Abstract
The latest ASCO/CAP guideline has recommended to report oestrogen receptor (ER) low cases (ERlo; 1–10%) as “ER low positive category”, prompting us to compare the clinicopathologic features, biomarkers, survival and treatment of the ERlo cases with other subgroups (ER negative (ERneg) and ER high (ERhi)). ERlo cases revealed more similar clinicopathologic and biomarker profiles (including younger age, larger tumour, high proliferation, HER2 and basal markers expression) to ERneg than ERhi cancers. The ERlo cases receiving hormonal therapy showed a similarly poor outcome as ERneg cancers. However, majority of ERlo cases were downstaged to stage I in the 8th AJCC pathological prognostic staging, highlighting a risk of potential under treatment. Overall, our data highlighted the differences of ERlo from other ERpos cases and their management should be considered separately.
Similar content being viewed by others
Background
Oestrogen receptor (ER) expression as assessed by immunohistochemistry is an important predictive marker for hormonal therapy (HT) in breast cancers. Most guidelines set a positive threshold at 1% or above of any staining intensity and such patients are eligible for HT. However, there is a concern that the cases with low ER expression (ERlo, i.e. 1–10%) may be biologically distinct from the high ER expressing cases (ERhi, i.e. >10%) and not benefit from HT.1 The latest ASCO/ CAP guideline has acknowledged this and recommended reporting ERlo tumours as “ER Low Positive” category.2 A standardised comment is suggested to acknowledge the limited data on the overall benefit of HT for ERlo patients, the heterogeneity in their behaviour and biology as well as their similarity to ER-negative (ERneg) cancers in gene profiling. Decision regarding appropriate treatment should be made after considering the totality of the information about the individual case. Here, we re-evaluated the characteristic of these ERlo cases in comparison with ERneg and ERhi cases and the relevance of the new ERlo category in breast cancer management.
Methods
The study included 1824 consecutive cases of breast cancer diagnosed between 2002 and 2009 from three involved hospitals (Prince of Wales Hospital, Kwong Wah Hospital and Tuen Mun Hospital). Baseline demographic, clinical, treatment and outcome information were retrieved from the medical records. All patients were managed according to the NCCN guidelines. Histologic features including grade, necrosis and stromal tumour infiltrating lymphocytes (sTIL) were assessed on H&E slides as described previously.3 Immunohistochemical data on routine breast markers (including ER, progesterone receptor (PR), HER2 and Ki67), basal markers (CK5/6, CK14, EGFR, p63 and c-Kit) and androgen receptor (AR) were retrieved from our previous tissue microarray analysis.3 ER expression was also verified with medical records, and all cases were categorised into ERneg (0%), ERlo (1–10%) and ERhi (>10%). Disease‐free survival (DFS) and breast-cancer-specific survival (BCSS) were analysed using the Kaplan–Meier method and compared between groups using the log‐rank test. Comparison of features between different ER groups was performed using Chi‐square or Fisher’s exact test. All statistical analyses were performed in SPSS version 23.
Results
Table 1 summarised the clinical, histologic and biomarker features of the cohort. Fifty-four cases (3%) were ERlo, 503 (27.6%) cases were ERneg and 1266 (69.4%) cases were ERhi. Compared to ERhi cases, ERlo cases were associated with larger tumour, higher grade, more necrosis, more sTIL, higher pN stage, high KI67, HER2, EGFR and CK5/6 positivity but PR and AR negativity (p ≤ 0.039). Among the ERlo cases, only 24 cases (46.0%) had high expression of PR, much lower than the 73.7% (928/1259) in ERhi cases. Compared to ERneg cases, ERlo cases were associated with higher PR but lower grade, lower expression of CK5/6 and CK14 (p ≤ 0.014). ERlo cases were associated with more LVI (p = 0.024 and 0.011, respectively) and younger age (p = 0.005 and 0.004, respectively) than both ERneg and ERhi groups.
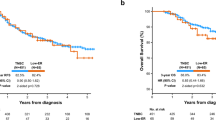
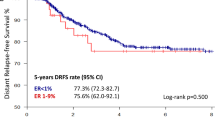
Among the cases with treatment data, 14.5% (56/385), 66.0% (33/50) and 94.8% (957/1010), respectively, of the ERneg, ERlo and ERhi cases received HT while 96.8% (299/309), 86.0% (43/50) and 64.8% (637/983) received chemotherapy, respectively. Most ERneg cases received HT were PRpos and some others had coexisting ERpos DCIS. Some ERlo/hi cases did not receive HT because of the higher ER diagnostic threshold applied for the earlier cases, patients’ comorbidity and refusal of treatment. Compared to ERhi cases, more ERlo cases received chemotherapy (p = 0.002), but less received HT (p < 0.001). Follow-up information was available for 1597 patients (median follow-up of 73 months, range 1–210 months). Among them, 3.1% and 66.1% have follow-up of ≤1 year and >5 years, respectively. The rate of relapse/mortality of ERlo cases (25.0%) was higher than ERhi cases (13.8%), but similar to ERneg cases (23.8%) (Table 1). Notably, high sTIL level showed a reduced mortality rate in both ERlo (low Vs high sTIL: 9.1 Vs 24.1%) and ERneg (14.4 Vs 24.0%) cancers. Additionally, the DFS of ERlo cases was significantly worse than ERhi cases (log-rank = 5.884, p = 0.015), but comparable to ERneg cases (log-rank = 0.020, p = 0.887) (supplementary Figure). Among patients receiving HT, those with ERlo cancers showed a significantly worse outcome than the ERhi cancer patients, but no difference from those ERneg cancer patients (without HT). If AJCC staging criteria were applied, 37 of the 49 (75.5%) ERlo cases would be downstaged by at least one substage (17 cases with ≥2 substages), and more ERlo cases were in pathological prognostic staging (PPS) stage I (55.1% (27/49)) compared to 18.0% stage I in anatomical staging (AS), and this may pose significant prognostic implication. Among all the PPS IA cases in the current cohort, cases of ERlo showed a significantly poorer DFS than ERhi cases (log-rank = 3.849, p = 0.050) (supplementary Figure).
Discussion
Here, we observed a similar proportion of ERlo cases as reported from a large series,4 but lower than some other smaller series.5,6 The ERlo cases, as reported,4,6 showed distinct clinicopathologic and biomarker profiles from ERhi cases. They were associated with expression of some basal markers, albeit at a lower rate than ERneg cases, and this was concordant with previous report that most ERlo cases were of basal molecular subtype.6 Thus, ERlo cases were heterogeneous, with some cases similar to ERneg cancers. Little apparent benefit from adjuvant HT for patients with low ER has been suggested.7 For treatment, it has been speculated that interventions for ERneg tumours may be appropriate for some ERlo cases. In fact, ERlo cases could behave clinically like triple negative breast cancer (TNBC) in terms of pathological complete response to neoadjuvant chemotherapy.8 Recently, immune blockade has been approved for treating TNBC.9 Despite the traditional view of ERpos cancers as non-immunogenic, the enrichment of sTIL and the associated reduced mortality within ERlo cases may suggest an active role of antitumour immunity and the potential of immunotherapy.
Recently, ER has been incorporated into the AJCC PPS together with PR, HER2 and grade. PPS shows a superior prognostication power than the traditional TNM AS.10 In the PPS, compared to the corresponding AS, if a breast cancer expresses ER and/or HER2, it will be downstaged. There is, however, a caveat as in the AJCC guideline, ER positivity was defined as expression in 1% or more of the tumour cells, without segregation into ERlo and ERhi. As we demonstrated, ERlo cases were biologically more similar to ERneg and showed worse survival in the downstaged cases. Thus, using the approach in AJCC staging, there is a real risk of downstaging ERlo cases that behave more like ERneg cases biologically, resulting in potentially under treatment.
This analysis confirmed that distinct behaviour of ERlo tumours, which are heterogeneous, with some resembling ERneg tumours biologically (higher likelihood of being basal-like, and worse prognosis), thus lending support to the new ASCO guideline. Furthermore, downstaging as per AJCC guideline for ERlo cases may incur a real possibility of risk underestimation and under treatment.
Limitations of the analysis included retrospective nature of the study and the small number of ERlo cases, which limited the power of statistical analysis. Moreover, some IHC data were obtained from TMA analysis. For PPS staging, no results from OncotypeDX were available.
References
Early Breast Cancer Trialists’ Collaborative Group, Davies, C., Godwin, J., Gray, R., Clarke, M., Cutter, D. et al. Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet 378, 771–784 (2011).
Allison, K. H., Hammond, M. E. H., Dowsett, M., McKernin, S. E., Carey, L. A., Fitzgibbons, P. L. et al. Estrogen and progesterone receptor testing in breast cancer: ASCO/CAP Guideline Update. J. Clin. Oncol. 38, 1346–1366 (2020).
Tsang, J. Y. S., Lee, M. A., Ni, Y. B., Chan, S. K., Cheung, S. Y., Chan, W. W. et al. Amyloid precursor protein is associated with aggressive behavior in nonluminal breast cancers. Oncologist 23, 1273–1281 (2018).
Yi, M., Huo, L., Koenig, K. B., Mittendorf, E. A., Meric-Bernstam, F., Kuerer, H. M. et al. Which threshold for ER positivity? a retrospective study based on 9639 patients. Ann. Oncol. 25, 1004–1011 (2014).
Balduzzi, A., Bagnardi, V., Rotmensz, N., Dellapasqua, S., Montagna, E., Cardillo, A. et al. Survival outcomes in breast cancer patients with low estrogen/progesterone receptor expression. Clin. Breast Cancer 14, 258–264 (2014).
Iwamoto, T., Booser, D., Valero, V., Murray, J. L., Koenig, K., Esteva, F. J. et al. Estrogen receptor (ER) mRNA and ER-related gene expression in breast cancers that are 1% to 10% ER-positive by immunohistochemistry. J. Clin. Oncol. 30, 729–734 (2012).
Chen, T., Zhang, N., Moran, M. S., Su, P., Haffty, B. G. & Yang, Q. Borderline ER-positive primary breast cancer gains no significant survival benefit from endocrine therapy: a systematic review and meta-analysis. Clin. Breast Cancer 18, 1–8 (2018).
Fujii, T., Kogawa, T., Dong, W., Sahin, A. A., Moulder, S., Litton, J. K. et al. Revisiting the definition of estrogen receptor positivity in HER2-negative primary breast cancer. Ann. Oncol. 28, 2420–2428 (2017).
Narayan, P., Wahby, S., Gao, J. J., Amiri-Kordestani, L., Ibrahim, A., Bloomquist, E. et al. FDA Approval Summary: Atezolizumab plus paclitaxel protein-bound for the treatment of patients with advanced or metastatic TNBC whose tumors express PD-L1. Clin. Cancer Res. https://doi.org/10.1158/1078-0432.CCR-19-3545 (2020).
Hu, J., Fung, M., Tsang, J. Y., Poon, I. K., Chan, S. K., Cheung, S. Y. et al. Improved prognostication for the updated AJCC breast cancer pathological prognostic staging varied in higher-stage groups. Clin. Breast Cancer 20, 253–261 (2020).
Author information
Authors and Affiliations
Contributions
I.P. collected the samples and performed the experiments; J.T. analysed data and wrote the paper; J.L. K.S. and S.C. collected and arranged clinic pathological data of cases; G.T. conceived the idea for the paper, provided guidance and critically revised the paper. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Joint CUHK-NTEC Research Ethics Committee. Waiver from patient’s consent was approved because of the retrospective and anonymised nature of this study. The study was performed in accordance with the Declaration of Helsinki.
Consent to publish
Not applicable.
Data availability
The dataset used and analysed in the current study is available from the corresponding author on reasonable request.
Competing interests
The authors declared no competing interests.
Funding information
No funding received for the current study.
Additional information
Note This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution 4.0 International (CC BY 4.0).
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Poon, I.K., Tsang, J.Y., Li, J. et al. The significance of highlighting the oestrogen receptor low category in breast cancer. Br J Cancer 123, 1223–1227 (2020). https://doi.org/10.1038/s41416-020-1009-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-020-1009-1
This article is cited by
-
Quantifying hormone receptor status in lobular breast cancer in an institutional series: the relationship between estrogen and progesterone receptor status and outcomes
Breast Cancer Research and Treatment (2023)
-
Relationship between ER expression by IHC or mRNA with Ki67 response to aromatase inhibition: a POETIC study
Breast Cancer Research (2022)
-
Association of H3K9me3 with breast cancer prognosis by estrogen receptor status
Clinical Epigenetics (2022)
-
49/w mit Lymphödem des Arms bei metastasiertem tripelnegativem Mammakarzinom
Der Onkologe (2022)
-
Characterization of estrogen receptor-low-positive breast cancer
Breast Cancer Research and Treatment (2021)