Abstract
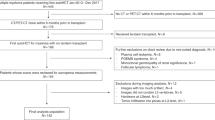
The prevalence of osteoporosis in post stem cell transplantation (SCT) is poorly defined. We performed a systematic review and meta-analysis to determine the prevalence of osteoporosis in patients with hematologic diseases who underwent SCT. PubMed, EMBASE, and Web of Science were searched (from inception to 30th April 2023) using Medical Subject Headlines to find studies that assessed the prevalence of osteoporosis among post SCT. Thirteen articles meeting the inclusion criteria were included in the analysis. The pooled prevalence rates of osteoporosis, osteopenia, and decreased bone mineral density (BMD) were determined to be 14.2% (95% CI 9.7–18.8), 36.0% (95% CI 23.8–48.2), and 47.8% (95% CI 36.6–58.9), respectively. Substantial heterogeneity was observed among the included studies (I² values ranged from 81% to 99%). Subgroup analyses revealed variations in prevalence based on gender, follow-up duration, age, region, sample size, and study quality. These findings suggest a high prevalence of osteoporosis in post-SCT patients. Given the negative impact of osteoporosis on prognosis and recipient survival, clinicians should prioritize preventive measures, early diagnosis, and effective treatments to minimize its impact.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Kendler DL, Body JJ, Brandi ML, Broady R, Cannata-Andia J, Cannata-Ortiz MJ, et al. Bone management in hematologic stem cell transplant recipients. Osteoporos Int. 2018;29:2597–610.
Khan Z, Agarwal NB, Bhurani D, Khan MA. Risk factors for hematopoietic stem cell transplantation-associated bone loss. Transplant Cell Ther. 2021;27:212–21.
Compston JE, McClung MR, Leslie WD. Osteoporosis. Lancet. 2019;393:364–76.
Clynes MA, Harvey NC, Curtis EM, Fuggle NR, Dennison EM, Cooper C. The epidemiology of osteoporosis. Br Med Bull. 2020;133:105–17.
Fuggle NR, Curtis EM, Ward KA, Harvey NC, Dennison EM, Cooper C. Fracture prediction, imaging and screening in osteoporosis. Nat Rev Endocrinol. 2019;15:535–47.
Force USPST, Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, et al. Screening for osteoporosis to prevent fractures: US Preventive Services Task Force recommendation statement. JAMA. 2018;319:2521–31.
Evenepoel P, Claes K, Meijers B, Laurent MR, Bammens B, Naesens M, et al. Bone mineral density, bone turnover markers, and incident fractures in de novo kidney transplant recipients. Kidney Int. 2019;95:1461–70.
Krol CG, Dekkers OM, Kroon HM, Rabelink TJ, van Hoek B, Hamdy NA. Longitudinal changes in BMD and fracture risk in orthotopic liver transplant recipients not using bone-modifying treatment. J Bone Miner Res. 2014;29:1763–9.
Durette G, Jomphe V, Bureau NJ, Poirier C, Ferraro P, Lands LC, et al. Long-term bone mineral density changes and fractures in lung transplant recipients with cystic fibrosis. J Cyst Fibros. 2021;20:525–32.
Tran TVM, Li X, Maalouf NM. Bone health outcomes in post-lung transplant patients with cystic fibrosis. J Cyst Fibros. 2023;22:381–7.
Seguro L, Pereira RMR, Seguro LPC, Caparbo VF, Avila MS, Mangini S, et al. Bone metabolism impairment in heart transplant: results from a prospective cohort study. Transplantation. 2020;104:873–80.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Available from: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Duggan SN, Smyth ND, Murphy A, Macnaughton D, O’Keefe SJ, Conlon KC. High prevalence of osteoporosis in patients with chronic pancreatitis: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2014;12:219–28.
Barberio B, Zamani M, Black CJ, Savarino EV, Ford AC. Prevalence of symptoms of anxiety and depression in patients with inflammatory bowel disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2021;6:359–70.
Benz E, Trajanoska K, Lahousse L, Schoufour JD, Terzikhan N, De Roos E, et al. Sarcopenia in COPD: a systematic review and meta-analysis. Eur Respir Rev. 2019;28:190049.
Castaneda S, Carmona L, Carvajal I, Arranz R, Diaz A, Garcia-Vadillo A. Reduction of bone mass in women after bone marrow transplantation. Calcif Tissue Int. 1997;60:343–7.
Baumgartner A, Moesch M, Zumsteg M, Struja T, Bernet S, Medinger M, et al. Predictors of impaired bone health in long-term survivors after allogeneic stem cell transplantation. Bone Marrow Transplant. 2019;54:1651–61.
Schimmer AD, Mah K, Bordeleau L, Cheung A, Ali V, Falconer M, et al. Decreased bone mineral density is common after autologous blood or marrow transplantation. Bone Marrow Transplant. 2001;28:387–91.
Leguy D, Magro L, Pierache A, Coiteux V, Yakoub Agha I, Cortet B, et al. Changes in bone mineral density after allogenic stem cell transplantation. Joint Bone Spine. 2022;89:105373.
Seneviratne AK, Wright C, Lam W, Lipton JH, Michelis FV. Comorbidity profile of adult survivors at 20 years following allogeneic hematopoietic cell transplantation. Eur J Haematol. 2021;106:241–9.
Gubrianska D, Machaczka M, Hassan M, Hagglund H, Ljungman P, Palmer M. Bone and hormonal status 10 years post-allogeneic bone marrow transplantation. Clin Transplant. 2019;33:e13742.
Yao S, Smiley SL, West K, Lamonica D, Battiwalla M, McCarthy PL, et al. Accelerated bone mineral density loss occurs with similar incidence and severity, but with different risk factors, after autologous versus allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2010;16:1130–7.
Abou-Mourad YR, Lau BC, Barnett MJ, Forrest DL, Hogge DE, Nantel SH, et al. Long-term outcome after allo-SCT: close follow-up on a large cohort treated with myeloablative regimens. Bone Marrow Transplant. 2010;45:295–302.
Yao S, McCarthy PL, Dunford LM, Roy DM, Brown K, Paplham P, et al. High prevalence of early-onset osteopenia/osteoporosis after allogeneic stem cell transplantation and improvement after bisphosphonate therapy. Bone Marrow Transplant. 2008;41:393–8.
Ria R, Scarponi AM, Falzetti F, Ballanti S, Di Ianni M, Sportoletti P, et al. Loss of bone mineral density and secondary hyperparathyroidism are complications of autologous stem cell transplantation. Leuk Lymphoma. 2007;48:923–30.
Massenkeil G, Fiene C, Rosen O, Michael R, Reisinger W, Arnold R. Loss of bone mass and vitamin D deficiency after hematopoietic stem cell transplantation: standard prophylactic measures fail to prevent osteoporosis. Leukemia. 2001;15:1701–5.
Schulte C, Beelen DW, Schaefer UW, Mann K. Bone loss in long-term survivors after transplantation of hematopoietic stem cells: a prospective study. Osteoporos Int. 2000;11:344–53.
Kashyap A, Kandeel F, Yamauchi D, Palmer JM, Niland JC, Molina A, et al. Effects of allogeneic bone marrow transplantation on recipient bone mineral density: a prospective study. Biol Blood Marrow Transplant. 2000;6:344–51.
Wang L, Yu W, Yin X, Cui L, Tang S, Jiang N, et al. Prevalence of osteoporosis and fracture in China: the China osteoporosis prevalence study. JAMA Netw Open. 2021;4:e2121106.
Tauchmanova L, Colao A, Lombardi G, Rotoli B, Selleri C. Bone loss and its management in long-term survivors from allogeneic stem cell transplantation. J Clin Endocrinol Metab. 2007;92:4536–45.
Anastasilakis AD, Tsourdi E, Makras P, Polyzos SA, Meier C, McCloskey EV, et al. Bone disease following solid organ transplantation: a narrative review and recommendations for management from The European Calcified Tissue Society. Bone. 2019;127:401–18.
Curtis EM, van der Velde R, Moon RJ, van den Bergh JP, Geusens P, de Vries F, et al. Epidemiology of fractures in the United Kingdom 1988-2012: Variation with age, sex, geography, ethnicity and socioeconomic status. Bone. 2016;87:19–26.
Zavatta G, Clarke BL. Glucocorticoid- and transplantation-induced osteoporosis. Endocrinol Metab Clin North Am. 2021;50:251–73.
Arias-Espinosa L, Acosta-Medina AA, Vargas-España A, Fuentes-Martin V, Colunga-Pedraza PR, Hawing-Zarate JA, et al. Acute leukemia relapse after hematopoietic stem cell transplantation: the good, the bad, and the ugly of isolated extramedullary relapse in a Latin American population. Transplant Cell Ther. 2023;29:510.e1–510.e9.
Shen Y, Huang X, Wu J, Lin X, Zhou X, Zhu Z, et al. The global burden of osteoporosis, low bone mass, and its related fracture in 204 countries and territories, 1990-2019. Front Endocrinol (Lausanne). 2022;13:882241.
Banfi A, Podesta M, Fazzuoli L, Sertoli MR, Venturini M, Santini G, et al. High-dose chemotherapy shows a dose-dependent toxicity to bone marrow osteoprogenitors: a mechanism for post-bone marrow transplantation osteopenia. Cancer. 2001;92:2419–28.
Funding
This study was funded by the National Natural Science Foundation of China (No. 81700044), the Huan-hua Talents Project from Sichuan Provincial People’s Hospital, and the Key R&D Program of the Department of Science and Technology of Sichuan Province (No. 2022YFS0600).
Author information
Authors and Affiliations
Contributions
YYM and PS conceived of the study concept and design. YYM and SJG performed the literature search, study selection and collected all data. YYM and PS contributed to the data analysis and interpretation of results. YYM drafted the manuscript, RX, XJY, and YPL revised the manuscript critically for important intellectual content. All authors reviewed the manuscript and approved the final submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, YM., Guo, SJ., Xiao, R. et al. Prevalence of osteoporosis among patients after stem cell transplantation: a systematic review and meta-analysis. Bone Marrow Transplant (2024). https://doi.org/10.1038/s41409-024-02243-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41409-024-02243-0