Abstract
Purpose
To describe the lid characteristics of recurrent upper eyelid trachomatous entropion and to report the long-term outcomes of a five-step surgical approach based on the principles of upper eyelid crease lamellar splitting and retractor release with redirection.
Subjects and methods
Retrospective case review of adult patients with recurrent upper eyelid trachomatous entropion who had undergone surgical correction using the five-step surgical technique between March 2014 and March 2018. Cases with primary entropion and/or <2 years of follow-up were excluded from this series.
Main outcome measures
Eyelid deformities (type of trichiasis, anterior lamellar laxity, lid margin abnormality, lid retraction and lagophthalmos), recurrence of entropion and trichiasis, cosmetic satisfaction, and surgical complications.
Results
Forty-two upper eyelids in 33 patients met inclusion criteria. Preoperative anterior lamellar laxity was present in 36 eyelids (85.7%), lid retraction in 31 eyelids (73.8%) with a mean preoperative MRD1 of 6.48 ± 1.1 mm, atrophic tarsus in 28 eyelids (66.7%), lid margin notching in 22 eyelids (52.4%), and lagophthalmos in 15 eyelids (35.7%). The surgical success rate was 92.9% (95% CI 0.805–0.985). There was no documented recurrence of entropion over a mean follow-up period of 31.79 months. Postoperative trichiasis without entropion occurred in three eyelids, which required repeat epilation.
Conclusions
The five step-approach based on the principles of lamellar splitting is effective in correction of recurrent trachomatous entropion with long-term stability. The procedure addresses the fundamental changes frequently seen in recurrent cases, in particular anterior lamellar laxity, scarred shortened posterior lamella, and trichiasis.
Similar content being viewed by others
Introduction
Repair of upper eyelid trachomatous entropion is challenging with recurrence rates as high as 61% with many techniques available [1, 2]. The widely used procedures, promulgated by the World Health Organization (WHO), carry the disadvantage of violating the tarsoconjunctiva [3]. This theoretically promotes inflammation [4] and may expedite the trachomatous scarring process with increased contracture of the conjunctiva and deeper tissues (tarsus and Muller’s muscle). Moreover, cutting through the tarsal plate may destabilize an already compromised eyelid with ultimate entropion recurrence [5].
Management of recurrent entropion is usually more complex than primary cases with poor outcomes due to sequelae from the original surgery and the progressive nature of the disease [6, 7]. Concurrent lid changes in recurrent upper lid cicatricial entropion are under-investigated. In addition, there is a scarcity of published data on the long-term outcomes of management of such cases.
The aim of this study is to investigate the lid characteristics of patients with recurrent upper lid trachomatous entropion and to present the outcomes of a five-step approach for surgical correction based on the principles of lamellar division.
Methods
In this retrospective study, the medical records of patients who underwent surgery for recurrent upper eyelid trachomatous entropion from March 2014 to March 2018 were reviewed. Clinical data included age, gender, laterality, prior surgical technique used, type of trichiasis, state of tarsus, lid margin abnormality, anterior lamellar laxity, overhanging skin fold and/or pretarsal skin laxity, margin reflex distance 1(MRD1), lid retraction, lagophthalmos, corneal status, and follow-up period. Anterior lamellar laxity was defined as an overhanging skin fold beyond the lid margin and/or pretarsal skin laxity. Upper eyelid retraction was defined as being present when the eyelid position was above the superior corneoscleral limbus. Lagophthalmos was considered to be present if the eyelids did not meet completely on gentle lid closure. Lid margin abnormality was defined as any lid margin notching and/or unidentifiable lid margin landmarks. Trichiasis was classified as the following: misdirected, metaplastic, entropic, and mixed [8]. Surgical success was defined as anatomic restoration of the upper eyelid margin without trichiasis, acceptable cosmetic appearance to the patient, and absence of any complication requiring intervention. Cases with primary entropion and/or <2 years of follow-up were excluded from this series. All subjects were treated in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained from all patients before the surgery including the possibility of publication of surgical information and eye photos. Fayoum University Ethics Committee (R112/2020) approved this retrospective chart review.
Surgical technique
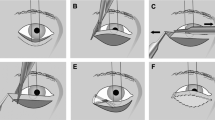
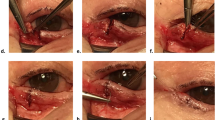
All procedures were performed under local anesthesia (with 2% lidocaine and 1:100,000 adrenaline) and intravenous sedation. Upper lid crease anterior lamellar recession (ALR) was performed as described previously [9,10,11] with the following five steps emphasized (Supplementary video 1, Supplementary fig. S1): 1, small upper blepharoplasty (Fig. 1a); 2, complete lamellar division with lid margin peeling where dissection between the tarsus and the pretarsal anterior lamella is continued across the lid margin beyond the lash follicles to include any posteriorly-located lashes or keratinization. A lid plate is used during this step to put the tarsus on stretch and to protect the eye (Fig. 1b); 3, disinsertion of the levator aponeurosis and Müller’s muscle from the tarsus with dissection of Muller’s muscle from the conjunctiva for 5 mm (Fig. 1c); 4, anterior lamellar repositioning on the tarsal plate using 3–4 interrupted mattress sutures leaving 3 mm of bare tarsus (Fig. 1d); 5, lid crease incision closure with incorporation of the edge of the Müller’s muscle-levator aponeurosis composite flap. These sutures don’t include tarsal bites (Fig. 1e, f).
a Small upper blepharoplasty with excision of small skin and muscle flap. b The anterior lamella (as a composite bipedicle flap of skin and orbicularis) has been completely separated from the tarsal plate with anterior lid margin peeling. c The upper eyelid retractors have been dissected off the tarsal plate and the underlying conjunctiva for 5 mm. d The detached anterior lamella is completely repositioned upward without tension. e The skin incision is closed incorporating the edge of upper lid retractors. f The surgical procedure is completed with 3 mm of tarsus left visible and a tight anterior lamella.
Results
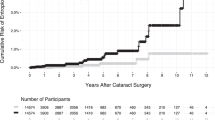
Forty-two upper eyelids in 33 patients (24 women and 9 men) were included in this series. The mean age at the time of surgery was 56.42 ± 8.65 years (range 37–67 years). Mean follow up for all patients was 31.79 months (SD 6.9 months, range 24–43 months). Posterior lamellar tarsal rotation (PLTR) was the original procedure in 20 eyelids (47.6%), bilamellar tarsal rotation (BLTR) in 14 eyelids (33.3%), and ALR in 7 eyelids (16.7%). Most eyelids had mixed types of trichiasis (Fig. 2): misdirected in 39 (92.9%); metaplastic in 38 (90.5%); entropic in 40 (95.2%); and partially epilated lashes in 25 eyelids (59.5%). All lashes were epilated in two eyelids (4.2%). Thirty-nine eyes (92.86%) had preoperative corneal erosions and corneal opacity was noted in 17 eyes (40.48%). Anterior lamellar laxity was present in 36 eyelids (85.7%) (Figs. 3, 4), lid retraction in 31 eyelids (73.8%) with a mean preoperative MRD1 of 6.48 ± 1.1 mm, atrophic tarsus in 28 eyelids (66.7%), lid margin notching in 22 eyelids (52.4%), and lagophthalmos in 15 eyelids (35.7%) (Table 1). Comparison of different eyelid characteristics across different types of surgery previously performed using Chi square test showed only statistically significant difference in lid margin abnormality. 60% of those who have lid margin abnormality had previous BLTR.
Surgical success was achieved in 39 eyelids (92.9%) (95% CI 0.805–0.985) (Figs. 2 through 4). There was no documented recurrence of entropion during the follow-up period. There were no patients who required reoperation for entropion. All patients reported symptomatic improvement after the procedure. No postoperative lagophthalmos on gentle lid closure was noticed in any patient. Postoperative trichiasis without entropion occurred in three eyelids, which required repeat epilation (Supplementary fig. S2). Anterior lamellar central necrosis occurred in three eyelids (7.1%); this healed spontaneously without sequelae (Fig. 5). Separated lid margins healed well with restoration of lid margin contour in all patients.
Discussion
In 1996, the WHO started a program to eliminate trachoma as a public health problem by 2020 [12], but it is clear that this goal will not be met on time. However, trachoma appears to be declining even in areas without a public health program possibly due to improved hygiene and sanitation [13, 14]. WHO recommends tarsal rotation procedures for all patients with entropion trichiasis [3]. One advantage of this surgery is that it is relatively simple to perform and can be taught to non-physicians. In spite of the global effort to improve the surgical quality, the overall failure rates of these surgeries are significant [6, 7, 15]. 10–75% of patients diagnosed with trichiasis were found to have a history of previous trichiasis surgery according to a primary analysis of data from the Global Trachoma Mapping Project [6]. Studies using tarsotomy procedures with a follow-up period above 1 year have reported varied incidence of postoperative trichiasis ranging from 33.9 to 65% [16,17,18,19].
There are common lid changes seen in patients with recurrent upper eyelid trachomatous entropion. The most frequently noticed in this series are anterior lamellar laxity and lid retraction with, in lesser degrees, atrophic tarsal plate, lid margin notching, and defective lid closure.
It is theorized that procedures involving direct tarsoconjunctival incision may trigger conjunctival inflammation and further scarring and shortening of the conjunctiva and deeper tissues (tarsal plate and Muller’s muscle) [2, 4]. Posterior lamellar shortening and fornix cicatrization explain both lid retraction [20, 21] and anterior lamellar laxity. Tarsoconjunctival shortening disturbs the anatomic balance between the anterior and posterior lamellae with secondary vertical eyelid skin redundancy. The overhanging skin fold mechanically rotates the lashes against the globe making the condition worse [8, 10]. Therefore, recurrent trachomatous entropion after previous surgery represents a unique challenge and usually necessitates more experience to assess and address the above pathophysiological changes.
In this series, we used the ALR procedure [8,9,10] which advantageously spares the posterior lamella with a focus on the following steps: 1- Small blepharoplasty which helps lessen the redundant skin fold, allowing pretrasal dissection and access to the upper lid retractors [10], 2- Complete lamellar splitting with meticulous dissection at the lid margin, peeling the entire anterior lid margin, allowing access to metaplastic lashes [10], 3- Upper lid retractor disinsertion from the tarsus with dissection free of the conjunctiva for at least 5 mm, allowing posterior lamellar advancement and correction of coexisting lid retraction and lagophthalmos [20], 4- Anterior lamellar recession for at least 3 mm on the advanced posterior lamella. Complete anterior lamellar separation as a bipedicle flap helps unrestrained upward repositioning [8, 9]. With healing, interlamellar scar tissue formation creates firm adhesion between the anterior lamella and the tarsal plate which gives a long-term control of pretarsal laxity. Anterior lamellar reposition without complete lid split will not overcome the cicatricial force at the tightly bound lid margin structures, which may hamper a potentially effective long-term outcome [22], 5- Lid crease incision closure including bites through the edge of levator aponeurosis- Muller’s muscle flap [9].
The centrepiece of this technique is to redirect the pull of the upper eyelid retractors from the tarsal plate to the recessed anterior lamella. This has a dual effect; first, it maintains an upward vector of traction on the anterior lamella with effective lash eversion abolishing the pretarsal skin laxity and preventing downward migration of the bipedicle flap during the healing process [23, 24]. Second, it allows recession of the posterior lamella inferiorly compensating for the shortened tarsoconjunctiva, correcting the concurrent lid retraction [16].
Sodhi et al. [25]. used a lamellar division procedure to treat surgical failures following PLTR in patients with UCE with good results. They reported associated lid anomalies with irregular lid margin and defective lid closure being the most frequent (52.2% and 36.96% respectively). They did not comment on palpebral fissure height or the presence of anterior lamellar laxity. A gray line incision was used for interlamellar dissection. We believe that this approach is not ideal for patients with anterior lamellar laxity as ALR will further aggravate the upper lid skin and orbicularis redundancy [8, 10, 19]. In addition, the lid margin is usually distorted in patients with UCE particularly recurrent cases with a difficult to identify gray line [11]. In contrast, a lid crease incision allows more controlled dissection at the lid margin without losing the plane or cutting through the tarsus [10].
Some researchers [26, 27] have reported good results with anterior lamellar excision/ eyelash resection for correction of recurrent cases. However, these were small series (4 and 12 upper eyelids in the studies of Moosavi et al. [26]. and Wu et al. [27]. respectively) with short follow-up periods. Eyelash resection alone will not correct anterior lamellar laxity and may aggravate eyelid retraction in addition to poor cosmesis.
In conclusion, the 5-step technique described is an effective treatment for recurrent trachomatous entropion. The procedure addresses the main contributors to recurrence. It is critical that repeat use of primary procedures not be advocated in patients with recurrent entropion, and, ideally, recurrent cases would be treated by physicians experienced in eyelid surgery. Ultimately, it becomes a “man-power” issue for the treatment of trachoma. However, with apparent decreasing rates of trachoma, it may be worth reconsidering the treatment recommendations by the WHO, as well as whether treatment by non-ophthalmologists should be promulgated, especially in cases of recurrence.
Summary
What was known before
-
Recurrence rate after trachomatous entropion correction is high with no ideal technique available to rectify recurrent cases.
What this study adds
-
There are characteristic lid changes in recurrent upper lid trachomatous entropion cases, in particular anterior lamellar laxity.
-
The five-step procedure is effective in recurrent trachomatous entropion and addresses the pathoanatomical deformities frequently seen in these cases.
References
Khandekar R, Mohammed AJ, Courtright P. Recurrence of trichiasis: a long-term follow-up study in the Sultanate of Oman. Ophthalmic Epidemiol. 2001;8:155–61.
Diab MM, Allen RC, Gawdat TI, Saif AS. Trachoma elimination, approaching 2020. Curr Opin Ophthalmol. 2018;29:451–7.
Merbs SL, Resnikoff S, Kello AB, Mariotti SP, Greene G, West SK. Trichiasis surgery for trachoma Geneva, Switzerland World Health Organization 2015. https://www.who.int/trachoma/resources/9789241549011/en/ (accessed 1/2/2020).
Burton MJ, Rajak SN, Ramadhani A, Weiss HA, Habtamu E, Abera B, et al. Post-operative recurrent trachomatous trichiasis is associated with increased conjunctival expression of S100A7 (psoriasin). PLoS Negl Trop Dis. 2012;6:e1985.
Kersten RC, Kleiner FP, Kulwin DR. Tarsotomy for the treatment of cicatricial entropion with trichiasis. Arch Ophthalmol. 1992;110:714–7.
World Health Organization Alliance for the Global Elimination of Trachoma by 2020. Second Global Scientific Meeting on Trachomatous Trichiasis. Cape Town, South Africa, November 4-6, 2015. https://www.who.int/trachoma/resources/who_htm_ntd_2016.5/en/(accessed 1/2/2020).
Habtamu E, Wondie T, Aweke S, Tadesse Z, Zerihun M, Gashaw B, et al. Predictors of Trachomatous Trichiasis Surgery Outcome. Ophthalmology. 2017;124:1143–55.
Rajak SN, Habtamu E, Weiss HA, Bedri A, Gebre T, Bailey RL, et al. The clinical phenotype of trachomatous trichiasis in Ethiopia: not all trichiasis is due to entropion. Investig Ophthalmol Vis Sci. 2011;52:7974–80.
Bi YL, Xu W, Rong A. Anterior lamellar repositioning with complete lid split: a modified method for treating upper eyelids trichiasis in Asian patients. J Plast Reconstr Aesthet Surg. 2009;62:1395–402.
Roth AH, Cannon PS, Selva D, Malhotra R. Management of upper eyelid cicatricial entropion. Clin Exp Ophthalmol. 2011;39:526–36.
Gawdat TI, Kamal MA, Saif AS, Diab MM. Anterior lamellar recession for management of upper eyelid cicatricial entropion and associated eyelid abnormalities. Int J Ophthalmol. 2017;10:1830–4.
World Health Assembly resolution WHA51.11 Global Elimination of Blinding Trachoma, 1988. https://www.who.int/news-room/fact-sheets/detail/trachoma (accessed 1/2/2020).
Jha H, Chaudary JS, Bhatta R, Miao Y, Osaki-Holm S, Gaynor B, et al. Disappearance of trachoma in western Nepal. Clin Infect Dis. 2002;35:765–8.
House J, Gaynor B, Taylor H, Lietman TM. The real challenge: can we discover why trachoma is disappearing before it’s gone? Int Ophthalmol Clin. 2007;47:63–76.
Gower EW, Munoz B, Rajak S, Habtamu E, West SK, Merbs SL, et al. Pre-operative trichiatic eyelash pattern predicts post-operative trachomatous trichiasis. PLoS Negl Trop Dis. 2019;13:e0007637.
Bowman RJ, Jatta B, Faal H, Bailey R, Foster A, Johnson GJ. Long-term follow-up of lid surgery for trichiasis in the Gambia: surgical success and patient perceptions. Eye. 2000;14:864–8.
Rajak SN, Makalo P, Sillah A, Holland MJ, Mabey DC, Bailey RL, et al. Trichiasis surgery in The Gambia: a 4-year prospective study. Invest Ophthalmol Vis Sci. 2010;51:4996–5001.
Gower EW, West SK, Harding JC, Cassard SD, Munoz BE, Othman MS, et al. Trachomatous trichiasis clamp vs standard bilamellar tarsal rotation instrumentation for trichiasis surgery: results of a randomized clinical trial. JAMA Ophthalmol. 2013;131:294–301.
Habtamu E, Rajak SN, Tadesse Z, Wondie T, Zerihun M, Guadie B, et al. Epilation for minor trachomatous trichiasis: four-year results of a randomised controlled trial. PLoS Negl Trop Dis. 2015;9:e0003558.
Collin JRO. Manual of Systematic Eyelid Surgery. 3rd ed. Philadelphia: Elsevier Health Sciences; 2006. p. 29–56.
Alsuhaibani AH, Al-Fakey YH. Unilateral Eyelid Lag and Retraction as Sequelae of Trachoma. Ophthalmic Plast Reconstr Surg. 2007;23:169–70.
Elder MJ, Collin R. Anterior lamellar repositioning and grey line split for upper lid entropion in ocular cicatricial pemphigoid. Eye. 1996;10:439–42.
Aghai GH, Gordiz A, Falavarjani K, Kashkouli MB. Anterior lamellar recession, blepharoplasty, and supratarsal fixation for cicatricial upper eyelid entropion without lagophthalmos. Eye. 2016;30:627–31.
Gawdat TI, Diab MM. Comment on: Upper eyelid levator-recession and anterior lamella repositioning through the gray-line - Avoiding a skin-crease incision. Indian J Ophthalmol. 2018;66:725–6.
Sodhi PK, Yadava U, Mehta DK. Efficacy of lamellar division for correcting cicatricial lid entropion and its associated features unrectified by the tarsal fracture technique. Orbit. 2002;21:9–17.
Moosavi AH, Mollan SP, Berry-Brincat A, Abbott J, Sutton GA, Murray A. Simple surgery for severe trichiasis. Ophthalmic Plast Reconstr Surg. 2007;23:296–7.
Wu AY, Thakker MM, Wladis EJ, Weinberg DA. Eyelash Resection Procedure for Severe, Recurrent, or Segmental Cicatricial Entropion. Ophthalmic Plast Reconstr Surg. 2010;26:112–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Diab, M.M., Allen, R.C. Recurrent upper eyelid trachomatous entropion repair: long-term efficacy of a five-step approach. Eye 35, 2781–2786 (2021). https://doi.org/10.1038/s41433-020-01306-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01306-y
This article is cited by
-
Comment on: Recurrent upper eyelid trachomatous entropion repair: long-term efficacy of a five-step approach
Eye (2022)
-
Comment on: Recurrent upper eyelid trachomatous entropion repair: long-term efficacy of a five-step approach
Eye (2022)
-
Reply: Recurrent upper eyelid trachomatous entropion repair: long-term efficacy of a five-step approach
Eye (2022)