Abstract
Background The COVID-19 pandemic presented significant challenges to healthcare workers worldwide, including the effect on the psychological wellbeing of dentists.
Aims To evaluate the impact of the early phases of the pandemic on the psychological health, long-term wellbeing and clinical service provision of dentists, as well as the identification of the key risk and protective factors for adverse mental health outcomes (MHOs) in this group.
Methods A systematic review of cross-sectional studies (n = 53) from public and private dentistry sectors was employed to delineate the risk and protective factors for adverse MHOs.
Results Self-reports from these studies (1 December 2019 to 31 December 2021), involving 45,671 dentists worldwide were analysed. Study findings were classified according to their psychological impact (as risk or protective factors), categorised as 'operational' or 'organisational' and subdivided into 'psychosocial', 'occupational', 'sociodemographic' and 'environmental' elements. A GRADE (Grading of Recommendations, Assessment, Development, and Evaluations) certainty of evidence score was calculated for all the identified factors.
Conclusions This review confirmed the negative impact of the pandemic on the MHOs of dentists worldwide. Pivotal risk factors included fear of infection, transmission to families, lack of personal protective equipment and possible direct contact with infected patients. Enhanced infection control protocols, individual resilience and organisational support were identified as important protective factors.
Key points
-
This systematic review confirms the impact of the early phases of the COVID-19 pandemic on the psychological health of dentists.
-
Benefits include the identification of the pre-eminent risk and protective factors for long-term psychological wellbeing.
-
The distinction between operational and organisational elements may provide an important future framework for understanding the impact of job stressors in additional high-stress healthcare professions.
Similar content being viewed by others
Introduction
There is heightened interest in the impact of the COVID-19 pandemic on the wellness of frontline healthcare workers (HCWs), including dentists. The pandemic has resulted in deployment of significant resources, including an array of HCWs, to mitigate spread of disease and to reduce associated morbidity and mortality.1 The World Health Organisation (WHO) declared the outbreak a public health emergency of international concern in January 20202 and a pandemic in March 2020.3 The scale of the pandemic is unprecedented, impacting society, the global economy and provision of healthcare services.4 HCWs have been confronted by multiple challenges, including the scale and duration of additional pandemic-driven healthcare demand,5 resultant overwhelming workload6 and ongoing concerns over availability of personal protective equipment (PPE).7 Perceived lack of adequate preparations and organisational support8 have amplified the mental burden on HCWs.9 Resultant elevated levels of stress, anxiety and symptoms of depression could have long-term psychological implications on all HCWs.10 However, most research on the impact of stress, psychological distress and burnout on mental health outcomes (MHOs) in HCWs has been historically focused on physicians11 and nurses.12
There is burgeoning interest in the impact of the pandemic on psychological wellbeing of dentists.13 Multiple studies have reported on the global prevalence of work-related stress,14 psychological distress (PD)4 and burnout in dentists.15 Identifiable dentist-specific stressors include scheduling pressures,16 management of anxious patients,17 patient demands,18 fear of litigation and over-regulation,14 and business process stresses.19 These stressors have been posited to impact dentists' professionalism,20 productivity,21 clinical decision-making22 and service delivery.23
The COVID-19 crisis presents a considerable challenge to all healthcare systems and workers,24 including a profound impact on dental professionals and global dental practice.25,26 Therefore, supporting the psychological wellbeing of dentists is a priority. This review seeks to evaluate research on the effects of the early phase of the COVID-19 pandemic on the psychological health of dentists.
This includes the identification of pivotal risk and protective factors for adverse MHOs in dentists, their specific impacts and the implications for both long-term psychological wellbeing and clinical service delivery.
Methods
Design and reporting of this study were informed by the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement 2020,27 recommendations of WHO28 and COVID-19 collaboration guidelines.29 Databases searched were CINAHL, Embase, PsycINFO and Medline. The British Dental Journal was hand-searched in order to identify additional references not captured in the search strategy, while the reference lists of included articles provided additional sources.
The search strategy was: (COVID-19 or Coronavirus or 2019-ncov or sars-cov-2 or cov) AND (dentist or dentistry or dental practice) AND (work-related stress or anxiety or depression or fear or psychological distress or burnout) AND (English language only and 01/12/2019 to 31/12/2021). Published observational and experimental studies reporting on psychological impact of the COVID-19 pandemic on dentists were reviewed. Inclusion criteria for selection were:
-
1.
Dentists working close to coronavirus (exposed to increased risk)
-
2.
Dentists on mandated leave of absence from regular dental practice during the COVID-19 pandemic
-
3.
Psychological impact on the MHOs of dentists during the COVID-19 pandemic
-
4.
1 OR 2 AND 3.
Exclusion criteria were non-English language articles, studies involving dental students and collection of data before the outbreak of COVID-19. The review focused on graduate dentists specifically and not dental students, as these two groups differ in important characteristics, such as job roles, overall level of experience and volume of pandemic work experience. The nature of dentists' work, clinical experience and job role are unique in the dental workforce. All 975 titles and abstracts resulting from the database searches were screened for eligibility (by BL) and 145 were subject to full-text review. A total of 53 studies passed all inclusion and exclusion criteria (see Figure 1).
Contributors BL, JH and AK all made substantial contributions to the conception and design of the work. BL is a dentist, while JH and AK are occupational health psychologists with an interest in workplace health and wellbeing. Data were extracted from the 53 articles and summarised in a tabulated format (online Supplementary Information - sheet 1). This included: demographic and background information from each study (country, study design, participant numbers, sex, practice setting); measurement tools employed; reported MHOs; and compliance with clinical protocols. Also included in the table were principal findings, associated psychological impacts, study limitations and reported risk and protective factors for MHOs.
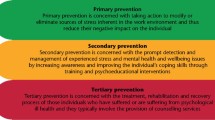
A narrative and tabulated data synthesis approach was employed.30,31 Outcomes of the selected studies were categorised according to the reported impact on psychological wellbeing of dentists, using criteria proposed by De Kock et al.,32 namely: a) general psychological impacts; b) risk factors associated with adverse MHOs; and c) protective factors against adverse MHOs. Multiple frameworks have been proposed that delineate work stressors, including the identification of operational and organisational stressors.33 In this review, risk and protective factors have been designated primarily as 'operational' or 'organisational' in nature (or both), and further sub-categorised into 'psychosocial', 'occupational', 'sociodemographic', or 'environmental' elements32 (Table 1).
Quality assessment of each study resulted in a GRADE (Grading of Recommendations, Assessment, Development, and Evaluations) certainty of evidence profile for each reported risk and protective factor associated with MHOs in dentists34 (online Supplementary Information - sheet 2). Sheet 3 in the online Supplementary Information presents the JBI Critical Appraisal Checklist for Cross-Sectional Studies that was used to assess individual study quality.35 The risk of bias was analysed using the Evidence Project appraisals tool36 (online Supplementary Information - sheet 4). Sheet 4 in the online Supplementary Information also reports on prior ethical approval status for each study.
Results
This review of 53 studies incorporates self-reports from 45,671 dentists (in over 70 countries) during the period December 2019 to December 2021. A majority of studies (n = 39) collected data between March and July 2020, corresponding to the initial phases of the COVID-19 pandemic. Analysis using the Joanna Briggs Institute critical appraisal checklist resulted in the studies being rated as 'excellent' (n = 7), 'good' (n = 9), 'fair' (n = 28) and 'poor' (n = 9). Prior ethical approval was reported in 77% of studies (n = 41). The Evidence Project risk of bias instrument confirmed 62% of studies (n = 33) as low risk for potential bias and 38% (n = 20) as high risk for bias. Multiple practice settings (private and public sector) and professional roles (majority general dentists) were included. The GRADE certainty of evidence score was applied to key identified risk factors (n = 17) and protective factors (n = 8). Baseline scores were designated as low (for all non-randomised controlled trial studies), as recommended by the Cochrane Consumers and Communication Group Advisory for Authors, and then either upgraded or downgraded according to their prescribed criteria.34
Results indicated that key risk factors provided a high certainty of the evidence, or very good indication of likely effect in three cases, a moderate certainty of evidence or good indication of likely effect in seven cases, and a low certainty or only some indication of effect in seven cases. Protective factors scored high (n = 3), moderate (n = 3) and low certainty of evidence (n = 2). Only two risk factors, namely age and sex, presented with significant conflicting opinions.
All included studies confirmed the substantial psychological impact of the COVID-19 pandemic on dentists. Validated measures employed to analyse anxiety, depression or burnout included the Generalised Anxiety Disorder Assessment (GAD-7),37 Patient Health Questionnaire-4 (PHQ-4),38 Depression Anxiety Stress Scale (DASS-21)39 and Maslach Burnout Inventory (MBI).40 GAD-7 was the most commonly used measure (seven studies).41,42,43,44,45,46,47
Categorisation of the specific MHOs for dentists (listed in Table 1) confirmed the reporting of symptoms of anxiety in 40 studies, including Chen et al.;43 fear in 44 studies;48,49 depression in 12 studies;50 psychological distress in 13 studies;51 burnout in 5 studies;52 and work-related stress in 22 studies.53 Ahmed et al.54 confirmed symptoms of anxiety in 78% of their reporting dentists, highlighting the fear of infection and transmission to families.
Fear of infection (n = 46),55 possible transmission to family members (n = 41),54 close contact with patients (n = 32)56 and the potential effects of aerosol generating procedures (n = 30)57 were the most prominent 'operational' ('occupational') risk factors. Two Italian studies recorded lower levels of severe anxiety at 9%44 and 6%.42 A Cameroon study58 confirmed reports of minimal or mild anxiety in 84% of participants, raising questions about the optimal approach to the definition of anxiety and highlighting possible reporting bias. A study on the prevalence of COVID-19 among 2,125 American dentists59 trialled a regimen of enhanced infection control protocols together with the Centre for Disease Control and Prevention's recommended levels of PPE supplies. Results confirmed a low COVID-19 prevalence of 0.9% (95% CI of 0.5-1.5) with a 3.6% testing positivity rate. This provided strong evidence for the impact of the combination of enhanced infection control protocols and appropriate PPE in the prevention of COVID-19 infection in dental settings.
Compliance with infection control protocols (n = 34),60 as well as access and availability of appropriate PPE supplies (n = 40),61,62,63 served as both 'operational' and 'organisational' ('occupational') risk factors, and potential protective factors for adverse MHOs in dentists.4
Results from Ahmed et al.54 reflect this duality, as despite 84% of their study group endorsing the use of recommended N95 masks, only 10% reported using them in practice. This emphasised worldwide organisational concerns with PPE production, delivery and costs.61 Similarly, Tysiac-Mista et al.64 reported that 71% of Polish dentists unilaterally suspended practice (despite no locally enforced lockdown) due to a lack of PPE, anxiety and fear. In contradistinction, a Brazilian study65 reported that a local group of dentists continued to provide regular dental care throughout their lockdown phase, despite acknowledging that their biosafety measures were not protective.
'Operational' ('sociodemographic') risk factors included age (n = 23),48,66,67,68,69 sex (n = 22),45,66,70,71 and predisposing medical history (n = 9).47,72 Gasparro et al.66 postulated that younger, less experienced dentists were more likely to develop psychological symptoms of anxiety and depression. In contrast, Hleyhel et al.67 asserted that younger dentists had superior knowledge of preventative measures (that could be considered to be protective if applied correctly). Chen et al.43 cited raised stress levels in male practitioners. However, in other studies, female dentists were reported to have higher levels of anxiety45 and fear.66 An association was also recorded between pre-existing medical conditions, symptoms of anxiety72 and prevalence of PD and depression.47
'Operational' ('environmental') risk factors were impacted by the review's narrow timeframe (n = 12)73 and the simultaneous absence of an approved vaccine in the early phases of the pandemic (n = 4).70 At this time, some dentists were also tasked with providing emergency dental care (often without adequate higher-level PPE).74,75
This scenario also highlighted the moral dilemma of many clinicians at having to defer patient dental care indefinitely.51,76 Additional 'operational' ('environmental') risk factors included: concerns for the long-term future of dentistry (n = 16);77 implications for the loss of earnings (n = 16);76 effect of pandemic-related inequalities of care (n = 4);78 and potential misinformation (n = 5) due to a perceived over-reliance on social media as a trusted source.41
Influential 'organisational' ('environmental') risk factors included perceived lack of pandemic preparedness (n = 18);55 absence of organisational support (n = 26);79 and an appeal to support less-developed countries.56 Reported 'operational' ('occupational') protective factors against adverse MHOs in dentists included the mitigating value of work experience (n = 10)68 and the knock-on effect of a successfully managed national COVID-19 campaign.80 Other notable protective factors were time off work,4 implementation of a vaccination campaign81 and improvements in training standards (n = 13).62 A variety of studies also advocated the promotion and use of purpose-built surgery equipment (n = 25),82 innovative dental treatment modalities, such as teledentistry,83 and track-and-trace mobile applications.84 The lone 'operational' ('environmental') protective factor reported was the development of individual resilience (n = 36),85 acknowledging the posited value of resilience (in conjunction with higher standards of knowledge and training) as a means of combating fear of contagion and associated anxiety.86 Uziel et al.,85 promoted the potential ability of dentists to manage their professional trauma as a self-growth opportunity. Additional reported factors included: an 'organisational' ('occupational') protective factor, namely, financial support (n = 21);42 combined 'operational'/'organisational' ('occupational') protective factors, including adequate PPE supplies (n = 37);71 enhanced infection control protocols (n = 33);87 and the pivotal 'organisational' ('environmental') protective factor, namely organisational support (n = 43).52,88
The magnitude of the impact of organisational support is highlighted in a study by Collin et al.4 on British dentists, that reported lower overall levels of PD during the national lockdown period than those recorded in 2017, using the same measure (57.8% vs 67.7%). This so-called public sector bubble effect was linked to the British Government's financial support package for NHS dentists during the pandemic lockdown period, highlighting the prospective value of providing appropriate and opportune organisational support.4 A similar initiative in Italy reportedly had little overall impact.66 It is noteworthy, however, that despite the reported decrease in levels of PD among UK dentists, the overall levels of PD in UK dentists remained high in comparison to other professions.4
Discussion
This review has confirmed the considerable psychological impact of the COVID-19 pandemic on the MHOs of dentists worldwide.89 Direct contact with patients during this period has been shown to generate fear of infection and possible secondary transmission to families, staff and patients.89Dentists considered the pandemic dangerous73 and felt unable to work safely during the early phases due to concerns over infection control protocols,90 the contemporaneous non-availability of a vaccine70 and a shortage of appropriate PPE.90 Dentists also highlighted longer-term fears for the economic viability of dental practices.76
Substantial evidence supports the assertion that fear of infection and subsequent transmission were accurate predictors of anxiety,91 depression,66 work-related stress,92 fear,93 PD61 and burnout.52 A broad spectrum of key risk and protective factors impacting the MHOs of dentists have also been identified and validated. Risk factors with strong evidence for impact included inadequate PPE supplies,91 compliance with infection control protocols81 and possible exposure to aerosol generating procedures.46 The protective factors with the strongest evidence included the development of individual resilience,85 enhanced compliance with recognised infection control protocols,89 guaranteed access to adequate PPE,91 availability of financial assistance44 and the pivotal role of effective organisational support.66
Given the prohibitions of routine dental care provision during the early stages of the pandemic and the cumulative impact of the risk factors reported by this review, it is not surprising that most dentists found this period particularly stressful and that their psychological wellbeing was challenged. The combined effect of dentist-specific stressors,14 which reportedly worsened during the pandemic,80 and the additional cumulative impact of the novel pandemic-specific stressors, was considerable.4
The identification of protective and risk factors, their classification into the 'operational' and 'organisational' typology, and their further sub-categorisation into 'psychosocial', 'occupational', 'sociodemographic' and 'environmental' elements32 underpins this review.
Symonds94 is reported to have first drawn this distinction between 'operational' and 'organisational' 'psychosocial' risk factors in their model on the emotional hazards of police work.33 'Organisational' 'psychosocial' factors were defined by Cox et al.95 as 'aspects of work design and the organisation and management of work, and their social and organisational contexts, that have the potential for causing psychological, social, or physical harm'. Houdmont et al.33 further suggested that in the UK policing context, this has resulted in the development of two parallel but disproportionate literatures. Ricciardelli and Carleton96 confirm the impact of both 'operational' and 'organisational' stressors on the MHOs of Canadian correctional workers, while also proposing that identified specific stressors may be modifiable. It is noteworthy that the outcomes of this review do not appear to map directly onto the current literature, with its apparent focus on 'operational' factors,33 but would rather seem to endorse a broader framework, with a mix of both 'operational' and 'organisational' elements.
This study underlines the potential value of appropriate organisational interventions, such as the recent UK public sector support package.4 Any future initiatives should, however, broaden their remit and incorporate an integral longer-term strategy for supporting both the physical and mental wellbeing of all dental professionals. The Management Standards approach97 offers a potential pathway to establishing a mutually agreeable and balanced relationship between the demands and responsibilities of both individual and organisational interventions,98 especially when linked to a robust theoretical framework, such as the job-demands and resources model.99
Limitations of this study included: an inability to infer causality due to the cross-sectional nature of the studies;100 the constraints of self-reporting; and the absence of a universal validated measure for reporting psychological impacts. Strengths of this study included: a worldwide distribution of data; rigorous analysis of study quality, risk of bias and certainty of the evidence; and substantial levels of concordance of reported clinical findings.
Conclusion
The COVID-19 pandemic has highlighted the presence of psychosocial working conditions that may have previously worked to the detriment of dentists.4 This hiatus could, however, provide a unique opportunity for the constructive re-engagement and reform of the profession, to the long-term benefit of all dental professionals and their patients.4 Future interventions must not only seek to bolster resilience but should modify working conditions to make them less problematic, including the contributions of organisational support from both regulatory bodies and central government alike. A holistic approach, centred on creating a healthy, safe and supportive working environment is recommended,32 in parallel with ongoing monitoring of the sustained impacts of the COVID-19 pandemic.4 Future research into both dentist-specific and pandemic-specific job stressors is advocated, including their complex interplay with identifiable risk and protective factors. The distinction between 'operational' and 'organisational' elements may provide an important future framework for understanding the impact of job stressors in additional high-stress healthcare professions.
References
Morgantini L A, Naha U, Wang H et al. Factors contributing to healthcare professional burnout during the COVID-19 pandemic: A rapid turnaround global survey. PLoS One 2020; DOI: 10.1371/journal.pone.0238217.
World Health Organisation. Statement on the second meeting of the International Health Regulations (2005). Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). 2020. Available at https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) (accessed August 2023).
Contini C, Caselli E, Martini F et al. COVID-19 Is a Multifaceted Challenging Pandemic Which Needs Urgent Public Health Interventions. Microorganisms 2020; 8: 1228.
Collin V, O´Selmo E, Whitehead P. Psychological distress and the perceived impact of the COVID-19 pandemic on UK dentists during a national lockdown. Br Dent J 2021; DOI: 10.1038/s41415-020-2592-5.
Shahbaz S, Ashraf M Z, Zakar R, Fischer F. Psychosocial, emotional and professional challenges faced by female healthcare professionals during the COVID-19 outbreak in Lahore, Pakistan: a qualitative study. BMC Womens Health 2021; 21: 197.
Shoja E, Aghamohammadi V, Bazyar H et al. Covid-19 effects on the workload of Iranian healthcare workers. BMC Public Health 2020; 20: 1636.
Gordon C, Thompson A. Use of protective equipment during the Covid-19 Pandemic. Br J Nurs 2020; 29: 748-752.
Afulani P A, Gyamerah A O, Nutor J J et al. Inadequate preparedness for response to COVID-19 is associated with stress and burnout among healthcare workers in Ghana. PLoS One 2021; DOI: 10.1371/journal.pone.0250294.
Mehta S, Machado F, Kwizera A et al. COVID-19: a heavy toll on health-care workers. Lancet Respir Med 2021; 9: 226-228.
Lai J, Ma S, Wang Y et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open 2020; DOI: 10.1001/jamanetworkopen.2020.3976.
Amoafo E, Hanbali N, Patel A, Singh P. What are the significant factors associated with burnout in doctors? Occup Med (Lond) 2015; 65: 117-121.
Firth-Cozens J, Payne R L. Stress in Health Professionals: Psychological and Organisational Causes and Interventions. Chichester: Wiley & Sons, 1999.
Molina-Hernández J, Fernández-Estevan L, Montero J, González-García L. Work environment, job satisfaction and burnout among Spanish dentists: a cross-sectional study. BMC Oral Health 2021; 21: 156.
Collin V, Toon M, O'Selmo E, Reynolds L, Whitehead P. A survey of stress, burnout and well-being in UK dentists. Br Dent J 2019; 226: 40-49.
Arora S, Knight A. Questionnaire Survey of Burnout Among Dentists in Singapore. Int Dent J 2021; 72: 161-168.
Miron C, Colosi H A. Work stress, health behaviours and coping strategies of dentists from Cluj-Napoca, Romania. Int Dent J 2018; 68: 152-161.
Meyerson J, Gelkopf M, Eli I, Uzil N. Burnout and professional quality of life among Israeli dentists: the role of sensory processing sensitivity. Int Dent J 2020; 70: 29-37.
Goetz K, Schuldei R, Steinhäuser J. Working conditions, job satisfaction and challenging encounters in dentistry: a cross-sectional study. Int Dent J 2019; 69: 44-49.
Johns R E, Jepsen D M. Sources of occupational stress in NSW and ACT dentists. Aust Dent J 2015; 60: 182-189.
Gorter R C, Eijkman M A, Hoogstraten J. Burnout and health among Dutch dentists. Eur J Oral Sci 2000; 108: 261-267.
Hakanen J J, Koivumäki J. Engaged or exhausted - How does it affect dentists' clinical productivity? Burnout Res 2014; 1: 12-18.
Chapman H R, Chipchase S Y, Bretherton R. The evaluation of a continuing professional development package for primary care dentists designed to reduce stress, build resilience and improve clinical decision-making. Br Dent J 2017; 223: 261-271.
Basson R A. Management and Prevention of Burnout in the Dental Practitioner. Dentistry 2013; DOI: 10.4172/2161-1122.1000168.
Fernandez R, Lord H, Halcomb E et al. Implications for COVID-19: A systematic review of nurses' experiences of working in acute care hospital settings during a respiratory pandemic. Int J Nurs Stud 2020; 111: 103637.
Humphris G, Knights J, Beaton L et al. Exploring the Effect of the COVID-19 Pandemic on the Dental Team: Preparedness, Psychological Impacts and Emotional Reactions. Front Oral Health 2021; DOI: 10.3389/froh.2021.669752.
Meng L, Hua F, Bian Z. Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine. J Dent Res 2020; 99: 481-487.
Page M J, McKenzie J E, Bossuyt P M et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; DOI: 10.1136/bmj.n71.
World Health Organisation. Rapid reviews to strengthen health policy and systems: a practical guide. 2017. Available at https://apps.who.int/iris/bitstream/handle/10665/258698/9789241512763-eng.pdf (accessed August 2023).
Garritty C, Gartlehner G, Nussbaumer-Streit B et al. Cochrane Rapid Reviews Methods Group offers evidence-informed guidance to conduct rapid reviews. J Clin Epidemiol 2021; 130: 13-22.
Campbell M, McKenzie J E, Sowden A et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ 2020; DOI: 10.1136/bmj.l6890.
Munn Z, Moola S, Lisy K, Riitano D. Systematic reviews of prevalence and incidence. In Joanna Briggs Institute Reviewer's Manual. Adelaide: The Joanna Briggs Institute, 2017.
De Kock J H, Latham H A, Leslie S J et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health 2021; 21: 104.
Houdmont J, Kerr R, Randall R. Organisational psychosocial hazard exposures in UK policing: Management standards indicator tool reference values. Policing Int J 2012; 35: 182-197.
Ryan R, Hill S. How to GRADE the quality of the evidence. Cochrane Consumers and Communication Group. 2016. Available at https://colorectal.cochrane.org/sites/colorectal.cochrane.org/files/public/uploads/how_to_grade.pdf (accessed August 2023).
Moola S, Munn Z, Tufanaru C et al. Systematic reviews of aetiology and risk. In Joanna Briggs Institute Reviewer's Manual. Adelaide: The Joanna Briggs Institute, 2017.
Kennedy C E, Fonner V A, Armstrong K A et al. The Evidence Project risk of bias tool: assessing study rigor for both randomized and non-randomized intervention studies. Syst Rev 2019; 8: 3.
Spitzer R L, Kroenke K, Williams J B, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006; 166: 1092-1097.
Kroenke K, Spitzer R L, Williams J B, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics 2009; 50: 613-621.
Lovibond P F, Lovibond S H. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther 1995; 33: 335-343.
Maslach C, Jackson S E, Leiter M P. MBI Maslach burnout inventory. Palo Alto: Consulting Psychologists Press, 1996.
Al-Amad S H, Hussein A. Anxiety among dental professionals and its association with their dependency on social media for health information: insights from the COVID-19 pandemic. BMC Psychol 2021; 9: 9.
Bellini P, Checchi V, Iani C, Bencivenni D, Consolo U. Psychological reactions to COVID-19 and epidemiological aspects of dental practitioners during lockdown in Italy. Minerva Dent Oral Sci 2021; 70: 32-43.
Chen Y, Li W. Influencing Factors Associated With Mental Health Outcomes Among Dental Medical Staff in Emergency Exposed to Coronavirus Disease 2019: A Multicentre Cross-Sectional Study in China. Front Psychiatry 2021; 12: 736172.
Consolo U, Bellini P, Bencivenni D, Iani C, Checchi V. Epidemiological Aspects and Psychological Reactions to COVID-19 of Dental Practitioners in the Northern Italy Districts of Modena and Reggio Emilia. Int J Environ Res Public Health 2020; 17: 3459.
Jyoti B, Kiran M, Srivastava R, Jaiswal V, Kumari S, Sinha A K. Psychological consequences of lockdown on dental professionals during the early phase of the COVID-19 pandemic. J Educ Health Promot 2021; 10: 472.
Kamal A T, Sukhia R H, Ghandhi D, Sukhia H R. Stress and anxiety among dental practitioners during the COVID-19 pandemic: A cross-sectional survey. Dent Med Probl 2021; 58: 139-146.
Tao J, Lin Y, Jiang L et al. Psychological Impact of the COVID-19 Pandemic on Emergency Dental Care Providers on the Front Lines in China. Int Dent J 2021; 71: 197-205.
Arif K, Malhotra S, Mohammad S et al. A Study to Assess the Knowledge and Perception of Practicing Dental Professionals Toward COVID-19 in Lucknow City. J Maxillofac Oral Surg 2022; 21: 961-971.
Ahmad M, Hussain U, Elahi A, Nazir A, Jawadtareen Chaudhary F A. Awareness of COVID-19 among dental practitioners of Multan. Pakistan J Med Health Sci 2021; 15: 1441-1444.
Alencar C M, Silva A M, Jural L A et al. Factors associated with depression, anxiety and stress among dentists during the COVID-19 pandemic. Braz Oral Res 2021; 35: e084.
Bagde R, Dandekeri S. Fear, Stress and Stigma of Covid-19 among Indian Dental Practitioners. J Evolution Med Dent Sci 2021; 10: 2433-2439.
Özarslan M, Caliskan S. Attitudes and predictive factors of psychological distress and occupational burnout among dentists during COVID-19 pandemic in Turkey. Curr Psychol 2021; 40: 3113-3124.
Aldhuwayhi S, Shaikh S A, Mallineni S K et al. Occupational Stress and Stress Busters Used Among Saudi Dental Practitioners During the COVID-19 Pandemic Outbreak. Disaster Med Public Health Prep 2022; 16: 1975-1981.
Ahmed M A, Jouhar R, Ahmed N et al. Fear and Practice Modifications among Dentists to Combat Novel Coronavirus Disease (COVID-19) Outbreak. Int J Environ Res Public Health 2020; 17: 2821.
Schmidt J, Perina V, Treglerova J, Pilbauerova N, Suchanek J, Smucler R. COVID-19 Prevalence among Czech Dentists. Int J Environ Res Public Health 2021; 18: 12488.
Balwani T R, Dubey S G, Sathe S, Chandak A, Khubchandani S. Assessment of fear psychosis and practice modification in dental fraternity to fight against COVID-19-a survey in Central India population. Int J Res Pharm Sci 2020; 11: 1339-1345.
Hasan S, Parmar S S, Saeed S. Depression, Anxiety, and Stress among Private Health Care Practitioners in Delhi NCR Region During Covid-19 Pandemic: A Cross-Sectional Study. Indian J Forensic Med Toxicol 2021; 15: 4074-4083.
Ebogo M, Danwang C, Endomba F T. Anxiety among Cameroonian dentists during the COVID-19 pandemic: A cross-sectional web-based survey. Advances Oral Maxillofac Surg 2021; 3: 100141.
Estrich C G, Mikkelsen M, Morrissey R et al. Estimating COVID-19 prevalence and infection control practices among US dentists. J Am Dent Assoc 2020; 151: 815-824.
Iorga M, Iurcov R, Pop L-M. The Relationship between Fear of Infection and Insomnia among Dentists from Oradea Metropolitan Area during the Outbreak of Sars-CoV-2 Pandemic. J Clin Med 2021; 10: 2494.
Duruk G, Gümüşboğa Z S, Çolak C. Investigation of Turkish dentists' clinical attitudes and behaviours towards the COVID-19 pandemic: a survey study. Braz Oral Res 2020; 34: e054.
Zeidi I M, Zeidi B M. Knowledge, attitude, fear, and practice towards coronavirus disease - 2019 preventive measures among Iranian dentists. Iranian Red Crescent Med J 2021; 23: 8.
Zeidi I, Zeidi B, Mirzaie S. Relationship Between Fear, Attitude and Knowledge, and COVID-19 Preventive Behaviours in Dentists. J Babol Univ Med Sci 2021; 23: 352-358.
Tysiąc-Miśta M, Dziedzic A. The Attitudes and Professional Approaches of Dental Practitioners during the COVID-19 Outbreak in Poland: A Cross-Sectional Survey. Int J Environ Res Public Health 2020; 17: 4703.
Vieira-Meyer A, Coutinho M B, Santos H P, Saintrain M V, Candeiro G T. Brazilian Primary and Secondary Public Oral Health Attention: Are Dentists Ready to Face the COVID-19 Pandemic? Disaster Med Public Health Prep 2022; 16: 254-261.
Gasparro R, Scandurra C, Maldonato N M et al. Perceived Job Insecurity and Depressive Symptoms among Italian Dentists: The Moderating Role of Fear of COVID-19. Int J Environ Res Public Health 2020; 17: 5338.
Hleyhel M, Haddad C, Haidar N, Charbachy M, Saleh N. Determinants of knowledge and prevention measures towards COVID-19 pandemic among Lebanese dentists: a cross sectional survey. BMC Oral Health 2021; 21: 241.
Serota K S, Andó B, Nagy K, Kovács I. Revealing Distress and Perceived Stress among Dentists at the Outset of the COVID-19 Pandemic: A Cross-Sectional Factor Analytic Study. Int J Environ Res Public Health 2021; 18: 11813.
Döken T, Bayram M, Bayram E, Ekmen H, r Gerçekcioğlu S N. Evaluation of anxiety levels among dentists working during the COVID-19 pandemic. Turk Endod J 2021; 6: 45-49.
Ismail N, Oweis Y, Alasmar A, Al-Raheam I A, Sabrah A. The change in stress and anxiety level caused by practicing dentistry during COVID-19 pandemic. Jordan Med J 2021; 55: 45-54.
Majeed M M, Saleem Z, Sarwar H, Ramzan Z, Iqbal S N, Naeem M M. The Psychology of Coronavirus Fear: Are Dentists of Pakistan Suffering from Corona-Phobia. J Pakistan Dent Assoc 2021; 30: 1-6.
Salehiniya H, Abbaszadeh H. Prevalence of corona-associated anxiety and mental health disorder among dentists during the COVID-19 pandemic. Neuropsychopharmacol Rep 2021; 41: 223-229.
Golchha V, Sharma P, Gupta B D, Yadav N. Impact of Covid 19 Pandemic on Dentists: Psychological Evaluation using DASS 21. Indian J Forensic Med Toxicol 2021; 15: 1232-1240.
Izzetti R, Gennai S, Nisi M et al. A perspective on dental activity during COVID-19: The Italian survey. Oral Dis 2021; 27: 694-702.
Sinjari B, Rexhepi I, Santilli M et al. The Impact of COVID-19 Related Lockdown on Dental Practice in Central Italy - Outcomes of A Survey. Int J Environ Res Public Health 2020; 17: 5780.
De Stefani A, Bruno G, Mutinelli S, Gracco A. COVID-19 Outbreak Perception in Italian Dentists. Int J Environ Res Public Health 2020; 17: 3867.
Çelik O E, Cansever I H. Evaluation of the effects of the COVID-19 pandemic on dentistry. Clin Exp Dent Res 2021; 7: 943-950.
Moraes R R, Correa M B, Queiroz A B et al. COVID-19 challenges to dentistry in the new pandemic epicentre: Brazil. PLoS One 2020; DOI: 10.1371/journal.pone.0242251.
Mahdee A F, Gul S S, Abdulkareem A A, Qasim S S. Anxiety, practice modification, and economic impact among Iraqi dentists during the COVID-19 outbreak. Front Med (Lausanne) 2020; 7: 595028.
Mekhemar M, Attia S, Dörfer C, Conrad J. The Psychological Impact of the COVID-19 Pandemic on Dentists in Germany. J Clin Med 2021; 10: 1008.
Suryakumari V B, Pallavi Reddy Y, Yadav S S, Doshi D, Reddy V S. Assessing Fear and Anxiety of Corona Virus Among Dental Practitioners. Disaster Med Public Health Prep 2022; 16: 555-560.
Sabea D W. Evaluation Of Responsiveness, Adaptation & Alertness For Sample Of Iraqi Dentists During COVID-19 Crunch/(Sample From Baghdad City). Sys Rev Pharm 2021; 12: 209-218.
Sadhurya M, Kannan A, Krithika C, Yesoda A K. Assessment of anxiety level and practice modifications among dentist during novel corona outbreak (Covid-19) in Tamilnadu. Int J Current Res Rev 2021; 13: 53-58.
Kinariwala N, Samaranayake L, Perera I, Patel Z. Knowledge, awareness and perceptions of coronavirus disease 2019 (COVID-19) in a cohort of Indian dental professionals: a questionnaire-based study. Stoma Edu J 2020; 7: 242-251.
Uziel N, Gilon E, Meyerson J et al. Dental personnel in Israel, Canada, and France during the COVID-19 pandemic: attitudes, worries, emotional responses, and posttraumatic growth. Quintessence Int 2021; 0: 444-453.
Mijiritsky E, Hamama-Raz Y, Liu F et al. Subjective Overload and Psychological Distress among Dentists during COVID-19. Int J Environ Res Public Health 2020; 17: 5074.
Cheng H-C, Chang Y-J, Liao S-R, Siewchaisakul P, Chen S L-S. The impact of COVID-19 on knowledge, attitude, and infection control behaviours among dentists. BMC Oral Health 2021; 21: 584.
Prasetyo Y T, Maulanti T, Persada S F, Redi A A, Young M N, Diaz J F. Factors influencing job satisfaction among dentists during the new normal of the COVID-19 pandemic in Indonesia: A structural equation modeling approach. Work 2021; 70: 365-376.
Uhlen M M, Ansteinsson V E, Stangvaltaite-Mouhat L et al. Psychological impact of the COVID-19 pandemic on dental health personnel in Norway. BMC Health Serv Res 2021; 21: 420.
Kamran R, Saba K, Azam S. Impact of COVID-19 on Pakistani dentists: a nationwide cross sectional study. BMC Oral Health 2021; 21: 59.
Ranka M S, Ranka S R. Survey of Mental Health of Dentists in the COVID-19 Pandemic in the UK. J Int Soc Prev Community Dent 2021; 11: 104-108.
Gungor A S, Donmez N A, Uslu Y S. Knowledge, stress levels, and clinical practice modifications of Turkish dentists due to COVID-19: a survey study. Braz Oral Res 2021; 35: e048.
Javed M Q, Chaudhary F A, Mohsin S F et al. Dental health care providers' concerns, perceived impact, and preparedness during the COVID-19 pandemic in Saudi Arabia. PeerJ 2021; DOI: 10.7717/peerj.11584.
Symonds M. Emotional hazards of police work. Am J Psychoanalysis 1970; 30: 155-160.
Cox T, Griffiths A, Rial-Gonzalez E. Work-related stress. Luxembourg: Office for Official Publications of the European Communities, 2000.
Ricciardelli R, Carleton R N. A qualitative application of the Job Demand-Control-Support (JDCS) to contextualize the occupational stress correctional workers experience. J Crime Justice 2022; 45: 135-151.
UK Government. What are the Management Standards? 2021. Available at https://www.hse.gov.uk/stress/standards/index.htm (accessed December 2021).
Mellor N, Smith P, Mackay C, Palferman D. The 'Management Standards' for stress in large organisations. Int J Workplace Health Manage 2007; 6: 4-17.
Bakker A B, Demerouti E. The Job Demands-Resources model: state of the art. J Managerial Psychol 2007; 22: 309-328.
Sedgwick P. Cross sectional studies: advantages and disadvantages. BMJ 2014; DOI: 10.1136/bmj.g2979.
Author information
Authors and Affiliations
Contributions
Brett Lefkowitz, Jonathan Houdmont and Alec Knight all made substantial contributions to the conception and design of the work. Brett Lefkowitz collected and analysed the data. Brett Lefkowitz and Alec Knight collaborated on the data analysis and interpretation. Brett Lefkowitz drafted the work, and all authors revised it critically for important intellectual content. All authors approved the final version and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest.
Relevant ethical standards and current best practice have been adhered to at all times. We approached the King's College London Research Ethics Committee for advice as to whether ethical clearance was required for this study. We were advised that formal research ethical clearance was not required as the study solely made use of data that were available in the public domain.
The authors confirm that the data supporting the findings of this study are available within the article (and/or) its supplementary materials.
Supplementary Information
Rights and permissions
Open Access. This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0.© The Author(s) 2023
About this article
Cite this article
Lefkowitz, B., Houdmont, J. & Knight, A. A systematic review of dentists' psychological wellbeing during the COVID-19 pandemic. Br Dent J (2023). https://doi.org/10.1038/s41415-023-6232-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41415-023-6232-8