Abstract
Background/objectives
To obtain a picture of the current status, training and governance for advanced practice and extended roles in the ophthalmic hospital non-medical workforce.
Methods
A 10 question, quantitative survey was designed with multidisciplinary members of the UK Ophthalmology Alliance and sent to the membership to obtain information on expanded non-medical roles.
Results
34 of the 58 UKOA member hospitals responded (58% response rate). All responding units were using registered optometrists, orthoptists and nurses to undertake expanded outpatient roles and 28/34 (82%) had expanded roles for undertaking procedures. Some units had large numbers of staff undertaking these roles. There were noticeable trends for certain professional groups to undertake certain roles. For example, nurses were undertaking most procedures, apart from lasers which were mainly delivered by optometrists. Nurses had the lowest banding and optometrists the highest for apparently similar roles. Training was mostly in-house apprenticeship style although some formal external qualifications were undertaken.
Conclusions
Ophthalmology is developing many innovative roles for the non-medical workforce and, with the launch of the OCCCF training, this is likely to increase. Terminology is confusing and a categorisation suitable for ophthalmology is proposed.
Similar content being viewed by others
Introduction
Ophthalmology has been particularly affected by rising demand, due to demographic changes and new treatments [1, 2]. Ophthalmology is now the busiest outpatient specialty and a 30–40% increase in demand is predicted over the next 20 years [3, 4]. The lack of capacity has been associated with significant harm to patients and there is a serious shortfall in ophthalmologist numbers [5, 6].
Ophthalmology has many highly skilled hospital non-medical professionals and many thousands more primary care optometrists [7]. The capacity crisis has driven ophthalmology service transformation, and a key lynchpin of national recommendations is changing the role of this multidisciplinary workforce [8,9,10,11,12,13,14].
Educational routes to support new roles for non-medical health care professionals (HCP) are sometimes through formal courses but, most commonly, through local, inconsistent and usually non-transferrable methods [4, 9, 15]. There is confusion over what roles are acceptable for different professionals, and issues such as Agenda for Change (AfC) banding or backfill for traditional roles have limited progress. The recent launch of the Ophthalmic Common Clinical Competency Framework (OCCCF) programme is hoped to increase the pace of change and consistency of standards [9]. Currently, there is no national overview of in-hospital HCP ophthalmic roles, to underpin expansion through shared learning and identification of the most clinically- and cost-effective models.
The United Kingdom Ophthalmology Alliance is a membership organisation founded in 2017 and all UK NHS hospital providers of ophthalmology services are eligible for membership. There are now more than 90 hospital members, working with stakeholders such as large ophthalmic patient charities and the professional colleges [16]. The UKOA undertook a survey of innovative roles undertaken by non-medical HCP in member hospitals.
Materials and methods
The aim of the survey was to explore the working practices of non-medical registered HCP (nurses, orthoptists and optometrists) in hospital ophthalmology services undertaking expanded (extended, advanced) roles, and the associated governance, indemnity, training and supervision.
The study population was taken from the UKOA hospital membership which, at the time, had 58 hospital ophthalmology members in England and Wales and no formal members in the other two UK nations.
The study used a 10 question, quantitative survey design. Some qualitative questions were also included to provide better understanding or allow clarification of answers. Multidisciplinary leaders of the UKOA workforce project team designed the questionnaire, which was refined by testing with the UKOA membership online and at UKOA national meetings, allowing amendments from all the registered professions, including ophthalmologists, and patient representatives from ophthalmic charity organisations.
Once agreed, the survey covered the following areas: independent consenting; outpatient roles; procedural/surgical roles; policies, protocol and guideline documents; training and qualifications; competency recording; job description and indemnity. For each area, details were required or data were classified for specific tasks and roles, and broken down by professional group (optometrist, orthoptist, nurse), banding and supervision requirements.
The survey was sent via email directly to all UKOA hospital members and also via email from the BIOS chair (VG) to relevant head orthoptists through the BIOS database. The local head orthoptist was asked to coordinate the data collection, provided with a paper form to support data collection if helpful, and return via an online system. The survey was sent out in 20th November 2018 and reminders regularly sent by email until 31st March 2019, via reminders on the UKOA website and in UKOA online news updates, and also given in person to attendees at UKOA meetings. Data were returned via the NHS Improvement online system Citizen Space Consultation Hub and analysis of the numerical data was performed using descriptive methods.
Results
Of the 58 surveys sent, 34 were returned completed, a response rate of 58% for the UKOA membership at the time. Only one was from Wales, the rest were from English units across NHS regions. There was a broad spread of type and size of units who responded, ranging from the very large specialist centres through teaching hospitals and university affiliated units to small and medium size district general ophthalmic units (Fig. 1).
Consenting
In 58.8% of units nurses were independent consenters for procedures, in 35% orthoptists and in 32% optometrists performed this role. Nurses consented for a broad range of procedures such as cataract surgery, intravitreal injections, trabeculectomy and anaesthetic, as well as for less invasive procedures such as fluorescein angiography, minor operations, botulinum toxin injections and laser capsulotomy. Orthoptists had a narrower range of consent practice, mainly squint surgery and botulinum toxin injections for ocular motility, and occasionally intravitreal injections, laser capsulotomy and cataract surgery. Optometrists also had a narrower remit, mainly cataract surgery and laser (capsulotomy, peripheral iridotomy [PI], argon retinal laser, selective laser trabeculoplasty [SLT]) and, in a small number of cases, intravitreal injections.
Outpatient roles
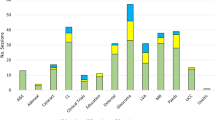
All units reported some innovative outpatient roles (Fig. 2a) but there was variability between the different professionals. Orthoptists had expanded into glaucoma and paediatric clinics and, to some degree, AMD and cataract clinics, but to a very small extent in most of the other subspecialties. Nurses played a major role in cataract clinics, AMD clinics, glaucoma clinics and A&E and minor eye care, and the other professionals had not made as much inroads into adnexal clinics and uveitis clinics as nurses. Optometrists undertook the majority of glaucoma clinics and diabetic retinopathy in-hospital screening clinics, were delivering a lot of care in AMD and paediatric clinics, and some A&E and cornea clinics.
a Roles in outpatients. b Roles in procedures. AMD age related macular degeneration, DR diabetic retinopathy, OCT optic coherence tomography, paeds paediatrics, PC primary care, preop pre-operative, postop post-operative, IV intravitreal, PI peripheral iridotomy, ops operations, botox botulinum toxin injection, CXL cross linking.
Numbers of practitioners per unit. In some areas of practice, a large number (we defined this as more than five) of practitioners had been developed per unit as shown in Table 1.
There were six to ten practitioners for preoperative cataract clinics in four units for nurses and one unit for optometrists, and in ten units for AMD active clinics. Ten units had six or more optometrists in glaucoma clinics. Six units had large numbers for A&E nurses and optometrists, and ten units had large numbers of orthoptists in paediatric clinics.
Supervision was defined by whether clinics were practitioner-led, that is no consultant working alongside the practitioner, or consultant-led, where the practitioner was working directly alongside the consultant, or a mixture.
For nurses (Fig. 3a) there were practitioner-led, consultant-led and mixed models. However, cataract postop clinics were primarily practitioner-led, whereas glaucoma, AMD active, corneal and adnexal post-op were mainly consultant-led. AMD active clinics and A&E were mixed.
a Nurses’ supervision. b Optometrists’ supervision. c Orthoptists’ supervision. AMD age related macular degeneration, DR diabetic retinopathy, OCT optic coherence tomography, paeds- paediatrics, PC primary care, preop = pre-operative, post op post-operative, CL consultant led, PL practitioner led, or mix.
For optometrists, things were different (Fig. 3b). The level of practice seemed more skewed towards the consultant-led or mixed model and less towards practitioner-led, even in cataract postop clinics where nurses were mainly performing without consultants in the clinic.
Orthoptists (Fig. 3c) were, like nurses, performing independent post-operative cataract clinics. Otherwise the rest was very consultant-led apart from paediatrics, where there was a mixed model but with a notable degree of practitioner-led care.
AfC banding (Table 1). There was often a range of banding reported for any given unit for each role. Nurses had generally a wider banding range for any given type of outpatient work, from band 5 to band 8, compared with the other professionals, with a preponderance of band 6–7. For optometrists, there were very few units in which an innovative role was delivered at band 5, with a spread of 6 to 8, and the vast majority at band 7 or 8. For orthoptists, again there was a range from band 5 to 8 but, apart from in paediatric clinics, there were no band 5s in innovative roles, and the trend was more towards band 7 for most roles.
Undertaking procedures
Most units had HCPs undertaking procedures (Fig. 2b), dominated by nurses. Optometrists were performing YAG lasers in more units than other professionals and had made some inroads into intravitreal injections. Orthoptists performed intravitreal injections, laser capsulotomies and botulinum toxin injections for blepharospasm and were starting to undertake botulinum injections for ocular motility. There were also a small number (n = 5) of units with staff (nearly all nurses) undertaking less invasive procedures such as corneal foreign body removal, subconjunctival injections, corneal scrapes, lacrimal syringing and punctal plug insertion and one unit with a nurse undertaking temporal artery biopsies.
Guidance documents
The Royal College of Ophthalmologists states innovative practice should be governed by policy or practice documents [17]. Only 20.6% of units had an overarching policy on advanced and extended role practice for HCPs for any specialty. However, there were documents guiding HCP practice for ophthalmology. In outpatients: for preoperative cataract clinics 91% of units had a document (including guideline, protocol, SOP or policy, sometimes more than one); for most other activity between 65–81% of units had a document; only 36% of units with postop adnexal, and 22% of units with general adnexal practice had a document and the only outpatient subspecialty where 100% units had a guidance document was uveitis. There did not seem to be a pattern to either size of unit or whether practice was practitioner- or consultant-led in terms of whether there were guidance documents. For procedures, units had documents as follows: minor operations 36%, botulinum toxin injections 55%, laser capsulotomy 58%, laser PI 66%, intravitreal injections 83% and only for corneal cross linking did 100% of units doing this practice have covering documents for the HCPs.
Training and qualifications
A combination of local consultant and cascade training, where trained HCPs train other HCPs, occurred for all roles; ~10% of units used only or mainly cascade training. There was limited use of formal (College of Optometrists higher qualifications, University MSc or equivalent) qualifications for many outpatient roles. There was some use of higher qualifications for cataract (15% all units undertaking this), paediatrics clinics (19%), A&E clinics (19%), cornea (30%) although not all practitioners would have the qualifications. There was more use in retinal clinics (AMD 40%, non-AMD retinal 37.5%) and particularly in glaucoma where 80% of units used these and the majority of the staff had these qualifications. For procedures, higher qualifications were rarely used and training was apprenticeship style, learning by working alongside more experienced clinicians.
Competencies
Most (82%) units had some degree of competency sign off system although most stated they did not have them comprehensively for all roles. 76% had job descriptions for most or all of the roles and all used a combination of existing trust indemnity and professional body indemnity to cover the practice.
Discussion
All the four UK nations have concluded that use of the non-medical workforce in innovative roles will be required to sustain national healthcare delivery [18,19,20,21,22]. The UK is at the forefront of this globally, able to drive this forward in a publicly funded, free at the point of access and national healthcare system, but many other countries are also pursuing this strategy [23,24,25,26]. There have been previous attempts to gain a national perspective on ophthalmology developments, usually concentrating on primary care optometry [27, 28]. A national survey of hospital optometrist roles with 70 responses showed that 96% of units surveyed had optometrists undertaking extended roles, of which glaucoma was the leading area (92%) and other areas being medical retina (71%), medical retina/diabetes (67%), cataract (55%) and corneal services (55%) [29]. In a small number of units optometrists performed laser capsulotomy, and occasionally undertook laser PI, SLT, intravitreal injections and chalazion surgery. There was a mix of practitioner-led and consultant-led services. The vast majority of training was apprentice style; external courses such as the College of Optometrists higher qualifications were undertaken, especially in glaucoma, but not for the majority.
The Way Forward provided an analysis of different models of care aimed at increasing capacity and contained limited numerical information on roles in glaucoma and cataract [4]. Of 42 departments interviewed, 21% had HCPs (six optometrist, two nurse, one both) seeing and listing cataract patients. In 90% units, HCPs saw cataract patients post-operatively of which approximately two thirds were in hospital. For glaucoma, 88% had incorporated non-ophthalmologists into their glaucoma services beyond the traditional roles but no further breakdown was included.
Our findings show that innovative roles are being undertaken widely by optometrists, orthoptists and nurses in hospital eye services. All responding units utilised staff in roles traditionally associated with ophthalmology doctors in outpatients and most were using HCPs for interventional procedures. Some (eight) units had, for any one professional group working in one subspecialty role, more than ten or even, for two large units, more than 20, undertaking the same work i.e. more than 20 nurses or more than 20 optometrists working in just one of the new roles. This is a no longer about one or two pioneering professionals breaking boundaries. The preponderance was, not surprisingly, in subspecialties with high demand or difficulty attracting enough medical staff (e.g. paediatrics). There is a significant amount of practice occurring without a consultant present. Informal “apprenticeship style” training, that is on the job alongside experienced practitioners, forms the majority of the education, with the exceptions of AMD outpatient care to an extent and glaucoma outpatient care to a very significant extent, where formal higher qualifications from Universities or the College of Optometrists are often gained. It is not possible to be certain whether this sample is fully representative of units across England and Wales. The survey was completed by 34 hospitals (of 58 UKOA members at the time in England and Wales). There may be a number of reasons why some units did not respond: the survey was detailed and required significant senior clinician and manager effort to collate the data, especially for larger units, which may not have reached a high priority for action given the current pressures on eye units; it may be that units who were less active and engaged with the UKOA and did not regularly send staff to the national meetings may have not have understood why the survey was relevant and important to them; and it may be that units which had not actively taken up this sort of practice felt less inclined to participate as they had less to showcase, potentially introducing bias into the results. The level of survey returns can be influenced by methodology and communication modes. We chose to use an online system for data collection and use email to send out of the link to the survey after discussions with member attendees at UKOA meetings indicated a strong preference to avoid paper communications and submission. This was felt by members to be more efficient, easier to share with other colleagues at their hospital, and fit with the general paper-light approach of the UKOA. However, at request of a small number of members, we also created a matching paper form to allow them to initially collate data locally before online submission, to ensure those who had a paper preference could be supported. Reminders to complete the survey were numerous and used a combination of approaches including email reminders, website news updates, and in person at our meetings, to encourage in a variety of ways. However, there are no other sources of data available on this crucial and widely recognised development to address the severe workforce and capacity issues causing patient safety issues in ophthalmology. Even given the limitations of the number of units involved, the findings do show that new hospital ophthalmology workforce models of care are occurring to a considerable degree.
It is interesting to see the relationship between different roles and different professional groups. In outpatients, the survey shows that orthoptists are mainly working in paediatrics and glaucoma, optometrists in cataract and glaucoma, nurses work across the board except paediatrics and slit lamp or OCT clinics for diabetic retinopathy screening referrals. For procedures, the differences are starker. Nurses form the basis of the non-medical delivery of procedures, apart from YAG lasers which optometrists more commonly perform. With the exception of botulinum toxin injections and, to a degree, intravitreal injections, the survey suggests orthoptists are not being utilised significantly in delivering procedures. There are differences in levels of independent working. For instance, it is not clear why, in this survey, nurse led postoperative cataract clinics are mainly independent yet optometrist led ones are not. What are the reasons for these differences? It is possible that nurses are thought to have more suitable basic training for procedures involving incisions or injections and holistic patient care, whilst optometrists have better core skills for slit lamps and therefore are more suited to deliver laser interventions. Possibly professionals themselves have a view on what they are best suited for, or units may mimic the choice of professionals based on what other units have already done. Non-medical intravitreal injecting began with nurses and this may have set a precedent which units feel they must follow.
The survey indicated a difference in banding for different professionals. Broadly nurses were banded at lower levels, orthoptists higher and optometrists received the highest banding. Some of this will be based on factors beyond the advanced role, such as core responsibilities, level of independence, case mix, experience, and which the data are not detailed enough to distinguish between. In addition, it may reflect the different degrees of autonomy on qualification, with orthoptists and optometrists having a higher degree of autonomy in their core roles. However, if this does represent a different level of pay for the same work between different professionals, this may need better consistency if we hope to attract and retain more staff, especially nurses, to these roles. The study did not support the anecdotal reports at the UKOA of widespread sessional banding, in which a professional only received the higher banding of pay during the sessions where the innovative role is delivered.
In 1997, Rose et al. were pivotal in recognising the range of ophthalmic care which lends itself to extended nursing practice and highlighted role extension as an ‘unclear concept’ [30]. In 2019 this lack of clarity persists as there is still much variability in the terminology used, particularly ‘extended roles’ and ‘advanced practice’, how this pertains to taking on roles previously associated with another profession, the levels of responsibility and breadth of education required, across multiple different UK nations, organisations and professions [20,21,22, 31,32,33,34]. Central to this is the balance between developing clinical experience and expertise versus the requirement to have undertaken formal development (to the masters level) in the three other developmental domains of education, leadership and research/development, and how this might define the terminology and the degree of independent autonomous practice. Nursing bodies and Health Education England clearly state the expectation that, for autonomous and/or independent practice, and to be termed an advanced clinical practitioner, a masters should have been undertaken, but BIOS and the College of Optometrists use the two terms differently [20,21,22, 31,32,33,34,35]. There is a balance to be achieved in ensuring appropriate education to take on new roles safely versus not setting the educational bar so high that we effectively exclude many HCPs who do not wish to pursue a highly academic route but who would be capable of delivering a wider scope of care.
Whatever the terminology, it is probably fair to say that there are three main levels of practice in innovative or non-core ophthalmology hospital HCP roles: those delivering very specific tasks or procedures which involve adherence to a standardised set of steps, ranging from lower risk procedures such as corneal scrapes through to higher risk procedures such as laser capsulotomy and intravitreal injections, which require very specific education and defined protocols but probably not a masters; those taking on more medical care including decision making roles but with clear supervision and as part of a consultant led team, for which the OCCCF and the College of Optometrists higher qualifications routes seem best aimed; and those undertaking much more independent and autonomous roles, for which a masters would be deemed important. We suggest in Table 2 a consistent terminology which would fit with current developments in ophthalmology, but accept this may change over time as roles and supporting funding and training programmes develop.
Those working in ophthalmology should be commended for developing innovative HCP roles to such an extent whilst dealing with severe capacity issues. To optimise this development, we need a system in which the training and skills of non-medical ophthalmic professionals can be harmonised across the UK to ensure quality and standards, and allow flexibility and free movement of staff without the need to repeatedly undertake local training. One move towards this is the OCCCF [9]. This allows wide access to a transferrable, consistent standard of training which can be accessed by OCCCF training or equivalence through other existing routes. At the moment the assessment process is still being finalised and it applies to only four subspecialty areas but more modules are likely to develop with time. This should support the upskilling, recruitment, retention and continued development of the wider ophthalmic clinical team, improved ophthalmic hospital capacity and ultimately safer and more patient centred care [36]. It would benefit from a clear funding stream.
It will need significant support from consultants to help HCPs to undertake the education and roles, to develop services, governance processes, associated guidance documents, which will require time to do this in already stretched job plans. Consultants will continue to provide overall supervision, oversight and leadership to ophthalmic services.
Summary
What was known before
-
Some non medical staff are undertaking roles traditionally associated with medical staff.
-
Workforce issues are driving an unknown increase in this.
-
The extent of the development and its governance has been unclear.
What this study adds
-
Demonstrates notable degree of expansion of roles for orthoptists, optometrists and nurses in eye hospital in clinics and procedure delivery over recent years.
-
Training is inconsistent and mainly locally delivered.
-
Currently strong links between each profession type and the type of work especially in delivering procedures.
-
Inconsistencies in remuneration which may create issues across the professions.
References
See the light. Improving capacity in NHS eyecare in England. All-Party Parliamentary Group on Eye Health and Visual Impairment. 2018. https://www.rnib.org.uk/professionals/health-professionals/appg-eye-capacity.
Mike Burdon, President RCOphth strongly condemns failure to stop the continuing crisis in hospital eye services. RCOphth. 2018. https://www.rcophth.ac.uk/2018/06/mike-burdon-president-rcophth-strongly-condemns-failure-to-stop-the-continuing-crisis-in-hospital-eye-services/.
NHS Digital Hospital Episode statistics. 2019. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics.
The Way Forward. Royal College of Ophthalmologists. 2017. https://www.rcophth.ac.uk/standards-publications-research/the-way-forward/.
Foot B, MacEwen C. Surveillance of sight loss due to delay in ophthalmic treatment or review: frequency, cause and outcome. Eye. 2017;31:771–5.
RCOphth Workforce census 2018. RCOphth. 2018. https://rcophth.ac.uk/wp-content/uploads/2019/02/RCOphth-Workforce-Census-2018.pdf.
ECOO Blue Book. 2015. European Council of Optometry and Optics. 2015. https://www.ecoo.info/wp-content/uploads/2016/03/ECOOBBFEB2016.pdf.
The Elective Care High Impact Interventions—Ophthalmology Specifications. NHS England. 2018. Transforming elective care services in ophthalmology. Elective Care Service Transformation Programme, NHS England. 2019. https://www.england.nhs.uk/wp-content/uploads/2019/01/ophthalmology-elective-care-handbook-v1.1.pdf.
The Ophthalmic Common Clinical Competency Framework (OCCCF). HEE/RCOphth/RCN/BIOS, College of Optometrists. 2019. https://www.hee.nhs.uk/our-work/advanced-clinical-practice/ophthalmology-common-clinical-competency-framework-curriculum.
CCECH Safe frameworks for eye health. Clinical Council for Eye Health. 2018. https://www.college-optometrists.org/the-college/ccehc/safe-systems-assurance-framework-for-eye-health.html.
NHS Education for Scotland. Optometry. 2020. https://www.nes.scot.nhs.uk/education-and-training/by-discipline/optometry/professional-development.aspx.
Together for health: Eye health care delivery plan 2013–8. NHS Wales. 2018. https://gweddill.gov.wales/docs/dhss/publications/150623eyeannualreporten.pdf.
Developing eye care partnerships 2012–7. Final project report 2017. Health and social care board. 2017. http://www.hscboard.hscni.net/download/PUBLICATIONS/OPTOMETRY/developing_eyecare_partnerships/DEP-Project-2012-2017-Final-Report.pdf.
Glaucoma diagnosis and management (NG81). NICE 2017. https://www.nice.org.uk/guidance/ng81.
The College of Optometrists Higher Qualifications. 2019. https://www.college-optometrists.org/cpd-and-cet/training-and-qualifications/higher-qualifications.html.
UK Ophthalmology Alliance. 2020. https://uk-oa.co.uk/.
Royal College of Ophthalmologists Quality Standards. 2018. https://www.rcophth.ac.uk/standards-publications-research/quality-and-safety/quality-standards/.
The NHS Long Term Plan. NHS England. 2019. https://www.longtermplan.nhs.uk/wp-content/uploads/2019/01/nhs-long-term-plan-june-2019.pdf.
The Interim People Plan. NHS England. NHS England/NHS Improvement. 2019. https://www.longtermplan.nhs.uk/wp-content/uploads/2019/05/Interim-NHS-People-Plan_June2019.pdf.
Advanced Nursing Practice Framework: Supporting Advanced Nursing Practice in Health and Social Care Trusts. The Northern Ireland Practice and Education Council for Nursing and midwifery. 2016.
NHS Wales Framework for Advanced Nursing, Midwifery and Allied Health Professional Practice in Wales. NHS Wales 2016. http://www.nwssp.wales.nhs.uk/sitesplus/documents/1178/NLIAH%20Advanced%20Practice%20Framework.pdf.
NHS Education for Scotland/Chief Nursing Office 2019. Advanced practice toolkit. http://www.advancedpractice.scot.nhs.uk/.
Astle W, Simms C, Anderson L. A workforce in crisis: a case study to expand allied ophthalmic personnel. Can J Ophthalmol. 2016;51:288–93.
Bolme S, Morken TS, Follestad T, Sorensen TL, Austeng D. Task shifting of intraocular injections from physicians to nurses: a randomized single-masked noninferiority study. Acta Ophthalmol. 2019. https://doi.org/10.1111/aos.14184.
Feng JJ, An L, Wang ZF, Zhan LL, Xu X. Analysis on ophthalmic human resource allocation and service delivery at county level in Mainland China in 2014. Yan KeZaZhi. 2018;54:929–34.
Browning DJ. Physician assistants and nurse practitioners in ophthalmology-has the time come? Am J Ophthalmol. 2018;186:ix–xi.
UK eye care service project Phase two: organisation of eye care services in the west midlands. College of Optometrists. 2010.
The enhanced eyecare evaluation scheme. College of Optometrists. 2018. https://www.college-optometrists.org/the-college/research/research-projects/enhanced-scheme-evaluation-project2.html.
Harper R, Creer R, Jackson J. Scope of practice of optometrists working in the UK Hospital Eye Service: a national survey. Ophthalmic Physiol Opt. 2016;36:197–206.
Rose K, Waterman H, Tullo A. the extended role of the nurse: reviewing implications for practice. Clin Effectiveness Nurs. 1997;1:31–37.
Advanced level nursing practice Section 1: The registered nurse working at an advanced level of practice. RCN. 2018. https://www.rcn.org.uk/professional-development/publications/pub-006895.
Extended roles in hospital optometry and liaison with community optometrists. The College of Optometrists. 2008.
Multi-professional framework for advanced clinical practice in England. Health Education England 2017.
Reshaping the workforce to deliver the care patients need. Nuffield Trust. 2016.
BIOS (British and Irish Orthoptic Society) Clinical Advisory Group. 2020. https://www.orthoptics.org.uk/resources/clinical-advisory-group/.
Health Education England. Framework to promote person-centred approaches in health and care. 2017. https://www.skillsforhealth.org.uk/services/item/575-person-centred-approaches-cstf-download.
Acknowledgements
With grateful thanks to professional colleagues from the UKOA member trusts and health boards in England and Wales who supplied data and information.
Funding
The UKOA is financially supported by NHS Improvement via the Getting it Right First Time (GIRFT) programme.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Greenwood, V., Stanford, P., Beddow, C. et al. Changing practice for the non-medical ophthalmic hospital workforce in the UK—a snapshot survey. Eye 35, 1886–1894 (2021). https://doi.org/10.1038/s41433-020-0955-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-0955-4
This article is cited by
-
Enhancing Ophthalmic Triage: identification of new clinical features to support healthcare professionals in triage
Eye (2024)
-
Providing capacity in glaucoma care using trained and accredited optometrists: A qualitative evaluation
Eye (2024)
-
An evaluation of optometric advanced skills within a UK tertiary based setting
Eye (2023)