Abstract
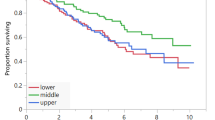
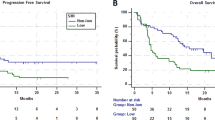
Sarcopenia, defined as loss of muscle mass, can occur with aging. We conducted a single-center retrospective analysis to evaluate the impact of muscle quality in multiple myeloma (MM), a hematologic cancer of older adults, undergoing autologous hematopoietic cell transplantation (autoHCT). Healthy muscle was quantified by measuring the percent of high-density muscle within the L3 psoas muscle using a novel computed tomography method in 142 eligible patients. Early post-transplant complications were assessed in the first 100 days after transplant. Sarcopenia, defined as ≤80% high-density muscle, was found in 72 (51%) patients. Sarcopenic obesity, defined as sarcopenia and a BMI ≥ 30, was found in 32 (23%) patients. One or more early complications occurred in 22 (16%) patients. Cardiovascular events accounted for 36% of all complications. Patients with sarcopenia had more cardiac complications (12.5%) than patients without (2.9%, p = 0.03). Multivariate analysis revealed increased BMI at transplant, but not sarcopenia, was associated with worse OS (hazard ratio: 1.11, 95% confidence interval: 1.02–1.22, p = 0.02). Our analysis suggests that sarcopenia is prevalent in MM and associated with increased early post-transplant cardiovascular complications in MM. Obesity, regardless of sarcopenia, is associated with worse survival in MM. Our study generates hypothesis-generating data to risk-stratify patients being considered for autoHCT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
von Haehling S, Morley JE, Anker SD. An overview of sarcopenia: facts and numbers on prevalence and clinical impact. J Cachexia Sarcopenia Muscle. 2010;1:129–33. https://doi.org/10.1007/s13539-010-0014-2.
Walston JD. Sarcopenia in older adults. Curr Opin Rheumatol. 2012;24:623–7. https://doi.org/10.1097/BOR.0b013e328358d59b.
Choi KM. Sarcopenia and sarcopenic obesity. Korean J Intern Med. 2016;31:1054–60. https://doi.org/10.3904/kjim.2016.193.
Carneiro IP, Mazurak VC, Prado CM. Clinical implications of sarcopenic obesity in cancer. Curr Oncol Rep. 2016;18:62. https://doi.org/10.1007/s11912-016-0546-5.
Caram MV, Bellile EL, Englesbe MJ, Terjimanian M, Wang SC, Griggs JJ, et al. Sarcopenia is associated with autologous transplant-related outcomes in patients with lymphoma. Leuk lymphoma. 2015;56:2855–62. https://doi.org/10.3109/10428194.2015.1014359.
Lanic H, Kraut-Tauzia J, Modzelewski R, Clatot F, Mareschal S, Picquenot JM, et al. Sarcopenia is an independent prognostic factor in elderly patients with diffuse large B-cell lymphoma treated with immunochemotherapy. Leuk lymphoma. 2014;55:817–23. https://doi.org/10.3109/10428194.2013.816421.
Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M et al. SEER Cancer Statistics Review, 1975–2016, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2016/, based on November 2018 SEER data submission, posted to the SEER web site, April 2019, 2019.
D’Souza A, Zhang MJ, Huang J, Fei M, Pasquini M, Hamadani M, et al. Trends in pre- and post-transplant therapies with first autologous hematopoietic cell transplantation among patients with multiple myeloma in the United States, 2004–14. Leukemia. 2017;31:1998–2000. https://doi.org/10.1038/leu.2017.185.
Sergentanis TN, Zagouri F, Tsilimidos G, Tsagianni A, Tseliou M, Dimopoulos MA, et al. Risk Factors for Multiple Myeloma: A Systematic Review of Meta-Analyses. Clin lymphoma, myeloma Leuk. 2015;15:563–77 e561-563. https://doi.org/10.1016/j.clml.2015.06.003.
Patel JJ, Baruah D, Sobush D, Koester K, Aase J, Zellner S, et al. Identifying high-attenuating and low-attenuating muscle using computerized tomography and exploring its impact on physical function and muscle strength in obese critically Ill patients. Nutr Clin Pr. 2020;35:133–41. https://doi.org/10.1002/ncp.10325.
Lodewick TM, van Nijnatten TJ, van Dam RM, van Mierlo K, Dello SA, Neumann UP, et al. Are sarcopenia, obesity and sarcopenic obesity predictive of outcome in patients with colorectal liver metastases? HPB. 2015;17:438–46. https://doi.org/10.1111/hpb.12373.
Tan BH, Birdsell LA, Martin L, Baracos VE, Fearon KC. Sarcopenia in an overweight or obese patient is an adverse prognostic factor in pancreatic cancer. Clin Cancer Res. 2009;15:6973–9. https://doi.org/10.1158/1078-0432.CCR-09-1525.
Chin SO, Rhee SY, Chon S, Hwang YC, Jeong IK, Oh S, et al. Sarcopenia is independently associated with cardiovascular disease in older Korean adults: the Korea National Health and Nutrition Examination Survey (KNHANES) from 2009. PLoS ONE. 2013;8:e60119. https://doi.org/10.1371/journal.pone.0060119.
Kang DO, Park SY, Choi BG, Na JO, Choi CU, Kim EJ, et al. Prognostic impact of low skeletal muscle mass on major adverse cardiovascular events in coronary artery disease: a propensity score-matched analysis of a single center all-comer cohort. J Clin Med. 2019; 8. https://doi.org/10.3390/jcm8050712.
Ko BJ, Chang Y, Jung HS, Yun KE, Kim CW, Park HS, et al. Relationship between low relative muscle mass and coronary artery calcification in healthy adults. Arterioscler Thromb Vasc Biol. 2016;36:1016–21. https://doi.org/10.1161/ATVBAHA.116.307156.
DeFilipp Z, Troschel FM, Qualls DA, Li S, Kuklinski MW, Kempner ME, et al. Evolution of body composition following autologous and allogeneic hematopoietic cell transplantation: incidence of sarcopenia and association with clinical outcomes. Biol Blood Marrow Transplant. 2018;24:1741–7. https://doi.org/10.1016/j.bbmt.2018.02.016.
Zakaria HM, Elibe E, Macki M, Smith R, Boyce-Fappiano D, Lee I, et al. Morphometrics predicts overall survival in patients with multiple myeloma spine metastasis: a retrospective cohort study. Surg Neurol Int. 2018;9:172. https://doi.org/10.4103/sni.sni_383_17.
Bhamidipati PK, Carson KR, Wildes T. Psoas cross-sectional area as radiographic measure of sarcopenia does not predict overall survival in multiple myeloma. Blood. 2013;122:5326. https://doi.org/10.1182/blood.V122.21.5326.5326.
Takeoka Y, Sakatoku K, Miura A, Yamamura R, Araki T, Seura H, et al. Prognostic effect of low subcutaneous adipose tissue on survival outcome in patients with multiple myeloma. Clin lymphoma, myeloma Leuk. 2016;16:434–41. https://doi.org/10.1016/j.clml.2016.04.010.
Mishra A, Pidala JA, Betts B, Fernandez H, Nishihori T, Extermann M, et al. Body composition predicts for survival in allogeneic (allo) hematopoietic stem cell transplantation (HCT) recipients. Biol Blood Marrow Tr. 2016;22:S69–S69. https://doi.org/10.1016/j.bbmt.2015.11.361.
Ellulu MS, Patimah I, Khaza’ai H, Rahmat A, Abed Y. Obesity and inflammation: the linking mechanism and the complications. Arch Med Sci. 2017;13:851–63. https://doi.org/10.5114/aoms.2016.58928.
Vogl DT, Wang T, Perez WS, Stadtmauer EA, Heitjan DF, Lazarus HM, et al. Effect of obesity on outcomes after autologous hematopoietic stem cell transplantation for multiple myeloma. Biol Blood Marrow Transplant: J Am Soc Blood Marrow Transplant. 2011;17:1765–74. https://doi.org/10.1016/j.bbmt.2011.05.005.
Prado CM, Gonzalez MC, Heymsfield SB. Body composition phenotypes and obesity paradox. Curr Opin Clin Nutr Metab Care. 2015;18:535–51. https://doi.org/10.1097/MCO.0000000000000216.
Oray M, Abu Samra K, Ebrahimiadib N, Meese H, Foster CS. Long-term side effects of glucocorticoids. Expert Opin drug Saf. 2016;15:457–65. https://doi.org/10.1517/14740338.2016.1140743.
Davis MP, Panikkar R. Sarcopenia associated with chemotherapy and targeted agents for cancer therapy. Ann Palliat Med. 2019;8:86–101. https://doi.org/10.21037/apm.2018.08.02.
Bouchonville MF, Villareal DT. Sarcopenic obesity: how do we treat it? Curr Opin Endocrinol Diabetes Obes. 2013;20:412–9. https://doi.org/10.1097/01.med.0000433071.11466.7f.
Hsu KJ, Liao CD, Tsai MW, Chen CN. Effects of exercise and nutritional intervention on body composition, metabolic health, and physical performance in adults with sarcopenic obesity: a meta-analysis. Nutrients. 2019; 11. https://doi.org/10.3390/nu11092163.
Koliaki C, Liatis S, Dalamaga M, Kokkinos A. Sarcopenic obesity: epidemiologic evidence, pathophysiology, and therapeutic perspectives. Curr Obes Rep. 2019;8:458–71. https://doi.org/10.1007/s13679-019-00359-9.
Smith L, McCourt O, Henrich M, Paton B, Yong K, Wardle J, et al. Multiple myeloma and physical activity: a scoping review. BMJ Open. 2015;5:e009576. https://doi.org/10.1136/bmjopen-2015-009576.
Acknowledgements
This work was funded by the 2019 American Society of Hematology Minority Medical Student Award Program (AW) and supported by a K23HL141445 from the National Heart, Lung, and Blood Institute (AD). Its contents are solely the responsibility of the authors and do not represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AW, DB, JP, AS, SC, SJ, and MS do not report any conflict of interest. BD reports grants and/or fees from Celgene, Takeda, Jannsen, Amgen, GSK; PH reports grants and fees from Celgene/BMS, Takeda, Janssen, Amgen, Sanofi, Karyopharm; AD reports grants Takeda, Sanofi, TeneoBio, EDO Mundipharma and Prothena, and fees from Prothena, Pfizer, Akcea, Imbrium
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Williams, A., Baruah, D., Patel, J. et al. Prevalence and significance of sarcopenia in multiple myeloma patients undergoing autologous hematopoietic cell transplantation. Bone Marrow Transplant 56, 225–231 (2021). https://doi.org/10.1038/s41409-020-01008-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-020-01008-9
This article is cited by
-
Muscle and fat composition in patients with newly diagnosed multiple myeloma
Blood Cancer Journal (2023)
-
A comprehensive review of the impact of obesity on plasma cell disorders
Leukemia (2022)
-
Exploring health behaviors and the feasibility of a lifestyle intervention for patients with multiple myeloma
Supportive Care in Cancer (2022)