Abstract
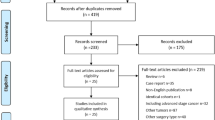
Gastric-tube feeding and post-pyloric feeding are the two most common forms of enteral nutrition, each with advantages and disadvantages. To explore the effects and safety of gastric-tube versus post-pyloric feeding in critical patients by comparing pulmonary aspiration- and nutrition-related outcomes, a meta-analysis was conducted. It was performed by systematically searching the following databases: PubMed, EMBASE, Cochrane library, BMJ best practice, ProQuest dissertations and theses, CINAHL, web of science, SinoMed, WANFANG, CNKI, and the platform of clinical trial registration. The databases were searched through December 31, 2019, and studies were evaluated by two independent researchers. Review Manager software was used for data analysis. We included 41 studies conducted in ten countries and involving 3248 participants. Meta-analysis showed that post-pyloric feeding had a lower incidence rate of pulmonary aspiration, gastric reflux, and pneumonia (P < 0.001, all), less incidence of gastrointestinal complications including vomiting, nausea, diarrhea, abdominal distension, high gastric residual volume, and constipation (P < 0.05, all), more optimal gastrointestinal nutrition including the percentage of total nutrition provided to the patient, the time to tolerate enteral nutrition, the time required to start feeding and the time required to reach nutritional targets (P < 0.05, all), shorter length of mechanical ventilation, stay in ICU and stay in hospital (P < 0.001, all), compared with gastric-tube feeding. No significant differences were shown in the time of gastrointestinal function recovery, mortality, or hospitalization expenses between the two feeding routes. This review provides evidence that post-pyloric feeding appears to be the safer and more effective choice, as compared to gastric-tube feeding among critical patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Kudsk KA. Beneficial effect of enteral feeding. Gastrointest Endosc Clin N Am. 2007;17:647–62.
McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: society of critical care medicine (SCCM) and American society for parenteral and enteral nutrition (A.S.P.E.N.). JPEN J Parenter Enter Nutr. 2016;40:159–211.
Acosta-Escribano J, Fernandez-Vivas M, Grau Carmona T, Caturla-Such J, Garcia-Martinez M, Menendez-Mainer A, et al. Gastric versus transpyloric feeding in severe traumatic brain injury: a prospective, randomized trial. Intensive Care Med. 2010;36:1532–9.
Zhou Y, Chen N. Effects of enteral nutrition through nasointestinal tube and nasogastric tube on prognosis and complications in patients with severe craniocerebral injury. J Preventive Med Chin People’s Liberation Army. 2019;37:72–4.
Friedman G, Flavia Couto CL, Becker M. Randomized study to compare nasojejunal with nasogastric nutrition in critically ill patients without prior evidence of altered gastric emptying. Indian J Crit Care Med. 2015;19:71–5.
Taylor SJ, Allan K, McWilliam H, Manara A, Brown J, Greenwood R. et al. A randomised controlled feasibility and proof-of-concept trial in delayed gastric emptying when metoclopramide fails: we should revisit nasointestinal feeding versus dual prokinetic treatment: achieving goal nutrition in critical illness and delayed gastric emptying: trial of nasointestinal feeding versus nasogastric feeding plus prokinetics. Clin Nutr Espen. 2016;14:1–8.
Zhang ZZ, Xiao HL, Wang Y, Wang GX. Effect of ultrasound guided-indwelling nasointestinal tube for enter nutrition support in patients with respiratory failure undergoing mechanical ventilation. J Clin Emerg. 2019;20:173–7.
Ding XR. Effects conparing of blind nasointestinal tube inserting and nasogastric tube nutrition support on patients with severe craniocerebral injury. Chin J Mod Nurs. 2018;24:1067–71.
White H, Sosnowski K, Tran K, Reeves A, Jones M. A randomised controlled comparison of early post-pyloric versus early gastric feeding to meet nutritional targets in ventilated intensive care patients. Crit Care. 2009;13:R187.
Hsu CW, Sun SF, Lin SL, Kang SP, Chu KA, Lin CH, et al. Duodenal versus gastric feeding in medical intensive care unit patients: a prospective, randomized, clinical study. Crit Care Med. 2009;37:1866–72.
Davies AR, Morrison SS, Bailey MJ, Bellomo R, Cooper DJ, Doig GS, et al. A multicenter, randomized controlled trial comparing early nasojejunal with nasogastric nutrition in critical illness. Crit Care Med. 2012;40:2342–8.
Wan B, Fu H, Yin J. Early jejunal feeding by bedside placement of a nasointestinal tube significantly improves nutritional status and reduces complications in critically ill patients versus enteral nutrition by a nasogastric tube. Asia Pac J Clin Nutr. 2015;24:51–7.
Chen FX, Xu C, Zhang CH. Effect of indwelling nasointestinal tube for enteral nutrition support in patients with severe craniocerebral trauma undergoing mechanical ventilation. Chin Crit Care Med. 2018;30:57–60.
Pan XD, Zhang JC, Tang RM, Sun LF. Effect of nasogastric tube decompression combined with nasointestinal tube nutritional support in the prognosis of patients with severe nervous system diseases. Chin J Crit Care Med. 2017;10:230–4.
Montecalvo MA, Steger KA, Farber HW, Smith BF, Dennis RC, Fitzpatrick GF, et al. Nutritional outcome and pneumonia in critical care patients randomized to gastric versus jejunal tube feedings. The critical care research team. Crit Care Med. 1992;20:1377–87.
Liu J, Hu A, Huang YX. Efficiency analysis of enteral nutrition supportive nursing by nasojejunal tube in treatment of patients with severe craniocerebral injury. J Clin Med. 2019;23:107–10.
Li WW, Gui SH, Ye HB, Qian QD, Tan JG. Effect of enteral nutrition by nasointestinal tube on prevention of ventilator-associated pneumonia. Chin J Nosocomiol. 2015;3:615–7.
Montejo JC, Grau T, Acosta J, Ruiz-Santana S, Planas M, García-de-Lorenzo A, et al. Multicenter, prospective, randomized, single-blind study comparing the efficacy and gastrointestinal complications of early jejunal feeding with early gastric feeding in critically ill patients. Crit Care Med. 2002;30:796–800.
Zhang Z, Xu X, Ding J, Ni H. Comparison of postpyloric tube feeding and gastric tube feeding in intensive care unit patients: a meta-analysis. Nutr Clin Pract. 2013;28:371–80.
Alkhawaja S, Martin C, Butler RJ, Gwadry-Sridhar F. Post-pyloric versus gastric tube feeding for preventing pneumonia and improving nutritional outcomes in critically ill adults. Cochrane Database Syst Rev. 2015;8:1–80.
Deane AM, Dhaliwal R, Day AG, Ridley EJ, Davies AR, Heyland DK. Comparisons between intragastric and small intestinal delivery of enteral nutrition in the critically ill: a systematic review and meta-analysis. Crit Care. 2013;17:R125.
Li Z, Qi JR, Zhao XK, Lin YQ, Zhao SD, Zhang ZD, et al. Risk-benefit profile of gastric vs transpyloric feeding in mechanically ventilated patients: a meta-analysis. Nutr Clin Pract. 2016;31:91–8.
Wang D, Zheng SQ, Chen XC, Jiang SW, Chen HB. Comparisons between small intestinal and gastric feeding in severe traumatic brain injury: a systematic review and meta-analysis of randomized controlled trials. J Neurosurg. 2015;123:1194–201.
Sajid MS, Harper A, Hussain Q, Forni L, Singh KK. An integrated systematic review and meta-analysis of published randomized controlled trials evaluating nasogastric against postpyloris (nasoduodenal and nasojejunal) feeding in critically ill patients admitted in intensive care unit. Eur J Clin Nutr. 2014;68:424–32.
Dutta AK, Goel A, Kirubakaran R, Chacko A, Tharyan P. Nasogastric versus nasojejunal tube feeding for severe acute pancreatitis. Cochrane Database Syst Rev. 2020;3:1–46.
Dong XW, Huang SL, Jiang ZH, Song YF, Zhang XS. Nasointestinal tubes versus nasogastric tubes in the management of small-bowel obstruction: a meta-analysis. Medicine. 2018;97:1–7.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–12.
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. Br Med J. 2011;18:343.
Boivin MA, Levy H. Gastric feeding with erythromycin is equivalent to transpyloric feeding in the critically ill. Crit Care Med. 2001;29:1916–9.
Chen GQ, Li ZE, Wang BJ, Liang FR, Sun K, Liu GR. Pneumonia in severe acute stroke patients fed by nasojejunal versus nasogastric tub. Int J Cardiovasc Dis. 2016;24:586–91.
Davies AR, Froomes PR, French CJ, Bellomo R, Gutteridge GA, Nyulasi I, et al. Randomized comparison of nasojejunal and nasogastric feeding in critically ill patients. Crit Care Med. 2002;30:586–90.
Day L, Stotts NA, Frankfurt A, Stralovich-Romani A, Volz M, Muwaswes M, et al. Gastric versus duodenal feeding in patients with neurological disease: a pilot study. J Neurosci Nurs. 2001;33:148–9. 55–9
Ding Y, Yang QH, Wang BJ. Raw rhubarb nasal jejunal tube perfusion applicaition value in acute pancreatitis. Chin Arch Tradit Chin Med. 2014;11:2785–7.
Eatock FC, Chong P, Menezes N, Murray L, McKay CJ, Carter CR, et al. A randomized study of early nasogastric versus nasojejunal feeding in severe acute pancreatitis. Am J Gastroenterol. 2005;100:432–9.
Esparza J, Boivin MA, Hartshorne MF, Levy H. Equal aspiration rates in gastrically and transpylorically fed critically ill patients. Intens Care Med. 2001;27:660–4.
Hou YH, Cao HH. Influence of nutrition support through nasojejunal tube on the gastrointestinal function of patients with severe craniocerebral injury. J Nurs Adm. 2013;13:733–5.
Jiang M, Wan NL, Li B, Li J. The effect of enteral nutrition support via nasojejunostomy on the prognosis of patients with mechanical ventilation in ICU after acute craniocerebral injury. Modern J Integr Tradit Chin West Med. 2016;32:2818–21.
Jin X, Shi Y, Wang DC, Liu HY, Li WB, Cai Y. et al. Application of gastroscopy assistant nasal intestinal tube placement and jejunum nutrition in patients with severe internal diseases. Chin J Endosc. 2018;24:28–32.
Kortbeek JB, Haigh PI, Doig C. Duodenal versus gastric feeding in ventilated blunt trauma patients: a randomized controlled trial. J Trauma. 1999;46:992–6.
Kearns PJ, Chin D, Mueller L, Wallace K, Jensen WA, Kirsch CM. The incidence of ventilator-associated pneumonia and success in nutrient delivery with gastric versus small intestinal feeding: a randomized clinical trial. CritCare Med. 2000;28:1742–6.
Li FL, Li H, Chen CH, Chen XP. Clinical observation on prevention of ventilator-associated pneumonia in patients with mechanical ventilation by enteral nutrition through naso intestinal tube. J Clin Res. 2017;034:1010–2.
Lou X. J. Early enteral nutrition of nasogastric tube in the treatment of severe acute pancreatitis [Master’s degree]. Sichuan Med University. 2015.
Neumann DA, DeLegge MH. Gastric versus small-bowel tube feeding in the intensive care unit: a prospective comparison of efficacy. Crit Care Med. 2002;30:1436–8.
Singh N, Sharma B, Sharma M, Sachdev V, Bhardwaj P, Mani K, et al. Evaluation of early enteral feeding through nasogastric and nasojejunal tube in severe acute pancreatitis: a noninferiority randomized controlled trial. Pancreas. 2012;41:153–9.
Wang HH, Wu Q, Zhao SB, Deng XM, Zheng SY, He XD. Use of nasojejunal tube in early enteral nutrition in severe traumatic brain injury patients under mechanical ventilation. Chin J Clin Nutr. 2015;23:23–6.
Wang XJ. The effects of nasogastric tube decompression and enteral nutrition support on the prognosis of patients with severe craniocerebral injury. Shanxi Med J. 2018;47:1290–3.
Wang J, Li FH, Hou JH, Zhou Q. Effect of nasogastric tube and nasal jejunum tube in enteral nutrition therapy of severe acute pancreatitis. Lab Med Clin. 2018;2265:2258–61.
Yin P. J. Analysis of the application and nursing effect of furcaix spiral naso intestinal tube in enteral nutrition of critical patients. Chin Nur Res. 2018;32:112.
Yu PP, Zhang HS, Li YF. Application of enteral nutrition through nasointestinal tube in severe craniocerebral trauma patients with mechanical ventilation. Chin J Mod Nurs. 2013;19:3830–2.
Zeng RC, Jiang FG, Xie Q. Comparison of nose jejunal tube and nasogastric tube in providing early enteral nutrition for patients with severe craniocerebral injury. Chin J Clin Nutr. 2010;18:355–7.
Zhang Q, Wang HQ, Yu XY, Yao XH, Wang HY. Comparison of application effect of nasogastric tube and nasal bowel nutritional support in stroke patients with dysphagia. J Math Med. 2016;29:1168–9.
Zheng SH, Tong QY, Zhu ZY, Li ZY, Yuan JH. Clinical observation on treatment of severe acute pancreatitis with Rhubarb by three different administration routes. Chin J Integr Tradit West Med Intens Crit Care. 2010;17:212–3.
Zhu Y, Yin H, Zhang R, Ye X, Wei J. Gastric versus postpyloric enteral nutrition in elderly patients (age >= 75 years) on mechanical ventilation: a single-center randomized trial. Crit Care. 2018;22:170.
Kharrazian D. Traumatic brain injury and the effect on the brain-gut axis. Alter Ther Health Med. 2015;21:28–32.
Houghton LA, Lee AS, Badri H, DeVault KR, Smith JA. Respiratory disease and the oesophagus: reflux, reflexes and microaspiration. Nat Rev Gastroenterol Hepatol. 2016;13:445–60.
Alhazzani W, Almasoud A, Jaeschke R, Lo BW, Sindi A, Altayyar S, et al. Small bowel feeding and risk of pneumonia in adult critically ill patients: a systematic review and meta-analysis of randomized trials. Crit Care. 2013;17:R127.
Funding
This research was funded by Capital Medical University Nature Project (Grant No. PYZ2018026).
Author information
Authors and Affiliations
Contributions
YL conceived and designed the study; acquired, analyzed, and interpreted the data; and drafted and revised the manuscript. YLW contributed to study design, data analysis, and manuscript revision. JNW contributed to data acquisition and analysis, and the drafting of the manuscript. BHZ contributed to data acquisition and analysis, and the drafting of the manuscript. LS contributed to data analysis and the drafting of the manuscript. QX contributed to study conception and design, data analysis and interpretation, and manuscript review and revision. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, Y., Wang, Y., Zhang, B. et al. Gastric-tube versus post-pyloric feeding in critical patients: a systematic review and meta-analysis of pulmonary aspiration- and nutrition-related outcomes. Eur J Clin Nutr 75, 1337–1348 (2021). https://doi.org/10.1038/s41430-021-00860-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-00860-2
This article is cited by
-
Stomach position evaluated using computed tomography is related to successful post-pyloric enteral feeding tube placement in critically ill patients: a retrospective observational study
Journal of Intensive Care (2023)
-
Nasogastric tube insertion length measurement and tip verification in adults: a narrative review
Critical Care (2023)
-
Ventilator-associated pneumonia prevention in the Intensive care unit using Postpyloric tube feeding in China (VIP study): study protocol for a randomized controlled trial
Trials (2022)
-
Challenges of Gastric Versus Post-pyloric Feeding in COVID-19 Disease
Current Surgery Reports (2022)