Abstract
This study aimed to examine the implications of reporting heterozygous losses of recessive genes in Chromosomal Microarray Analysis (CMA), based on the incidence of microdeletions of three common hearing impairment genes in the local cohort and the prevalence of sequence variants in these genes in worldwide databases. Prevalence of heterozygous microdeletions in OTOA and STRC genes, as well as deletions in the DFNB1 locus encompassing GJB6 gene, was determined using electronic database of Rabin Medical Center. ClinVar archive and Deafness Variation Database were used to generate a list of clinically significant sequence variants in these three genes, as well as GJB2 gene, and estimation of the frequency of sequence variants was performed. Of the 19,189 CMA tests were performed in our laboratory, 107 STRC microdeletions were found (0.56%), followed in frequency by OTOA deletions (39, 0.2%), and DFNB1 locus deletions (10, 0.05%). The estimated risk for a hearing loss in the examined individual carrying the microdeletion was estimated as 0.11–0.67% for STRC, 0.016–0.13% for OTOA, and 1.9–7.5% in the DFNB1 locus (including double heterozygocity with GJB2 clinically significant sequence variants). The risks were higher in specific populations. In conclusion, we believe that that general decision whether to report or to disregard such incidental findings cannot be part of a uniform policy, but rather based on a detailed evaluation of origin-specific variants for each gene, with a careful consideration and discussion whether to include the microdeletion in the final report for each patient.
Similar content being viewed by others
Introduction
Chromosomal Microarray Analysis (CMA) is currently the test of choice in patients with neurodevelopmental disorders and/or congenital anomalies, as well as in fetuses with structural aberrations [1]. In addition, it has been shown that CMA can detect clinically significant (i.e., pathogenic and likely pathogenic) copy number variants (CNVs) in up to 1.4% of low-risk pregnancies [2].
When done in whole genome approach, CMA testing can detect copy number losses encompassing genes for recessive disorders, diagnosing a carrier state. As such findings are not expected to influence the health status of the examined patient, while on the other hand may be associated with morbidity in case of sequence variants in the second allele and with future morbidity of the offspring, the duty to report these CNVs is controversial. The first version of American College of Medical Genetics and Genomics (ACMG) standards and guidelines for interpretation and reporting of postnatal constitutional CNVs, published in 2011, stated that “comprehensive reporting of heterozygous recessive variants is outside the scope of the intended use of these tests and, in general, is not recommended. Disclosure of recessive variants may be considered in cases of well-characterized recessive disorders, for which carrier frequency is reasonably high in the patient population and/or carrier screening is commonly available, or in recessive disorders with clinical features consistent with the patient’s reason for referral” [3]. The 2014 Belgian prenatal array guidelines state that “carriership for an autosomal recessive condition will only be communicated if the carrier frequency is sufficiently high (with a cut-off on 1:50)” [4]. The 2019 European guidelines for constitutional cytogenomic analysis state that benign and likely benign variants “are not to be included in the final report, unless, for example, it concerns a loss encompassing a recessive disease gene matching the clinical phenotype of the patient” [5]. Similarly, the 2016 Israeli guidelines state that “routine detailed reporting of CNVs associated with carrier state for recessive disorders is not recommended”. The updated 2019 ACMG guidelines, however, state that “there are some situations when disclosure of carrier status is recommended” (rather than “may be considered”), such as “well-characterized disorders where loss of function is the established disease mechanism” [6]. This lack of uniformity has led various laboratories to consider reporting all heterozygous deletions encompassing autosomal recessive disease genes.
In this study, we aimed to examine the prevalence of heterozygous microdeletions encompassing genes of autosomal recessive inheritance in a large cohort of microarray analyses, and to estimate the risk for affected offspring in case these findings are reported.
As a pilot model, we focused on three genes associated with autosomal recessive non-syndromic hearing impairment: OTOA gene (OMIM #607038), STRC gene (OMIM #606440) and GJB6 gene (OMIM #604418). These genes were chosen as relatively common causes of autosomal recessive hearing loss, known for many years, and having a well-defined and early onset phenotype. In addition, both numerous sequence variants and recurrent microdeletions in these genes are known to be associated with the phenotype. Finally, genetic variants in these genes are universal to all populations and not unique to a particular ethnic origin.
Thus, the purpose of our study was to examine the implications of reporting heterozygous losses of recessive genes in CMA tests, based on the incidence of microdeletions of three common hearing impairment genes in the local cohort and the prevalence of sequence variants in these genes in worldwide databases.
Methods
The steps undertaken to estimate the implications of reporting heterozygous microdeletions in the examined genes are presented in Fig. 1.
1. Calculation of estimated prevalence of heterozygous microdeletions in OTOA and STRC genes, and deletions in the DFNB1 locus
Due to paucity of data in medical literature or professional databases regarding the prevalence of such CNVs, a search was performed using the electronic database of Genetic laboratory of Rabin Medical Center (one of the largest Israeli genetic laboratories) through the years 2013–March 2020.
CMA analysis
The CMA analysis was performed using two single-nucleotide polymorphism–based array platforms:
-
1.
Illumina (San Diego, CA) during the years 2013–2016 [7].
-
2.
CytoScan 750K array (Affymetrix, Santa Clara, CA, USA) now part of Thermo Fisher Scientific (Thermo Fisher Scientific, Inc.; Waltham, MA, USA), between 2017 and 2019 [8].
The data were analyzed by Nexus Copy Number software 7.5 (BioDiscovery, El Segundo, CA, USA) and Chromosome Analysis Suite (ChAS) v3.1software (Thermo Fisher Scientific, Inc), respectively.
Our local database includes prenatal samples of amniotic fluid or chorionic villi sampling, as well as postnatal microarray analyses. Prenatal CMA tests are performed in two major groups: fetuses with abnormal sonographic findings, and low-risk pregnancies (which include parental request, advanced maternal age, soft sonographic markers for chromosomal abnormality and abnormal maternal screening for common trisomies). Postnatal DNA samples are drawn from blood of individuals with congenital malformations or neurodevelopmental disorders, or from healthy and phenotypically normal individuals performing microarray testing due to demonstration of various microarray findings in their children/fetuses (mostly due to variants of uncertain significance).
For the data analysis, we excluded patients with hearing loss. In addition, we excluded any family members of cases with previously diagnosed OTOA, STRC and DFNB1 locus microdeletions, such that only one case with specific microdeletion was included in the final analysis.
The search for microdeletions encompassing the examined genes was performed using the following coordinates by the human genome assembly GRCh37 (hg19) in UCSC Genome Browser (https://genome.ucsc.edu/index.html):
- STRC gene - chromosome 15: 44,006,787-44,010,016.
- OTOA gene - chromosome 16: 21,689,835-21,772,050.
- GJB6 gene - chromosome 13: 20,796,110-20,806,534.
The prevalence of microdeletions encompassing the examined genes was presented as percentage with 95% confidence intervals, as well as ratios. In addition, we performed a comparison of prenatal vs. postnatal frequency of microdeletions, as well as comparison between these frequencies in fetuses with abnormal ultrasound vs. low-risk pregnancies, and between cases vs. healthy controls, using the Chi-square calculator with Yates’ correction. This subgroup comparison was done to examine whether the whole cohort can be used as one single group to represent the general population.
The study was approved by the Institutional Review Board (no. of approval 0231-15, date of approval April 27, 2015).
2. Calculation of the estimated prevalence of sequence variants in OTOA, STRC, and GJB2 genes
ClinVar archive was used (https://www.ncbi.nlm.nih.gov/clinvar/) to generate a list of sequence variants in the examined genes [9]. The search was restricted to pathogenic and/or likely pathogenic, single gene, variant length <51 bp in size, and method type of “clinical testing”. In addition, a list of sequence variants was generated in GJB2 gene, causing autosomal recessive deafness-1B in the form of double heterozygosity with deletions in DFNB1 locus. As variants in GJB6 do not cause non-syndromic hearing loss, this gene was not included in the analysis.
We used Genome Aggregation Database as the preferred data set to retrieve the allele frequency of each variant (due to highest number of examined individuals) [10]. If data were unavailable regarding the specific variant, it was retrieved from Exome Aggregation Consortium, followed by dbSNP and any available data set.
Additional generation and estimation of the frequency of sequence variants was performed using Deafness Variation Database (DVD: http://deafnessvariationdatabase.org/) [11], summarizing the frequencies of pathogenic and likely pathogenic sequence variants.
In addition, a meta-analysis of Mahdieh and Rabbani was used for the ethnic-specific carrier frequency of the common GJB2 variant (35delG) [12]. Finally, the frequency of STRC, OTOA, and GJB2 sequence variants in Ashkenazi Jewish population in Israel was calculated, according to the Israel National Genetic Database https://medicine.ekmd.huji.ac.il/En/INGD/Pages/default.aspx).
3. Statistical analysis for estimated risk calculation
3a. Calculation of the estimated risk for hearing impairment in an individual diagnosed with microdeletion encompassing OTOA, STRC genes or DFNB1 locus (including prenatal CMA):
In this case, hearing impairment could be caused by the presence of a sequence variant on the other allele, inherited from the second parent. Thus, the risk for hearing loss was estimated as the prevalence of sequence variants divided by two.
3b. Calculation of the estimated risk for an affected child in case of a parent carrying a microdeletion encompassing OTOA, STRC genes or DFNB1 locus:
To calculate the chance for a child with hearing loss for a parent carrying a microdeletion encompassing OTOA, STRC gene or DFNB1 locus, the chances to be diagnosed with a microdeletion were summed with the frequency of sequence variants, and divided by four, in concordance with Mendelian inheritance principles (Fig. 1). This risk was considered as the number of partners needed to be examined to detect one affected child.
In addition, a separate calculation was performed for the risk for Deafness-Infertility syndrome (DIS) in microdeletions encompassing STRC and CATSPER2 genes (OMIM #611102).
Results
Patient cohort
Overall, 19,189 CMA tests were performed in our laboratory from 2013 to March 2020. Of these, 13,121 tests were performed using Illumina platform, while additional 6068 CMA tests were performed during 2017–2020 using Cytoscan array (Table 1).
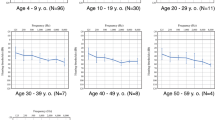
Cohort examined by Illumina platform is thoroughly described in a previous manuscript [7]. Briefly, single parental origin was reported in 22.6% of the patients, two origins were observed in 23.1%, multiple origins in 30.3%, while in 24% the origin was not reported. Of the patients with single parental origin, the largest proportions belonged to Ashkenazi Jewish descent (65.6%) and Muslim Arabs (15.2%). Yemenite Jews, Druze, Uzbekistan Bukharan Jews, Moroccan Jews, and Bedouins constituted between 2 and 3% each.
As in samples examined by Cytoscan array a separate annotation was given to maternal and paternal origin, the analysis of allele frequency could be performed in more details (Table 2). In this population, the most prevalent origins were full or partial Ashkenazi Jews (34.9%), followed by Moroccan Jews (12.2%), Iraqi Jews (9.6%), Yemen Jews (7.0%), Iranian Jews (4.9%), and Muslim Arabs (4.8%).
Estimated prevalence of heterozygous microdeletions in OTOA, STRC genes and DFNB1 locus
The frequency of microdeletions encompassing OTOA, STRC, genes and DFNB1 locus, including 95% confidence intervals is presented in Table 1 and Supplementary Table 1. Overall, 156 deletions were found (0.81%, one in 123). STRC deletions were the most common, yielding a frequency of one in every 179 CMA tests (0.56%). It must be noted that all the detected microdeletions in STRC gene encompassed CATSPER2 gene. Second in their prevalence OTOA deletions were noted, involving one in every 492 CMA tests (0.2%), while the lowest prevalence was noted in the occurrence of microdeletions in the DFNB1 locus, approaching one in every 2000 CMA tests. The CNVs were submitted to ClinVar database—SUB8692904.
No statistically significant differences were noted between all the subgroups (i.e., prenatal vs. postnatal cohorts, fetuses with abnormal ultrasound vs. low-risk pregnancies, and between cases vs. healthy controls) (Table 1).
Allele frequency of microdeletions by specific origins is presented in Table 2. Looking at origins with over 100 representative subjects, the highest frequency of STRC microdeletions was noted in Greece Jews (2.23%), OTOA microdeletions—in Bukhara Jews (1.21%), and microdeletions in the DFNB1 locus—in Egypt Jews (0.28%).
Estimated prevalence of sequence variants in OTOA, STRC, and GJB2 genes
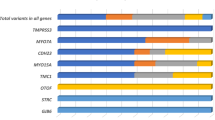
ClinVar database search for pathogenic and likely pathogenic sequence variants in the examined genes (April 30, 2020) yielded 27 variants in STRC gene, and 10 in OTOA gene (Supplementary Table 2). In addition, 105 variants were found in GJB2 gene.
The highest allele frequency of sequence variants was shown in the GJB2 gene—3.8%, or one in 26 (Table 2). Second was the STRC gene—0.21% (one in 477), followed by the OTOA gene—0.03% (one in 3165).
DVD search (February 9, 2021) yielded 80 variants in STRC gene, 44 in OTOA gene, and 428 in GJB2 gene (Supplementary Table 3). Summary of the frequencies yielded higher numbers for the three examined genes compared to ClinVar database: 1.34 vs. 0.21 for STRC, 0.26 vs. 0.032 for OTOA, and 15.1% vs. 3.79% for GJB2 variants, respectively.
Calculation of the estimated morbidity risks for an affected individual/future child
Based on the frequency of DVD sequence variants, the risk for a hearing loss in an individual carrying STRC microdeletion was estimated as 0.67 (one in 149), and the risk for a child with hearing impairment for a parent carrying a heterozygous STRC microdeletion was estimated as 0.48%, or one in 210 (Table 3). The risks were lower for OTOA microdeletions: 0.13% for an affected individual, and 0.12% for an affected child.
As the rate of sequence variants in GJB2 gene was 15.1%, the highest risks for hearing loss were demonstrated in heterozygous carriers of microdeletions in the DFNB1 locus—7.53% risk for hearing loss in a carrier individual (one in 13), and a 3.78% risk for an affected double heterozygous child (one in 24).
The risk for Deafness-Infertility syndrome in the progeny of individuals carrying a microdeletion encompassing STRC and CATSPER2 genes was estimated as 1/2*0.56%*1/2 = 0.14%, or one in 714.
In addition, judging by the ethnic-specific carrier frequency of the 35delG variant in GJB2 gene [12], the risk for a child with hearing loss for parent with incidentally diagnosed microdeletion in the DFNB1 locus can reach up to 1:205 if the second spouse is of European origin, and up to 1:250 in Australian and certain American origin (Table 4).
Finally, risks for Ashkenazi Jewish population are presented in Table 5. According to the Israel National Genetic Database, the frequency of a founder c.4171 C > G (p.(Arg1391Gly)) STRC variant in Israeli Ashkenazi Jewish population is 0.5%. Thus, the risk for hearing loss in an individual carrying STRC microdeletion was estimated as 0.25% (one in 400). Combined with a 1.35% prevalence of STRC microdeletions in this origin, the risk for a child with hearing loss for a parent carrying an incidental STRC microdeletion, with an Ashkenazi Jewish spouse, is 0.46%, or one in 216. The risk for Deafness-Infertility syndrome in the progeny of Ashkenazi Jewish individuals carrying a microdeletion encompassing STRC and CATSPER2 genes is 0.34%, or one in 296.
Moreover, the overall prevalence of GJB2 sequence variants in Ashkenazi Jewish population was calculated as 7.23%, i.e., one in 14 (a sum of 0.75% for c.35delG, 1.6% for c.109 G > A, 1.6% for c.101 T > C, 3.26% for c.167delT, and 0.02% for c.94 C > T) (Supplementary Table 3). Thus, the estimated risk for hearing loss in Ashkenazi Jewish individual carrying microdeletion in the DFNB1 locus was estimated as 3.6%, or one in 28; whereas the risk for a child with hearing loss for a parent carrying an incidental microdeletion in the DFNB1 locus, with an Ashkenazi Jewish spouse, is 1.85%, or one in 54.
Comment
Autosomal recessive disorders are a significant cause of severe childhood mortality and mortality, affecting at least 25 in 10,000 children [13]. Thus, detection and reporting of carrier status for heterozygous recessive variants is of great importance for future reproductive counseling, as well as early diagnosis and treatment. Preconception carrier screening for reproductive purposes is recommended by numerous guidelines, whether limited pan-ethnic (for cystic fibrosis and spinal muscular atrophy) and ancestry-based genetic testing for common sequence variants, and up to high-throughput genotyping and sequencing approaches that allow simultaneous testing of numerous genetic disorders [14]. However, guidelines referring to next generation sequencing techniques define “incidental or secondary findings” as disease-causing variants in 59 medically actionable genes related to autosomal dominant severe and preventable conditions, and do not recommend reporting carrier status of recessive genes [15]. Thus, the 2019 ACMG recommendation to disclose carrier status in microarray analysis on certain terms, such as “reasonably high carrier frequency in the patient population” [6], is a new and unusual decision.
It must be noted that the frequency of incidental heterozygous CMA microdeletions encompassing any genes of autosomal recessive disorders has not been thoroughly described in the literature. This can be the reason for the controversial policies whether to report such findings. Thus, in this pilot model we chose to focus on three recurrent copy number losses of genes associated with non-syndromic hearing loss. Hearing impairment is a multifactorial condition, affecting up to 1 in 500 newborns with a pre-lingual hearing impairment [16]. Traditionally, the diagnosis of genetic causes of hearing loss was performed by Sanger sequencing to search for sequence variants. However, in the last decade numerous papers were published describing the contribution of CNVs (i.e., deletions and duplications of approximately 1 kb) to genetic deafness. For example, in 2014 Shearer et al. have examined 686 patients with hearing loss and identified CNVs within a known deafness gene in 15.2% of these cases [17]. The most common CNVs (73%) involved STRC gene, followed by CNVs in OTOA (13%).
In our study, we demonstrate the heterozygous microdeletions encompassing STRC, OTOA genes and the DFNB1 locus can overall be demonstrated in up to every 123 microarray analyses. Demonstration of similar frequency between various subgroups supports the assumption that microdeletions encompassing STRC, OTOA and the DFNB1 locus are truly incidental findings, and that the whole cohort can be used as a single group for estimation of the prevalence. The considerable frequency of recurrent microdeletions encompassing OTOA and STRC genes, as well as DFNB1 locus raises a question whether these microdeletions should be reported as incidental findings in all microarray tests. It must be noted that these three genes associated with hearing loss were chosen as a pilot model, and thus the overall prevalence of microdeletions encompassing autosomal recessive genes, as well as the expected risk for an affected offspring, may be much higher. According to ethical standards for human subjects’ research, incidental findings should be reported when knowledge of the information bears a strong net benefit for the patient or the offspring [18]. The “strong net benefit” category includes genetic information that can be used in reproductive decision-making, e.g., to ameliorate or avoid significant risk for offspring of a condition likely to be life-threatening or grave. Early detection of genetic disorders is crucial for the application of palliative treatments and special education. In addition, diagnosis of carrier state may allow the couples informed decisions regarding reproductive plans.
Despite the obvious benefits, the question whether to include any heterozygous losses of genes associated with known autosomal recessive diseases in the final microarray report is not easy to answer. It depends on numerous parameters unique for each gene, including the severity and age of onset of the associated disorder, carrier frequency in the patient population, and the availability of genetic counseling and testing. In addition, a variable phenotype for different variants should be taken into account, as well as the possibility of unknown phenotype in case of double heterozygosity for all genetic variants. In our analysis we show that the estimated risks for morbidity in the examined individual and future progeny vary for each gene and the specific population, and range from as low as one in 1703 for OTOA microdeletions, and up to one in 28 for deletions in the DFNB1 locus in Ashkenazi Jewish population.
Based on the results of our model pilot for heterozygous microdeletions encompassing three hearing impairment genes, the reporting of such findings should not be based on a uniform recommendation but should be individually considered. Although potentially cumbersome, for each microdeletion encompassing a gene associated with autosomal recessive disorder, the frequency of known disease-causing sequence variants and deletions in this gene should be calculated in the specific origin. Also, a cut-off for the risk for an affected proband must be determined. For instance, as the risks for an affected individual or future child for microdeletions in the DFNB1 locus in this Ashkenazi Jewish community reach 1:28 and 1:54, respectively, it seems that incidental microdeletions in the DFNB1 locus in this community should be reported. Of note, the partner can be examined only for the common origin-specific common variants, rather than performing gene sequencing, which could lower the costs of the genetic testing. On the contrary, as the risk for OTOA sequence variants and microdeletions was estimated as 0.24%, the risk for an affected child in the case of a parent with incidentally diagnosed OTOA microdeletion is 1:862. This means that “number needed to test”, i.e., the number of spouses which will need to undergo OTOA genetic sequencing to detect one affected child, is 862, an unacceptably high number. Furthermore, as no common sequence variants are known in OTOA gene, genetic testing of the partner would demand whole gene sequencing, with associated costs.
Additional point needs to be considered is that STRC, OTOA and GJB6 are relatively common and well-explored genes. If, according to the new ACMG recommendations, we are to report any heterozygous losses of recessive genes, including those in which the frequency of sequence variants is unknown, the numbers of CMA analyses with autosomal recessive incidental findings can be unacceptably high, so that almost every partner will have to perform complementary gene sequencing. For instance, analytical validation of 36,859 patients by sequencing-based expanded carrier screening panel of 235 genes with panel-wide CNV calling has shown that novel CNVs constitute 9.2% of variants associated with fetal disease [19]. Of the screened 7498 couples, 335 (4.5%) were identified as at risk for an affected offspring, showing that about 1 in 300 pregnancies could be affected by at least one serious condition. This high frequency of carrier rate implies that position papers and guidelines should carefully consider the approach to incidental findings.
In summary, in this model pilot of microarray microdeletions encompassing genes associated with autosomal recessive hearing loss, we tested the option of reporting such CNVs as an incidental finding. The carrier frequency is not uniform for all three genes demonstrated, and not for every population. Thus, the general decision whether to report or to disregard such findings cannot be part of a uniform policy, for all recessive genes, for all genetic variants or for all populations, but rather should be based on a detailed evaluation of origin-specific sequence variants for each gene, with a careful consideration and discussion whether to include the microdeletion in the final report for each patient.
In addition, the issue of possible incidental findings should be meticulously discussed with the patients before diagnostic or prenatal testing, as not all individuals may be willing to be informed of such findings. As the choice to have access to the knowledge of carrier status belongs to the patient and their parents, genetic counselors could help patients and their families navigate the intricacies and implications for such findings. Since there is evidence stating that every person might be a carrier of up to 30 sequence variants in autosomal recessive genes, the universal recommendation to report such findings might involve almost every sample, in the context of microarray as well as whole exome sequencing performed for various indications. Eventually, each prenatal microarray will necessitate further sequencing of the sample, up to complementary exome sequencing. While currently this is not readily feasible, since each method of genetic testing carries an additional cost, this may be relevant for the future in which all tests will be performed by low-cost whole genome approach.
References
American College of O, Gynecologists’ Committee on Practice B-O, Committee on G, Society for Maternal-Fetal M. Practice Bulletin No. 162: Prenatal Diagnostic Testing for Genetic Disorders. Obstet Gynecol. 2016;127:e108–22.
Sagi-Dain L, Cohen Vig L, Kahana S, Yacobson S, Tenne T, Agmon-Fishman I, et al. Chromosomal microarray vs. NIPS: analysis of 5541 low-risk pregnancies. Genet Med. 2019;21:2462–7.
Kearney HM, Thorland EC, Brown KK, Quintero-Rivera F, South ST. Working Group of the American College of Medical Genetics Laboratory Quality Assurance C. American College of Medical Genetics standards and guidelines for interpretation and reporting of postnatal constitutional copy number variants. Genet Med. 2011;13:680–5.
Vanakker O, Vilain C, Janssens K, Van der Aa N, Smits G, Bandelier C, et al. Implementation of genomic arrays in prenatal diagnosis: the Belgian approach to meet the challenges. Eur J Med Genet. 2014;57:151–6.
Silva M, de Leeuw N, Mann K, Schuring-Blom H, Morgan S, Giardino D, et al. European guidelines for constitutional cytogenomic analysis. Eur J Hum Genet.2019;27:1–16.
Riggs ER, Andersen EF, Cherry AM, Kantarci S, Kearney H, Patel A, et al. Technical standards for the interpretation and reporting of constitutional copy-number variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics (ACMG) and the Clinical Genome Resource (ClinGen). Genet Med. 2020;22:245–57.
Maya I, Smirin-Yosef P, Kahana S, Morag S, Yacobson S, Agmon-Fishman I, et al. A study of normal copy number variations in Israeli population. Hum Genet. 2021;140:553–63.
Maya I, Sharony R, Yacobson S, Kahana S, Yeshaya J, Tenne T, et al. When genotype is not predictive of phenotype: implications for genetic counseling based on 21,594 chromosomal microarray analysis examinations. Genet Med. 2018;20:128–31.
Landrum MJ, Lee JM, Benson M, Brown G, Chao C, Chitipiralla S, et al. ClinVar: public archive of interpretations of clinically relevant variants. Nucleic Acids Res. 2016;44:D862–8.
Karczewski KJ, Francioli LC, Tiao G, Cummings BB, Alfoldi J, Wang Q, et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature. 2020;581:434–43.
Azaiez H, Booth KT, Ephraim SS, Crone B, Black-Ziegelbein EA, Marini RJ, et al. Genomic Landscape and Mutational Signatures of Deafness-Associated Genes. Am J Hum Genet. 2018;103:484–97.
Mahdieh N, Rabbani B. Statistical study of 35delG mutation of GJB2 gene: a meta-analysis of carrier frequency. Int J Audiol. 2009;48:363–70.
Edwards JG, Feldman G, Goldberg J, Gregg AR, Norton ME, Rose NC, et al. Expanded carrier screening in reproductive medicine-points to consider: a joint statement of the American College of Medical Genetics and Genomics, American College of Obstetricians and Gynecologists, National Society of Genetic Counselors, Perinatal Quality Foundation, and Society for Maternal-Fetal Medicine. Obstet Gynecol. 2015;125:653–62.
Beauchamp KA, Muzzey D, Wong KK, Hogan GJ, Karimi K, Candille SI, et al. Systematic design and comparison of expanded carrier screening panels. Genet Med. 2018;20:55–63.
Kalia SS, Adelman K, Bale SJ, Chung WK, Eng C, Evans JP, et al. Recommendations for reporting of secondary findings in clinical exome and genome sequencing, 2016 update (ACMG SF v2.0): a policy statement of the American College of Medical Genetics and Genomics. Genet Med. 2017;19:249–55.
Hilgert N, Smith RJ, Van Camp G. Forty-six genes causing nonsyndromic hearing impairment: which ones should be analyzed in DNA diagnostics? Mutat Res. 2009;681:189–96.
Shearer AE, Kolbe DL, Azaiez H, Sloan CM, Frees KL, Weaver AE, et al. Copy number variants are a common cause of non-syndromic hearing loss. Genome Med. 2014;6:37.
Wolf SM, Lawrenz FP, Nelson CA, Kahn JP, Cho MK, Clayton EW, et al. Managing incidental findings in human subjects research: analysis and recommendations. J Law Med Ethics. 2008;36:219–48.
Hogan GJ, Vysotskaia VS, Beauchamp KA, Seisenberger S, Grauman PV, Haas KR, et al. Validation of an Expanded Carrier Screen that Optimizes Sensitivity via Full-Exon Sequencing and Panel-wide Copy Number Variant Identification. Clin Chem. 2018;64:1063–73.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Maya, I., Basel-Salmon, L. & Sagi-Dain, L. Is it time to report carrier state for recessive disorders in every microarray analysis?—A pilot model based on hearing loss genes deletions. Eur J Hum Genet 29, 1292–1300 (2021). https://doi.org/10.1038/s41431-021-00856-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-021-00856-3
This article is cited by
-
Deafness—family matters
European Journal of Human Genetics (2022)