Abstract
Objectives
To determine whether cataract surgery is associated with an increased risk of subsequent lower eyelid entropion and evaluate potential associated factors.
Methods
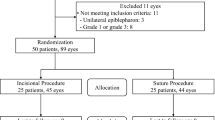
This retrospective cohort study included consecutive patients undergoing first eye cataract surgery over a 10-year period at a single institution (n = 14,574). The fellow phakic eye served as control. Patient records were evaluated up until either the time of second eye cataract surgery or any other intraocular or adnexal surgery. The primary outcome was the rate of entropion repair in both the pseudophakic (exposed) group and the phakic control group. Groups were compared using relative risk and Kaplan–Meier analysis. Multivariate logistic regression was used to compare pre-specified characteristics of those patients that underwent entropion repair in their pseudophakic eye with those that did not.
Results
A fourfold higher relative risk of undergoing entropion repair was observed in eyes that had undergone cataract surgery compared with the fellow unoperated eye (95% confidence interval 1.6–9.8; P < 0.001) with an increased risk at all timepoints between 1 and 12 years according to Kaplan–Meier analysis (P = 0.001). Median time to entropion repair after cataract surgery was 58 months (range 3–124). Documented intraoperative patient factors such as patient or eye movement, eyelid squeezing, pain or anxiety were an independent risk factor for subsequent entropion (P < 0.0001).
Conclusions
Cataract surgery is associated with an increased risk of subsequent lower eyelid entropion. Surgeons should be aware of this risk in the pre- and post-operative assessment of patients undergoing cataract surgery.
Similar content being viewed by others
Introduction
Lower eyelid entropion is characterised by inward turning of the lower eyelid margin. Involutional entropion accounts for the majority of cases, with a prevalence of 2.1% in people aged over 60 years old. Keratopathy and dry eye syndrome are observed in over 60% and 70% of cases respectively [1]. Surgical correction is almost always indicated to minimise both patient symptoms and the risk of ocular complications such as chronic conjunctivitis, corneal scarring, microbial keratitis, ulceration and perforation. The main causative factors in the development of involutional entropion are horizontal lower eyelid laxity, lower lid retractor dehiscence and overriding of the preseptal orbicularis oculi onto its pretarsal component [2,3,4,5].
There is a well-established association between cataract surgery and post-operative eyelid malposition, with upper eyelid ptosis being the most widely accepted of these and affecting 11.4% of patients [6]. The relatively higher proportion of pseudophakic patients undergoing entropion repair has previously led to a speculative association between cataract surgery and involutional entropion [7]. This association was not corroborated by others in a prospective study of patients undergoing cataract surgery with 6 months follow-up [8].
Motivated by this discrepancy in the literature and the clinical significance of entropion, the aim of this study was to determine whether there is indeed an increased relative risk of entropion after cataract surgery. Secondary objectives included establishing the post-operative timing of any subsequent entropion surgery and determining the cumulative risk with time post-operatively. Potential additional risk factors were also considered. Meeting these objectives will help to inform both patients and surgeons. It might also offer new insight and understanding into the potential effects of cataract surgery on the adnexal tissues.
Methods
This retrospective cohort study was undertaken at University Hospital Southampton, a large teaching hospital and tertiary referral unit in the United Kingdom. The work was approved and conducted in accordance with institutional governance as an evaluation of existing practice and therefore determined to be exempt from ethical committee review in line with guidance from the NHS Health Research Authority [9, 10]. The study protocol and data collection adhered to the tenets of the Declaration of Helsinki. We identified all consecutive patients undergoing first eye cataract surgery at the host institution over a 10-year period (July 2007 to June 2017) through an informatics search of electronic health records and surgical case coding records. The side undergoing cataract surgery served as the ‘exposed’ pseudophakic eye, with the fellow phakic eye acting as a ‘control’, thereby matched for age, sex and follow-up duration. The electronic records and clinical coding records of all patients were further screened for a history of ocular or adnexal surgery preceding their first eye cataract surgery, and any such cases were excluded. The end of the follow-up period was defined by the last available clinical outpatient follow-up as of December 31st 2019. In cases where the participant underwent cataract surgery in the fellow (second) eye or underwent any other subsequent ocular/adnexal surgery in either eye (excluding entropion repair) before the date of their final clinic review, we defined the end of follow-up as the date of any such surgery. Those patients that underwent entropion repair during the follow-up period were identified from the health records. We further scrutinised all available historical health records of these patients to ensure that there was no pre-existing diagnosis of entropion or any preceding history of ocular or adnexal surgery prior to their cataract procedure.
We extracted demographic characteristics (age and sex) and intraoperative data for all participants. Intraoperative data included surgery duration, type of anaesthesia, intraoperative complications and any documented “intraoperative patient factors”. We defined intraoperative patient factors as any written commentary in the operation note that was related to either patient or eye movement, eyelid squeezing, pain, anxiety or a strong Bell’s reflex.
Statistical analysis
The relative risk of undergoing subsequent entropion repair after cataract surgery was calculated by comparing the rate of entropion surgery between the exposed (pseudophakic) group and their matched control (phakic) eyes. Kaplan–Meier analysis was conducted to determine the cumulative risk of subsequent entropion repair after cataract surgery in both the pseudophakic eye and the phakic control eye. The two Kaplan–Meier curves were compared using Log-rank testing. We calculated the absolute risk of entropion within 1, 5- and 10-years following cataract surgery in both groups.
To investigate potential variables associated with entropion development, we conducted univariate logistic analyses, comparing those patients who underwent subsequent entropion repair in their “exposed” pseudophakic eye against all remaining cases. The chi-square and Mann-Whitney tests were used for categorical and quantitative variables respectively. Odds ratios (OR) with 95% confidence intervals (CI) were computed. Proceeding with multivariate logistic regression analysis, we included all variables that showed a P value ≤ 0.2 in the univariate analysis. We considered a P value ≤ 0.05 as statistically significant. All data manipulation and statistical analysis were conducted using R (version 3.6.2; R Core Team; Vienna, Austria) and referenced packages [11,12,13].
Results
Out of 16128 first eye cataract cases performed, 1554 were excluded due to prior ocular or adnexal surgery. Patient characteristics of the remaining cases are presented in Table 1. Of the remaining 14,574 cases, 30 eyes of 28 patients were identified as having subsequent entropion repair in either eye during the follow-up period. Of those 30 eyes, 22 patients received entropion surgery in the exposed (pseudophakic) eye, 4 in the control (phakic) eye and 2 underwent bilateral entropion repair. Thus, the overall relative risk of requiring subsequent entropion correction in the exposed (cataract surgery) group versus the matched control group (no cataract surgery) was 4.0 (95% CI 1.6–9.8; P < 0.001). Median time from cataract surgery to ipsilateral entropion repair was 58 months (range 3–124, n = 24).
Kaplan–Meier analysis demonstrates that the cumulative risk of undergoing entropion repair in the eye following cataract surgery is higher than the fellow control eye at all timepoints post-operatively (Fig. 1). The difference in these cumulative risk curves is statistically significant (P = 0.001). The absolute risk of undergoing entropion repair in the same eye within the first year after cataract surgery is 0.1%, increasing to 0.5% at 5 years and 2.3% at 10 years. This compares with 0.0%, 0.2%, and 0.8% for the same timepoints in the control eye.
Univariate analysis (Table 2) showed that significant variables associated with higher odds of entropion correction following cataract surgery were older age (78.0 ± 5.3 vs 74.9 ± 11.4 years; OR = 1.03; P = 0.04) and documented intra-operative patient factors (42.9% vs 9.1%; OR = 11.2; P < 0.001). The use of topical ± intracameral anaesthesia was associated with reduced odds (54.2% vs 65.5%, OR = 0.45; P = 0.02). Fitting a multivariate logistic regression model (Table 2), only the documentation of intra-operative patient factors was found to be an independent risk factor for entropion correction following cataract surgery (OR = 11.10; 95% CI = 3.69–35.18; P < 0.001).
Discussion
The present study found a fourfold increase in the risk of entropion repair following cataract surgery, compared with phakic controls. The absolute risk tends to increase with time at greater rate compared with controls. The issue whether cataract may increase the risk of subsequent entropion has been given limited attention and remains controversial. On the one hand, an association between cataract surgery and entropion onset had only been tentatively speculated in 1990 by Hurwitz et al. [7]. The authors observed a higher rate of pseudophakia amongst 29 patients undergoing entropion repair. Because age is a likely confounder of both entropion and cataract, our own study better corroborates the hypothesis of Hurwitz et al. by controlling for this (as well as for sex and follow-up duration). In further agreement with Hurwitz et al, the present study showed that the onset of entropion after cataract surgery is delayed, occurring on average almost 5 years later.
In conflicting evidence, Hosal et al. conducted a prospective study of 124 patients undergoing cataract surgery and reported no cases of post-operative entropion throughout a follow-up of 6 months [8]. Conversely, the findings presented here are based on an initial cohort of more than 14,000 patients with 3908, 982 and 127 patients included at 1, 5 and 10 years respectively. In light of our own findings, the study of Hosal et al. appears to be limited by both an underpowered sample size and a short follow-up, which could explain this disparity.
Our results offer some useful insights regarding possible factors implicated in the aetiology of entropion after cataract surgery. The anatomy of the lower eyelids is similar to that of the upper lids. In persistent post-operative ptosis, it is perioperative dehiscence of the levator palpebrae superioris (LPS) and/or increased horizontal lid laxity that are generally considered to be the main aetiological factors [14]. Any corresponding insult to the lower eyelid might result in retractor dehiscence or increased horizontal laxity; both key drivers in the development of entropion [2,3,4,5]. Whereas post-operative ptosis is generally reported as being observed immediately after surgery, we found a significant delay in the onset of post-operative entropion. We postulate that this may be because in the upper eyelid, acute dehiscence might result in an immediate drop in lid height due to the primary role of the LPS in elevating the lid. In contrast, the lower eyelid retractors work in partnership with the canthal ligaments and inherent lid elasticity to oppose the pretarsal orbicularis and prevent inward rotation of the eyelid margin. The delay in onset might suggest that cataract surgery might accelerate involutional changes in the structural anatomy of the eyelids without inducing immediate frank entropion. Indeed, in our experience, increased inferior fornix fat prolapse can be observed in some patients as a potential sign of retractor dehiscence following cataract surgery but without any manifest entropion (Fig. 2) [4]. We propose that future prospective study of this is indicated, along with the effect of cataract surgery on other eyelid parameters such horizontal laxity or orbicularis override.
The eyelid speculum has been widely implicated by others as a potential contributor to post-operative ptosis [6, 14, 15]. As the speculum widens the palpebral aperture, in some patients it might actually place the levator complex and lower lid retractors under eccentric tension, particularly in narrower palpebral apertures [15] or if the vector forces are directed too anteriorly, too forcefully or for too long (Fig. 3a, b). This hypothesis of speculum-induced trauma might be supported by our finding that there was a significant association between the risk of subsequent entropion repair and the documentation of intra-operative patient factors such as eye movement, eyelid squeezing, pain, anxiety and/or a strong Bell’s reflex during cataract surgery. Forceful contraction of orbicularis oculi might exacerbate any speculum-induced tension on the retractors [16], as might upward movement of the globe (Fig. 3c). This latter point is supported by an analogous observation in the upper eyelid by some authors; that the rates of postoperative ptosis are comparatively higher where the globe is placed under downward traction in counterforce to the LPS e.g., in cataract surgery using bridle sutures [17], or in some instances of glaucoma surgery [18, 19]. This has been challenged by others [14, 20], and an alternative theory is that rather than increase the vertical eyelid laxity, the speculum might put the eyelids under excess horizontal tension [14]. We suggest that neither should be considered mutually exclusive. Regardless of the exact mechanism, it seems that there is mounting evidence that the speculum may be in some way implicated in accelerating certain involutional changes in the eyelids.
Historically, the aetiological role of local anaesthesia has also been considered in the development of post-operative eyelid malpositions such as ptosis, but most frequently in the context of a transient and self-limiting effect [20,21,22]. In the present study, the use of topical ± intracameral anaesthesia appeared to be associated with a lower odds of subsequent entropion, when compared with the use of retrobulbar, peribulbar or sub-Tenon administration. More importantly, this association was not found to be independent of age, sex, operative duration and intra-operative factors during multivariate analysis. As such, the apparent “protective” administration of topical anaesthesia might simply reflect the more straightforward nature of these cases or other unmeasured confounders.
As a result of this study, we propose that surgeons should pay particular attention to the eyelid anatomy before, during and after cataract surgery, and counsel patients appropriately. In patients who may be particularly susceptible to post-operative involutional eyelid changes (e.g., older patients, and those with pre-existing involutional changes or where there may be difficulty in maintaining comfort and positioning), care should be taken to optimise a relaxed patient state and minimise stress on the periocular tissue. Based on previous studies and personal experience, particular attention should be paid to those with smaller palpebral apertures.
Limitations
This study highlights specific challenges in studying the risk of entropion after cataract surgery. Namely, those challenges are the sample size requirements, delay in onset of entropion and the need to control for key confounders such as age, sex and follow-up duration. With the findings of our study, it is now apparent that a prospective interventional comparative study would not be feasible. The retrospective nature of this study design attempts to overcome these barriers, but in doing so we acknowledge some important limitations. Firstly, only the risk of subsequent surgery for entropion was studied. However, compared with other lid malpositions such as ptosis and ectropion, surgery is almost always recommended for lower eyelid entropion due to the physical irritation and risk of corneal complications. Therefore, we regard entropion surgery a reasonable proxy for entropion per se. Secondly, there are potential biases in patient selection and attrition when retrospectively censoring patients according to their follow-up time. Unsurprisingly, we found that only a minority of patients (27%) undergoing first eye cataract surgery have a subsequent review in the same institution beyond 12 months without having had their second eye cataract (or any other procedure) performed. By 5 years, only 6.8% fall into this scenario, and by 10 years, this is less than 1%. We acknowledge that this subgroup of patients might have confounding factors such as previous trauma or ocular co-morbidities that we could not reliably control or measure and that might predispose them to a greater (or lesser) risk of entropion. Thirdly, there are limitations in the accuracy and completeness of operative data extracted (and particularly with documented operative commentary regarding intra-operative patient characteristics). That said, we identified no reason to believe that this would introduce any undue bias in multivariate analysis (both surgeon grade and the rate of complications were similar between groups). Incomplete or inaccurate electronic records might also affect the reliability of identifying and screening patients retrospectively. An effort was made to minimise this by scrutinising all available health records (paper and electronic) for those patients that did indeed go on to receive subsequent entropion surgery. However, of the remaining patients that did not undergo entropion surgery, it is possible that some might have been inadvertently considered in our analysis because screening of inaccurate or incomplete records led to their inclusion. The potential consequences of this would ultimately serve to proportionally increase the absolute risk rate of entropion repair in both the control and exposed groups; the absolute risk of entropion quoted in this commentary and observed in Fig. 1 might better be considered as a ‘minimum’ absolute risk. Given that the included cases with subsequent entropion were all matched with the subject’s fellow eye, the relative risk that we observed would not be affected by this limitation.
Conclusion
The present study demonstrates an increased risk of entropion repair following cataract surgery, which becomes more apparent with time. While the precise mechanisms of this association are not yet fully established, this study has identified factors associated with increased risk including age, anaesthetic type and specific intraoperative patient characteristics, with only the latter being independent of other measured variables. This study adds to the existing evidence that cataract surgery has the potential to accelerate involutional changes in the eyelids. It highlights the importance of the oculoplastic assessment both pre- and post-operatively, a mindfulness of the periocular tissue intra-operatively and calls for future research into potentially addressable aetiological factors.
Summary
What was known before
-
Cataract surgery is associated with eyelid malposition, most notably upper eyelid ptosis.
-
Cataract surgery has been postulated as a risk factor for lower eyelid involutional entropion.
What this study adds
-
Cataract surgery is associated with a fourfold increased risk of entropion development, when age, sex and follow-up period is controlled for.
-
Age, anaesthetic type and specific intra-operative patient characteristics were associated with subsequent entropion repair, with the latter being an independent risk factor.
References
Damasceno RW, Osaki MH, Dantas PEC, Belfort RJ. Involutional entropion and ectropion of the lower eyelid: prevalence and associated risk factors in the elderly population. Ophthal Plast Reconstr Surg. 2011;27:317–20.
Chu Y-C, Yang J-W, Tsai Y-J, Wu S-Y, Liao Y-L, Chu H-Y. Correction of involutional entropion with retractor redirection. Orbit Amst Neth. 2016;35:207–11.
Marcet MM, Phelps PO, Lai JSM. Involutional entropion: risk factors and surgical remedies. Curr Opin Ophthalmol. 2015;26:416–21.
Beigi B, Kashkouli MB, Shaw A, Murthy R. Fornix fat prolapse as a sign for involutional entropion. Ophthalmology. 2008;115:1608–12.
Miletić D, Kuzmanović Elabjer B, Bušić M, Bišćan Tvrdi A, Petrović Z, Bosnar D, et al. Histopathological changes in involutional lower eyelid entropion: the tarsus is thickened! Can J Ophthalmol. 2016;51:482–6.
Wang Y, Lou L, Liu Z, Ye J. Incidence and risk of ptosis following ocular surgery: a systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol Albrecht Von Graefes Arch Klin Exp Ophthalmol. 2019;257:397–404.
Hurwitz JJ, Smith D, Corin SM. Association of entropion with cataract surgery. Ophthal Plast Reconstr Surg. 1990;6:25–7.
Hosal BM, Tekeli O, Gürsel E. Eyelid malpositions after cataract surgery. Eur J Ophthalmol. 1998;8:12–5.
Health Research Authority (HRA). Defining Research. Available from: http://www.hra-decisiontools.org.uk/research/docs/DefiningResearchTable_Oct2017-1.pdf
Health Research Authority (HRA). Decision Tool—‘Is my study research?’. Available from: http://www.hra-decisiontools.org.uk/research/question1.html
R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2019.
Kassambara A, Kosinski M, Biecek P, Fabian S survminer: Drawing Survival Curves using ‘ggplot2’ [Internet]. 2020. Available from: https://CRAN.R-project.org/package=survminer
Therneau T, Lumley T, Atkinson E, Crowson C survival: Survival Analysis [Internet]. 2020. Available from: https://CRAN.R-project.org/package=survival
Mehat MS, Sood V, Madge S. Blepharoptosis following anterior segment surgery: a new theory for an old problem. Orbit Amst Neth. 2012;31:274–8.
Crosby NJ, Shepherd D, Murray A. Mechanical testing of lid speculae and relationship to postoperative ptosis. Eye. 2013;27:1098–101.
Linberg JV, McDonald MB, Safir A, Googe JM.Ptosis following radial keratotomy. Performed using a rigid eyelid speculum. Ophthalmol. 1986;93:1509–12.
Singh SK, Sekhar GC, Gupta S. Etiology of ptosis after cataract surgery. J Cataract Refract Surg. 1997;23:1409–13.
Park AJ, Eliassi-Rad B, Desai MA. Ptosis after glaucoma surgery. Clin Ophthalmol. 2017;11:1483–9.
Naruo-Tsuchisaka A, Maruyama K, Arimoto G, Goto H. Incidence of postoperative ptosis following trabeculectomy with mitomycin C. J Glaucoma 2015;24:417–20.
Patel JI, Blount M, Jones C. Surgical blepharoptosis-the bridle suture factor? Eye Lond Engl. 2002;16:535–7.
Deady JP, Price NJ, Sutton GA. Ptosis following cataract and trabeculectomy surgery. Br J Ophthalmol. 1989;73:283–5.
Ropo A, Ruusuvaara P, Nikki P. Ptosis following periocular or general anaesthesia in cataract surgery. Acta Ophthalmol. 1992;70:262–5.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s concept and design, the collection and interpretation of data and preparation of the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schulz, C.B., Fallico, M., Rothwell, A. et al. Lower eyelid involutional entropion following cataract surgery. Eye 36, 175–181 (2022). https://doi.org/10.1038/s41433-021-01466-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01466-5