Abstract
Inflammatory Bowel Disease (IBD), a chronic nonspecific intestinal inflammatory disease, is comprised of Ulcerative Colitis (UC) and Crohn’s Disease (CD). IBD is closely related to a systemic inflammatory reaction and affects the progression of many intestinal and extraintestinal diseases. As one of the representative bacteria for probiotic-assisted therapy in IBD, multiple strains of Lactobacillus have been proven to alleviate intestinal damage and strengthen the intestinal immunological barrier, epithelial cell barrier, and mucus barrier. Lactobacillus also spares no effort in the alleviation of IBD-related diseases such as Colitis-associated Colorectal cancer (CAC), Alzheimer’s Disease (AD), Depression, Anxiety, Autoimmune Hepatitis (AIH), and so on via gut-brain axis and gut-liver axis. This article aims to discuss the role of Lactobacillus in IBD and IBD-related diseases, including its underlying mechanisms and related curative strategies from the present to the future.
Similar content being viewed by others
Facts
-
Lactobacillus is a representative of probiotic-assisted therapy in IBD and is approved to alleviate colitis in both mice with DSS-induced colitis and IBD patients.
-
IBD was pointed out to impact the systemic inflammatory reaction, leading to the aggravation of other extraintestinal diseases, especially in the liver and CNS.
-
The combination of Lactobacillus and other probiotics or prebiotics is widely used in treating IBD in clinical trial stages, and some of them have apparent therapeutic effects.
Open questions
-
What are the specific mechanisms Lactobacillus possesses to alleviate IBD?
-
What role does Lactobacillus play in IBD-related diseases in the gut-brain and gut-liver axes?
-
Does the effect of probiotics change with the degree of inflammation in IBD and IBD-related diseases?
-
How can we reasonably combine the use of probiotics and prebiotics in treating IBD and IBD-related conditions to maximize the effectiveness of Lactobacillus?
Introduction
Inflammatory Bowel Disease (IBD), a chronic nonspecific intestinal inflammatory disease that generally causes abdominal pain, diarrhea, and bloody stools, displayed its globalization from Western developed regions to newly industrialized countries in the twenty-first century [1]. IBD is comprised of ulcerative colitis (UC) and Crohn’s Disease (CD), the former mainly causing successional shallow ulcers with intestinal crypt abscesses in lamina propria and the latter represented by segmental distributed deep ulcers accompanied with non-caseating granulomas in all layers of the intestinal wall which explained its high tendentiousness in fistulation [2]. The existing treatment of IBD focused on amino-salicylic acid preparation, glucocorticoids, immunosuppressants, and new-emerging biological agents such as infliximab and adalimumab. Though possessing low mortality, frequent relapse, and high disability rate of IBD made it a heavy burden to not only public health but also the fiscal and resources in healthcare systems, announcing the urgent demand to explore applicable therapeutic methods to alleviate the misery of IBD patients in both active and remission period.
Gut microbiota, consisting of bacteria, archaea, fungi, viruses, and parasites, was closely related to intestinal disease occurrence, development, and prognosis [3]. Among the above microbes, research in the field of human intestinal bacteria, mainly including Firmicutes, Bacteroidetes, Actinobacteria, Fusobacteria, Proteobacteria, Verrucomicrobia, and Cyanobacteria, were booming and showed terrific development prospects in recent years [4]. Within the considerable collective of intestinal bacteria, Lactobacillus, a prominent member of the Firmicutes, caused widespread concern as its subpopulations were put forward to affect the deterioration of course in IBD patients as well as to display its protective effect in the experimental colitis mouse model [5]. Despite the significant talent lactobacillus unveiled, summaries to wrap up its particular underlying mechanism of action in IBD and IBD-related diseases were limited. Therefore, we are here to promulgate the role of Lactobacillus in IBD and IBD-related disorders and the microbiota-gut-brain axis (MGBA) to propose our insights.
The subspecies of Lactobacillus and its relationship with IBD
Lactobacillus, a genus of gram-positive anaerobic bacteria without spores, was named after its capability to decompose glucose and other sugars into lactic acid. As a member of Firmicutes, it belonged to the class Bacillus, order Lactobacillales, family Lactobacillus. It was comprised of various subspecies, including Lactobacillus acidophilus, Lactobacillus salivarius, Lactobacillus plantarum, Lactobacillus casei, Lactobacillus rhamnosus, Lactobacillus gasseri, and so on [6]. According to available data, it was estimated that this genus accounted for about 0.3% of the total bacterial count in the human colon, while when it comes to human duodenum, the figure reached up to 6% [7, 8]. Based on experimental research in Lactobacillus and mice with experimental colitis so far, the majority of Lactobacillus’ subspecies did good to the intestinal health and helped with the restoration of the host from excessive intestinal inflammation as what we would put later, while only a fraction played the opposite conducts. As for the latter, for example, it has been observed that the supernatant of Lactobacillus delbrueckii CU/22 could lead to the apoptosis and necrosis of HT-29 cells, suggesting that careful consideration ought to be involved in choosing probiotics as adjuvant therapy of IBD [9].
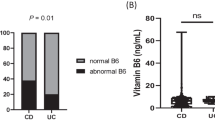
When we looked at the clinical analysis, there was a positive correlation between intestinal Lactobacillus abundance and clinical symptoms in UC patients, as expected, while the situations in CD patients were still under dispute [5, 10, 11]. Consequently, great importance ought to be attached to proclaiming the role of Lactobacillus in IBD.
The mechanism underlying the barrier-protective effect of Lactobacillus in IBD
The effect of Lactobacillus on the immunological barrier
The effect of Lactobacillus on immune cells
As the first line of defense against microbiota, intestinal mucosa harbors numerous immune cells consisting of lymphocytes, dendritic cells, granulocytes, etc. Their methodical interactions with each other maintain immune homeostasis in both peripheral blood and intestinal mucosal microenvironment. However, under colitis, such tacit understanding cooperation received severe interference. In patients with IBD, there was proved to exist a pathological transformation from Tregs to Th17 in peripheral blood, and the subsequently reduced Treg/Th17 ratio observed in both adults and pediatric patients may, to a certain extent, explain the hampered systemic immunosuppressive function [12,13,14]. Besides, though possessing specific divergence in the subtype of numerous immune cells, UC and CD patients were recorded to display higher neutrophil-to-lymphocyte ratio (NLR) in peripheral blood compared to healthy controls [15]. Regarding the immune microenvironment in the inflamed colonic tissue, the frequency of M1-like macrophages, activated DCs, plasmacytoid DCs, and monocytes increased as well [16]. To summarize, the hyperfunction of pro-inflammatory cells and the low vitality of anti-inflammatory cells resulted in disturbed immune homeostasis, which could be a prospective reversible therapeutic target for IBD.
The aptitude of Lactobacillus to restore the altered immune cells proportion was proved in many pieces of research, which pointed out the strengthened anti-inflammatory force and hindered pro-inflammatory power after the administration of Lactobacillus strains such as Lactobacillus reuteri and Lactobacillus rhamnosus. Respectively, Lactobacillus reuteri was able to not only prevent the recruitment of neutrophils and the expansion of DCs in the intestinal mucosa but also increase the frequency of Tregs in mesenteric lymph nodes which were the supreme headquarters of intestinal immune cells [17]. Apart from Lactobacillus reuteri, Lactobacillus rhamnosus was also competent in interfering with the relative abundance of immune cells since it was proved to decrease the Th17/Treg ratio through the JAK-STAT signaling pathway with the presence of toll-like receptor 2 (TLR2) in the colon of mice with DSS-induced colitis [18]. In addition, it has been uncovered that soluble factors that existed in the supernatants of Lactobacillus rhamnosus could promote the mitochondrial pathway-dependent apoptosis of specific immune cells, mainly monocytes, without affecting intestinal epithelial cells (IECs), indicating its desirable value in the prevention of excessive inflammatory activation [19].
Except for changing the number and proportion of different immune cells, the phenotype of immune cells was also transformed by Lactobacillus. As a vital constituent of antigen-presenting cells (APCs), macrophage possesses two exact opposite-in-function phenotypes, M1 and M2, the former polarized by lipopolysaccharide (LPS), producing pro-inflammatory cytokines such as IL-1β, IL-6, IL-12, IL-23, and TNF-α, the latter polarized by Th2 cytokines, producing anti-inflammatory cytokines such as IL-10 and TGF-β [20]. Lactobacillus reuteri GroEL, a kind of hot shock protein (HSP) homologous with human HSP60, was found to regulate the phenotypic modulation of macrophages concretely embodied in that it inhibited M1-like macrophage markers while enhancing the expression of M2-like macrophage markers by how it relieved the inflammatory pressure in mice [21]. Except for Lactobacillus reuteri, Lactobacillus rhamnosus Lr32 and Lactobacillus salivarius Ls33 protected mice from TNBS-induced colitis by promoting DCs’ differentiation to a specific tolerogenic phenotype featured by their inability neither to produce cytokines or chemokines nor to express co-stimulatory molecules to activate T cells [22]. More precisely, these peculiar DCs conveyed their anti-inflammatory capability by reducing the expression of pro-inflammatory mediators containing IL-17 and IL-23 and negatively regulating T-cell function via overexpressing indoleamine 2, 3 dioxygenases (IDO) [22].
In the above research outcomes, Lactobacillus interfered with the excessive activation of intestinal and body inflammatory reactions in multiple directions and angles by changing the number, recruitment, and differentiation of immune cells, thus limiting the development and exacerbation of IBD.
The effect of Lactobacillus on inflammatory cytokines and underlying mechanisms
Dialectically, there was a correlation between immune cell distribution and the secretion of inflammatory cytokines since numerous immune cells secreted inflammatory cytokines, which could, in turn, interfere with their recruitment and function. Just as we derived it from the previous section, various Lactobacillus strains represented by Lactobacillus rhamnosus [23], Lactobacillus jensenii [24], Lactobacillus reuteri [17], Lactobacillus casei [25], and Lactobacillus plantrum [26], downregulated the production of pro-inflammatory mediators such as interleukin-6 (IL-6), interleukin-1β (IL-1β), tumor necrosis factor-α (TNF-α) and otherwise in the inflamed tissues of colitis mice. Meanwhile, the expression of anti-inflammatory mediators was upregulated by Lactobacillus as well. A pleiotropic factor played a role in immunomodulation, G-CSF, negatively associated with pro-inflammatory mediators such as TNF-α, IL-23, and IL-12, was constitutively expressed at a high level in intestinal lamina propria cells both in mouse and healthy individuals, but at a relatively low level in IBD patients [27]. Lactobacillus rhamnosus GR-1, according to Andrew J Martins and his colleagues, could escalate the expression of G-CSF in healthy individuals but failed to reverse G-CSF reduction in IBD patients, thus exhibited their prophylaxis but not treatment value [27].
The mechanisms were diligently explored after observing that the lactobacillus mentioned above hampered the production and secretion of inflammatory mediators. The pattern recognition receptor (PRR) family was elucidated instrumental in the anti-inflammatory effect of various strains. To illustrate, by contacting with toll-like receptor 4 (TLR4) and inhibiting its downstream TLR4/Myd88/NF-κB signaling axis in colon tissues of mice, a novel soluble protein HM0539 from Lactobacillus rhamnosus downregulated the expression of cyclooxygenase-2 (COX-2) and inducible nitric oxide synthase (iNOS), therefore hindered the production of prostaglandin E2 (PGE2) and nitric oxide (NO), two vital inflammatory mediators in the gut [23]. Let aside the TLR family, the nucleotide-binding oligomerization domain (NOD) family also mediated robust recognition. NOD2 was elucidated to identify strain-specific muropeptides secreted from peptidoglycan (PGN), a cell-wall component of Lactobacillus, to activate different response programs of immune cells and lead to quite the opposite influence in the production of an assortment of cytokines [28].
While hindering the production of inflammatory cytokines, Lactobacillus could also accelerate the degradation of tissue-distributed inflammatory-related factors. Interferon-inducible protein-10 (IP-10), a proinflammatory chemokine whose combination with its receptor CXCR3 activated multiple signaling pathways to recruit lymphocytes and lead to the influx of inflammatory cytokines into inflamed mucosa, could be selectively degraded by lactocepin, a protease encoded by Lactobacillus casei or Lactobacillus paracasei. Meanwhile, Lactobacillus casei-fed mice with colitis revealed a significantly interfered infiltration of T cells and ameliorated inflammation in cecal tissue compared to the control group [29]. Coincidentally, IP-10 was also noticed in another research where the degradation was explained as that Lactobacillus casei could hinder the vesicle transport of IP-10 to the cell membrane, which was crucial as a prerequisite for the function of IP-10 [30].
In general, Lactobacillus changed the downstream signal pathway by combining with specific recognition receptors, thus affecting the release and degradation of inflammatory factors to alleviate intestinal inflammation ultimately.
The effect of Lactobacillus on intestinal epithelial cell barrier
Tight junctions (TJs) widely exist in the lateral surface of IECs near the luminal side of the intestine, conducted as important complexes to seal the spaces between IECs, maintain cell polarity, and sustain the permeability barrier. TJs comprised transmembrane proteins such as occludins and claudins and peripheral membrane proteins such as ZO (zonula occludens proteins) [31]. TJs were observed downregulated in mice with DSS-induced colitis, resulting in elevated intestinal mucosa permeability, which may cause bacteria translocation, ion exchange disorder, etc. However, the administration of a great variety of Lactobacillus salvaged this disaster. Lactobacillus acidophilus KLDS 1.0901, Lactobacillus plantarum KLDS 1.0318, and Lactobacillus helveticus KLDS 1.8701, as well as their mixture possessed excellent ability to restore the expression of TJs, including E-cadherin, ZO-1, occludin and claudin-1in mice with colitis [32]. In addition, as a probiotic mixture comprised of Bifidobacterium, Lactobacillus acidophilus, and Enterococcus, Bifico, which was demonstrated to induce the alleviation of both TNBS-induced experimental colitis in mice and IBD patients, also increased TJs expression in DSS-induced colitis in mice [33].
Heat shock protein (HSP), widely existing in all kinds of organisms ranging from bacteria to mammalities and showing high evolutionary conservation, guarantees the correct fold of proteins and protects cells from injuries such as hyperthermia and oxidative stress. In DSS-induced colitis, the expression of HSP is delineated to decrease, indicating the undermined stress protective mechanism in IECs. However, these unpleasant damages could be reversed by the peroral treatment with Lactobacillus reuteri as announced by the research that strain ATCC PTA 4659 displayed the capability to restore the expression of HSP25 and Hsp70 and subsequently help to maintain the integrity of the cytoskeleton and free IECs from oxidative injury in rodent model with colitis. In addition, ATCC PTA 4659 could also strengthen the barrier-preserving TJs between IECs, contributing to its anti-inflammatory effect [17]. As a supplement, soluble factors obtained from Lactobacillus GG were also revealed to participate in the upregulation of Hsp25 and Hsp72 in IECs with the indispensable help of P38 and JNK, two subtribes in the MAPK pathway [34].
Apart from HSP, antioxidant enzymes (AOEs), which were demonstrated to decrease in quantity in the case of enteritis, also played a role in cell protection against attack from oxygen radicals. To cite an example, superoxide dismutase (SOD), especially Mn-SOD, a representative of protective enzymes that neutralized reactive oxygen species (ROS), which were inducers of inflammation in various diseases, was measured reduced in inflamed tissue from IBD patients [35]. In addition to SOD, there exited glutathione peroxidase (GSH-Px), catalase (CAT), and so on in the serum and colonic tissue, devoted to insulating intestinal mucosa from oxidative injury. In this aspect, Lactobacillus plantarum ZS62, the oral administration of which alleviated the severity of DSS-induced colitis in mice, was proved to upregulate the levels of CAT and T-SOD in the serum, and the expression of Cu/Zn SOD, Mn SOD, GSH-Px, CAT in inflamed colon tissues [26]. As a supplement, Lactobacillus gasseri producing Mn-SOD ameliorated the inflammation in IL-10-deficient mice with distinctly decreased infiltration of neutrophils and macrophages into colitis tissue, too [36]. A similar effect emerged in Lactobacillus delbrueckii subsp. Bulgaricus B3 and Lactobacillus delbrueckii subsp. Bulgaricus A13 as well [37].
Under the circumstances of a wrecked epithelial barrier, IECs got injured. At the same time, extracellular matrix glycosaminoglycans (GAGs) were exposed to the intestinal microflora, released GAG-degrading enzymes comprised of chondroitinase, hyaluronidase, and tryptophanase, the productions of which could conversely exert a cytotoxic effect on IECs [38, 39]. At this point, such a vicious circle was broken by Lactobacillus plantarum HY115 and Lactobacillus brevis HY7401; both were detected to reduce the production of GAG-degrading enzymes mentioned above in gut microflora by how they protected IECs against injury, which may also explain the colitis alleviation to a certain extent [40].
In a word, various Lactobacillus strains spared no effort in protecting IECs via strengthening the intestinal tract barrier, upregulating HSP expression, enhancing the storage of AOEs, and reducing IEC-harmful products from intestinal microbiota.
The effect of Lactobacillus on the intestinal mucus barrier
The intestinal mucus barrier, mainly comprised of mucins, covers the intestine’s surface, protecting IECs from toxic substances, digestive enzymes, and bacteria. Mucins were commonly divided into transmembrane mucin represented by Muc 3/4/12/13/17 and mucin able to form a gel, such as Muc 2, whose absence led to a higher trend of colitis and colon cancer [41, 42]. In LPS-treated mice, the expression of Muc-2 and Muc-4 was downregulated, which was reversed by supplement of Lactobacillus rhamnosus LAB3 and Lactobacillus plantarum LAB39, indicating the effect of the above two strains in protecting mucus barrier in LPS-induced colitis [43]. A new synbiotic, FCT, made of Lactobacillus gasseri 505 and cudrania tricuspidata leaf extract, successfully increased the expression of Muc-2 and TFF3 in mice. The same results were also obtained from Lactobacillus casei strain Shirota (LcS) and the mixture of Lactobacillus acidophilus KLDS 1.0901, Lactobacillus helveticus KLDS 1.8701, and Lactobacillus plantarum KLDS 1.0318 [32, 44]. Interestingly, by comparing the adhesion ability to mucin of microbiota ranging from lactobacillus over fecal coliforms, bifidobacteria, and clostridia to total anaerobes, an in vitro adhesion experiment pointed out that it was Lactobacillus rhamnosus GG that adhered most selectively to mucin, indicating its crucial role in maintaining the mucus barrier [45].
To better demonstrate our statement about the mechanism underlying the barrier-protective effect of Lactobacillus in IBD, a figure was shown here to summarize our point of view. (Fig. 1)
Lactobacillus maintained the intestinal immune barrier by altering the number of immune cells and the expression level of inflammatory factors. At the same time, it strengthened the cellular barrier by affecting the tight junction of intestinal epithelial cells and the expression level of intracellular protective proteins. Finally, it strengthened the mucus barrier by increasing the expression of protective mucin.
The role of Lactobacillus in intestinal microbiota microenvironment in IBD
While the gut immune microenvironment of IBD patients was disrupted, their gut microbiota balance was also in a state of disorder. In detail, the abundance of Firmicutes, Verrucomicrobia, Akkermansia, and Lactobacillus, considered beneficial bacteria, decreased, while Bacteroidetes increased [46]. Due to the complexity of gut microbiota, the interaction between microorganisms in IBD should be taken seriously. Although the direct interaction between gut bacteria has not yet been fully elucidated, many microorganism supplements have been detected to affect the abundance of other intestinal flora in IBD-related studies. Therefore, it is inferred that they may have a synergistic and antagonistic relationship.
For example, the Lactobacillus plantarum Q7 supplement reduced the abundance of Proteobacteria, which was generally seen as pro-inflammatory bacteria, and increased the number of Bifidobacteria and Muribaculaceae, seen as anti-inflammatory genera [47]. The synergist of Lactobacillus and Bifidobacteria was also greatly important in another two studies focused on colitis and colitis-related depression [48, 49]. Aside from Lactobacillus and Bifidobacteria, different Lactobacillus strains, such as L. rhamnosus BY-02 and L. plantarum BY-05, also worked together and produced better results [50]. Moreover, it has been observed that Lactobacillus paracasei L9 improves colitis by expanding butyrate-producing bacteria such as Lachnospiraceae and Ruminococcaceae, which was observed reduced in colitis, indicating that they may have cooperation in treating colitis [11, 51].
Furthermore, the additional treatment of other bacteria may also influence the abundance of Lactobacillus. Pediococcus pentosaceus CECT 8330, a protective bacterium that could alleviate DSS-induced colitis, was found to elevate the quantity of Lactobacillus, Bifidobacterium as well as Dubosiella in mice intestine, suggesting that these bacteria may be in the same camp in alleviating enteritis [52]. Except for Pediococcus pentosaceus and Bacillus subtilis, Bifidobacterium bifidum was also proven to increase the amount of Lactobacillus and thus prevent colitis from exacerbating [53, 54].
When we mentioned the gut microenvironment of IBD patients, it was not only bacteria that should be considered. As we can anticipate, the intestinal condition of IBD patients is more complex than that of experimental colitis mice because of different microbial compositions and opportunistic infections caused by specific fungi. To better imitate the microenvironment in colitis, additional Candida albicans were colonized to the mouse gastrointestinal tract together with DSS administration as they do in the intestines of patients with colitis [55]. The results showed that Lactobacillus rhamnosus L34 could ameliorate gut local inflammation, gut-leakage severity, fecal dysbiosis, and systemic inflammation caused by opportunistic infection represented by Candida albicans in colitis, indicating the confrontation of Lactobacillus with pathogenic fungi to alleviate colitis in IBD [55].
Chinese herbal medicine and food that could enhance colitis and alter the abundance of Lactobacillus in IBD
As a regular probiotic in the intestine, the abundance of Lactobacillus is easily affected by food and oral medication. As a chronic disease prone to recurrence and persistence, the importance of daily diet and traditional Chinese medicine treatment should not be ignored in treating IBD. In this field, many traditional Chinese medicines have been pointed out in laboratory research to improve the abundance of Lactobacillus in the intestine while alleviating enteritis, such as Ampelopsis, Lithospermum, Rhubarb and so on [56,57,58]. Meanwhile, food containing fructooligosaccharides, glycerol monolaurate, Glycine, etc., was also beneficial for IBD alleviation [59,60,61]. After showcasing the many benefits of Lactobacillus in enteritis, we summarized the Chinese herbal medicines, foods, and their active ingredients that can change the abundance of Lactobacillus in IBD-related research (Table 1).
The role of Lactobacillus in IBD-related gut-liver axis
As the connections between different organs receive increasing attention, the gut-liver axis emerged as a new perspective for recognizing liver diseases. IBD and intestinal inflammation were addressed to be tightly associated with viral hepatitis, autoimmune hepatitis (AIH), primary biliary cirrhosis (PBC), and primary sclerosing cholangitis (PSC), with the link between regarded as gut commensals, pathogens, and intestinal antigens [62]. To illustrate, statistical data displayed that more than 75% of PSC patients simultaneously suffered from IBD, mostly UC [63]. A retrospective study on Chinese IBD patients revealed a higher prevalence of HBV infection in IBD patients than in non-IBD patients [64]. In addition, the application of immunosuppressive medicines in IBD caused a significantly higher trend of liver dysfunction in hepatitis virus carriers, especially the combined use of multiple immunosuppressants in HBV carriers [65]. Regarding HBV vaccination, the response rate to the HBV vaccination was also lower among IBD patients under anti-TNF therapy compared to healthy controls [66]. In terms of hepatocellular carcinoma, the upregulated inflammatory mediators also led to a positive correlation with the incidence rate of hepatocellular carcinoma in patients with IBD [67]. All the above revealed the close connection between IBD and liver diseases.
As a sterile organ, the liver is often the primary victim of intestinal inflammation accompanied by bacterial translocation. Therefore, in studies related to liver diseases, direct contact with bacteria often exacerbated the development of the disease, and Lactobacillus is no exception. Under intestinal inflammation, increased intestinal permeability allowed for bacterial translocation and passage from the portal vein into the liver, contributing to the pathogenesis of numerous diseases such as AIH and cholestatic liver disease. Specifically, the production of IL-17 by intrahepatic γδ T cells, pivotal in the exacerbation of cholestatic liver diseases, was observed up-regulated when γδ TCR+ cells were exposed to heat-killed Lactobacillus gasseri [68]. The same results were observed when Lactobacillus gasseri was intraperitoneally injected into mice, leading to increased serum levels of IL17 and inflammatory cell infiltration into the liver [68]. In AIH, it has been proved that a signaling pathway mediated by hydrocarbon receptor (AhR) was necessary for ongoing AIH-like pathology, and Lactobacillus reuteri could release an AhR ligand, indole-3-aldehyde (I3A), thus promoting the differentiation of CD8 T cells in vitro and AIH-like pathology in mice [69]. Therefore, hepatic translocation of Lactobacillus acted unfriendly to the outcome of liver diseases.
However, when the barrier function of the intestine was in a normal state or not wholly paralyzed, which indicated that the occurrence of bacterial translocation is not allowed, gratifying results emerged as the supplement of Lactobacillus in the gut could alleviate AIH severity through microbiota-gut-liver axis. To demonstrate, in experimental AIH, Lactobacillus rhamnosus GG supernatant treatment successfully limited liver damage with the existence of polymeric immunoglobulin receptors [70]. Meanwhile, in a clinical trial, the Lactobacillus supplement enhanced the suppressive effects of prednisone on the levels of clinical indexes in AIH patients [71]. After experiments in mice, the mechanism may be due to prednisone’s enhanced suppressive capability on Tfh cell proportion in peripheral blood monocytes through the TLR4/MyD88/NF-κB pathway after Lactobacillus application [71].
In summary, the impact of Lactobacillus on liver diseases under enteritis seemed to be a dynamic process influenced mainly by the integrity of the intestinal barrier. Anyway, the role of Lactobacillus in the gut liver axis is worthy of recognition, and how to grasp its balance point in gut liver axis-related diseases is also worth further exploration.
The role of Lactobacillus in IBD-related gut-brain axis
With the rise of gut-brain axis research, gut microbiota was emphasized to affect numerous central nervous system activities (CNS) activities. Other than interfering with brain shape in healthy conditions and resting-state brain function, microbiota also labored to commit numerous CNS diseases such as Alzheimer’s Disease (AD), depression, and anxiety [72, 73]. Here, we emphasized the role of Lactobacillus in the IBD-related microbiota-gut-brain axis (MGBA).
The role of Lactobacillus in memory and cognition
According to several extensive cohort studies, a significant parallel relationship existed between Alzheimer’s disease and IBD. At the same time, the credible explanation may be attributed to NLRP3-dependent neuroinflammation and accumulation of amyloid plaques induced by increased neutrophils [74,75,76]. As one of the typical symptoms of AD, the decline of memory and cognition has brought great psychological suffering to AD patients and their families. Hopefully, a recent study has uncovered a relationship between the gut microbiome and host memory and cognition in germ-free (GF) mice with supplementary microbiota or not. Specifically, supplementary Lactobacillus reuteri F275, Lactobacillus plantarum BDGP2 and Lactobacillus brevis BDGP6 significantly improved memory capacity compared to uninoculated GF mice, and Lactobacillus plantarum P8, as well as Lactobacillus casei ATCC 393, successfully enhanced cognitive traits of hosts, proclaiming the participation of Lactobacillus in preserving memory & cognition via MGBA [77,78,79].
To twig the way Lactobacillus acted in MGBA, many genera were tested in experiments for their function mechanism. In healthy mice, the benefit of Lactobacillus acidophilus in ameliorating cognition has already been verified, of which the critical factor was ascertained as butyrate Lactobacillus acidophilus produced [80]. As for the related signaling pathway, in the AD rodent model, ProBiotic-4, a probiotic preparation composed of Bifidobacterium lactis, Bifidobacterium bifidum, Lactobacillus acidophilus, and Lactobacillus casei altered the memory deficits, synaptic and cerebral neuronal injuries, of which the mechanism may be associated with inhibition of NF-κB signaling pathway mediated by TLR4 and RIG-I, with the comprehensive details remained to be explored [81]. What is more critical, CCAAT/enhancer binding protein β/asparagine endopeptidase (C/EBPβ/AEP) signaling pathway, cleaving Tau and β-amyloid precursor protein in the brain and resulting in the pathogenesis of AD, was proved to have existed in the gut of AD mouse model and possess a mutual interaction with AD progression in the brain. However, Lactobacillus salivarius inhibited the above signaling pathway and led to attenuated amyloidogenic processes in the gut, suggesting a probable therapeutic target in AD through MGBA [82].
The role of Lactobacillus in depression and anxiety
Highly comorbid with IBD and functional bowel disorders, depression and anxiety aroused worldwide concern. Meanwhile, the auxiliary mitigation of Lactobacillus in psychiatric disorders in IBD and other diseases, such as anxiety in the postpartum period, was reported in several clinical studies, with the comprehensive mechanism still requiring elucidation [83,84,85].
As one of the hypotheses of depression etiology, depression was used to being knitted together with inflammatory cytokines in the hippocampus. In this field, a crucial inflammatory factor, IL-1β, was observed downregulated by Lactobacillus gasseri NK109 with the simultaneous upregulated expression of brain-derived neurotrophic factor (BDNF) in the hippocampus of mice with cognitive impairment and depression induced by Escherichia coli K1, suggesting its alleviation in brain inflammation against neuropsychiatric disorders caused by bacterial infection [86]. Another key player who got involved in managing many physiological and psychological processes, GABA, was a primary inhibitory neurotransmitter in the CNS. In improving the behavioral performance of mice, Lactobacillus rhamnosus JB-1 was included and found to affect the expression of GABA receptors in the brain in a region-dependent manner. To put it more rigorously, Lactobacillus rhamnosus JB-1 was recorded to increase GABA(B1b) mRNA in cortical regions while reducing it in the hippocampus, amygdala, and locus coeruleus. As for GABA(Aα2), the expression was detected reduced in the prefrontal cortex and amygdala while increasing in the hippocampus [87]. As an additional remark, the effect of Lactobacillus rhamnosus JB-1 in depression and anxiety was CD4 + CD25 + T cells dependent [88]. Set aside as neurotransmitters, enzymes got affected, too. As a noteworthy factor whose activity seen to correlate with depression in the cerebral cortex, xanthine oxidase was also inhibited by Lactobacillus paracasei CCFM1229 and Lactobacillus rhamnosus CCFM1228, which also became an essential link between Lactobacillus intervention in depression [89] Expectedly, there also existed researches attributing the protective effect of Lactobacillus to its product such as ergothioneine produced by Lactobacillus reuteri. The oral administration of ergothioneine had a preventative effect on depressive behaviors induced by social defeat stress (SDS) in rodents, especially on sleep abnormalities in the rapid eye movement sleep phase [90]. These alterations indicated the possible mechanism Lactobacillus may hold to affect emotion and behavior.
Moreover, given the benefits humanity could gain from Lactobacillus, researchers began trying to prevent diseases before they happened and made a breakthrough. The early life colonization of Lactobacillus rhamnosus could relieve anxiety-like behavior in adulthood with an accompanying increased abundance of beneficial bacteria such as Akkermansia and Bifidobacteria in rodent intestine, proclaiming the necessity of lactobacillus supplementary in the absence of disease [91].
In a word, to portray the role of Lactobacillus in the gut-liver axis and gut-brain axis more intuitively, we exhibited a figure here to describe the process involved (Fig. 2).
The role of Lactobacillus in the gut–liver axis was related to the severity of enteritis, which was directly proportional to the integrity of the intestinal barrier. In neurological diseases, due to the presence of the blood–brain barrier, metabolites of Lactobacillus had a certain alleviating effect on cognition, memory, depression and anxiety.
The role of Lactobacillus in CAC
In consideration of the relationship between IBD and Colitis-associated Colorectal cancer (CAC), as well as the anti-inflammatory effect of Lactobacillus, wonders were raised whether Lactobacillus would have the anti-tumor ability in tumorigenesis or therapeutic capability in the treatment of CAC. First but not foremost, an Anti-tumor effect was observed in Lactobacillus bulgaricus, of which the administration inhibited mean tumor size and total tumor volume in azoxymethane (AOM)/ DSS-induced CAC mouse model with remarkably reduced pro-inflammatory cytokines containing IL-6, TNF-α, IL-1β, IL-17, and IL-23 [92]. Similarly, a specific polysaccharide-peptidoglycan complex (PSPG) derived from specific Lactobacillus casei Shirota, but not other strains, was also proclaimed to limit tumor growth via inhibiting the activation of the IL-6/STAT3 signaling pathway [93]. In the aspect of the tumor stage, the anti-proliferation effect of Lactobacillus helveticus NS8 in enterocytes was found to be more efficient at the early stage of CAC, indicating its vital role in the prevention of tumorigenesis [94].
Given the anti-tumor effect of single strains, the mixture of lactobacillus and other probiotics was also attached to attention and obtained lots of expected results. A probiotic combination of Lactobacillus acidophilus, Bifidobacterium bifidum, and Lactobacillus rhamnosus showed its potential chemo-preventive effect as it hampered tumor growth in both number and volume in mice with AOM/DSS induced CAC [95]. Compared with probiotics, research on symbiotics has also been a hotspot recently. Synbiotics refers to combining probiotics and prebiotics or adding vitamins, trace elements, etc. Synbiotics can exert the physiological bacterial activity of probiotics and selectively and rapidly increase the number of such bacteria, making the probiotics’ function more significant and lasting [96]. It has been reported that synbiotics offered help in the inhibition of CAC in a research program that claimed that FCT, a synbiotic consisting of Lactobacillus gasseri 505 and cudrania tricuspidata leaf extract, successfully reduced incidence of colonic tumors, as well as damage to the colonic mucosa with significantly downregulated pro-inflammatory cytokines, upregulated TJs and increased pro-apoptotic factors such as p53, p21, and Bax, proclaiming its therapeutic value in CAC [97]. The role of Lactobacillus in CAC is displayed in figure (Fig. 3).
The role of Lactobacillus in CAC varied with disease progression. In the stage of enteritis, it inhibited the expression of inflammatory factors and hindered related signaling pathways. In the stage of dysplasia, it not only hindered the progression of CAC in the early stage, but also promoted tumor cell apoptosis during the advanced stage, thereby delaying the progression of CAC.
Lactobacillus-related treatment in IBD and IBD-related diseases
As the same principle as the application of Lactobacillus acidophilus in the fermentation industry, to better take advantage of the anti-inflammatory benefits of Lactobacillus, development in reverse engineering of anti-inflammatory fermented foods specially designed for IBD patients was brought into the agenda. At the laboratory stage, in mice with m2,4,6-trinitrobenzene sulfonic acid (TNBS)-induced colitis, single-strain lactobacillus-fermented milk, as well as an experimental pressed cheese fermented by two strains comprised of Lactobacillus delbrueckii and Propionibacterium freudenreichii, another probiotic featured by producing propionic acid and acetic acid from carbohydrate, was observed to modulate intestinal and systemic inflammation, relieve the severity of symptoms, meanwhile offer adequate protection against not only colonic oxidative stress but epithelial cell damages [98]. In addition, compared with the therapeutic value of a specific single strain, probiotic consortia containing Lactobacillus reuteri, Lactobacillus gasseri, Lactobacillus acidophilus, and Bifidobacterium lactis were demonstrated to better ameliorate DSS-induced colitis in the mouse model, with their mixed metabolites receiving slightly inferior benefits by comparison with the whole strain [99].
As we have put it before, synbiotics, a combination of probiotics and prebiotics, or the addition of vitamins, trace elements, and so on, have been widely used in IBD-related studies recently. Among various synbiotics, vitamin D (VitD) became an emerging component demonstrating rapport with Lactobacillus in relieving intestinal inflammation [100]. To illustrate, VitD levels were usually negatively correlated with IBD activity. However, VitD supplementation alone failed to reduce IBD severity since its effect was limited by the downregulation of vitamin D receptor (VDR), whose downregulation resulted in damaged autophagy in inflammatory status [101]. At this point, Lactobacillus was recorded to restore the hindered expression of VDR in human cell line HCT116 and intestinal organoids, and Lactobacillus rhamnosus GG secreting p40 demonstrate good partnership with VitD in promoting colonic epithelial proliferation and alleviating colitis in mice, proposing a promising combination in clinical application [101, 102].
In the innovative attempt to treat IBD, Fecal Microbiota Transplantation (FMT) has achieved particular success. Surprisingly, the relative abundance of Lactobacillus after antibiotics positively correlated with engraftment in FMT and improved clinical reaction. Therefore, it may be possible to try moderately supplementing Lactobacillus after antibiotic cleaning to enhance the clinical efficacy of FMT and better alleviate colitis in IBD patients.
In recent years, in addition to traditional salicylic acid preparations and hormones, biological agents have greatly alleviated the severity of enteritis in the clinical treatment of IBD patients. Among them, the most commonly used monoclonal antibodies in clinical practice are infliximab, adalimumab, ustekinumab, and vedolizumab. In this area, co-administration of Lactobacillus gasseri and tumor necrosis factor-alpha inhibitor infliximab improved colitis in mice [103]. At a deeper level of clinical application, we have noticed that multiple studies have mentioned the correlation between the efficacy of biological agents and the composition of gut microbiota in patients [104]. However, due to insufficient sample size and limited research cases, there is currently no research to make a judgment on whether Lactobacillus can be used as a biological agent for efficacy prediction, which is precisely what we want to emphasize: more research ought to be invested in evaluating the predictive and monitoring effects of Lactobacillus on IBD.
Considering their remarkable anti-inflammatory benefits, the therapeutic application of Lactobacillus in patients with IBD and IBD-related diseases was on the way. Some of them have already been implemented with a result published and available to the public, and some of them were still in recruiting or even just taken shape. Here, a table that offered an overview of relative clinical trials comprised of projects in progress was listed to facilitate researchers and patients to search for helpful information (Table 2).
Conclusions and prospects
Undoubtedly, as the most common probiotics, Lactobacillus played a vital role in maintaining the ecological balance of intestinal flora since it exerted excellent anti-inflammatory effects in IBD and IBD-related intestinal diseases such as CAC, as well as CNS diseases and liver diseases represented by AD, PD, and AIH, in both mouse model and clinical patients ranging from children to adults. As a symbiotic existence with the host, it helped to maintain the immune microenvironment in the intestinal mucosa, confine the over-activation of inflammatory signals, and safeguard IECs from multifarious threats to support patients in overcoming the intestinal inflammatory storm. Though sharing numerous resemblances, each stain’s anti-inflammatory principle and functional component were not identical because of the specific characteristics of different subspecies. Therefore, the combined utilization of different strains of Lactobacillus to develop more efficient probiotics or to jointly use Lactobacillus with other probiotics or prebiotics will become a powerful adjuvant therapy to meet the requirement of patients suffering from IBD and IBD-related diseases. In this regard, emerging microorganisms in recent years, such as Akkermansia muciniphila, Ruminococcus gnavus, and so on, may be called powerful candidates to deliver a partnership with Lactobacillus, which still demands experimental verification.
With the development and popularization of various new technologies, multiple sequencing techniques have gradually been used to study gut microbiota, including Lactobacillus. To cite a case, a combination of global RNA sequencing of human biopsies and bacterial DNA sequencing was carried out to precisely describe the effects of Lactobacillus rhamnosus GG on the human intestine, displaying an activation and proliferation of existing B cells in jejunum and proposing that the treatment of probiotics should be individualized [105]. In addition, to better describe the effect of exogenous prebiotics on overall gut microbiome stability in probiotic consumption, shotgun metagenomic sequencing successfully pointed out that continuous galactooligosaccharide supplement could promote the growth of Lactobacillus plantarum and decreased its single-nucleotide polymorphisms (SNPs) mutation under competitive conditions [106]. In brief, sequencing techniques have become a method that can accurately reflect the relationship between probiotics and the host gut immune microenvironment.
In the author’s view, although Lactobacillus has been proven to have many anti-inflammatory effects in mice, its clinical efficacy is still hindered by issues such as low vitality and low bioavailability in gastrointestinal transportation. Research in Ligilactobacillus salivarius developed a new packaging method for probiotics, which means layer-by-layer (LbL) encapsulating a single bacterium with chitosan and alginate to tremendously increase the potential of Ligilactobacillus salivarius in alleviating colitis [107]. Moreover, an adhesive core-shell hydrogel microsphere, colon-targeted, was fabricated by advanced gas-shearing technology and ionic diffusion method to prolong the local drug dwell time. Thus, we eagerly anticipate applying similar technologies in the colon-targeted transportation of Lactobacillus to improve their bioavailability [108]. Therefore, while we focus on the rational combination of probiotics with probiotics or prebiotics, an effective packaging method for probiotics seems to double our efforts with half the effort.
In the end, we emphatically proclaim the magnitude of Lactobacillus in the gut-liver axis and gut-brain axis and appeal for more attention on probiotics in communication between multiple systems, which will provide more options for relieving patients with IBD-related diseases from affliction.
References
Kaplan GG, Windsor JW. The four epidemiological stages in the global evolution of inflammatory bowel disease. Nat Rev Gastroenterol Hepatol. 2021;18:56–66.
Magro F, Langner C, Driessen A, Ensari A, Geboes K, Mantzaris GJ, et al. European consensus on the histopathology of inflammatory bowel disease. J Crohn’s Colitis. 2013;7:827–51.
Lozupone CA, Stombaugh JI, Gordon JI, Jansson JK, Knight R. Diversity, stability and resilience of the human gut microbiota. Nature. 2012;489:220–30.
Butler S, O’Dwyer JP. Stability criteria for complex microbial communities. Nat Commun. 2018;9:2970.
Ganji-Arjenaki M, Rafieian-Kopaei M. Probiotics are a good choice in remission of inflammatory bowel diseases: a meta-analysis and systematic review. J Cell Physiol. 2018;233:2091–103.
Heeney DD, Gareau MG, Marco ML. Intestinal Lactobacillus in health and disease, a driver or just along for the ride? Curr Opin Biotechnol. 2018;49:140–7.
Almonacid DE, Kraal L, Ossandon FJ, Budovskaya YV, Cardenas JP, Bik EM, et al. Correction: 16S rRNA gene sequencing and healthy reference ranges for 28 clinically relevant microbial taxa from the human gut microbiome. PLoS One. 2019;14:e0212474.
Nistal E, Caminero A, Herrán AR, Pérez-Andres J, Vivas S, Ruiz de Morales JM, et al. Study of duodenal bacterial communities by 16S rRNA gene analysis in adults with active celiac disease vs. non-celiac disease controls. J Appl Microbiol. 2016;120:1691–700.
Strus M, Janczyk A, Gonet-Surowka A, Brzychczy-Wloch M, Stochel G, Kochan P, et al. Effect of hydrogen peroxide of bacterial origin on apoptosis and necrosis of gut mucosa epithelial cells as a possible pathomechanism of inflammatory bowel disease and cancer. J Physiol Pharm. 2009;60:55–60.
Lewis JD, Chen EZ, Baldassano RN, Otley AR, Griffiths AM, Lee D, et al. Inflammation, antibiotics, and diet as environmental stressors of the gut microbiome in pediatric Crohn’s disease. Cell Host Microbe. 2017;22:247.
Wang W, Chen L, Zhou R, Wang X, Song L, Huang S, et al. Increased proportions of Bifidobacterium and the Lactobacillus group and loss of butyrate-producing bacteria in inflammatory bowel disease. J Clin Microbiol. 2014;52:398–406.
Ueno A, Jijon H, Chan R, Ford K, Hirota C, Kaplan GG, et al. Increased prevalence of circulating novel IL-17 secreting Foxp3 expressing CD4+ T cells and defective suppressive function of circulating Foxp3+ regulatory cells support plasticity between Th17 and regulatory T cells in inflammatory bowel disease patients. Inflamm Bowel Dis. 2013;19:2522–34.
Geng X, Xue J. Expression of Treg/Th17 cells as well as related cytokines in patients with inflammatory bowel disease. Pak J Med Sci. 2016;32:1164–8.
Zhu XM, Shi YZ, Cheng M, Wang DF, Fan JF. Serum IL-6, IL-23 profile and Treg/Th17 peripheral cell populations in pediatric patients with inflammatory bowel disease. Pharmazie. 2017;72:283–7.
Fu W, Fu H, Ye W, Han Y, Liu X, Zhu S, et al. Peripheral blood neutrophil-to-lymphocyte ratio in inflammatory bowel disease and disease activity: a meta-analysis. Int Immunopharmacol. 2021;101:108235.
Liu H, Dasgupta S, Fu Y, Bailey B, Roy C, Lightcap E, et al. Subsets of mononuclear phagocytes are enriched in the inflamed colons of patients with IBD. BMC Immunol. 2019;20:42.
Liu HY, Gu F, Zhu C, Yuan L, Zhu C, Zhu M, et al. Epithelial heat shock proteins mediate the protective effects of limosilactobacillus reuteri in dextran sulfate sodium-induced colitis. Front Immunol. 2022;13:865982.
Jia L, Wu R, Han N, Fu J, Luo Z, Guo L, et al. Porphyromonas gingivalis and Lactobacillus rhamnosus GG regulate the Th17/Treg balance in colitis via TLR4 and TLR2. Clin Transl Immunol. 2020;9:e1213.
Chiu YH, Hsieh YJ, Liao KW, Peng KC. Preferential promotion of apoptosis of monocytes by Lactobacillus casei rhamnosus soluble factors. Clin Nutr. 2010;29:131–40.
Shapouri-Moghaddam A, Mohammadian S, Vazini H, Taghadosi M, Esmaeili SA, Mardani F, et al. Macrophage plasticity, polarization, and function in health and disease. J Cell Physiol. 2018;233:6425–40.
Dias AMM, Douhard R, Hermetet F, Regimbeau M, Lopez TE, Gonzalez D, et al. Lactobacillus stress protein GroEL prevents colonic inflammation. J Gastroenterol. 2021;56:442–55.
Foligne B, Zoumpopoulou G, Dewulf J, Ben Younes A, Chareyre F, Sirard JC, et al. A key role of dendritic cells in probiotic functionality. PLoS One. 2007;2:e313.
Li Y, Yang S, Lun J, Gao J, Gao X, Gong Z, et al. Inhibitory effects of the Lactobacillus rhamnosus GG effector protein HM0539 on inflammatory response through the TLR4/MyD88/NF-кB axis. Front Immunol. 2020;11:551449.
Sato N, Garcia-Castillo V, Yuzawa M, Islam MA, Albarracin L, Tomokiyo M, et al. Immunobiotic Lactobacillus jensenii TL2937 alleviates dextran sodium sulfate-induced colitis by differentially modulating the transcriptomic response of intestinal epithelial cells. Front Immunol. 2020;11:2174.
Llopis M, Antolin M, Carol M, Borruel N, Casellas F, Martinez C, et al. Lactobacillus casei downregulates commensals’ inflammatory signals in Crohn’s disease mucosa. Inflamm Bowel Dis. 2009;15:275–83.
Pan Y, Ning Y, Hu J, Wang Z, Chen X, Zhao X. The preventive effect of Lactobacillus plantarum ZS62 on DSS-induced IBD by regulating oxidative stress and the immune response. Oxid Med Cell Longev. 2021;2021:9416794.
Martins AJ, Colquhoun P, Reid G, Kim SO. Reduced expression of basal and probiotic-inducible G-CSF in intestinal mononuclear cells is associated with inflammatory bowel disease. Inflamm Bowel Dis. 2009;15:515–25.
Macho Fernandez E, Valenti V, Rockel C, Hermann C, Pot B, Boneca IG, et al. Anti-inflammatory capacity of selected lactobacilli in experimental colitis is driven by NOD2-mediated recognition of a specific peptidoglycan-derived muropeptide. Gut. 2011;60:1050–9.
von Schillde MA, Hörmannsperger G, Weiher M, Alpert CA, Hahne H, Bäuerl C, et al. Lactocepin secreted by Lactobacillus exerts anti-inflammatory effects by selectively degrading proinflammatory chemokines. Cell Host Microbe. 2012;11:387–96.
Hoermannsperger G, Clavel T, Hoffmann M, Reiff C, Kelly D, Loh G, et al. Post-translational inhibition of IP-10 secretion in IEC by probiotic bacteria: impact on chronic inflammation. PLoS One. 2009;4:e4365.
Tsukita S, Furuse M, Itoh M. Multifunctional strands in tight junctions. Nat Rev Mol Cell Biol. 2001;2:285–93.
Shi J, Xie Q, Yue Y, Chen Q, Zhao L, Evivie SE, et al. Gut microbiota modulation and anti-inflammatory properties of mixed lactobacilli in dextran sodium sulfate-induced colitis in mice. Food Funct. 2021;12:5130–43.
Zhang Y, Zhao X, Zhu Y, Ma J, Ma H, Zhang H. Probiotic mixture protects dextran sulfate sodium-induced colitis by altering tight junction protein expressions and increasing tregs. Mediators Inflamm. 2018;2018:9416391.
Tao Y, Drabik KA, Waypa TS, Musch MW, Alverdy JC, Schneewind O, et al. Soluble factors from Lactobacillus GG activate MAPKs and induce cytoprotective heat shock proteins in intestinal epithelial cells. Am J Physiol Cell Physiol. 2006;290:C1018–30.
Kruidenier L, Kuiper I, van Duijn W, Marklund SL, van Hogezand RA, Lamers CB, et al. Differential mucosal expression of three superoxide dismutase isoforms in inflammatory bowel disease. J Pathol. 2003;201:7–16.
Carroll IM, Andrus JM, Bruno-Bárcena JM, Klaenhammer TR, Hassan HM, Threadgill DS. Anti-inflammatory properties of Lactobacillus gasseri expressing manganese superoxide dismutase using the interleukin 10-deficient mouse model of colitis. Am J Physiol Gastrointest Liver Physiol. 2007;293:G729–38.
Sengül N, Işık S, Aslım B, Uçar G, Demirbağ AE. The effect of exopolysaccharide-producing probiotic strains on gut oxidative damage in experimental colitis. Dig Dis Sci. 2011;56:707–14.
Salyers AA, Pajeau M, McCarthy RE. Importance of mucopolysaccharides as substrates for Bacteroides thetaiotaomicron growing in intestinal tracts of exgermfree mice. Appl Environ Microbiol. 1988;54:1970–6.
Salyers AA, Vercellotti JR, West SE, Wilkins TD. Fermentation of mucin and plant polysaccharides by strains of Bacteroides from the human colon. Appl Environ Microbiol. 1977;33:319–22.
Lee HS, Han SY, Bae EA, Huh CS, Ahn YT, Lee JH, et al. Lactic acid bacteria inhibit proinflammatory cytokine expression and bacterial glycosaminoglycan degradation activity in dextran sulfate sodium-induced colitic mice. Int Immunopharmacol. 2008;8:574–80.
Van der Sluis M, De Koning BA, De Bruijn AC, Velcich A, Meijerink JP, Van Goudoever JB, et al. Muc2-deficient mice spontaneously develop colitis, indicating that MUC2 is critical for colonic protection. Gastroenterology. 2006;131:117–29.
Paone P, Cani PD. Mucus barrier, mucins and gut microbiota: the expected slimy partners? Gut. 2020;69:2232–43.
Bhatia R, Sharma S, Bhadada SK, Bishnoi M, Kondepudi KK. Lactic acid bacterial supplementation ameliorated the lipopolysaccharide-induced gut inflammation and dysbiosis in mice. Front Microbiol. 2022;13:930928.
Wong WY, Chan BD, Sham TT, Lee MM, Chan CO, Chau CT, et al. Lactobacillus casei strain shirota ameliorates dextran sulfate sodium-induced colitis in mice by increasing taurine-conjugated bile acids and inhibiting NF-κB signaling via stabilization of IκBα. Front Nutr. 2022;9:816836.
Van den Abbeele P, Grootaert C, Possemiers S, Verstraete W, Verbeken K, Van de Wiele T. In vitro model to study the modulation of the mucin-adhered bacterial community. Appl Microbiol Biotechnol. 2009;83:349–59.
Huang P, Wang X, Wang S, Wu Z, Zhou Z, Shao G, et al. Treatment of inflammatory bowel disease: potential effect of NMN on intestinal barrier and gut microbiota. Curr Res Food Sci. 2022;5:1403–11.
Hao H, Zhang X, Tong L, Liu Q, Liang X, Bu Y, et al. Effect of extracellular vesicles derived from Lactobacillus plantarum Q7 on gut microbiota and ulcerative colitis in mice. Front Immunol. 2021;12:777147.
Yoo JW, Shin YJ, Ma X, Son YH, Jang HM, Lee CK, et al. The alleviation of gut microbiota-induced depression and colitis in mice by anti-inflammatory probiotics NK151, NK173, and NK175. Nutrients. 2022;14:2080.
Li SC, Hsu WF, Chang JS, Shih CK. Combination of Lactobacillus acidophilus and bifidobacterium animalis subsp. lactis shows a stronger anti-inflammatory effect than individual strains in HT-29 cells. Nutrients. 2019;11:969.
Liu Y, Zhang H, Xie A, Sun J, Yang H, Li J, et al. Lactobacillus rhamnosus and L. plantarum combination treatment ameliorated colitis symptoms in a mouse model by altering intestinal microbial composition and suppressing inflammatory response. Mol Nutr Food Res. 2023;67:e2200340.
Deng M, Wu X, Duan X, Xu J, Yang X, Sheng X, et al. Lactobacillus paracasei L9 improves colitis by expanding butyrate-producing bacteria that inhibit the IL-6/STAT3 signaling pathway. Food Funct. 2021;12:10700–13.
Dong F, Xiao F, Li X, Li Y, Wang X, Yu G, et al. Pediococcus pentosaceus CECT 8330 protects DSS-induced colitis and regulates the intestinal microbiota and immune responses in mice. J Transl Med. 2022;20:33.
Zhang X, Tong Y, Lyu X, Wang J, Wang Y, Yang R. Prevention and alleviation of dextran sulfate sodium salt-induced inflammatory bowel disease in mice with bacillus subtilis-fermented milk via inhibition of the inflammatory responses and regulation of the intestinal flora. Front Microbiol. 2020;11:622354.
Feng C, Zhang W, Zhang T, He Q, Kwok LY, Tan Y, et al. Heat-killed Bifidobacterium bifidum B1628 may alleviate dextran sulfate sodium-induced colitis in mice, and the anti-inflammatory effect is associated with gut microbiota modulation. Nutrients. 2022;14:5233.
Panpetch W, Hiengrach P, Nilgate S, Tumwasorn S, Somboonna N, Wilantho A, et al. Additional Candida albicans administration enhances the severity of dextran sulfate solution induced colitis mouse model through leaky gut-enhanced systemic inflammation and gut-dysbiosis but attenuated by Lactobacillus rhamnosus L34. Gut Microbes. 2020;11:465–80.
Dong S, Zhu M, Wang K, Zhao X, Hu L, Jing W, et al. Dihydromyricetin improves DSS-induced colitis in mice via modulation of fecal-bacteria-related bile acid metabolism. Pharm Res. 2021;171:105767.
Lin H, Ma X, Yang X, Chen Q, Wen Z, Yang M, et al. Natural shikonin and acetyl-shikonin improve intestinal microbial and protein composition to alleviate colitis-associated colorectal cancer. Int Immunopharmacol. 2022;111:109097.
Wu J, Wei Z, Cheng P, Qian C, Xu F, Yang Y, et al. Rhein modulates host purine metabolism in intestine through gut microbiota and ameliorates experimental colitis. Theranostics. 2020;10:10665–79.
Liao M, Zhang Y, Qiu Y, Wu Z, Zhong Z, Zeng X, et al. Fructooligosaccharide supplementation alleviated the pathological immune response and prevented the impairment of intestinal barrier in DSS-induced acute colitis mice. Food Funct. 2021;12:9844–54.
Mo Q, Liu T, Fu A, Ruan S, Zhong H, Tang J, et al. Novel gut microbiota patterns involved in the attenuation of dextran sodium sulfate-induced mouse colitis mediated by glycerol monolaurate via inducing anti-inflammatory responses. mBio. 2021;12:e0214821.
Zhang Y, Jiang D, Jin Y, Jia H, Yang Y, Kim IH, et al. Glycine attenuates Citrobacter rodentium-induced colitis by regulating ATF6-mediated endoplasmic reticulum stress in mice. Mol Nutr Food Res. 2021;65:e2001065.
Trivedi PJ, Adams DH. Mucosal immunity in liver autoimmunity: a comprehensive review. J Autoimmun. 2013;46:97–111.
Yimam KK, Bowlus CL. Diagnosis and classification of primary sclerosing cholangitis. Autoimmun Rev. 2014;13:445–50.
Huang ML, Xu XT, Shen J, Qiao YQ, Dai ZH, Ran ZH. Prevalence and factors related to hepatitis B and C infection in inflammatory bowel disease patients in China: a retrospective study. J Crohns Colitis. 2014;8:282–7.
Loras C, Gisbert JP, Mínguez M, Merino O, Bujanda L, Saro C, et al. Liver dysfunction related to hepatitis B and C in patients with inflammatory bowel disease treated with immunosuppressive therapy. Gut. 2010;59:1340–6.
Gisbert JP, Villagrasa JR, Rodríguez-Nogueiras A, Chaparro M. Efficacy of hepatitis B vaccination and revaccination and factors impacting on response in patients with inflammatory bowel disease. Am J Gastroenterol. 2012;107:1460–6.
Aleksandrova K, Boeing H, Nöthlings U, Jenab M, Fedirko V, Kaaks R, et al. Inflammatory and metabolic biomarkers and risk of liver and biliary tract cancer. Hepatology. 2014;60:858–71.
Tedesco D, Thapa M, Chin CY, Ge Y, Gong M, Li J, et al. Alterations in intestinal microbiota lead to production of interleukin 17 by intrahepatic γδ T-cell receptor-positive cells and pathogenesis of cholestatic liver disease. Gastroenterology. 2018;154:2178–93.
Pandey SP, Bender MJ, McPherson AC, Phelps CM, Sanchez LM, Rana M, et al. Tet2 deficiency drives liver microbiome dysbiosis triggering Tc1 cell autoimmune hepatitis. Cell Host Microbe. 2022;30:1003–19.e10.
Lin H, Lin J, Pan T, Li T, Jiang H, Fang Y, et al. Polymeric immunoglobulin receptor deficiency exacerbates autoimmune hepatitis by inducing intestinal dysbiosis and barrier dysfunction. Cell Death Dis. 2023;14:68.
Ma L, Zhang L, Zhuang Y, Ding Y, Chen J. Lactobacillus improves the effects of prednisone on autoimmune hepatitis via gut microbiota-mediated follicular helper T cells. Cell Commun Signal. 2022;20:83.
Rode J, Edebol Carlman HMT, König J, Hutchinson AN, Thunberg P, Persson J, et al. Multi-strain probiotic mixture affects brain morphology and resting state brain function in healthy subjects: an RCT. Cells. 2022;11:2922.
Kim GH, Lee YC, Kim TJ, Kim ER, Hong SN, Chang DK, et al. Risk of neurodegenerative diseases in patients with inflammatory bowel disease: a nationwide population-based cohort study. J Crohns Colitis. 2022;16:436–43.
Zhang B, Wang HE, Bai YM, Tsai SJ, Su TP, Chen TJ, et al. Inflammatory bowel disease is associated with higher dementia risk: a nationwide longitudinal study. Gut. 2021;70:85–91.
Kaneko R, Matsui A, Watanabe M, Harada Y, Kanamori M, Awata N, et al. Increased neutrophils in inflammatory bowel disease accelerate the accumulation of amyloid plaques in the mouse model of Alzheimer’s disease. Inflamm Regen. 2023;43:20.
He XF, Li LL, Xian WB, Li MY, Zhang LY, Xu JH, et al. Chronic colitis exacerbates NLRP3-dependent neuroinflammation and cognitive impairment in middle-aged brain. J Neuroinflammation. 2021;18:153.
Lew LC, Hor YY, Yusoff NAA, Choi SB, Yusoff MSB, Roslan NS, et al. Probiotic Lactobacillus plantarum P8 alleviated stress and anxiety while enhancing memory and cognition in stressed adults: a randomised, double-blind, placebo-controlled study. Clin Nutr. 2019;38:2053–64.
Mao JH, Kim YM, Zhou YX, Hu D, Zhong C, Chang H, et al. Correction to: genetic and metabolic links between the murine microbiome and memory. Microbiome. 2020;8:73.
Qiao L, Chen Y, Song X, Dou X, Xu C. Selenium nanoparticles-enriched Lactobacillus casei ATCC 393 prevents cognitive dysfunction in mice through modulating microbiota-gut-brain axis. Int J Nanomed. 2022;17:4807–27.
Jeon S, Kim H, Kim J, Seol D, Jo J, Choi Y, et al. Positive effect of Lactobacillus acidophilus EG004 on cognitive ability of healthy mice by fecal microbiome analysis using full-length 16S-23S rRNA metagenome sequencing. Microbiol Spectr. 2022;10:e0181521.
Yang X, Yu D, Xue L, Li H, Du J. Probiotics modulate the microbiota-gut-brain axis and improve memory deficits in aged SAMP8 mice. Acta Pharm Sin B. 2020;10:475–87.
Chen C, Ahn EH, Kang SS, Liu X, Alam A, Ye K. Gut dysbiosis contributes to amyloid pathology, associated with C/EBPβ/AEP signaling activation in Alzheimer’s disease mouse model. Sci Adv. 2020;6:eaba0466.
Diaz Heijtz R, Wang S, Anuar F, Qian Y, Björkholm B, Samuelsson A, et al. Normal gut microbiota modulates brain development and behavior. Proc Natl Acad Sci USA. 2011;108:3047–52.
Lyte M, Li W, Opitz N, Gaykema RP, Goehler LE. Induction of anxiety-like behavior in mice during the initial stages of infection with the agent of murine colonic hyperplasia Citrobacter rodentium. Physiol Behav. 2006;89:350–7.
Slykerman RF, Hood F, Wickens K, Thompson JMD, Barthow C, Murphy R, et al. Effect of Lactobacillus rhamnosus HN001 in pregnancy on postpartum symptoms of depression and anxiety: a randomised double-blind placebo-controlled trial. EBioMedicine. 2017;24:159–65.
Yun SW, Kim JK, Lee KE, Oh YJ, Choi HJ, Han MJ, et al. A probiotic Lactobacillus gasseri alleviates escherichia coli-induced cognitive impairment and depression in mice by regulating IL-1β expression and gut microbiota. Nutrients. 2020;12:3441.
Bravo JA, Forsythe P, Chew MV, Escaravage E, Savignac HM, Dinan TG, et al. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc Natl Acad Sci USA. 2011;108:16050–5.
Liu Y, Mian MF, McVey Neufeld KA, Forsythe P. CD4(+)CD25(+) T cells are essential for behavioral effects of Lactobacillus rhamnosus JB-1 in male BALB/c mice. Brain Behav Immun. 2020;88:451–60.
Xu M, Tian P, Zhu H, Zou R, Zhao J, Zhang H, et al. Lactobacillus paracasei CCFM1229 and Lactobacillus rhamnosus CCFM1228 alleviated depression- and anxiety-related symptoms of chronic stress-induced depression in mice by regulating xanthine oxidase activity in the brain. Nutrients. 2022;14:1294.
Matsuda Y, Ozawa N, Shinozaki T, Wakabayashi KI, Suzuki K, Kawano Y, et al. Ergothioneine, a metabolite of the gut bacterium Lactobacillus reuteri, protects against stress-induced sleep disturbances. Transl Psychiatry. 2020;10:170.
Zhou B, Jin G, Pang X, Mo Q, Bao J, Liu T, et al. Lactobacillus rhamnosus GG colonization in early life regulates gut-brain axis and relieves anxiety-like behavior in adulthood. Pharm Res. 2022;177:106090.
Silveira DSC, Veronez LC, Lopes-Júnior LC, Anatriello E, Brunaldi MO, Pereira-da-Silva G. Lactobacillus bulgaricus inhibits colitis-associated cancer via a negative regulation of intestinal inflammation in azoxymethane/dextran sodium sulfate model. World J Gastroenterol. 2020;26:6782–94.
Matsumoto S, Hara T, Nagaoka M, Mike A, Mitsuyama K, Sako T, et al. A component of polysaccharide peptidoglycan complex on Lactobacillus induced an improvement of murine model of inflammatory bowel disease and colitis-associated cancer. Immunology. 2009;128:e170–80.
Rong J, Liu S, Hu C, Liu C. Single probiotic supplement suppresses colitis-associated colorectal tumorigenesis by modulating inflammatory development and microbial homeostasis. J Gastroenterol Hepatol. 2019;34:1182–92.
Mendes MCS, Paulino DS, Brambilla SR, Camargo JA, Persinoti GF, Carvalheira JBC. Microbiota modification by probiotic supplementation reduces colitis associated colon cancer in mice. World J Gastroenterol. 2018;24:1995–2008.
Markowiak P, Śliżewska K. Effects of probiotics, prebiotics, and synbiotics on human health. Nutrients. 2017;9:1021.
Oh NS, Lee JY, Kim YT, Kim SH, Lee JH. Cancer-protective effect of a synbiotic combination between Lactobacillus gasseri 505 and a Cudrania tricuspidata leaf extract on colitis-associated colorectal cancer. Gut Microbes. 2020;12:1785803.
Plé C, Breton J, Richoux R, Nurdin M, Deutsch SM, Falentin H, et al. Combining selected immunomodulatory Propionibacterium freudenreichii and Lactobacillus delbrueckii strains: Reverse engineering development of an anti-inflammatory cheese. Mol Nutr Food Res. 2016;60:935–48.
Xu L, Liu B, Huang L, Li Z, Cheng Y, Tian Y, et al. Probiotic consortia and their metabolites ameliorate the symptoms of inflammatory bowel diseases in a colitis mouse model. Microbiol Spectr. 2022;10:e0065722.
Costanzo M, Cesi V, Palone F, Pierdomenico M, Colantoni E, Leter B, et al. Krill oil, vitamin D and Lactobacillus reuteri cooperate to reduce gut inflammation. Benef Microbes. 2018;9:389–99.
Chen D, Tang H, Li Y, Yang H, Wang H, Tan B, et al. Vitamin D3 and Lactobacillus rhamnosus GG/p40 synergize to protect mice from colitis by promoting Vitamin D receptor expression and epithelial proliferation. Inflamm Bowel Dis. 2023;29:620–32.
Lu R, Shang M, Zhang YG, Jiao Y, Xia Y, Garrett S, et al. Lactic Acid Bacteria Isolated From Korean Kimchi Activate the Vitamin D Receptor-autophagy Signaling Pathways. Inflamm Bowel Dis. 2020;26:1199–211.
Han DH, Kim WK, Lee C, Park S, Lee K, Jang SJ, et al. Co-administration of Lactobacillus gasseri KBL697 and tumor necrosis factor-alpha inhibitor infliximab improves colitis in mice. Sci Rep. 2022;12:9640.
Radhakrishnan ST, Alexander JL, Mullish BH, Gallagher KI, Powell N, Hicks LC, et al. Systematic review: the association between the gut microbiota and medical therapies in inflammatory bowel disease. Aliment Pharm Ther. 2022;55:26–48.
Bornholdt J, Broholm C, Chen Y, Rago A, Sloth S, Hendel J, et al. Personalized B cell response to the Lactobacillus rhamnosus GG probiotic in healthy human subjects: a randomized trial. Gut Microbes. 2020;12:1–14.
Ma C, Wasti S, Huang S, Zhang Z, Mishra R, Jiang S, et al. The gut microbiome stability is altered by probiotic ingestion and improved by the continuous supplementation of galactooligosaccharide. Gut Microbes. 2020;12:1785252.
Yao M, Lu Y, Zhang T, Xie J, Han S, Zhang S, et al. Improved functionality of Ligilactobacillus salivarius Li01 in alleviating colonic inflammation by layer-by-layer microencapsulation. NPJ Biofilms Microbiomes. 2021;7:58.
Liu H, Cai Z, Wang F, Hong L, Deng L, Zhong J, et al. Colon-targeted adhesive hydrogel microsphere for regulation of gut immunity and flora. Adv Sci (Weinh). 2021;8:e2101619.
Funding
This work was supported by the [National Natural Science Foundation of China], [8197032978].
Author information
Authors and Affiliations
Contributions
Guarantor of the article: QY. QY designed and oversaw the review. CL constructed the figures and tables and wrote the manuscript. KP, SX, and YL revised the manuscript. All authors approved the final manuscript and agreed to be responsible for this review.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, C., Peng, K., Xiao, S. et al. The role of Lactobacillus in inflammatory bowel disease: from actualities to prospects. Cell Death Discov. 9, 361 (2023). https://doi.org/10.1038/s41420-023-01666-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41420-023-01666-w