ophthalmol. 2020;55:167–71.
Ahmed RA, Eltanamly RM. Orbital epidermoid cysts: A diagnosis to consider. J Ophthalmol. 2014;2014:508425.
Tay E, Yee AC, Luthert PJ, Rose GE. Congenital respiratory epithelial cysts of the orbit: a rare cause of major orbital impairment. Ophthal Plast Reconstr Surg. 2014;30:116–9.
Goh RL, Hardy TG, Williams RA, McNab AA. Respiratory epithelial cysts of the orbit. Orbit. 2016;35:245–9.
Newton C, Dutton JJ, Klintworth GK. A respiratory epithelial choristomatous cyst of the orbit. Ophthalmology. 1985;92:1754–7.
Jakobiec FA, Roh M, Stagner AM, Yoon MK. Choristomatous respiratory cyst restricted to the upper eyelid. Ophthalmic Plast Reconstr Surg. 2016;32:15–18.
Thanos A, Jakobiec FA, Mendoza PR, Hatton MP. Ectopic (choristomatous) orbital respiratory cyst: histopathology and immuno- histochemistry. Surv Ophthalmol. 2014;59:328–33.
Yeh C, Atillasoy C, Seykora JT, Lee V. A rare case of a periorbital respiratory (choristomatous) cyst. J Cutan Pathol. 2021;48:171–3.
Eggert JE, Harris GJ, Caya JG. Respiratory epithelial cyst of the orbit. Ophthalmic Plast Reconstr Surg. 1998;4:101–4.
Morris WR, Fleming JC. Respiratory choristomatous cysts in the temporal orbit. Ophthalmic Plast Reconstr Surg. 2001;17:462–4.
Mee JJ, McNab AA, McKelvie P. Respiratory epithelial orbital cysts. Clin Exp Ophthalmol. 2002;30:356–60.
Shields JA, Shields CL. Orbital cysts of childhood – classification, clinical features, and management. Surv Ophthalmol. 2004;49:281–99.
Jakobiec FA, Bonanno PA, Sigelman J. Conjunctival adnexal cysts and dermoids. Arch Ophthalmol. 1978;96:1404–9.
Goldstein MH, Soparkar CN, Kersten RC, Orcutt JC, Patrinely JR, Holds J. Conjunctival cysts of the orbit. Ophthalmology. 1998;105:2056–60.
Rose GE, O’Donnell BA. Congenital orbital cysts associated with the common sheath of superior rectus and levator palpebrae superioris muscles. Ophthalmology. 1995;102:135–8.
Acknowledgements
Professor Geoffrey Rose receives some funding from the National Institute of Health Research (NIHR) Biomedical Research Centre at Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology.
Author information
Authors and Affiliations
Contributions
CW collected and analysed the data, reviewed the literature and drafted the paper. KV collected and analysed the data, reviewed the literature and revised the draft paper. CT provided histopathological input, with photomicrographs and text where appropriate, together with review of the manuscript. GER originated and designed the investigation, analysed the data, revised the manuscript at each stage, and provided the final version for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wilde, C., Vahdani, K., Thaung, C. et al. Presenting features for developmental cysts of the orbit. Eye 37, 309–312 (2023). https://doi.org/10.1038/s41433-022-01929-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-01929-3