Abstract
Background
Conjunctival papilloma is often resistant to treatment. Various therapies have been reported with no gold standard. The purpose of this study was to compare treatment outcomes after various therapies.
Methods
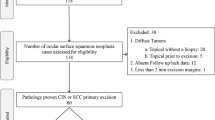
A retrospective chart review of 30 conjunctival papilloma patients from 2009–2020. Data on demographics, tumour characteristics, primary treatment and outcomes were collected. The primary outcome was the frequency of complete tumour resolution and recurrence rate of each primary therapy. The secondary outcome was treatment related side effects.
Results
The mean age was 57.5 years (3–93 years) with male predominance (n = 22, 73.3%). Eleven eyes were treated with interferon α-2b (IFN), seven with 5-fluorouracil (5FU), and 10 with excision biopsy and cryotherapy (6 with adjuvant therapy with IFN). The frequency of tumour resolution was 36.4% (4/11), 28.5% (2/7), and 100% (10/10) in each group, respectively. The mean time to resolution was faster in the surgical group compared to the medical group (1 day vs 159 days, p < 0.001). There was higher tumour recurrence with 11% in the surgical vs 0% in the medical group at 6 months and at 12 months, 22% recurrence in the surgical and 0% in the medical group (p = 0.52). However, the differences were not statistically significant.
Conclusion
Papilloma resolution is faster with surgical excision as compared to medical therapy. However, recurrences are more frequent after surgical versus medical treatment.
Similar content being viewed by others
Introduction
Conjunctival papilloma is a benign conjunctival tumour of epithelial origin [1, 2] and accounts for 1–16% of all conjunctival tumours [3,4,5,6]. It is typically seen in males between the ages of 20–40 [2, 6,7,8,9]. Similar to condyloma acuminata, it has a strong association with human papilloma virus(HPV) low risk type 6 and 11 [10, 11]. However, HPV high risk types 16, 18, 33 and 45 have also been reported in tissue PCR testing of conjunctival papillomas [1, 12,13,14,15,16,17,18]. Papilloma lesions can appear as solitary or multiple masses and can occur anywhere on the ocular surface with involvement of one or both eyes. In the paediatric age group, papillomas tend to be bilateral and multifocal in nature [1, 8, 9]. The clinical appearance of papilloma is divided into exophytic and inverted types. The exophytic subtypes, pedunculated and sessile, are the most common [19]. Lesions can be asymptomatic, or cause irritation, itching, and decreased visual acuity if the lesion encroaches on the visual axis. The diagnosis of conjunctival papilloma can be made clinically. The pathognomonic sign is a floppy, mobile papillary lesion with the presence of stalk at the base of tumour but lack thereof does not exclude the diagnosis [9].
Management of conjunctival papilloma remains a topic of debate. Traditionally, surgical excision with a “no touch” technique, described by Shields et al. has been recommended [20]. This technique describes tumour excision with a 2–4 mm wide margin without direct contact between the tumour and the surgical instruments. Double-freeze slow thaw cryotherapy is then applied to the conjunctival margin. The recurrence frequency of papilloma has been reported to be in the range of 3–27% [2, 6,7,8]. The potential for recurrence, especially in the paediatric age group, and the possible surgical complications of symblepharon and scar formation have highlighted the advantages of medication treatment [8, 9]. Several case reports have described successful outcomes using medical therapy for the treatment of primary and recurrent conjunctival papilloma, including interferon alfa-2b (IFN) [21,22,23,24,25,26], mitomycin C (MMC) [27,28,29], 5-fluorouracil (5FU) [9] and cimetidine [8, 30, 31]. A gap remains, however, as the literature on successful medical treatment of conjunctival papilloma is limited to case reports without comparisons between therapies. As such, in this study, we aimed to compare the treatment outcomes and side effects of the therapeutic options provided to our patients; IFN, 5FU, cimetidine, and surgical excision with adjunctive therapy. The primary outcomes were tumour resolution frequency and the recurrence rate of each therapy. Secondary outcomes were side effects of treatment.
Materials and methods
This retrospective study was approved by the University of Miami and Miami Veterans Affair Hospital Institutional Review Boards and was conducted in agreement with the principles of the Declaration of Helsinki and was compliant with the Health Insurance Portability and Accountability Act. A clinical database search for cases of conjunctival papilloma between January 2009 and December 2020 was performed at Bascom Palmer Eye Institute, University of Miami Miller School of Medicine, and the Miami Veterans Affairs Hospital. A retrospective chart review of all patients with clinical and/or pathologic diagnosis of conjunctival papilloma was conducted.
Demographic information including age, sex, race, and ethnicity was collected. Data on underlying medical history, immune status and ocular disease was obtained. The presence of cutaneous or genital papilloma was noted, if documented. History of prior treatment of papilloma was also noted, if applicable.
Collected clinical findings included laterality, number of papillomas per eye, location, size (broadest vertical and horizontal diameter) and configuration (pedunculated, sessile, or inverted), and associated features (feeder vessels, intrinsic vasculature, pigmentation). These were collected based on clinical description and verified by slit lamp photography, when available. Histopathologic report and HPV testing results were also noted if available.
Details on the primary treatment regimen was recorded. Generally, we prefer medical over surgical treatment and topical IFN was our first option. Topical 5FU was our next choice. We generally used cimetidine as an adjunct to topical therapy, but we did have one patient who did not want topicals and resolved with only the oral cimetidine. However, if the patient chose surgical treatment after the discussion of possible post-op complications including recurrence, we did the excisional biopsy with cryotherapy and usually with subconjunctival injection of interferon at the time of surgery. Individuals were grouped into categories based on their primary treatment. Individuals were placed into the medical treatment group if they received only medical therapy as a treatment for conjunctival papilloma. This included individuals who received IFN (topical or intralesional injection), 5FU (topical or intralesional injection), and/or oral cimetidine. Individuals were placed into the surgical treatment group if they underwent excisional biopsy of their lesions as primary treatment. Most individuals in the surgical group received a combination of intraoperative adjuvant therapy e.g., cryotherapy, intra-operative IFN injection, or MMC. Post-operative adjuvant therapy in each patient was also documented if present.
In general, topical IFN (1 MIU/ml) eyedrops were used 4 times daily until resolution of the papilloma. IFN (3 MIU/0.5 ml) injections were given every two weeks. Topical 5FU 1% was applied in cycles, 4 times daily for 1 week then a 3-week holiday. The treatment continued in cycle-fashioned until complete clinical resolution. 5FU (25 mg/0.5 ml) injections, when utilized, were given every 2 weeks. Oral cimetidine 800 mg was dosed 3 times daily. All patients in the surgical group had tumour excision using the “no touch” technique with adjunctive cryotherapy (double-freeze slow thaw). Often additional intraoperative adjunctive therapies such as an interferon injection or MMC were incorporated depending on the surgical planning. Post-operative adjunct medication was not routinely prescribed unless the histopathologic result showed positive margin of tumour.
Outcomes were categorized as complete tumour resolution or no resolution (which included both partial and no improvement). In addition, time to resolution and recurrence were noted, as applicable. Duration of treatment (in days) and side effects of treatment were also recorded.
IBM SPSS Statistics for Macintosh, Version 27.0 (IBM Inc., IL, USA) was utilized for the statistical analysis. Descriptive statistics were used to summarize demographics as well as tumour characteristics. Continuous variables were compared with independent student’s T-test. Categorical variables were compared with Chi-square. Kaplan-Meier survival analysis was used to calculate time to tumour resolution and time to tumour recurrence. Cox proportional hazard analysis was used to assess factors associated with time to resolution and recurrence rate. P values of less than 0.05 were considered statistically significant.
Results
Demographic data of the 30 patients is shown in Table 1. The mean age at diagnosis was 57.5 years (median 57 years, age range 3–93 years). The majority of patients were white (83.3%) and male (73.3%). Immunocompromised status (HIV n = 2, post splenectomy n = 1) was found in 10% of patient. No difference in demographic data was found between the medical and surgical groups.
Tumour characteristics grouped by primary treatment are shown in Table 1. Papilloma affected both eyes equally and no patient with bilateral involvement was found. Multiple papillomas were found in 5 patients of which three were adults. Both patients in the paediatric age group (n = 2) had multiple papillomas. Overall, there was a greater number of papillomas per eye in the surgical vs medical group (2.5 vs 1.15, p = 0.02). The bulbar and palpebral conjunctiva were the two most common locations for papilloma with equal frequency (33% both n = 10). Nasal papilloma was the most frequent location (13.3%, n = 16). Bulbar conjunctival papilloma, especially in the temporal region, were more likely to approached surgically (60%, n = 6) vs medically (20%, n = 4) p = 0.04. Caruncular and nasal bulbar papilloma were more likely to be managed with medical treatment, but the difference did not reach statistically significance (p = 0.37, p = 0.12, respectively).
Table 2. displays data on the primary treatments and outcomes in the medical group. Medical treatment included IFN (topical eyedrops in 10, intralesional injection in 1 patient), 5FU (topical eyedrops in 6, injection in 1 patient), both IFN and 5FU (IFN intralesional injection and topical 5FU eyedrops in 1 patient), and oral cimetidine (primary therapy in 1, adjunctive with IFN in 3, adjunctive with 5FU in 6 patients).
Complete tumour resolution was noted in 35% of patients in the medical group. The mean time to resolution in medication group was 159 days (SD 98, range 21–330 days). In individuals whose papilloma did not resolve with medical therapy (n = 13, 65%), partial resolution was observed in 45.4% (5 of 11) of IFN patients and 28.5% (2 of 7) of 5FU patients. Table 3 shows a summary of further management in each case.
All patients in surgical group had “no touch” excision technique with adjunctive cryotherapy. In addition, further intraoperative therapy was given including intraoperative IFN injection [6], MMC application [2] and, absolute alcohol on corneal surface [1]. Five were closed with AMT.
In the surgical group, histopathologic confirmation was obtained in all patients. Of note, 2 of the surgical patients had positive surgical margins, one of which had a recurrence 6 weeks after surgery. This patient was then treated with topical 5FU eyedrops and was cured. The other patient with positive margins was empirically treated with 2 cycles of topical 5FU eyedrops beginning 8 weeks post-operatively and did not recur.
Overall, the surgery group had a high frequency of tumour resolution compared to the medical group (100% vs 35%, p = 0.001) and a shorter mean time to tumour resolution (Fig. 1-A)
Recurrence rates were assessed in the 17 individuals (7 medical, 10 surgical) who achieved complete tumour resolution. Kaplan-Meier survival analysis showed no recurrences in the medical group at 6 months and 1 year and the surgical group had recurrences of 11% at 6 months and 22% at 1 year (Fig. 1-B). One patient in the medical group recurred at 24 months, and the overall frequency of recurrence was 14% in medical group (1 of 7) and 30% (3 of 10) in surgical group (p = 0.52). Superior papilloma location increased the risk for recurrence (hazard ratio (HR) 13.97; p = 0,06; 95%CI 0.87–223.65) on univariate Cox-regression modelling, this approached but did not reach statistical significance.
Representative clinical photos demonstrating response to medical and surgical treatment are presented in Fig. 2.
Regarding side effects, one patient was noted to have conjunctivitis during topical 5FU eyedrop treatment and was empirically treated with topical antibiotic. Two patients experienced gastrointestinal tract problem (e.g. diarrhoea) during treatment with oral cimetidine. No side effects were found in IFN α-2b eyedrop group. Patients receiving IFN subconjunctival injections had transient fever/chills. In surgical group, 4 patients developed post-operative symblepharon and scarring.
Discussion
In this study, we identified 30 individuals with papilloma and found that while surgery led to immediate resolution of papilloma, the frequency of recurrence was higher after surgical vs medical treatment, although the difference was not statistically significant. Overall, our patient demographics are similar to prior reports in that we noted a male predominance [2, 4, 7, 8]. However, our patients were older (mean age 57.5 years) compared to other papers, where the mean age at diagnosis ranged from 39–47 years [2, 7, 8]. Lesion location in our study was also consistent with prior reports, with bulbar conjunctiva [6], palpebral conjunctiva [2] and caruncle [4, 7, 8] reported as the most common locations in different studies. Interestingly, a possible explanation of why the medial and inferior locations of papilloma formation are so common has been postulated. A combination of tear flow from the superolateral fornix to the inferonasal lacrimal drainage system coupled with eye rubbing causing HPV autoinoculation is the hypothesized mechanism [2].
Tumour resolution frequency was significantly higher (100% vs 35%) and faster in the surgical group vs medical group. This outcome was expected as excisional biopsy removed all clinically visible lesions by the first day post-operatively. Cimetidine, IFN, and 5FU were the medications most often used as primary therapy in our study.
Cimetidine, a H2-receptor antagonist agent, is commonly used for peptic ulcer management. When used at high dosage of 30–40 mg/kg, it has been shown to have immunomodulatory effect [30, 32, 33]. Due to this property, oral cimetidine has been reported to be useful in management of various systemic and cutaneous diseases such as treatment for recurrent respiratory papillomas [32, 34, 35]. Shields et al. reported a case of recurrent conjunctival papilloma in a 9-year-old boy that achieved nearly complete resolution after 4 months using oral cimetidine alone [30]. In our study, we have only one adult patient who received oral cimetidine as sole therapy, which also achieved complete tumour resolution. While not specifically indicated for children, it has been used in the paediatric population for respiratory and cutaneous papillomatosis and further studies are needed. The number of patients is too small to make any conclusion regarding its efficacy.
IFN, a glycoprotein with antiviral, antitumour and immunomodulatory effect, is thought to act by enhancing the host innate immune response and reducing the viral load of HPV in infected conjunctival cells [36]. The first use of IFN in conjunctival papilloma was reported by Schechter et al in 2002 [21]. In his paper, both patients achieved complete resolution of papilloma after treatment with topical IFN 1 MIU/ml four times daily for 6 weeks and 3 months. No recurrences were noted after 18 and 40 months of follow up, respectively. Since then, 8 additional publications, encompassing 8 additional patients, reported outcomes of IFN as a treatment for papilloma. Combining studies, a 70% resolution frequency (7 of 10) was reported, which is higher than in our current study (35%) [12, 22,23,24, 26, 37,38,39]. However, positive-result publication bias likely explains this discrepancy to some degree. In the literature, recurrent papillomas were less likely to completely respond to IFN therapy (2 of 4) [12, 21, 24, 38] than primary papilloma (5 of 6) [21,22,23, 26, 37, 39]. Failure of response to topical IFN but full response to topical MMC in an immunocompromised patient (on oral tacrolimus after liver transplantation) suggests that possibly host immune responses may be a necessary factor for response to IFN [39]. Overall, our treatment range of 21–210 days is consistent with prior reports that ranged from 14–240 days [21,22,23, 26]. In the current study, all cases that achieved resolution were treated with topical IFN eye drops. Resolution3333 was not achieved in eyes treated with IFN injections alone (n = 1), despite intralesional IFN demonstrating benefit in ocular surface squamous neoplasm (OSSN) [40]. The number treated with IFN injections is too small to make a conclusion on efficacy.
Topical 5FU, an antimetabolite drug that inhibits DNA formation by blocking the enzyme thymidylate synthetase, is an effective treatment of choice for OSSN in our institution [41]. However, only sparse data are available on its use in papilloma. Two studies, encompassing 3 patients reported on the use of 5FU in conjunctival papilloma [9, 12]. One study reported complete lesion resolution in a 78-year-old female after 6 cycles of topical 1% 5FU. However, the patient had a tumour recurrence at 11 months [9]. Another study reported two individuals (34-year-old female and a 71-year-old male) who did not achieve lesion resolution despite topical 5FU use (length of treatment not specified) [12]. Overall, our frequency of resolution (28.5%) is similar to that of the literature (33%).
When comparing between the two main medications given in this study, a higher frequency of individuals experienced resolution with IFN versus 5FU. However, due to a small number of patients in each medication subgroup, it is not possible to robustly compare the groups. Of note, both medications showed a good safety profile with no serious side effects.
A major finding in this paper is that individuals treated with medical therapy had fewer recurrences than those treated with surgical therapy, although the numbers did not reach statistical significance. Overall, our recurrence frequency in the surgical group of 30% was higher to that reported for papilloma in the prior literature (recurrence frequency 3–27%) [2, 6,7,8]. In one study, the recurrence frequency of papilloma was 22.7% (n = 22), with adjunctive cryotherapy lowering that frequency from 50 to 7%[7]. The lowest recurrence frequency (3% over a 36 month follow up period) comes from a paper that examined outcomes in 64 individuals with papilloma (some individuals had multiple lesions). This may be due to the fact that the majority of tumours (92%, n = 91) underwent surgical removal with cryotherapy and postoperative treatment (oral cimetidine and/or topical IFN for 3 months after surgery) [8]. All patients in our surgical group received adjuvant cryotherapy. However, our recurrence rate was 22% at 1 year. This discrepancy from the published literature may be due in part to viral shedding at the time of excision or the fact that we had a larger portion of multiple papillomas in this subgroup. Our findings support the current debate that recurrences are more common after surgical excision than reports suggest [8, 9, 42]. Our findings suggests that more data is needed regarding optimal post-operative adjuvant therapy for papillomas that are surgically excised.
Our study findings must be considered in light of its limitations which included a retrospective analysis with non-standard treatment in a limited number of patients. However, the strength of our study is that it represents the largest cohort treated with topical medication, both IFN and 5FU, and a comparative surgical group.
The clinical implication of this study is that while surgical excision has a faster time to resolution, medical therapy may have the advantage of less frequent recurrences. Perhaps a combination of medical and surgical treatment would be optimal, and this is a subject for future study. Furthermore, the benefits of medical therapy must be considered along with potential out-of-pocket costs to the patients (a monthly supply of IFN in the United States is ~800USD and 5FU ~50 USD). Future research is needed to optimize both the time to resolution and frequency of recurrence in papilloma, identify new treatment modalities, and to evaluate which patient and tumour factors influence resolution and recurrence.
Summary
What was known before
-
Conjunctival papilloma is often resistant to treatment. Various therapies have been reported with no gold standard treatment.
What this study adds
-
Papilloma resolution is faster with surgical excision as compared to medical therapy. However, recurrences are more frequent after surgical versus medical treatment.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Shields CL, Shields JA. Tumors of the conjunctiva and cornea. Surv Ophthalmol. 2004;49:3–24.
Sjö N, Heegaard S, Prause JU. Conjunctival papilloma. Acta Ophthalmol Scand. 2000;78:663–6.
Asadi-Amoli F, Ghanadan A. Survey of 274 patients with conjunctival neoplastic lesions in Farabi Eye Hospital, Tehran 2006–2012. J Curr Ophthalmol. 2015;27:37–40.
Shields CL, Alset AE, Boal NS, Casey MG, Knapp AN, Sugarman JA, et al. Conjunctival tumors in 5002 cases. comparative analysis of benign versus malignant counterparts. The 2016 James D. Allen Lecture. Am J Ophthalmol. 2017;173:106–33.
Shields CL, Demirci H, Karatza E, Shields JA. Clinical survey of 1643 melanocytic and nonmelanocytic conjunctival tumors. Ophthalmology. 2004;111:1747–54.
Ash JE. Epibulbar tumors*. Am J Ophthalmol. 1950;33:1203–19.
Huang Y-M, Huang Y-Y, Yang H-Y, Tsai C-C, Yu W-K, Kao S-C, et al. Conjunctival papilloma: Clinical features, outcome, and factors related to recurrence. Taiwan J Ophthalmol. 2018;8:15–8.
Kaliki S, Arepalli S, Shields CL, Klein K, Sun H, Hysenj E, et al. Conjunctival Papilloma: Features and Outcomes Based on Age at Initial Examination. JAMA Ophthalmol. 2013;131:585.
Theotoka D, Morkin MI, Galor A, Karp CL. Update on diagnosis and management of conjunctival papilloma. Eye Vis. 2019;6:18.
Yanofsky VR, Patel RV, Goldenberg G. Genital warts. J Clin Aesthetic Dermatol. 2012;5:25–36.
Aubin F, Prétet J-L, Jacquard A-C, Saunier M, Carcopino X, Jaroud F, et al. Human papillomavirus genotype distribution in external acuminata condylomata: a large French National Study (EDiTH IV). Clin Infect Dis. 2008;47:610–5.
de Keizer RJW, de Wolff-Rouendaal D. Topical alpha-interferon in recurrent conjunctival papilloma. Acta Ophthalmol Scand. 2003;81:193–6.
Hanbazazh M, Gyure KA. Ocular human papillomavirus infections. Arch Pathol Lab Med. 2018;142:706–10.
Minchiotti S, Masucci L, Santos MSD, Perrella E, Graffeo R, Lambiase A, et al. Conjunctival papilloma and human papillomavirus: identification of HPV types by PCR. Eur J Ophthalmol. 2006;16:473–7.
Sjö NC, von Buchwald C, Cassonnet P, Norrild B, Prause JU, Vinding T, et al. Human papillomavirus in normal conjunctival tissue and in conjunctival papilloma: types and frequencies in a large series. Br J Ophthalmol. 2007;91:1014–5.
Sjö NC, Heegaard S, Prause JU, von Buchwald C, Lindeberg H. Human papillomavirus in conjunctival papilloma. Br J Ophthalmol. 2001;85:785–7.
Verma V, Shen D, Sieving PC, Chan C-C. The role of infectious agents in the etiology of ocular adnexal neoplasia. Surv Ophthalmol. 2008;53:312–31.
Ramberg I, Heegaard S. Human papillomavirus related neoplasia of the ocular adnexa. Viruses. 2021;13:1522.
Mannis M, Holland E Cornea [Internet]. 4th ed. Elsevier; 2016 [cited 2020 Apr 15]. 2016 p. Available from: https://www.elsevier.com/books/cornea-2-volume-set/mannis/978-0-323-35757-9
Shields JA, Shields CL, De, Potter P. Surgical management of conjunctival tumors. The 1994 Lynn B. McMahan Lecture. Arch Ophthalmol Chic Ill 1960. 1997;115:808–15.
Schechter BA, Rand WJ, Velazquez GE, Williams WD, Starasoler L. Treatment of conjunctival papillomata with topical interferon Alfa-2b. Am J Ophthalmol. 2002;134:268–70.
Morgenstern KE. Long-term administration of topical interferon Alfa-2β in the treatment of conjunctival squamous papilloma. Arch Ophthalmol. 2003;121:1052.
Falco LA, Gruosso PJ, Skolnick K, Bejar L. Topical interferon alpha 2 beta therapy in the management of conjunctival papilloma. Optom St Louis Mo. 2007;78:162–6.
Kothari M, Mody K, Chatterjee D. Resolution of recurrent conjunctival papilloma after topical and intralesional interferon α2b with partial excision in a child. J Am Assoc Pediatr Ophthalmol Strabismus. 2009;13:523–5.
Muralidhar R, Sudan R, Bajaj MS, Sharma V. Topical interferon α-2b as an adjunctive therapy in recurrent conjunctival papilloma. Int Ophthalmol. 2009;29:61–2.
Bolek B, Wylęgała A, Teper S, Kokot J, Wylęgała E Treatment of conjunctival papilloma with topical interferon alpha-2b - case report. Medicine (Baltimore) [Internet]. 2020 Feb [cited 2021 Feb 7];99. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7035065/
Hawkins AS, Yu J, Hamming NA, Rubenstein JB. Treatment of recurrent conjunctival papillomatosis with mitomycin C. Am J Ophthalmol. 1999;128:638–40.
Parrozzani R, Frizziero L, Midena E. Giant ocular surface squamous cell papilloma treated with topical mitomycin C. JAMA Ophthalmol. 2017;135:e170681.
Yuen HKL, Yeung EFY, Chan NR, Chi SCC, Lam DSC. The use of postoperative topical mitomycin C in the treatment of recurrent conjunctival papilloma. Cornea 2002;21:838–9.
Shields CL, Lally MR, Singh AD, Shields JA, Nowinski T. Oral cimetidine (Tagamet) for recalcitrant, diffuse conjunctival papillomatosis. Am J Ophthalmol. 1999;128:362–4.
Chang S-W, Huang Z-L. Oral cimetidine adjuvant therapy for recalcitrant, diffuse conjunctival papillomatosis. Cornea 2006;25:687–90.
Harcourt JP, Worley G, Leighton SEJ. Cimetidine treatment for recurrent respiratory papillomatosis. Int J Pediatr Otorhinolaryngol. 1999;51:109–13.
Takeuchi Y, Shigemura T, Kobayashi N, Nagumo H, Furumoto M, Ogasawara K, et al. Clinical features and new diagnostic criteria for the syndrome of periodic fever, aphthous stomatitis, pharyngitis, and cervical adenitis. Int J Rheum Dis. 2019;22:1489–97.
Patel A, Orban N. Infantile recurrent respiratory papillomatosis: review of adjuvant therapies. J Laryngol Otol. 2021;135:958–63.
Das BB, Anton K, Soares N, Riojas S, Mcdermott J, Knox L, et al. Cimetidine: a safe treatment option for cutaneous warts in pediatric heart transplant recipients. Med Sci Basel Switz. 2018;6:E30.
Lewczuk N, Zdebik A, Bogusławska J. Interferon alpha 2a and 2b in ophthalmology: a review. J Interferon Cytokine Res J Int Soc Interferon Cytokine Res. 2019;39:259–72.
Parulekar MV, Khooshabeh R, Graham C. Topical and intralesional interferon therapy for recurrent lacrimal papilloma. Eye 2002;16:649–51.
Singh M, Gautam N, Gupta A, Kaur M. Interferon alfa-2b in the management of recurrent conjunctival papillomatosis. Indian J Ophthalmol. 2016;64:778–80.
Ganapathy PS, Plesec T, Singh AD. Conjunctival squamous papilloma refractory to interferon α-2b in a patient on systemic immunosuppression (tacrolimus). Am J Ophthalmol Case Rep. 2017;6:1–3.
Al Bayyat G, Arreaza-Kaufman D, Venkateswaran N, Galor A, Karp CL. Update on pharmacotherapy for ocular surface squamous neoplasia. Eye Vis. 2019;6:24.
Joag MG, Sise A, Murillo JC, Sayed-Ahmed IO, Wong JR, Mercado C, et al. Topical 5-fluorouracil 1% as primary treatment for ocular surface squamous neoplasia. Ophthalmology. 2016;123:1442–8.
Tseng S-H. Conjunctival papilloma. Ophthalmology. 2009;116:1013.e1.
Funding
NIH Center Core Grant P30EY014801, RPB Unrestricted Award and Career Development Awards, The Dr. Ronald and Alicia Lepke Grant, The Lee and Claire Hager Grant, The H. Scott Huizenga Grant, The Grant and Diana Stanton-Thornbrough Grant, The Robert Baer Family Grant, The Emilyn Page and Mark Feldberg Grant, The Jose Ferreira de Melo Grant, The Robert and Virginia Farr Grant, The Richard and Kathy Lesser Grant, The Michele and Ted Kaplan Grant, The Calvin and Flavia Oak Foundation, The Honourable A. Jay Cristol Grant, The Carol Soffer Grant, The Christian Kathe Grant, and The Richard Azar Family Grant (Dr. Karp/institutional grants), Mr. and Mrs. Irwin Friedman Grant, The Roberto and Antonia Menendez Family Grant, The Stephen Takach Grant, The Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Clinical Sciences R&D (CSRD) I01 CX002015 (Dr. Galor) and Biomedical Laboratory R&D (BLRD) Service I01 BX004893 (Dr. Galor), Department of Defense Gulf War Illness Research Program (GWIRP) W81XWH-20-1-0579 (Dr. Galor) and Vision Research Program (VRP) W81XWH-20-1-0820 (Dr. Galor), National Eye Institute R01EY026174 (Dr. Galor) and R61EY032468 (Dr. Galor), and Research to Prevent Blindness Unrestricted Grant (institutional). Nikolaidis institution (Dr. Theotoka).
Author information
Authors and Affiliations
Contributions
WS: conception of the study, data acquisition, analysis and draughting the manuscript. DT: data acquisition and analysis. MZ: data acquisition and draughting the manuscript. AG: conception of the study, data analysis, critical revision of the manuscript. CK: conception of the study, data analysis, final approval of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sripawadkul, W., Theotoka, D., Zein, M. et al. Conjunctival papilloma treatment outcomes: a 12-year-retrospective study. Eye 37, 977–982 (2023). https://doi.org/10.1038/s41433-022-02329-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02329-3
This article is cited by
-
Ocular oncology demystified
Eye (2022)