Abstract
Introduction Mental health and wellbeing of the dental team has been brought into sharp focus during the COVID-19 pandemic. Despite this renewed interest, there has been longstanding issues with poor mental health and wellbeing in the dental profession for some time. While there is some evidence that documents poor mental wellbeing amongst dentists, there appears to be a lack of evidence concerning dental care professionals.
Aims To explore the level of mental wellbeing and stress amongst dental hygienists and therapists (DHTs) in South West England.
Method An online survey was distributed to DHTs in South West England via two professional networks.
Results A total of 129 surveys were completed. The mean levels of reported wellbeing were lower amongst DHTs than the general population and 45% of respondents reported high anxiety levels. Younger respondents reported lower levels of life satisfaction. Plus, 43.5% of dental therapists reported performing solely dental hygiene treatments, with those performing no dental therapy reporting lower happiness levels.
Conclusion Low mental wellbeing amongst DHTs in the South West has been identified in this survey and this is likely to impact negatively on the morale and motivation of the workforce, leading to increased levels of absenteeism and ultimately, loss of colleagues from the dental workforce. The stress encountered by DHTs is largely workplace-related and therefore, there is an increased need for team- and organisation-delivered interventions to improve mental wellbeing for this group.
Key points
-
Dental therapists and hygienists in South West England experience low levels of mental wellbeing compared to the general population.
-
The stress experienced by dental therapists and hygienists is predominantly workplace-centred.
-
A large proportion of the dental therapy profession in South West England are not working to their full scope of practice. Efforts to improve this may be beneficial for their mental wellbeing and would bring wider benefits to team-working, patient care and potentially NHS access.
Similar content being viewed by others
Introduction
It is widely accepted that dentistry is a stressful occupation,1,2,3,4 with a recent report suggesting that 'the high levels of self-reported stress, burnout and psychological distress…are a serious concern to the profession'.2 The recent COVID-19 pandemic has undoubtedly led to many additional challenges within the dental working environment.1,5 This has exacerbated existing stressors, such as financial pressures, NHS targets, staffing, time management and patient complaints.6,7 It has recently been reported that the impact of nation-wide increases in hospitalisations, death rates and tightening national restrictions during the course of the pandemic, in addition to personal COVID-19-related trauma, resulted in decreased psychological resources available to dental staff, which contributed to increased levels of fatigue, burnout and depressive symptoms in the workforce.8,9 These findings were not consistent across all dental staff and a great deal of variance in response to the pandemic was recorded, emphasising the importance of a tailored response to the emotional demands associated with dental care provision.9
Deterioration in mental health and wellbeing was evident before the COVID-19 pandemic, with a recent General Dental Council (GDC) report highlighting the increasing number of dentists demonstrating signs of burnout, poorer wellbeing and suicide ideation over the last decade.1,2Reports on stress among general dental practitioners have identified numerous systemic stressors, including time limitations, working environment, the NHS contract, fear of regulation and litigation, unrealistically high workload and patient issues.3,4,10,11The risk of litigation or regulatory chastisement have increasingly been recognised as major stressors for many, with dentists reported to be operating 'under constant fear of persecution'.2
Anxiety, stress or mental-health-related issues can impact significantly on clinical performance and although the evidence in dentistry is sparse, research in other areas of health care demonstrate a strong link between stress and impaired surgical competence and communication,12 with issues of burnout resulting in compromised work performance, absenteeism13 and worsening patient safety.14,15 Burnout can often lead to depression and stress increases the risk of developing mental health conditions, such as depression, alcoholism and drug addiction.3,4,16,17,18 Mental health and wellness of the dental team is critical in maintaining and retaining a healthy workforce. A recent report published by Dental Protection suggests that as many as half of dentists have considered leaving the profession due to concerns over their own personal wellbeing.19
Despite a growing evidence base relating to the mental health and wellbeing of dentists, the GDC report demonstrates a lack of evidence regarding the levels of mental wellbeing among other members of the dental team. Dental care professionals (DCPs) account for 63% of GDC registrants,20 encompassing a wide range of professional groups, each with a very individual skill set. In a study conducted among Northern Irish dentists and DCPs in 2011, it was reported that 20% of DCPs experienced psychological ill-health; however, this study fails to differentiate between the professional groups under the umbrella term of DCPs.21 A decade later, during the COVID-19 pandemic, mental wellbeing was again assessed in a UK dental hospital, which revealed that 53.3% of staff demonstrated symptoms of generalised anxiety.5 This study, undertaken in 2020, differentiates between DCPs, with dental nurses demonstrating the highest anxiety levels; however, no dental therapists or hygienists were recruited in this study.5
Dental therapists and hygienists (DHTs) account for a significant proportion of DCPs, yet this professional group would appear to be under-represented in the academic literature. An annual increase in the number of registrants and a desire for DCPs to contribute more effectively to NHS provision will reinforce the relevance of research across all dental professional groups to ensure their needs are met within future mental wellness strategies.
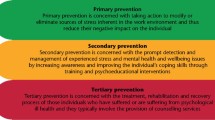
In order to provide safe and effective health care, organisations must protect their staff against burnout and emotional exhaustion through targeted intervention and prevention strategies.15 Within the dental sector, the Dental Professional Alliance has introduced the Mental wellness in dentistry framework, which enables dental workplaces to prioritise staff mental health.22 The framework provides guidance on how to promote mental wellbeing among the whole dental team and places emphasis on the importance of prevention and early intervention. This aligns with the NHS Long Term Plan, which aims to improve the NHS as a workplace and improve support offered to staff.23
This report aims to improve the evidence base, particularly in regards to prevalence, for mental wellbeing and stress among DHTs to better inform future practice and prevention strategies.
Methodology
Sample
An online survey was distributed to DHTs in the South West England branches of the British Association of Dental Therapists (BADT) and the British Society of Dental Hygiene and Therapy (BSDHT). The survey was distributed via a mailing list to the 207 members of the BADT (79 members) and BSDHT (128 members) in the South West region. The survey was also publicised on social media, including an open invitation on professional networking groups. Prior to distribution, the survey was piloted among DHTs practising in other regions of the UK.
The survey was launched at the start of December 2021 and was open for eight weeks, with a reminder email sent in the first week of January 2022. Details of the study, follow-up support, their right to withdraw at any time and a consent statement were included in the survey. Return of the survey was taken as consent to the process.
Participants
Survey participants were required to be registered DHTs currently providing dental services in the seven integrated care systems of South West England which comprises: Bristol, Cornwall, Dorset, Devon, Gloucestershire, Somerset and Wiltshire. Students and retired participants were excluded from the sample. Similarly, those delivering care outside of South West England were not included, regardless of home address.
Materials
The survey was distributed online using the Microsoft Forms platform and included questions related to:
-
Basic demographics
-
Working patterns
-
Qualification status
-
Wellbeing
-
Wellbeing in response to COVID-19 pandemic stress.
The survey was designed to incorporate a similar structure and pre-validated domains used in previous surveys of dentists, with permission sought and granted from previous survey authors. The Office for National Statistics (ONS)-4 tool was used to measure wellbeing among the respondents.24 This is divided into four questions on a scale of 0-10, with questions relating to life satisfaction, worthwhileness, happiness and anxiety.
Questions related to life satisfaction, worthwhileness and happiness were scored as 'low' if respondents reported scores of 0-4.24 Anxiety was scored as 'high' if respondents reported scores of between 6-10.24
Following the questions relating to life satisfaction, worthwhileness and happiness, respondents were asked if they thought their answers would have been different before the COVID-19 pandemic. These were grouped into: 'yes - higher scores since COVID-19 pandemic'; 'yes - lower scores since COVID-19 pandemic'; 'no - the same'; and 'not sure'. The same question was asked following the anxiety section of the ONS-4 measure.
Stress
A single measure of stress was used, which has been utilised in many large-scale national surveys, which asked respondents: 'in general, how do you find your job?'.25 The results of which were recorded on a Likert-scale, ranging from 'not at all stressful' to 'extremely stressful'.
The work stress in dentistry (WSID) measure, developed by Cooper et al.,26 was also used to identify stressors in the workplace. Following the use of this measure by Collin et al., questions related to litigation and regulation were again utilised.2 The questions were answered on a Likert-scale from 'not at all stressful' to 'extremely stressful' and were grouped into the following categories: work pressure; pay related; work content; dealing with patients; and litigation and regulation. An additional response of 'not applicable' was included, as some areas may not be applicable to all respondents based on working patterns.
Finally, an open-ended free response question was included, asking: 'are there other areas of your work that you feel are stressful?'.
Completion of the Health Research Authority decision tool determined that ethical approval for the survey was not required. This was a cross-sectional survey design with recruitment via professional groups and no personal identifiable data collected. Appropriate consent was obtained from each participant for use of their anonymous data.
Results
Overall, there were 129 responses to the survey, representing a response rate of 62.3%.
Of the 129 responses, four respondents were not currently practising as dental therapists or hygienists and were therefore excluded from the final data analysis. Similarly, 11 respondents failed to complete the full survey and one respondent was working outside the area of interest and were similarly excluded. Therefore, 113 responses were used in the final analysis.
Frequency analyses were carried out to describe respondent characteristics and demographics using SPSS Statistics v28. Two-sided Pearson's chi-squared tests and Fischer's exact tests were used to compare variables. Statistical significance was set with a p-value of 0.05. Figure 1 is presented with error bars set at 95% confidence intervals.
Sample demographics are detailed in Table 1.
With regards to field of practice, 85% of respondents worked primarily in general dental practice, with 8% based in teaching or research institutions, 2.7% in the community service, 1.8% in the armed forces, 1.8% in hospital services and 0.9% in specialist referral practices.
From the sampled dental therapists, 43.5% (n = 20) reported performing dental hygiene treatments only, with 56.6% performing any aspect of dental therapy in their role.
Wellbeing
The mean score reported by DHTs for life satisfaction was 6.56 (standard deviation [SD] = 1.81), worthwhile was 6.8 (SD = 1.93), happiness 6.52 (SD = 2.39) and anxiety 4.82 (SD = 2.91).
Overall, 14% (n = 16) of respondents reported low life satisfaction scores, 12% (n = 14) of respondents reported low worthwhile scores and 22% (n = 25) reported low happiness scores. Further, 45% (n = 51) of those surveyed reported high anxiety levels.
The number of respondents reporting low life satisfaction, worthwhileness and happiness scores were analysed by age, the number of years post qualification and the scope of practice delivered in their role. When comparing low life satisfaction scores against age, a significant difference was observed between those aged 45 or under and those aged above 45 (p = 0.049), indicating a higher frequency of younger DHTs reporting low life satisfaction compared with their older colleagues.
Dental therapists who routinely provided care within their scope of practice reported similar levels of wellbeing compared to those who provided hygiene treatments only. Where dental therapists only provided hygiene treatments, they reported statistically significant lower levels of happiness (p = 0.038).
COVID-19 pandemic
In total, 35.4% (n = 40) of respondents reported that their scores for life satisfaction, worthwhileness and happiness are lower since the COVID-19 pandemic. Similarly, 46% (n = 52) reported that their anxiety scores are higher since the COVID-19 pandemic.
Stress
On the single item of stress measure, 37.2% (n = 42) of respondents reported scores equating to high stress levels.
No significant difference was observed in occupational stress levels between those who worked exclusively privately and those who performed elements of NHS care (p = 0.128), or between therapists who performed solely hygiene procedures and those who performed elements of dental therapy (p = 0.555).
Sources of stress
Sources of stress were examined using the WSID measure and this was used to determine the most frequent sources of stress at work reported as 'very stressful' or 'extremely stressful'. The top ten sources of stress from the survey can be seen in Table 2.
Discussion
The findings of this survey indicate low levels of life satisfaction, worthwhileness and happiness in DHTs compared to the general population (Fig. 1) and comparatively higher levels of reported anxiety.27 This may, in part, be attributed to the COVID-19 pandemic, which has had far reaching effects on the dental sector. In this survey, 46% of respondents reported that their anxiety levels were higher since the start of the COVID-19 pandemic, a trend that is consistent in the general population, with reported work-related stress and anxiety increasing on pre-pandemic levels.28 Work-related anxiety, stress and depression accounted for 50% of work-related ill-health in the general population in 2020/2021.28 This is likely to be similar, if not higher, in the dental sector, where wellbeing is comparatively lower. Higher levels of staff suffering from work-related ill-health is likely to have wider implications for patient care delivery through higher levels of absenteeism and sick leave.
This survey has revealed that almost half of dental therapists are not working to their full scope of practice, with 43.5% performing hygiene treatments only. These results demonstrate the underutilisation of dental therapists in the South West region, a finding that is consistent across the UK29 and internationally.30 With a lack of opportunities to deliver their full scope of practice, therapists risk losing confidence and competence in the skills they have acquired. This can have negative consequences at many different levels, including effective team-working, patient care, future career development, professional fulfilment and personal mental health and wellbeing. Dually qualified dental hygienist-therapists may choose to work as hygienists due to local market factors and systemic barriers within the existing NHS contract, which fails to incentivise the use of therapists.31
Our findings indicate that dental therapists who performed hygiene treatments only reported significantly lower levels of happiness than their colleagues who performed elements of dental therapy. It has been previously reported that among UK DHTs, the most important predictor for overall job satisfaction is the variety of clinical activity performed, with a lack of therapy procedures being a source of disappointment and frustration for many.32 In terms of care provision, it is reported that approximately 70% of routine care provided under the current general dental services NHS contract could be performed by dental therapists.33
At a time where access to NHS dentistry is under unprecedented pressure, it is unfortunate that we have a highly-skilled workforce who are being under-utilised due largely to failings within the current NHS dental contract. It is hoped that dental contract reform in England, when finally implemented, will support greater skill-mix, efficiency in care delivery and utilisation of all available workforce. There is clearly a sense of urgency to introduce change; however, there is some debate as to the extent to which this can be provided in the NHS without significant structural reform.34 Following the introduction of direct access for DHTs in 2013,35 two-thirds of those treating patients without prescription from a dentist felt that providing care in this manner increased their job satisfaction.34 It has also been reported that patients feel more satisfied when being treated by dental therapists as opposed to dentists36and full utilisation of a therapist's skill set is likely to bring improved satisfaction to not only the treating practitioner, but also to dentists, employers and patients.
While this survey demonstrates fewer DHTs suffer from high work-stress compared to dentists, the sources of stress encountered vary considerably. Collin et al.2 reported that four of the top five stressors experienced by dentists involved the fear of litigation and over-regulation: threat of complaints; risk of making a mistake; bureaucracy; and concern about the GDC. Comparing this to the top five stressors reported by DHTs in this survey (Table 2), it can be observed that these stressors are more focused within the workplace itself and are related to the structural and organisational factors experienced by therapists and hygienists. Gallagher et al. proposed a model for categorising wellbeing influences, including: macro-level factors relating to professional regulation and systems; meso-level factors related to workplace and job specification; and micro-level factors incorporating relationships and personal factors.37 Application of this model would indicate that the predominant influences on the wellbeing of DHTs occur at the meso-level and involve workplace factors, such as time pressures and patient factors, as opposed to dentists, whose predominant influences occur at macro-level (system pressure and risk of litigation). It might therefore be inferred that the high stress experienced by DHTs relates more to the working environment and practice owners and managers should consider which elements of support are likely to be the most effective.
Ensuring that staff within the profession have improved levels of mental wellbeing is vital for recruitment and retention. High levels of work stress and low wellbeing reported in this survey have the potential to cause recruitment and retention difficulties for key members of the dental team. The UK dental sector is facing significant challenges relating to staff retention, with 40% of dentists in a British Dental Association study anticipating a change in career or early retirement in the next 12 months.38 Similarly, it is anticipated that one-third of UK dental nurses also plan on leaving the profession in the next two years,39 resulting in a significantly depleted dental workforce.
In respect to this survey, younger DHTs reported significantly lower levels of life satisfaction than their older colleagues, which may reflect the lack of social interaction during the COVID-19 pandemic and the resultant isolation. These findings are mirrored in studies conducted over two decades ago, indicating there may be deeper seated reasons for this observation.40 Lower job satisfaction, disengagement and exhaustion are all factors that increase intent to leave the profession.41 This is already having implications for staff retention in the USA, where 8% of dental hygienists left the workforce at the start of the COVID-19 pandemic.42 Promoting wellbeing and improving job satisfaction is likely to slow the flow of dental professionals leaving the industry and this must be a priority for employers and commissioners.
There are limitations to this survey. The overall response rate of 62% was moderate, although this rate is consistent with other questionnaire-based studies of health professionals.43 The results may therefore be subject to selection bias and caution should be applied to their generalisability. There may also be some individuals who received the invitation to participate twice as they featured in both professional networks and although there is a theoretical risk of duplicate responses, we feel this is unlikely. There is no demographic data available locally to compare the profile of non-responders to the sampling frame and so the results must be interpreted with caution, as the issues identified here may not be representative of other DHTs locally or nationally in England. Nevertheless, this survey provides useful information on this important and underreported issue within the dental therapy and hygienist workforce.
Conclusion
This survey demonstrates that mental wellbeing among the dental therapy and hygiene community in South West England is poorer than the general population. Lower rates of wellbeing, higher stress levels and increased anxiety among the workforce is likely to result in increased rates of absenteeism and risks further loss of dental professionals from the workforce. The survey also highlights the underutilisation of dental therapists in the region, which is unlikely to improve without significant structural reform. Dentists' wellbeing is primarily influenced by regulatory pressures, while DHTs experience most stress in the workplace. Efforts must be concentrated to enhance wellbeing within the workplace to improve mental wellbeing at a practice level. The introduction of the Mental wellness in dentistry framework22 is seen as an excellent resource, which is likely to have benefits for clinicians, their employers and the communities they serve.
References
General Dental Council. Mental Health and Wellbeing in Dentistry: A Rapid Evidence Assessment. 2021. Available at https://www.gdc-uk.org/docs/default-source/research/mental-health-and-wellbeing-in-dentistry27973e06-eb0f-4ee2-b92f-7fee3d2baf5b.pdf?sfvrsn=511f2ef9_5 (accessed June 2022).
Collin V, Toon M, O'Selmo E, Reynolds L, Whitehead P. A survey of stress, burnout and well-being in UK dentists. Br Dent J 2019; 226: 40-49.
British Dental Association. The Mental Health and Well-being of UK Dentists: A Qualitative Study. 2017. Available at https://bda.org/about-the-bda/campaigns/Documents/The%20Mental%20Health%20and%20Well-being%20of%20UK%20Dentists.pdf (accessed November 2022).
Myers H L, Myers L B. 'It's difficult being a dentist': stress and health in the general dental practitioner. Br Dent J 2004; 197: 89-93.
Mahendran K, Patel S, Sproat C. Psychosocial effects of the COVID-19 pandemic on staff in a dental teaching hospital. Br Dent J 2020; 229: 127-132.
Dental Protection. Covid-19: Dental Protection survey reveals top 5 worries for dentists. 2020. Available at https://www.dentalprotection.org/uk/articles/covid-19-dental-protection-survey-reveals-top-5-worries-for-dentists (accessed July 2022).
Bretherton R, Chapman H R, Chipchase S. A study to explore specific stressors and coping strategies in primary dental care practice. Br Dent J 2016; 220: 471-478.
Humphris G, Knights J, Beaten L et al. Exploring the Effect of the COVID-19 Padenmic on the Dental Team: Preparedness, Psychological Impacts and Emotional Reactions. Front Oral Health 2021; 2: 669752.
Freeman R, Knights J, Beaton L et al. Prediction of emotional exhaustion over the course of the COVID-19 pandemic in primary care dental staff: an intensive longitudinal study. BMJ Open 2021; DOI: 10.1136/bmjopen-2021-054827.
Chapman H, Chipchase S Y, Bretherton R. Understanding emotionally relevant situations in primary dental practice. 2. Reported effects of emotionally charged situations. Br Dent J 2015; DOI: 10.1038/sj.bdj.2015.852.
British Dental Association. Sources of Work-related Stress among Salaried Primary Care Dentists in the UK. 2014. Available at https://bda.org/about-the-bda/campaigns/Documents/Sources%20of%20stress%20among%20salaried%20dentists.pdf (accessed November 2022).
Arora S, Sevdalis N, Nestel D, Woloshynowych M, Darzi A, Kneebone R. The impact of stress on surgical performance: a systematic review of the literature. Surgery 2010; 147: 318-330.
Dyrbye L N, Shanafelt T D, Johnson P O, Johnson L A, Satele D, West C P. A cross-sectional study exploring the relationship between burnout, absenteeism, and job performance among American nurses. BMC Nurs 2019; 18: 57.
Garcia C L, de Abreu L C, Ramos J L S et al. Influence of Burnout on Patient Safety: Systematic Review and Meta-Analysis. Medicina (Kaunas) 2019; 55: 553.
Hall L, Johnson J, Watt I, Tsipa A, O'Connor D B. Healthcare Staff Wellbeing, Burnout, and Patient Safety: A Systematic Review. PLoS ONE 2016; DOI: 10.1371/journal.pone.0159015.
Denton D A, Newton J T, Bower E J. Occupational burnout and work engagement: a national survey of dentists in the United Kingdom. Br Dent J 2008; DOI: 10.1038/sj.bdj.2008.654.
Hill K B, Burke F J T, Brown J et al. Dental practitioners and ill health retirement: a qualitative investigation into the causes and effects. Br Dent J 2010; DOI: 10.1038/sj.bdj.2010.814.
Kay E J, Lowe J C. A survey of stress levels, self-perceived health and health-related behaviours of UK dental practitioners in 2005. Br Dent J 2008; DOI: 10.1038/sj.bdj.2008.490.
Dental Protection. Half of dentists in the UK have considered leaving dentistry for reasons of personal wellbeing. 2020. Available at https://www.dentalprotection.org/uk/articles/half-of-dentists-in-the-uk-have-considered-leaving-dentistry-for-reasons-of-personal-wellbeing (accessed July 2022).
General Dental Council. Registration report - January 2022. 2022. Available at https://www.gdc-uk.org/docs/default-source/registration-reports/registration-report_january-2022.pdf?sfvrsn=bd140c06_5 (accessed June 2022).
Gorter R C, Freeman R. Burnout and engagement in relation with job demands and resources among dental staff in Northern Ireland. Community Dent Oral Epidemiol 2011; 39: 87-95.
Mental Health Wellness in Dentistry. Framework. 2022. Available at https://mhwd.org/framework/ (accessed June 2022).
NHS. The NHS Long Term Plan. 2019. Available at https://www.longtermplan.nhs.uk/publication/nhs-long-term-plan/ (accessed May 2022).
Office for National Statistics. Personal well-being user guidance. 2018. Available at https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/methodologies/personalwellbeingsurveyuserguide (accessed February 2022).
Houdmont J, Cox T, Griffiths A. Work-related stress case definitions and prevalence rates in national surveys. Occup Med (Lond) 2010; 60: 658-661.
Cooper C L, Watts J, Baglioni Jr A J, Kelly M. Occupational stress among general practice dentists. J Occup Psychol 1988; 61: 163-174.
Office for National Statistics. Quarterly personal well-being estimates - non-seasonally adjusted. 2022. Available at https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/datasets/quarterlypersonalwellbeingestimatesnonseasonally adjusted (accessed February 2022).
Health and Safety Executive. Work-related stress, anxiety or depression statistics in Great Britain, 2022. 2022. Available at https://www.hse.gov.uk/statistics/causdis/stress.pdf (accessed November 2022).
Godson J H, Williams S A, Csikar J I, Bradley S, Rowbotham J. Dental therapy in the United Kingdom: part 2. A survey of reported working practices. Br Dent J 2009; 207: 417-423.
Chen D, Hayes M, Holden A. A global review of the education and career pathways of dental therapists, dental hygienists and oral health therapists. Br Dent J 2021; 230: 533-538.
Williams S A, Bradley S, Godson J H, Csikar J I, Rowbotham J. Dental therapy in the United Kingdom: part 3. Financial aspects of current working practices. Br Dent J 2009; 207: 477-483.
Turner S, Ross M K, Ibbetson R J. Job satisfaction among dually qualified dental hygienist-therapists in UK primary care: a structural model. Br Dent J 2011; DOI: 10.1038/sj.bdj.2011.50.
Gallagher J E, Lim Z, Harper P R. Workforce skill mix: modelling the potential for dental therapists in state-funded primary dental care. Int Dent J 2013; 63: 57-64.
Turner S, Ross M. Direct access: how is it working? Br Dent J 2017; 222: 191-197.
General Dental Council. Direct Access. 2019. Available at https://www.gdc-uk.org/standards-guidance/standards-and-guidance/direct-access (accessed June 2022).
Sun N, Burnside G, Harris R. Patient satisfaction with care by dental therapists. Br Dent J 2010; DOI: 10.1038/sj.bdj.2010.209.
Gallagher J E, Colonio-Salazar F B, White S. Supporting dentists' health and wellbeing - workforce assets under stress: a qualitative study in England. Br Dent J 2021; DOI: 10.1038/s41415-021-3130-9.
Westgarth D. The dental workforce: An assessment of the recruitment market. BDJ In Pract 2022; 35: 14-18.
Dentistry. Dentistry Census - dentistry risks losing one third of UK's dental nurses in next two years. 2022. Available at https://dentistry.co.uk/2022/04/18/dentistry-census-dentistry-risks-losing-one-third-of-uks-dental-nurses-in-the-next-two-years/ (accessed May 2022).
Gibbons D, Corrigan M, Newton J. The working practices and job satisfaction of dental therapists: findings of a national survey. Br Dent J 2000; 189: 435-438.
Patel B M, Boyd L D, Vineyard J, LaSpina L. Job Satisfaction, Burnout, and Intention to Leave among Dental Hygienists in Clinical Practice. J Dent Hyg 2021; 95: 28-35.
Gurenlian J R, Morrissey R, Estrich C G et al. Employment Patterns of Dental Hygienists in the United States During the COVID-19 Pandemic. J Dent Hyg 2021; 95: 17-24.
Edwards P J, Roberts I, Clarke M J et al. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev 2009; DOI: 10.1002/14651858.MR000008.pub4.
Acknowledgements
We would like to thank the British Dental Association for sharing their survey and the University of Plymouth Medical School for statistical support.
Author information
Authors and Affiliations
Contributions
The study was conceptualised by Georgia Hallett, Robert Witton and Ian Mills. The survey was developed by Georgia Hallett and reviewed by Robert Witton and Ian Mills. Data analysis was performed by Georgia Hallett with assistance from the University of Plymouth medical statistics team. The draft manuscript was prepared by Georgia Hallett, with contributions from Robert Witton and Ian Mills.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest.
Completion of the Health Research Authority decision tool determined that ethical approval for the survey was not required. This was a cross-sectional survey design with recruitment via professional groups and no personal identifiable data collected.
Details of the study, follow-up support, the right to withdraw at any time and a consent statement were included in the survey and return of the survey was taken as consent to the process. Appropriate consent was obtained from each participant for use of their anonymous data.
Rights and permissions
About this article
Cite this article
Hallett, G., Witton, R. & Mills, I. A survey of mental wellbeing and stress among dental therapists and hygienists in South West England. Br Dent J (2022). https://doi.org/10.1038/s41415-022-5357-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41415-022-5357-5
This article is cited by
-
Dental practice workforce challenges in rural England: survey into recruitment and retention in Devon and Cornwall
British Dental Journal (2023)