Abstract
Background
Air pollution is a cause of lung cancer and is associated with bladder cancer. However, the relationship between air pollution and these cancers in regions of low pollution is unclear. We investigated associations between fine particulate matter (PM2.5), nitrogen dioxide, and black carbon (BC), and both these cancers in a low-pollution city.
Methods
A cohort of 11,679 men ≥65 years old in Perth (Western Australia) were followed from 1996–1999 until 2018. Pollutant concentrations, as a time-varying variable, were estimated at participants’ residential addresses using land use regression models. Incident lung and bladder cancer were identified through the Western Australian Cancer Registry. Risks were estimated using Cox proportional-hazard models (age as the timescale), adjusting for smoking, socioeconomic status, and co-pollutants.
Results
Lung cancer was associated with PM2.5 and BC in the adjusted single-pollutant models. A weak positive association was observed between ambient air pollution and squamous cell lung carcinoma but not lung adenocarcinoma. Positive associations were observed with bladder cancer, although these were not statistically significant. Associations were attenuated in two-pollutant models.
Conclusion
Low-level ambient air pollution is associated with lung, and possibly bladder, cancer among older men, suggesting there is no known safe level for air pollution as a carcinogen.

Similar content being viewed by others
Background
Lung and bladder cancers are significant causes of mortality and morbidity in Australia and worldwide [1,2,3]. Ambient air pollution is a known lung carcinogen and possible bladder carcinogen, but the risk in regions with low pollution is unclear.
Ambient air pollution and lung cancer
Lung cancer is the fifth highest cancer diagnosis and a leading cause of cancer-attributable mortality in Australia [2]. Whilst tobacco smoking remains the strongest known risk factor for lung cancer, international studies have observed that the proportion of non-smoking-related lung cancers is increasing [4,5,6,7]. Ambient air pollution may be contributing to this increase [8, 9]. In 2013, ambient air pollution and particulate matter, independently, were classified as Group 1 carcinogens for lung cancer by the International Agency for Research on Cancer (IARC) [10]. The relationship has been confirmed in further meta-analyses [11,12,13]. Some studies have observed increased lung cancer risks in regions where pollution concentrations were below the region-specific air quality guidelines, and suggested that even low concentrations of air pollution increase the risk of lung cancer [14,15,16,17,18,19]. However, other studies in low-pollution regions have not shown an increased risk [20,21,22].
The association between other pollutants and lung cancer is less clear. Significant associations between nitrogen dioxide (NO2) and lung cancer have been identified in regions in Europe [23,24,25], and North America [16, 19, 26], but the data are not consistent [14, 27, 28]. No associations were observed for studies conducted in China [29], Korea [30, 31], and Iran [32]. Studies between black carbon (BC) and lung cancer have also produced inconsistent results [14, 23, 25, 33].
Some studies have investigated associations between pollutants and histological lung cancer subtypes, such as adenocarcinoma and squamous cell carcinoma (SCC), but these are conflicting [14, 18, 23]. Significant associations were observed between (fine particulate matter (PM2.5) and adenocarcinoma, but not other subtypes [14, 18]; however, further studies are required [12, 34]. No association was observed between NO2 and SCC or adenocarcinoma [14, 30], while studies investigating other air pollutants and different histological subtypes of lung cancer have also found that there were no significant associations [14, 23].
Ambient air pollution and bladder cancer
Bladder cancer accounts for approximately 2.0% of all new cancer diagnoses in Australia [3]. In 2013, the IARC concluded that there was a possible association between air pollution and bladder cancer, but epidemiological evidence was limited [10]. Associations between PM2.5 and bladder cancer have been observed [20, 27, 35,36,37], but most of these were not statistically significant. No association between PM2.5 and bladder cancer was reported in a pooled cohort study in Europe [38]. Studies investigating associations between NO2 or BC and bladder cancer are scarce. No associations between NO2 and bladder cancer were observed in studies conducted in Europe [36, 37] and the United State of America (USA) [27]. Similarly, no association between BC and bladder cancer was observed in recent studies in Europe [36, 38].
The evidence that a broad range of adverse health effects occurring in regions of low concentrations of pollution is increasing, which resulted in the World Health Organization (WHO) lowering their targets for several air pollutants in the 2021 publication of The WHO Air Quality Guidelines [9]. However, the cancer risks of low-pollution exposure remain unclear. Ambient air pollution in Australian metropolitan cities is generally low [39] and, therefore, conducting studies in Australia provides an opportunity to study cancer incidence in a low-pollution region.
Our primary aims were to investigate whether exposures to low concentrations of air pollutants, specifically PM2.5, NO2, and BC, were associated with an increased risk of lung and bladder cancer incidence in older men (≥65 years). Our secondary aim was to investigate if exposures to these pollutants were associated with histological subtypes of lung cancer, specifically adenocarcinoma and SCC.
Methods
Study design and participants
Participants were members of an ongoing cohort study, the Health In Men Study (HIMS) [40]. The HIMS recruited 12,203 men aged between 65 and 84 years old, living in metropolitan Perth, the capital city of Western Australia (WA), from April 1996 to January 1999 [40]. The men were recruited from the Australian electoral roll; voting is compulsory in Australia and all Australian citizens ≥18 years are required to register on the electoral roll. The HIMS have been followed since 1996, both actively (questionnaires and health assessments) and passively (via the WA Data Linkage Systems (WADLS)) [40]. Using the WADLS, the cohort is linked to several health data collections including the WA Cancer Registry and Mortality Register. Written consent was obtained by all participants, and ethics approval was granted by the Department of Health WA Human Research Ethics Committee, and the University of WA Human Research Ethics Committee.
Assessment of exposure
We estimated concentrations of PM2.5, NO2 and BC at each participants’ household address at recruitment using validated Land Use Regression (LUR) models, which are described in detail elsewhere [41, 42]. The development of LUR models followed the protocols of the ESCAPE study [43]. Extensive seasonal air monitoring of PM2.5, NO2 and BC across the Perth Metropolitan area was conducted in 2012, through a purpose-designed air monitoring campaign. The LUR models were developed to predict the measured concentrations of PM2.5, NO2 and BC from environmental predictor variables, including road traffic type and volume, open green spaces, land use, buildings, population density, as well as water bodies [42]. The LUR models were in turn used to predict the air pollution concentrations at each participants’ household recruitment address.
Concentrations of PM2.5 and NO2 from 1995 to 2011 were estimated through back-extrapolation, based on the 2012 LUR model and the fixed air monitoring sites in Perth Metropolitan region, maintained by the WA Department of Water and Environmental Regulation. Exposure estimates from 2013 to 2019 were calculated using a similar method but with forward-extrapolation from the LUR model. Extrapolation of LUR models to predict pollutant concentrations up to 17 years earlier and 5–10 years later has been used and validated in other studies [44,45,46]. Concentrations were obtained for each pollutant at each participants’ address for each year of the study.
Although PM2.5 and NO2 measures were available from fixed monitoring sites, BC was not directly measured and available. To obtain BC estimates for extrapolation, temporal NO2 concentration ratios were used as a proxy for temporal changes to BC, as the concentration of BC and NO2 were correlated (r = 0.7). The method to obtain these is described elsewhere [42].
For the analyses, exposures to PM2.5, NO2 and BC were considered in a continuous, time-varying manner, where the average annual pollutant concentration was allowed to vary for each year of follow-up, i.e., a one-yearly moving average, from the year of recruitment to either the outcome of interest, death, or the end of follow-up, whichever occurred first.
Assessment of outcome
Incident lung and bladder cancer cases diagnosed between 1996 and December 2018 were ascertained by data linkage to the WA Cancer Registry, which records all cases of cancer in WA (see Supplementary Methods) [47]. The respective International Classification of Diseases for Oncology, third edition (ICD-O-3) topography codes were C34.0–34.9 for malignant lung cancer, and C67.0–67.9 for malignant bladder cancer. For those with multiple lung or bladder cancers, only the first malignant cancer was included in their respective cohorts. Participants with a diagnosis of lung and bladder cancer prior to recruitment were excluded from these analyses. We also excluded metastatic lung and bladder cancer. Participants with other cancer types were included in the study.
Two histological subtypes of lung cancer were investigated, categorised by ICD-O-3 histology codes. These were: SCC (8051–8084) and adenocarcinoma (8140–8149, 8160–8162, 8190–8221, 8260–8337, 8350–8351, 8570–8576, 8940–8941). These subtypes accounted for 50% of all lung cancers observed. Other histological groups of lung cancer (including basal cell carcinoma, other specific carcinomas, unspecified carcinomas and sarcomas and soft tissue tumours) were not studied separately, as there were too few events.
Other variables
Data were collected at recruitment using questionnaires and health assessments, and the following baseline data were considered for analyses: age, height and weight, socioeconomic status (SES) and the self-reported variables: country of birth, smoking status, alcohol consumption, physical activity [40]. The SES was based on residential postcodes and determined through the Socio-Economic Indices For Areas, an index which was developed by the Australian Bureau of Statistics [48]. To determine which potentially confounding variables to adjust for, we developed Direct Acyclic Graphs (DAGs) on variables based upon the literature [14, 40], and used the online platform http://www.dagitty.net/ (DAGitty version 3.0, Nijmegen, NL). These are described in Supplementary Figs. S1 and S2. For lung cancer, the minimal adjustment set was participant age and SES, and for bladder cancer, the minimal adjustment set was age, SES and smoking status. Smoking status was also included in the analysis for lung cancer, as it is the strongest known risk factor for lung cancer [2]. Details of these covariates are presented in the Supplementary Methods.
Statistical methods and data analyses
Of the 12,203 participants in the original HIMS, because our air pollution estimates were restricted to the Perth Metropolitan Area, 476 men were excluded for this reason (Supplementary Fig. S3). A further 48 participants were excluded due to missing data on smoking status (n = 43) and SES (n = 5), leaving 11,679 study participants. For the lung cancer analyses, we excluded participants with lung cancer diagnosed prior to HIMS recruitment (n = 62), leaving 11,617 participants for this analysis. Similarly, for bladder cancer, participants with previous diagnoses (n = 52) were excluded, leaving 11,627 participants for the bladder cancer analysis.
Cox proportional hazards regression analyses, with age as the timescale, were used to model the association of pollutant concentrations, on both lung and bladder cancer incidence. Separate models were performed for lung and bladder cancers, and the event of interest was the time of the first primary cancer of interest. For each respective cancer analysis, participants without the event were censored at either their date of death or at the end of the follow-up period of 31 December 2018, whichever occurred first. Mortality data were available from the WA mortality register. Both lung and bladder cancer models were adjusted for baseline area-level SES and smoking status. As there is evidence that smoking may be an effect modifier in the relationship between air pollution and lung cancer [14, 15, 22, 35], we also ran models stratifying by smoking status. In these stratified models, we provide estimates of the relationships between each pollutant and cancer outcome for each smoking status strata.
Two-pollutant models were developed for PM2.5, NO2 and BC. That is, for each pollutant (PM2.5, NO2 or BC), we also adjusted for each of the other two pollutants, in separate models. All two-pollutant models were also adjusted for baseline SES and smoking status.
The proportional hazards assumption was assessed using plots of Schoenfeld residuals, and no violations were detected. To allow for non-linearity in the relationship between each pollutant and each cancer outcome, we considered models where each pollutant was entered as a restricted cubic spline with three knots. Knot locations were determined by the recommendations in Harrell [49]. When modelling non-linear relationships, it is not appropriate to present a single hazard ratio (HR), as the HR is not constrained to be constant across the exposure range as seen when modelling a linear relationship. As we have modelled the relationship between air pollutants and incident cancers non-linearly, we report HRs and 95% confidence intervals (95% CIs) for multiple pollutant concentrations occurring within the concentration range observed in our study, when compared with a reference, also within our study range. This helps to describe how the relationship may change over the range of pollutant concentrations. Specifically, PM2.5 concentrations of 3, 5, and 7 µg/m3 are compared with a reference value of 1 µg/m3, NO2 concentrations of 10, 15, and 25 µg/m3 are compared with a reference value of 5 µg/m3, and BC concentrations of 0.8 × 10−5, 1.2 × 10−5, and 1.6 × 10−5 m−1 are compared with a reference value of 0.5 × 10−5 m−1.
Five sets of sensitivity analyses were conducted. The first was assigning a baseline pollutant exposure to all participants. This was the average concentration of each pollutant during the participant’s recruitment year. Current studies have used baseline concentrations to estimate participant exposures to ambient air pollutants [14, 38, 43]. This analysis would enable us to compare our findings with other studies that have used similar exposure measures, as well as with comparing with the use of time-varying measures in our study.
When using age as the timescale, comparisons are made between participants at specific ages, as opposed to specific calendar years of exposure. As such, we conducted a sensitivity analysis which included an interaction between birth cohort (birth years 1914–1924 and 1925–1932) and each air pollutant to see whether the impact of air pollution on lung and bladder cancer differed for those born at different times.
The third set of sensitivity analyses excluded participants who had a lung or bladder cancer diagnosis in the first two years of follow-up, in addition to those who were excluded due to diagnoses prior to recruitment. This factored in lung or bladder cancer cases at baseline that may have had delayed diagnosis or registration to the WA Cancer Registry.
Exposure estimates were based on residential addresses at the time of recruitment, thus assuming that all participants had lived at the same residential address the whole time, and as such, a fourth set of analyses was done to exclude participants who had moved addresses (‘movers’) during the follow-up period. Participants who had moved addresses from the baseline during the study were recorded in the HIMS dataset.
Finally, we also included all available covariates from the DAGs in the primary analyses to assess the robustness of our models.
All analyses were performed using Stata software package 17.0 (StataCorp, College Station, TX).
Results
Study population characteristics
Baseline demographic and lifestyle characteristics of the study participants are presented in Table 1. The mean age at baseline was 72.1 (SD ± 4.4) years old. Most participants had high area-level SES (64%) and were former smokers (59.6%). Most of the former smokers had quit more than 10 years prior to recruitment.
Air pollutant concentrations of study population
Average concentrations in the starting year of the study (1996) were: 5.65 µg/m3 for PM2.5, 15.83 µg/m3 for NO2, and 1.06 × 10−5 m−1 for BC. Average concentrations at the end of the study (2018) were: 4.35 µg/m3 for PM2.5, 11.20 µg/m3 for NO2, and 0.81 × 10−5 m−1 for BC. Further distributional information is described in Supplementary Table S1. Pairwise correlations between the three pollutants at recruitment all had Spearman’s rho (r) <0.7 (Supplementary Table S2). Participants with cancer events had slightly higher mean concentrations of PM2.5, NO2 and BC, compared to those who did not have the respective cancer event at recruitment (Table 2).
Associations between ambient air pollutants and lung cancer
There were 692 (6.0%) lung cancer events identified during the study period, with a total follow-up time of 158,479 person-years.
Positive associations between the pollutants and lung cancer were observed in both crude and adjusted models (Table 3). In the adjusted single-pollutant model, HRs for PM2.5 and BC, but not NO2, were mostly statistically significant. In the two-pollutant models, the results for PM2.5 were attenuated, and lost statistical significance, when controlling, separately, for NO2 and BC. The results for BC were attenuated when controlling for PM2.5 but not for NO2, but stayed statistically significant.
Ambient air pollution and lung cancer histological subtypes
In the lung cancer cohort, there were 138 (1.2%) SCCs and 201 (1.7%) adenocarcinomas of the lung reported during follow-up (Table 4). Concentrations of PM2.5 and BC of participants were positively associated with both SCC and adenocarcinoma, across the unadjusted and adjusted single-pollutant models, although these were not significant. The HRs in the respective two-pollutant models were further attenuated, except for BC when controlled for NO2. Concentrations of NO2 were positively associated with SCC, but not ADC in the single-pollutant models. No associations between incident lung cancer and NO2 were observed across all two-pollutant models.
Associations between ambient air pollutants and bladder cancer
There were 224 incident bladder cancer events (1.9%), during 158,440 person-years of follow-up. Concentrations of PM2.5 and BC were positively associated with bladder cancer in their respective single and two-pollutant models, although these were not statistically significant (Table 3). A weak positive association was observed between NO2 and bladder cancer in single-pollutant models; however, this was attenuated when adjusted for other co-pollutants.
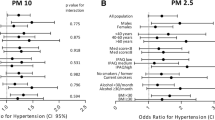
We observed evidence of a non-linear relationship between pollutants and both lung and bladder cancer (Fig. 1).
Graphs showing 3-knot restricted cubic spline regression demonstrating non-linear associations between ambient air pollutants and incident lung cancer, bladder cancer, and histological subtypes of lung cancer (adenocarcinoma and squamous cell carcinoma), in the HIMS cohort for the single-pollutant unadjusted models. i) Lung cancer: PM2.5. ii) Lung cancer: NO2. iii) Lung cancer: BC. iv) Bladder cancer: PM2.5. v) Bladder cancer: NO2. vi) Bladder cancer: BC. vii) ADC: PM2.5. viii) ADC: NO2. ix) ADC: BC. x) SCC: PM2.5. xi) SCC: NO2. xii) SCC: BC.
Stratification by smoking status
When stratified by smoking status, positive associations were observed between all pollutants and lung cancer for the former smokers’ group who had quit smoking ≥10 years ago in the single-pollutant models, but not consistently in other smoking groups (Supplementary Table S3). Bladder cancer estimates were relatively consistent across the different smoking cohorts.
Sensitivity analyses
Baseline pollutant exposure
For lung cancer, the HRs associated with baseline concentrations of PM2.5 and BC remained mostly significant in the crude and adjusted single-pollutant models (Supplementary Table S4). A positive, but non-significant, association was observed between incident lung cancer and NO2 in the single-pollutant models. Positive associations between baseline exposures of PM2.5 and BC and incident bladder cancer were also observed, but not with NO2. In the lung cancer histological subtype analysis, the incidence of SCC was positively associated with baseline concentrations of all pollutants in the crude and adjusted single-pollutant models; however, the confidence intervals were very wide (Supplementary Table S5). Positive associations were also observed between incident lung adenocarcinoma with PM2.5 and BC, but not with NO2. Evidence of a non-linear relationship was observed between ambient air pollutants, and both lung and bladder cancer (Supplementary Fig. S4).
Birth cohort
For both lung and bladder cancer analyses, no significant interactions were observed between ambient air pollutants and the birth cohorts (all p values > 0.09).
Two-year cancer exclusion
The overall findings were similar when participants with incident lung or bladder cancer in the first 2 years of follow-up were excluded (Supplementary Table S6).
Excluding movers
The associations between PM2.5, NO2 and BC and both lung and bladder cancer remained similar after excluding participants who had moved residential addresses during the follow-up period (Supplementary Table S7).
Inclusion of all covariates in the primary analyses
We also did not observe significant changes in associations when other available covariates were added to the models (Supplementary Table S8).
Discussion
We observed positive associations between follow-up exposures to PM2.5, NO2 and BC, and both incident lung and bladder cancer. The concentrations of PM2.5 and NO2 in this study were low and, on average, below Australian air quality standards (current annual average thresholds are 8 µg/m3 and 15 ppb (≈28 µg/m3), respectively [39]), and lower than has been reported in other ‘low-pollution’ studies [14,15,16,17,18,19, 35, 36].
The range of exposure concentrations for each pollutant reported in our study was narrow. The annual average concentrations (and range) during follow-up for: PM2.5 was 4.63 µg/m3 (0.01–9.20 µg/m3), NO2 was 13.59 µg/m3 (0.82–29.02 µg/m3), and BC was 0.98 × 0.5 × 10−5 m−1 (0.08–2.03 × 10−5 m−1). Our findings support the notion that there may not be a threshold concentration for the carcinogenic effects of ambient air pollution.
Lung cancer and PM2.5
The associations between PM2.5 and lung cancer were consistent with recent studies conducted in the USA [15, 35], Canada [17,18,19], and Europe [14, 50], where an increase in lung cancer risk was observed with relatively low concentrations of PM2.5 exposures. For example, the ELAPSE study [14], a pooled cohort of seven countries in Europe, reported a median annual concentration of 15.4 µg/m3, and a pooled-HR of 1.13 (95% CI: 1.05–1.23) per 5 µg/m3 increase in PM2.5. Studies in Canada with lower exposure concentrations reported HRs of 1.02 (95% CI: 1.01–1.05) per 5.3 µg/m3 [19], 1.16 (95% CI: 1.07–1.25) per 10 µg/m3 [17], and 1.34 (95% CI: 1.10–1.65) per 10 µg/m3 [18], where average respective PM2.5 concentrations were 7.68 µg/m3 (mean), 7.4 µg/m3 (mean), and 9.1 µg/m3 (median). On the other hand, the Biobank study [50] in the United Kingdom (UK) reported a high HR of 1.63 (95% CI: 1.33–2.01) per 5 µg/m3 increase in PM2.5 with mean PM2.5 concentration of 10 µg/m3. Recent studies (with a wider exposure range) have suggested that the relative risk of lung cancer (with each incremental increase in pollutant) may be greater at lower concentrations of PM2.5, compared to higher concentrations [14, 17, 19]. Because of the narrow exposure range in our study, we could not investigate this further.
Lung cancer and NO2 and BC
The association between ambient NO2 and lung cancer has regularly been observed [16, 19, 23,24,25,26, 29,30,31,32, 50, 51], although not in all studies [27, 28]. In regions with low NO2, significant associations with lung cancer have been found in studies conducted in the Netherlands [23,24,25], the UK [50], the USA [26], and Canada [16, 19]. The average concentrations of NO2 reported in these studies were below European Air Quality Standards of <40 µg/m3 [52]. In our study, the NO2 concentrations were below the Australian standard of 28 µg/m3. We observed non-significant associations between NO2 and lung cancer, which was a similar finding to a pooled analysis of European cohorts in relatively low-pollution areas (HR = 1.02, 95% CI = 0.97–1.07) [14].
We observed significant associations between BC and lung cancer in all models. There is currently a paucity of studies on BC and lung cancer. We identified three studies and one pooled analysis that investigated associations between BC and lung cancer [14, 23, 25, 33]. Two studies found significant associations with lung cancer; [23, 25] the multi-centre European ELAPSE Study did not find an association between lung cancer and BC [14], and the French Gazel Cohort Study [33] reported non-statistically significant associations between lung cancer and BC. Given the limited studies, further research is needed to better understand potential associations.
In 2012, the IARC declared diesel engine exhaust as a Group 1 human carcinogen [53]. Ambient BC is a common proxy for diesel [54] and, therefore, our findings may reflect the association between diesel engine exhaust and lung cancer. In Australia, the proportion of cars that are diesel powered is growing steadily and accounts for over 26% of all motor vehicles in this country [55]. Despite efforts to reduce total emissions in ambient air, there is a growing trend towards driving diesel-powered sports utility and utility vehicles, leading to greater production of tail-pipe pollutants [56].
Whilst positive associations were observed between both NO2 and BC and lung cancer, when analysed together, a positive, but non-significant association, with lung cancer remained with BC but not with NO2. This suggests that the association of NO2 with lung cancer is in part reflecting the effects of BC. The HRs were stronger when NO2 was included in the model with BC, suggesting there may be additive effects. As both NO2 and BC are produced from traffic-related pollution, they are often present together [33].
Air pollutants and lung cancer histological subtypes
The relationship between histological subtypes of lung cancer and ambient air pollution remains unclear. Positive associations were observed between BC and both SCC and adenocarcinoma, across both single and two-pollutant models. Positive, but non-significant, associations were also observed for PM2.5 and both histological lung cancer subtypes in the single-pollutant models. The effects were attenuated in the two-pollutant models, particularly for lung adenocarcinoma. Concentrations of NO2 were positively associated with increasing risk of SCC; however, effects were also attenuated after controlling for other pollutants. No associations were observed for NO2 with adenocarcinoma.
Our findings contrast the results from previous studies, where stronger associations between PM2.5 and adenocarcinoma have been observed, compared with other lung cancer subtypes [18, 43]. The ELAPSE study also observed associations between PM2.5 and adenocarcinoma, but not with SCC [14]. However, no associations were observed between NO2 or BC, with either adenocarcinoma and SCC [14]. Hart et al. [23]. also reported no associations for between different histological subtypes of lung cancer, and either NO2 or black smoke. These studies used single-pollutant models and did not adjust for co-pollutants. The risk of incident SCC (and not adenocarcinoma) was not found to be associated with PM2.5, NO2 and BC in previous studies.
Bladder cancer and PM2.5, NO2 and BC
There was a positive association between PM2.5 and bladder cancer, although this was not statistically significant. This is consistent with the multi-centre European study, the ELAPSE Study [36], where a positive but non-significant association was identified. Positive associations between ambient air pollution and bladder cancer were also described in the report by IARC in 2013 [10] and in a more recent study in the USA [27]. However, no associations were observed for other studies conducted in Spain [37], the USA [35], and another pooled multi-cohort study in Europe [38].
Exposures to NO2 were not associated with bladder cancer, which is consistent with existing literature. No associations with bladder cancer were reported in studies in Spain [37], the USA [27], and a multi-centre European study [38]. However, a positive, albeit non-significant, association was observed with BC across all pollutant models. This differed from the ELAPSE Study [36], where no association between BC and bladder cancer was reported. We observed that NO2 and BC were not independent of each other, and the presence of both in the co-pollutant analysis resulted in attenuation of their respective effects on bladder cancer.
Baseline pollutant exposures
Associations using baseline exposures for ambient air pollutants were similar to the time-varying exposures, for both lung and bladder cancer analyses. The pattern of associations between baseline concentrations of PM2.5, NO2 and BC and both respective cancers remained consistent in the sensitivity analyses (Supplementary Tables S4 and S5). The use of pollutant exposures estimated at residential home addresses at the time of recruitment as a measure of long-term pollutant exposure is a common method used in the literature to examine risk of chronic health effects [14, 38, 43]. However, assigning time-varying exposures provides a more precise assignment and enables a greater detection in the effect measure, which may be more important in low-level air pollution studies. A Canadian study investigating low-level ambient air pollution and mortality also observed differences in these effect measures, and suggested that time-varying estimates for these studies are important, particularly for pollutants with high spatial resolution [16]. However, the ELAPSE Study observed minimal difference in effect measures with different exposure metrics including baseline, annual average, and time-varying concentrations in their sensitivity analyses [14].
Stratified by smoking status
We observed modest effect modification by smoking status in the lung cancer analysis, and this has also been observed in the literature [14, 15, 22, 35]. Positive associations between lung cancer and ambient air pollutants were observed in the group that had quit smoking ≥10 years ago, but not the never-smoker group. Positive associations have been observed in studies between lung cancer and PM2.5 in never-smokers [14, 15]. Another study observed positive associations when analysis was restricted to participants who had never smoked, or had quit ≥10 years ago [22]. A recent meta-analysis also found a higher risk of lung cancer with PM2.5 in never and former smokers, compared to current smokers; however, the results were imprecise [12]. Another study found PM2.5-associated lung cancer mortality was higher in the never-smokers cohort (HR = 1.73, 95% CI = 1.20–2.49) compared to the full cohort (HR = 1.13, 95% CI = 1.00–1.26) [35].
Smoking status did not modify the effect of ambient air pollutants and bladder cancer in our study. Our findings were similar to other studies, where a non-significant interaction between smoking status [36] and pack-years smoked [37] was observed with ambient air pollutants.
Strengths and limitations
Our study had several strengths. The follow-up time of 22 years was suitable for lung and bladder cancer, which both have long latency periods. Analysing data from an older-aged cohort is a consideration of a population particularly vulnerable to the health effects of hazardous air pollution. The HIMS is linked to the WADLS and follow-up data for all participants were available through data linkage, including to state hospital records and mortality registry. Reporting cancer diagnoses to the WA Cancer Registry is also a mandatory requirement for WA health practitioners [47]. The WADLS has stringent checking procedures, with low rates of errors in their datasets [57]. Tracking all participants reduced the potential for attrition bias that may occur from loss to follow-up.
The validated LUR models had good performance, and could explain variability in PM2.5, NO2 and BC concentrations in Perth by approximately 67%, 69% and 85%, respectively [41, 42]. However, whilst LUR models have been used and validated for back- and forward-extrapolation in previous studies, we did not have validation data to justify the extrapolation of our models for Perth (WA).
The HIMS cohort only included older, mainly Caucasian men, limiting generalisability. Many studies in the literature have used large-scale cohorts (such as populations across multiple countries and sites [14, 50]), and have drawn from national or state-wide administrative and health surveillance databases [17,18,19, 35]. These studies include both middle and older-aged adults, and both males and females, resulting in a greater heterogeneity of participants. Female-only studies have also been conducted, such as participants recruited from the Canadian National Breast Screening Study [18]. In contrast, the HIMS cohort was originally recruited for a randomised screening trial for Abdominal Aortic Aneurysms [40], and included older-aged men from a single city only.
Although we reported a large number of lung cancer events, the case counts for bladder cancer and histological subtypes of lung cancer were relatively fewer. This could limit the statistical power of these analyses. Whilst our sample size was relatively small compared to other studies, our cohort was a subset of the population most vulnerable to lung (and bladder) cancers. Evaluating lesser-known cancer risk factors such as air pollution was, therefore, suitable and relevant for our cohort.
Pollution estimates were from residential addresses and did not consider where they spent their time. Personal exposure to air pollution is dependent on the day-to-day microenvironments of the individual, which include both indoor and outdoor exposures at their home [58].
Other residual confounding for lung cancer risk may not have been considered. For example, the UK Biobank Study observed that genetic factors could increase the effect of ambient air pollution on lung cancer by 50% [50]. Genetic factor analyses were outside the study scope. Finally, confounding was determined at recruitment; hence, lifestyle changes (such as smoking status) during follow-up were not considered.
Conclusion
In conclusion, we found an increased risk of lung and possible increase of bladder cancer in a cohort of older men in Perth, WA, residing in areas where ambient air pollution concentrations are typically considered very low. This adds to the increasing evidence that negative health effects are being identified at low concentrations of air pollution. Further studies are needed to understand the carcinogenic potential of ambient air pollution at low concentrations.
Data availability
Data were obtained from the HIMS, and HIMAQs, and the WADLS. Access to these datasets requires approval from these groups.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. https://doi.org/10.3322/caac.21660.
Cancer Australia. Lung Cancer in Australia statistics. Strawberry Hills (NSW): Commonwealth of Australia; 2021 [revised October 20, 2020]. https://www.canceraustralia.gov.au/affected-cancer/cancer-types/lung-cancer/lung-cancer-australia-statistics. Accessed March 9, 2021.
Cancer Australia. Bladder cancer statistics in Australia. Strawberry Hills (NSW): Commonwealth of Australia; 2021 [revised October 20, 2020]. https://www.canceraustralia.gov.au/affected-cancer/cancer-types/bladder-cancer/bladder-cancer-statistics-australia. Accessed March 9, 2021.
Cufari ME, Proli C, De Sousa P, Raubenheimer H, Al Sahaf M, Chavan H, et al. Increasing frequency of non-smoking lung cancer: presentation of patients with early disease to a tertiary institution in the UK. Eur J Cancer. 2017;84:55–59. https://doi.org/10.1016/j.ejca.2017.06.031.
Bhopal A, Peake MD, Gilligan D, Cosford P. Lung cancer in never-smokers: a hidden disease. J R Soc Med. 2019;112:269–71. https://doi.org/10.1177/0141076819843654.
Pelosof L, Ahn C, Gao A, Horn L, Madrigales A, Cox J, et al. Proportion of never-smoker non-small cell lung cancer patients at three diverse institutions. J Natl Cancer Inst. 2017;109:295. https://doi.org/10.1093/jnci/djw295.
Toh C-K, Ong W-S, Lim W-T, Tan DS-W, Ng Q-S, Kanesvaran R, et al. A decade of never-smokers among lung cancer patients – increasing trend and improved survival. Clin Lung Cancer. 2018;19:e539–50. https://doi.org/10.1016/j.cllc.2018.03.013.
Australian Institute of Health and Welfare. Cancer series: Lung cancer in Australia – an overview. Canberra (ACT); 2011. p. 206 Report No.: CAN 58. https://www.aihw.gov.au/reports/cancer/lung-cancer-in-australia-overview/contents/table-of-contents.
World Health Organization. WHO global air quality guidelines: particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide. Geneva: World Health Organization; 2021. p. 273. https://apps.who.int/iris/handle/10665/345329.
Loomis D, Grosse Y, Lauby-Secretan B, El Ghissassi F, Bouvard V, Benbrahim-Tallaa L, et al. The carcinogenicity of outdoor air pollution. Lancet Oncol. 2013;14:1262–3. https://doi.org/10.1016/s1470-2045(13)70487-x.
Chen J, Hoek G. Long-term exposure to PM and all-cause and cause-specific mortality: a systematic review and meta-analysis. Environ Int. 2020;143:105974. https://doi.org/10.1016/j.envint.2020.105974.
Yu P, Guo S, Xu R, Ye T, Li S, Sim MR, et al. Cohort studies of long-term exposure to outdoor particulate matter and risks of cancer: a systematic review and meta-analysis. Innov J. 2021;2:100143. https://doi.org/10.1016/j.xinn.2021.100143.
Hamra GB, Laden F, Cohen AJ, Raaschou-Nielsen O, Brauer M, Loomis D. Lung cancer and exposure to nitrogen dioxide and traffic: a systematic review and meta-analysis. Environ Health Perspect. 2015;123:1107–12. https://doi.org/10.1289/ehp.1408882.
Hvidtfeldt UA, Severi G, Andersen ZJ, Atkinson R, Bauwelinck M, Bellander T, et al. Long-term low-level ambient air pollution exposure and risk of lung cancer – a pooled analysis of 7 European cohorts. Environ Int. 2021;146:106249. https://doi.org/10.1016/j.envint.2020.106249.
Gharibvand L, Shavlik D, Ghamsary M, Beeson WL, Soret S, Knutsen R, et al. The association between ambient fine particulate air pollution and lung cancer incidence: results from the AHSMOG-2 Study. Environ Health Perspect. 2017;125:378–84. https://doi.org/10.1289/EHP124.
Crouse DL, Peters PA, Hystad P, Brook JR, van Donkelaar A, Martin RV, et al. Ambient PM2.5, O3, and NO2 exposures and associations with mortality over 16 years of follow-up in the Canadian Census Health and Environment Cohort (CanCHEC). Environ Health Perspect. 2015;123:1180–6. https://doi.org/10.1289/ehp.1409276.
Pinault LL, Weichenthal S, Crouse DL, Brauer M, Erickson A, van Donkelaar A, et al. Associations between fine particulate matter and mortality in the 2001 Canadian Census Health and Environment Cohort. Environ Res. 2017;159:406–15. https://doi.org/10.1016/j.envres.2017.08.037.
Tomczak A, Miller AB, Weichenthal SA, To T, Wall C, van Donkelaar A, et al. Long-term exposure to fine particulate matter air pollution and the risk of lung cancer among participants of the Canadian National Breast Screening Study. Int J Cancer. 2016;139:1958–66. https://doi.org/10.1002/ijc.30255.
Bai L, Shin S, Burnett RT, Kwong JC, Hystad P, van Donkelaar A, et al. Exposure to ambient air pollution and the incidence of lung cancer and breast cancer in the Ontario Population Health and Environment Cohort. Int J Cancer. 2020;146:2450–9. https://doi.org/10.1002/ijc.32575.
Coleman Nathan C, Burnett Richard T, Ezzati M, Marshall Julian D, Robinson Allen L, Pope CA. Fine particulate matter exposure and cancer incidence: analysis of SEER Cancer Registry Data from 1992–2016. Environ Health Perspect. 2020;128:107004. https://doi.org/10.1289/EHP7246.
Wang B, Eum K-D, Kazemiparkouhi F, Li C, Manjourides J, Pavlu V, et al. The impact of long-term PM2.5 exposure on specific causes of death: exposure-response curves and effect modification among 53 million U.S. Medicare beneficiaries. Environ Health. 2020;19:20. https://doi.org/10.1186/s12940-020-00575-0.
Puett Robin C, Hart Jaime E, Yanosky Jeff D, Spiegelman D, Wang M, Fisher J, et al. Particulate matter air pollution exposure, distance to road, and incident lung cancer in the nurses’ health study cohort. Environ Health Perspect. 2014;122:926–32. https://doi.org/10.1289/ehp.1307490.
Hart J, Spiegelman D, Beelen R, Hoek G, Brunekreef B, Schouten L, et al. Long-term ambient residential traffic-related exposures and measurement error-adjusted risk of incident lung cancer in the Netherlands Cohort Study on Diet and Cancer. Environ Health Perspect. 2015;123:860–6. https://doi.org/10.1289/ehp.1408762.
Fischer PH, Marra M, Ameling CB, Hoek G, Beelen R, de Hoogh K, et al. Air pollution and mortality in seven million adults: The Dutch Environmental Longitudinal Study (DUELS). Environ Health Perspect. 2015;123:697–704. https://doi.org/10.1289/ehp.1408254.
Klompmaker JO, Janssen NAH, Bloemsma LD, Marra M, Lebret E, Gehring U, et al. Effects of exposure to surrounding green, air pollution and traffic noise with non-accidental and cause-specific mortality in the Dutch national cohort. Environ Health. 2021;20:82. https://doi.org/10.1186/s12940-021-00769-0.
Eum K-D, Honda TJ, Wang B, Kazemiparkouhi F, Manjourides J, Pun VC, et al. Long-term nitrogen dioxide exposure and cause-specific mortality in the U.S. Medicare population. Environ Res. 2022;207:112154. https://doi.org/10.1016/j.envres.2021.112154.
Turner MC, Krewski D, Diver WR, Pope CA III, Burnett RT, Jerrett M, et al. Ambient air pollution and cancer mortality in the Cancer Prevention Study II. Environ Health Perspect. 2017;125:087013. https://doi.org/10.1289/EHP1249.
Gowda SN, DeRoos AJ, Hunt RP, Gassett AJ, Mirabelli MC, Bird CE, et al. Ambient air pollution and lung cancer risk among never-smokers in the Women’s Health Initiative. Environ Epidemiol. 2019;3:e076. https://doi.org/10.1097/EE9.0000000000000076.
Chen X, Zhang L, Huang J, Song F, Zhang L, Qian Z, et al. Long-term exposure to urban air pollution and lung cancer mortality: a 12-year cohort study in Northern China. Sci Total Environ. 2016;571:855–61. https://doi.org/10.1016/j.scitotenv.2016.07.064.
Moon DH, Kwon SO, Kim S-Y, Kim WJ. Air pollution and incidence of lung cancer by histological type in Korean adults: a Korean National Health Insurance Service Health Examinee Cohort Study. Int J Environ Res Public Health. 2020;17:915. https://doi.org/10.3390/ijerph17030915.
Yang S, Kim OJ, Shin M, Kim WJ, Kim SY. Association between long-term exposure to high levels of ambient air pollution and incidence of lung cancer in a population-based cohort. Environ Res. 2021;198:111214. https://doi.org/10.1016/j.envres.2021.111214.
Khorrami Z, Pourkhosravani M, Rezapour M, Etemad K, Taghavi-Shahri SM, Kunzli N, et al. Multiple air pollutant exposure and lung cancer in Tehran, Iran. Sci Rep. 2021;11:9239. https://doi.org/10.1038/s41598-021-88643-4.
Lequy E, Siemiatycki J, de Hoogh K, Vienneau D, Dupuy J, Gares V, et al. Contribution of long-term exposure to outdoor black carbon to the carcinogenicity of air pollution: evidence regarding risk of cancer in the Gazel Cohort. Environ Health Perspect. 2021;129:037005. https://doi.org/10.1289/EHP8719.
Turner MC, Andersen ZJ, Baccarelli A, Diver WR, Gapstur SM, Pope CA III, et al. Outdoor air pollution and cancer: an overview of the current evidence and public health recommendations. CA Cancer J Clin. 2020;70:460–79. https://doi.org/10.3322/caac.21632.
Coleman NC, Burnett RT, Higbee JD, Lefler JS, Merrill RM, Ezzati M, et al. Cancer mortality risk, fine particulate air pollution, and smoking in a large, representative cohort of US adults. Cancer causes control. 2020;31:767–76. https://doi.org/10.1007/s10552-020-01317-w.
Chen J, Rodopoulou S, Strak M, de Hoogh K, Taj T, Poulsen AH, et al. Long-term exposure to ambient air pollution and bladder cancer incidence in a pooled European cohort: the ELAPSE project. Br J Cancer. 2022;126:1499–507. https://doi.org/10.1038/s41416-022-01735-4.
Turner MC, Gracia-Lavedan E, Cirac M, Castaño-Vinyals G, Malats N, Tardon A, et al. Ambient air pollution and incident bladder cancer risk: updated analysis of the Spanish Bladder Cancer Study. Int J Cancer. 2019;145:894–900. https://doi.org/10.1002/ijc.32136.
Pedersen M, Stafoggia M, Weinmayr G, Andersen ZJ, Galassi C, Sommar J, et al. Is there an association between ambient air pollution and bladder cancer incidence? Analysis of 15 European cohorts. Eur Urol Focus. 2018;4:113–20. https://doi.org/10.1016/j.euf.2016.11.008.
Department of Agriculture, Water and the Environment. National Environment Protection (Ambient Air Quality) Measure. Canberra (ACT): Commonwealth of Australia; c2021. https://www.awe.gov.au/environment/protection/air-quality/ambient-air-quality-nepm.
Norman PE, Flicker L, Almeida OP, Hankey GJ, Hyde Z, Jamrozik K, et al. Cohort profile: The Health In Men Study (HIMS). Int J Epidemiol. 2008;38:48–52. https://doi.org/10.1093/ije/dyn041.
Dirgawati M, Barnes R, Wheeler AJ, Arnold A, McCaul KA, Stuart AL, et al. Development of Land Use Regression models for predicting exposure to NO2 and NOx in Metropolitan Perth, Western Australia. Environ Model Softw. 2015;74:258–67. https://doi.org/10.1016/j.envsoft.2015.07.008.
Dirgawati M, Heyworth JS, Wheeler AJ, McCaul KA, Blake D, Boeyen J, et al. Development of Land Use Regression models for particulate matter and associated components in a low air pollutant concentration airshed. Atmos Environ. 2016;144:69–78. https://doi.org/10.1016/j.atmosenv.2016.08.013.
Raaschou-Nielsen O, Andersen ZJ, Beelen R, Samoli E, Stafoggia M, Weinmayr G. et al. Air pollution and lung cancer incidence in 17 European cohorts: prospective analyses from the European Study of Cohorts for Air Pollution Effects (ESCAPE). Lancet Oncol. 2013;14:813–22. https://doi.org/10.1016/S1470-2045(13)70279-1.
Cesaroni G, Badaloni C, Gariazzo C, Stafoggia M, Sozzi R, Davoli M, et al. Long-term exposure to urban air pollution and mortality in a cohort of more than a million adults in Rome. Environ Health Perspect. 2013;121:324–31. https://doi.org/10.1289/ehp.1205862.
Vizcaino P, Lavalle C. Development of European NO2 Land Use Regression Model for present and future exposure assessment: implications for policy analysis. Environ Pollut. 2018;240:140–54. https://doi.org/10.1016/j.envpol.2018.03.075.
Gulliver J, de Hoogh K, Hansell A, Vienneau D, et al. Development and back-extrapolation of NO2 land use regression models for historic exposure assessment in Great Britain. Environ Sci Technol. 2013;47:7804–11. https://doi.org/10.1021/es4008849.
Health (Western Australian Cancer Register) Regulations 2011 (WA). https://www.legislation.wa.gov.au/legislation/statutes.nsf/main_mrtitle_12239_homepage.html.
Australian Bureau of Statistics. Technical paper: Socio-Economic Indexes for Areas (SEIFA) 2016. Canberra (ACT): Commonwealth of Australia; 2016. https://www.abs.gov.au/ausstats/abs@.nsf/PrimaryMainFeatures/4364.0.55.001.
Harrell FE. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. New York: Springer; 2001.
Huang Y, Zhu M, Ji M, Fan J, Xie J, Wei X, et al. Air pollution, genetic factors, and the risk of lung cancer: a prospective study in the UK Biobank. Am J Respir Crit Care Med. 2021;204:817–25. https://doi.org/10.1164/rccm.202011-4063OC.
Lamichhane DK, Kim HC, Choi CM, Shin MH, Shim YM, Leem JH, et al. Lung cancer risk and residential exposure to air pollution: a Korean population-based case-control study. Yonsei Med J. 2017;58:1111–8. https://doi.org/10.3349/ymj.2017.58.6.1111.
Ortiz AG, Guerreiro C, Soares J Air Quality in Europe – 2020 Report. Luxembourg: European Environment Agency; 2020. p. 164. Report No.: 09/2020. https://www.eea.europa.eu/publications/air-quality-in-europe-2020-report.
International Agency for Research on Cancer. IARC: Diesel Engine Exhaust Carcinogenic. Lyon: World Health Organization; 2012. p. 4. Report No.: 213. https://www.iarc.who.int/wp-content/uploads/2018/07/pr213_E.pdf.
Janssen NA, Gerlofs-Nijland ME, Lanki T, Salonen RO, Cassee F, Hoek G, et al. Health effects of black carbon. Copenhagen: World Health Organization; 2012. p. 96. https://www.euro.who.int/__data/assets/pdf_file/0004/162535/e96541.pdf.
Australian Bureau of Statistics. Motor Vehicle Census, Australia. Canberra (ACT): Commonwealth of Australia; 2021. https://www.abs.gov.au/statistics/industry/tourism-and-transport/motor-vehicle-census-australia/31-jan-2021.
Terrill M, Buffurd I, Fox L. The Grattan car plan: practical policies for cleaner transport and better cities. Melbourne (VIC): Grattan Institute; 2021. p. 78. Report No.: 2021-14. https://grattan.edu.au/report/grattan-car-plan/.
Eitelhuber T. Data linkage – making the right connections. East Perth (WA): Western Australia Department of Health; 2016. p. 3. https://www.datalinkage-wa.org.au/wp-content/uploads/2019/02/Data-Linkage-Branch-Linkage-Quality.pdf. Accessed March 15, 2021.
Dias D, Tchepel O. Spatial and temporal dynamics in air pollution exposure assessment. Int J Environ Res Public Health. 2018;15:558. https://doi.org/10.3390/ijerph15030558.
Acknowledgements
We would like to thank all participants and staff of the Health In Men Study (HIMS). We would also like to acknowledge the Western Australian Data Linkage System (WADLS) for the provision of data relevant to this study, and the Western Australia Department of Water and Environment Regulation for providing air pollution data from 1995 to 2019.
Funding
The HIMS and The HIMAQs are funded by competitive project grants from the National Health and Medical Research Council of Australia (NHMRC grant: 1128083 and 1003589, respectively). LF is supported by a Medical Research Future Fund Next Generation Clinical Researchers Practitioner Fellowship (1155669). JG is funded by an NHMRC Practitioner Fellowship (1117061) and Queensland Government Senior Clinical Research Fellowship. The funding sources had no role in the study design, data collection and analysis, nor any input in the preparation of the manuscript. Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
EHL, PF, MLT and JH conceptualised and designed the work, interpreted the data and performed data analysis. JH, MN, BBY, OPA, GJH, JG, CE, LF and SR contributed to data collection, study design and obtained funding. EHL prepared the first draft of the manuscript. PF, MLT and JH supervised this work. MN, BBY, OPA, GJH, JG, CE, LF and SR revised the manuscript. All authors reviewed the manuscript for important intellectual content, and approved the final version for publication.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Written information and consent forms were provided to all study participants at the time of recruitment, and all procedures and activities followed the principles of the Declaration of Helsinki. The HIMS has had Ethics committee approvals since initial recruitment in 1996 (University of Western Australia (UWA) Human Research Ethics Committee (HREC), RA/4/1/5765). The current study has been approved by both the Department of Health Western Australia (HDWA) HREC (RGS0000002777) and the UWA HREC (2022/ET000199).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lim, E.H., Franklin, P., Trevenen, M.L. et al. Exposure to low-level ambient air pollution and the relationship with lung and bladder cancer in older men, in Perth, Western Australia. Br J Cancer 129, 1500–1509 (2023). https://doi.org/10.1038/s41416-023-02411-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-023-02411-x