Abstract
Purpose
To assess margins and the rate of local recurrence of ocular surface squamous neoplasia after excision with a 2 mm margin and cryotherapy at a single ophthalmic oncology center.
Outcome measures
(1) Conjunctival margin were assessed as positive, negative, or indeterminate margins. (2) Feasibility of repair without a graft. (3) Local recurrence.
Methods
Retrospective chart review of histologically proven conjunctival intraepithelial neoplasia and invasive squamous cell carcinoma cases that underwent excision with a 2 mm margin and cryotherapy.
Results
Eighty cases met inclusion criteria for the quantitative analysis. The margin was positive in six cases (7.5%), four of which were treated with post-op topical immunotherapy/chemotherapy. Of the six positive margin cases, there was one recurrence which occurred in the patient who did not receive post-op topical adjuvant therapy, however resolved after starting topical treatment. Conjunctival repair without use of a graft was feasible in 74 (93%) cases with a mean basal diameter of 6.4 mm. Total number of local recurrence was seen in three cases (4%), which were successfully treated with adjuvant topical treatment (one positive margin case, one indeterminate margin case) or repeat resection followed by episcleral plaque brachytherapy (one negative margin case).
Conclusion
Excision with 2 mm margin of OSSN is not associated with high rates of positive surgical margins. Even those with positive margins, when treated with adjuvant topical therapy did not develop recurrence. While achieving low rates of local recurrence, the conjunctiva is conserved, thereby minimizing the need for amniotic membrane or free conjunctival grafts for conjunctival repair.
Similar content being viewed by others
Introduction
Ocular surface squamous neoplasia (OSSN) describes the spectrum of mild ocular surface dysplasia to advanced intraepithelial dysplasia to invasive squamous cell carcinoma with extension beyond the basement membrane [1]. Treatment of OSSN ranges from purely surgical resection to exclusively topical (Interferon (IFN)-2B (injections or drops), fluorouracil (5-FU) 1%, or mitomycin C (MMC) 0.04%) to a combination of surgical and topical therapy [2].
In surgical oncology, tissue margin evaluation following excision is of paramount importance [3]. Although HIV [4], ultraviolet light exposure [5], petroleum products [6], heavy cigarette smoking [6], age [7], male sex [7], and human papilloma virus [8] are risk factors for OSSN, positive margin status is the most important factor in predicting recurrence of OSSN [9]. An array of techniques have been undertaken to reduce the rate of recurrence by performing excision using 4 mm margins, adjuvant cryotherapy, and postsurgical topical therapy [10, 11]. The 4 mm margin was an attempt to obtain negative margins, however this often occurred at the expense of a larger conjunctival defect requiring auto grafts or an amniotic membrane for conjunctival repair [11,12,13].
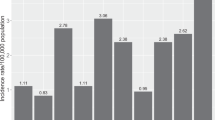
Conversely, a few studies have reported outcomes following excision with variable 2–4 mm margin [10, 14,15,16]. Although published OSSN recurrence rates vary significantly [9,10,11, 13,14,15,16,17,18,19,20], recent studies from USA compared to non-USA studies are associated with lower rates of recurrence as well as fewer invasive squamous cell carcinoma (SCC) cases compared to conjunctival intraepithelial neoplasia (CIN) [9,10,11, 13,14,15,16,17,18,19,20,21,22,23,24]. Yet the margin status (positive, negative, or indeterminate) that reflects not only surgical technique but also sample handling, and histopathological evaluation following primary excision has been reported only infrequently [9, 17]. Surgical margin status is an important outcome measure as it is independent of the histopathologic grade (CIN vs. invasive SCC) [19], use of adjuvant therapy (cryotherapy, chemotherapy) [10], and follow-up duration, all of which influence commonly reported outcome of recurrence rates.
In efforts to conserve the conjunctiva to facilitate closure without a graft, we have excised OSSN with narrow (2 mm) margins using standard surgical techniques. In this study, we report outcome measures of surgical margin status, the feasibility of conjunctival closure without a graft, and local recurrence rates of OSSN, while comparing these results with the published data.
Methods
We performed a systematic review of literature and identified published studies from PubMed (National Library of Medicine) from inception to October 2019. Non-English papers were excluded. Papers which described primary excision of OSSN were included in the analysis. Outcome measures included conjunctival margin status (positive, negative, or indeterminate margins), feasibility of repair without a graft and local recurrence. Data regarding corneal and scleral positive margins were collected, but is not part of the comparative analysis since the focus of this study is to evaluate outcomes with 2 mm conjunctival margin. Values extracted were total number of OSSN cases, proportion of CIN cases, size of surgical margin, margin status, use of cryotherapy, recurrence rate, and mean/median follow-up duration. Studies were excluded that did not contain the outcome values or if exenteration was the predominant initial treatment. The reviewed literature outcome data were compared with the current study for statistical difference with paired t test. Statistically significant was determined as equal or less than p = 0.05. Descriptive statistical analyses were performed.
We then conducted a single-center retrospective chart review of ophthalmic oncology patients who were clinically diagnosed by slit-lamp evaluation with OSSN at the Cole Eye Institute of the Cleveland Clinic between 2004 and 2019. Patients were included in the quantitative analysis who underwent primary excision with a 2 mm margin with double freeze cryotherapy in all cases and had pathology proven OSSN. This study protocol was approved by the institutional review board of the Cleveland Clinic, and adhered to the ethical principles of the Declaration of Helsinki. Patient files were reviewed for demographic information, OSSN characteristics, and initial treatment method as well as follow-up treatment in cases of recurrence. Cases were excluded if initial excision was done by a provider other than senior author (ADS), surgical margins were <2 mm, used topical immunotherapy or chemotherapy alone or in conjunction with surgery in the setting of negative margins, or lacked necessary data. For tumors with diffuse involvement or ill-defined edges, following confirmation of diagnosis with incisional biopsy, topical therapy was used. The quantitative data was de-identified.
The details of surgical technique are described elsewhere [25, 26], but the key component for a conjunctival limbal lesion included a sterile field and lid speculum followed by identifying and measuring the size of conjunctival lesion up to the edge of the thickened epithelium as seen through microscope. Using a fine tip ink pen the incision site was marked 2 mm from the thickened epithelial edge. Bipolar cautery was applied along the marked edges. The epithelium and stroma were cut down to sclera with Wescott scissors. The specimen was only elevated using forceps applied to the margin and not on the tumor. Then, using a beaver blade, the lesion was undermined and evaluated for tumor adhesions to the sclera. If scleral adhesion suggestive of invasion was present, then 10–30% scleral flap was performed reflecting it toward the limbus. For corneal involvement, an alcohol epitheliectomy was done by applying absolute alcohol for 1 min to the involved epithelium with 1 mm healthy epithelium as a safety margin while rest of the cornea was protected by viscoelastic. The denatured corneal epithelium was reflected toward the limbus. The excision was completed by limbal dissection removing the corneal component and the conjunctival component as a single piece. Double freeze cryotherapy was applied to conjunctival edges, but not along limbus. Direct closure was performed if wound defect was 10 mm or less. In general, for defects greater than 10 mm an autograph or amniotic membrane was placed. Special care was taken to flatten the specimen on round filter paper in order to avoid curling of the tissue edges. Specimens were inked for assessment of margins and/or presence of cauterized edge was indicative of margin when seen on microscopy. Formalin fixed paraffin embedded tissue with hematoxylin and eosin staining were classified as conjunctival intraepithelial neoplasia (CIN or Tis) or invasive SCC according to the American Joint Committee on Cancer classification system (8th edition) [27].
Results
From the literature review, fifteen articles met the inclusion criteria [9,10,11, 13,14,15,16,17,18,19,20,21,22,23,24]. There was one randomized control trial [24], 14 were observational studies (13 retrospective cohort studies [9,10,11, 14,15,16,17,18,19,20,21,22,23], and 1 case-control study) [13]. Of the 15 studies, 7 were from the USA. A total of 1257 OSSN cases were analyzed in the 15 studies, 979 (78%) were CIN and 278 (22%) were SCC. On weighted average, 33% of cases had positive margins [9, 13,14,15,16,17, 19, 21,22,23,24]. The average number of indeterminate tumor margin was 5% in two studies [9, 17]. The application of cryotherapy was variable in each study with an average use in 42% of cases [9,10,11, 13,14,15,16, 18,19,20,21,22, 24]. The overall weighted rate of recurrence was 19% [9,10,11, 13,14,15,16,17,18,19,20]. Of the positive margin cases, recurrence rate was 31% while it was 14% in excisions with negative margins [9, 11, 13,14,15, 17, 19]. The average follow-up time was 42 months (Table 1). Seven of the studies performed excision with margins greater than 2 mm beyond the visible tumor, of which six studies analyzed recurrence showing an overall weighted rate of recurrence of 15%.
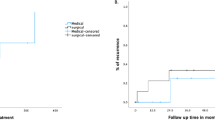
In our study, 80 cases were included in the quantitative analysis. Thirty-eight cases were excluded (diffuse tumors without a biopsy [20], topical therapy prior to excision [5], incomplete data [12], and <2 mm excision margin [1]). Of the 80 cases, 67 cases were CIN and 13 were SCC (Fig. 1). Median age at diagnosis was 71 years (range: 36–91), and mean follow-up time was 24 months. Most OSSN were located on nasal bulbar limbus (n = 44; 56%), then temporal (n = 34; 41%), and inferior (n = 2; 2.5%). The predominant appearance was as a gelatinous lesion (28, 45%), followed by papillomatous (18, 29%), and then leukoplakic (16, 26%). Vast majority of tumors (73, 91%) were 10.0 mm or less in largest basal diameter (LBD) (Fig. 2). The pathological classification was predominately CIN (Tis) (55%) (Table 2).
The assessment of tissue margins revealed that conjunctival margins were positive in 6 cases (8%), negative in 69 cases (86%), and indeterminate in 5 cases (6%). Postoperative topical therapy (immunotherapy or chemotherapy) was used in four cases with positive margins. Of these four cases, there was no recurrence. However, one of the two positive margin cases that were observed developed recurrence, but resolved after starting topical treatment. The subset of six positive margins was followed for average of 55 months. Additionally, scleral invasion of SCC was observed in three cases (4%) unrelated to the six positive conjunctival margin cases. Episcleral plaque brachytherapy (Iodine-125) was used in all three cases of scleral invasion.
Of the 80 primary excisions, 74 (93%) were able to undergo primary closure of the conjunctiva, while 3 (4%) required amniotic membranes and 3 (4%) free flap auto grafts. The average LBD of OSSN was 6.4 mm (Table 2).
There were three cases of recurrence. When comparing with margin status, the recurrence rate was 17% (1/6 cases) in the positive margin and 1.5% (1/69 cases) in negative margin group and 20% (1/5 cases) in the indeterminate group. Case 1 was a papillomatous nasal CIN 3/3 with the LBD of 5 and 4 mm corneal involvement initially received MMC 0.04% for four cycles (1 week on, 1 week off) for chemoreduction and then underwent excision with cryotherapy which had positive conjunctival margins (low grade dysplasia). No topical treatment was initially given, however once recurrence was detected (28 months later) by anterior segment (AS)-OCT, patient was then started on IFNα2b 3 million IU/mL injections every 2 weeks with topical IFNα2b 1 million IU/mL. After 2 months, progression was noted while on IFN and therefore switched to 5-FU 1% drops for 1 week with partial regression. Due to surface toxicity, he was switched back to IFNα2b 1 million IU/mL for 6 months to achieve full resolution. There was no recurrence over the subsequent 3 years of follow-up. Case 2 was a papillomatous nasal CIN 3/3 with LBD of 5 and 2.5 mm of corneal involvement which underwent excision with episcleral dissection and cryotherapy resulting in negative margins. Recurrence was seen on AS-OCT 7 months after excision. Patient was started on IFNα2b 1 million IU/mL topical drops QID for 4 months, which included 1 month beyond complete resolution by AS-OCT. Patient has not had recurrence for the past 3.5 years. Case 3 was a leukoplakic nasal SCC diagnosed clinically and with AS-OCT with a LBD of 8 and 3 mm corneal involvement that underwent excision, scleral flap, and cryotherapy which had indeterminate tumor involvement at the conjunctival margins. Recurrence was detected at slit-lamp 10 months after primary excision. Due to concern for scleral invasion, repeat excision with scleral flap was performed. Pathology showed scleral invasion requiring iodine-125 plaque brachytherapy following which remains recurrence free at last follow-up (1.5 years).
Discussion
At our center we primarily treat localized OSSN with surgical excision with a 2 mm margins in order to conserve normal tissue. We additionally apply double freeze thaw cryotherapy to the conjunctival wound edges as cryotherapy has been shown to reduce rates of recurrence [16, 28]. Our approach is supported by equivalent long-term recurrence rates and complications between topical interferon alpha2b (INFα2b) drops versus surgery [13]. We acknowledge that primary topical immunotherapy has an important role especially in non-discrete or diffuse tumors [29]. We identified over 3 decades of data evaluating 1257 eyes which underwent surgical excision with evaluation of surgical margins and/or recurrence rates from review of the literature. Overall, the published literature showed lower incidence of SCC than CIN in the USA (15%) compared to non-USA studies (40%). Additionally, rates of recurrence of OSSN were lower in the USA (5%; including our study) than non-USA studies (22%) [9,10,11, 13,14,15,16,17,18,19,20,21,22,23,24].
Conjunctival margin assessment
The reviewed literature supports the notion that positive tissue margins may be the most important factor predicting recurrence, with 31% occurring in positive tissue margins and 14% in negative tissue margins [9, 11, 13,14,15, 17, 19]. Although seven of the reviewed studies reported excision with a margin >2 mm, the average weighted proportion of positive margins was 33% in contrast to 8% in our data set (P < 0.01). This may be due to our surgical technique wherein we carefully identify the extent of the thickened epithelium and mark the measured 2 mm clear zone margin following careful assessment of photos, topographic drawings (to highlight specific details not evident on slit-lamp photos to guide follow-up changes and detection of recurrences), and intraoperative examination, which ensures accurate dissection. We believe that proper handling of the excised sample by placement on the filter paper and spreading of the tissue and unrolling of edges prior to immersion in fixative are critical for accurate assessment of the conjunctival margin [12]. Our rate of indeterminate margins of 6% was comparable to the average rate of 5% reported in two studies (P = 0.62) (Table 3) [9, 17].
Feasibility of primary repair
In an effort to obtain negative surgical margins and reduce the rate of recurrence, many have performed wide 4 mm margins, however this often resulted in a large wound defect requiring either an amniotic membrane or a conjunctival autograft to close the defect [11,12,13]. Reducing surgical area also is important to reduce the rate of limbal stem cell deficiency. This study showed that using a 2 mm margin did not increase the risk of recurrence compared to wider margins 2–4 mm in size. In addition, due to the smaller margin (2 mm) we were able to use primary conjunctival closure in the vast majority of cases (74 [93%]) (Fig. 3) with only three cases that required auto grafts and three cases amniotic membranes with excellent ocular surface healing. The mean LBD of our OSSN cases was 6.4 mm (median and mode = 6 mm) (Table 2). As an example, an average size 6 mm LBD limbal OSSN with a 2 mm margin would result in a 10 mm LBD wound defect in contrast to a 14 mm wound defect in a 4 mm margin resection. The effects on the surface area of the surgical defect are even more evident, wherein the total area (πr2) resected with a 2 mm margin when comparted to a 4 mm margin would be almost 50% smaller (79 mm2 vs. 154 mm2, respectively) (Fig. 4).
Local recurrence
There are many variables including histopathologic grade (CIN vs. invasive SCC) [19], use of adjuvant therapy (cryotherapy, chemotherapy) [10], and follow-up duration that can influence recurrence rates making it challenging to compare recurrence rates between series (Table 3). Surgical margin status, an important factor predicting recurrence [9, 11, 13,14,15, 17, 19], can be an important outcome measure when comparing surgical techniques. Of the six cases that were margin positive for OSSN, four were treated with post-op topical chemotherapy, of which there were no cases of recurrence. Only 1 of the 2 positive margin cases that were observed developed recurrence, however resolved with topical immunotherapy/chemotherapy. We found that the rate of recurrence of OSSN after primary surgical resection with 2 mm was 4% compared to the weighted average of 19% in 12 studies [9,10,11, 13,14,15,16,17,18,19,20], and 15% in the six studies that performed surgical margins greater than 2 mm beyond the visible tumor [11, 13, 15, 16, 20, 24]. The recurrence rate was much lower (1.5%, 1/69 cases) with negative margins compared to positive margin (17%, 1/6 cases) and indeterminate groups (20%, 1/5 cases) again emphasizing the importance of achieving negative margins. Each of the three recurrences in our study were successfully treated with adjuvant therapy. Since the recurrence rate was high in the indeterminate group (20%, 1/5 cases) and was comparable to positive margin (17%, 1/6 cases), we recommend providing adjuvant topical therapy to not only all positive margins cases but also indeterminate margins cases. We are unable to compare recurrence rates in the indeterminate margin group with previous studies because such classification of margin status has not been reported and should be distinguished from margin status “unknown”. The recurrence of OSSN with negative histopathologic margins can be explained on the basis of “sampling error” induced by limited number of histopathologic sections of the sample or microscopic “skip area”. In addition, noncontiguous recurrence is not likely to be influenced by the status of the surgical margins.
Limitation
This study included only discreet tumors, which allow for visualization of the thickened epithelial edge as describe in the surgical procedure methods that in addition to excision received cryotherapy. All non-discreet tumors underwent topical therapy and were not included in this study. Another limitation is that 4 of the 15 studies did not disclose margin status, likewise, 5 of the studies did not discuss the excised margins measurement. In addition, in review of literature, recurrence rate was not only influence by the excised margin size but also use of cryotherapy (Table 3). However, our results are not surprising given the findings of a systematic review that concluded the optimal approach for minimizing the likelihood of disease persistence or recurrence was primary surgical excision followed by topical INFα2b for cases with positive surgical margins [30].
In conclusion, excision with 2 mm margin of CIN is not associated with high rates of positive surgical margins. While achieving low rates of local recurrence, the conjunctiva is conserved, thereby minimizing the need for amniotic membrane or free conjunctival grafts for conjunctival repair while preserving limbal stem cells. If surgical margins are positive or indeterminate, adjuvant topical therapy should be considered. All cases with positive margins that received postoperative adjuvant therapy did not develop recurrence.
Summary
What was known before
-
OSSN has a high incidence of recurrence without cryotherapy after resection.
What this study adds
-
Excision of OSSN with 2 mm margins is not associated with high rates of positive surgical margins.
References
Sayed-Ahmed IO, Palioura S, Galor A, Karp CL. Diagnosis and medical management of ocular surface squamous neoplasia. Expert Rev Ophthalmol. 2017;12:11–9.
Atallah M, Joag M, Galor A, Amescua G, Nanji A, Wang J, et al. Role of high resolution optical coherence tomography in diagnosing ocular surface squamous neoplasia with coexisting ocular surface diseases. Ocul Surf. 2017;15:688–95.
Raza SM, Habib A, Wang WL, Gildey PW, Conley AP, Nader ME, et al. Surgical management of primary skull base osteosarcomas: impact of margin status and patterns of relapse. Neurosurgery. 2020;86:E23–32.
Guech-Ongey M, Engels EA, Goedert JJ, Biggar RJ, Mbulaiteye SM. Elevated risk for squamous cell carcinoma of the conjunctiva among adults with AIDS in the United States. Int J Cancer. 2008;122:2590–3.
Lee GA, Hirst LW. Incidence of ocular surface epithelial dysplasia in metropolitan Brisbane. A 10-year survey. Arch Ophthalmol. 1992;110:525–7.
Napora C, Cohen EJ, Genvert GI, Presson AC, Arentsen JJ, Eagle RC, et al. Factors associated with conjunctival intraepithelial neoplasia: a case control study. Ophthalmic Surg. 1990;21:27–30.
Lee GA, Hirst LW. Retrospective study of ocular surface squamous neoplasia. Aust N Z J Ophthalmol. 1997;25:269–76.
Scott IU, Karp CL, Nuovo GJ. Human papillomavirus 16 and 18 expression in conjunctival intraepithelial neoplasia. Ophthalmology. 2002;109:542–7.
Tabin G, Levin S, Snibson G, Loughnan M, Taylor H. Late recurrences and the necessity for long-term follow-up in corneal and conjunctival intraepithelial neoplasia. Ophthalmology. 1997;104:485–92.
Peksayar G, Altan-Yaycioglu R, Onal S. Excision and cryosurgery in the treatment of conjunctival malignant epithelial tumours. Eye. 2003;17:228–32.
Sturges A, Butt AL, Lai JE, Chodosh J. Topical interferon or surgical excision for the management of primary ocular surface squamous neoplasia. Ophthalmology. 2008;115:1297–302.e1.
Shields CL, Shields JA. Tumors of the conjunctiva and cornea. Surv Ophthalmol. 2004;49:3–24.
Nanji AA, Moon CS, Galor A, Sein J, Oellers P, Karp CL. Surgical versus medical treatment of ocular surface squamous neoplasia: a comparison of recurrences and complications. Ophthalmology. 2014;121:994–1000.
Sudesh S, Rapuano CJ, Cohen EJ, Eagle RC Jr., Laibson PR. Surgical management of ocular surface squamous neoplasms: the experience from a cornea center. Cornea. 2000;19:278–83.
Palamar M, Kaya E, Egrilmez S, Akalin T, Yagci A. Amniotic membrane transplantation in surgical management of ocular surface squamous neoplasias: long-term results. Eye. 2014;28:1131–5.
Mirzayev I, Gunduz AK, Ozalp Ates FS, Ozcan G, Isik MU. Factors affecting recurrence after surgical treatment in cases with ocular surface squamous neoplasia. Int J Ophthalmol. 2019;12:1426–31.
Erie JC, Campbell RJ, Liesegang TJ. Conjunctival and corneal intraepithelial and invasive neoplasia. Ophthalmology. 1986;93:176–83.
Tunc M, Char DH, Crawford B, Miller T. Intraepithelial and invasive squamous cell carcinoma of the conjunctiva: analysis of 60 cases. Br J Ophthalmol. 1999;83:98–103.
McKelvie PA, Daniell M, McNab A, Loughnan M, Santamaria JD. Squamous cell carcinoma of the conjunctiva: a series of 26 cases. Br J Ophthalmol. 2002;86:168–73.
Gunduz K, Ucakhan OO, Kanpolat A, Gunalp I. Nonpreserved human amniotic membrane transplantation for conjunctival reconstruction after excision of extensive ocular surface neoplasia. Eye. 2006;20:351–7.
Zaki AA, Farid SF. Management of intraepithelial and invasive neoplasia of the cornea and conjunctiva: a long-term follow up. Cornea. 2009;28:986–8.
Kao AA, Galor A, Karp CL, Abdelaziz A, Feuer WJ, Dubovy SR. Clinicopathologic correlation of ocular surface squamous neoplasms at Bascom Palmer Eye Institute: 2001 to 2010. Ophthalmology. 2012;119:1773–6.
Kenawy N, Garrick A, Heimann H, Coupland SE, Damato BE. Conjunctival squamous cell neoplasia: the Liverpool ocular oncology centre experience. Graefes Arch Clin Exp Ophthalmol. 2015;253:143–50.
Gichuhi S, Macharia E, Kabiru J, Zindamoyen AM, Rono H, Ollando E, et al. Topical fluorouracil after surgery for ocular surface squamous neoplasia in Kenya: a randomised, double-blind, placebo-controlled trial. Lancet Glob Health. 2016;4:e378–85.
Pe'er J, Singh AD, Damato BE. Clinical ophthalmic oncology: eyelid and conjunctiva, vol. 2. Cham, Switzerland: Springer, Springer Nature Switzerland AG; 2019.
Singh AD, Damato BE. Clinical ophthalmic oncology: basic principles, vol. 1, 3rd ed. Cham, Switzerland: Springer, Springer Nature Switzerland AG; 2019.
Conway RM, Graue GF, Pelayes DE, Pe'er J, Wilson MW, Wittekind CW, et al. Conjunctival carcinoma. American Joint Committee on Cancer (AJCC). AJCC Cancer Staging Manual. 8th ed. New York: Springer; 2017.
Fraunfelder FT, Wingfield D. Management of intraepithelial conjunctival tumors and squamous cell carcinomas. Am J Ophthalmol. 1983;95:359–63.
Mercado CL, Pole C, Wong J, Batlle JF, Roque F, Shaikh N, et al. Surgical versus medical treatment for ocular surface squamous neoplasia: a quality of life comparison. Ocul Surf. 2019;17:60–3.
Siedlecki AN, Tapp S, Tosteson AN, Larson RJ, Karp CL, Lietman T, et al. Surgery versus interferon Alpha-2b treatment strategies for ocular surface squamous neoplasia: a literature-based decision analysis. Cornea. 2016;35:613–8.
Funding
This work was supported by an unrestricted departmental grant from Research to Prevent Blindness Challenge Grant, to the Cole Eye Institute, Cleveland Clinic.
Author information
Authors and Affiliations
Contributions
ADS was responsible for study concept and design. Acquisition, analysis, and interpretation of data done by RCB, HS, VR, CB, and GY. Drafting of the paper by RCB and ADS. Critical revision of the paper for important intellectual content performed by RCB, GY, and ADS. Administrative, technical, and material support by GY and ADS.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bowen, R.C., Soto, H., Raval, V. et al. Ocular surface squamous neoplasia: outcomes following primary excision with 2 mm margin and cryotherapy. Eye 35, 3102–3109 (2021). https://doi.org/10.1038/s41433-020-01353-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01353-5