Abstract
Rituximab-based chemo-immunotherapy is currently the standard first-line treatment for Waldenstrom macroglobulinaemia (WM), while ibrutinib has emerged as an alternative. In the absence of randomised trials (RCTs) comparing these regimens, the optimal first-line treatment for WM remains uncertain. In this systematic review and meta-analysis, we sought to assess the efficacy and safety of first-line treatment regimens for WM. We searched key databases from January 2007 to March 2023, including phase II and III trials, including treatment-naïve WM patients treated with rituximab-based regimens or ibrutinib. Response rates, progression-free survival (PFS), overall survival (OS), and toxicities were evaluated. Four phase III and seven phase II trials were included among 736 unique records. Pooled response rates from all comparative and non-comparative trials were 46%, 33% and 26% for bendamustine rituximab (BR), bortezomib-dexamethasone, cyclophosphamide, rituximab (BDRC) and ibrutinib rituximab (IR), respectively. Two-year pooled PFS was 89%, 81% and 82% with BR, BDRC and IR, respectively. Neuropathy was more frequent with bortezomib, while haematologic and cardiac toxicities were more common with chemo-immunotherapy and ibrutinib-based regimens respectively. Our findings suggest that BR yields higher response rates than bortezomib or ibrutinib-based combinations. RCTs comparing BR against emerging therapies, including novel Bruton Tyrosine Kinase Inhibitors, are warranted.
Similar content being viewed by others
Introduction
Waldenstrom macroglobulinaemia (WM) is a rare mature B-cell neoplasm characterised by clonal lymphoplasmacytic (LPL) bone marrow (BM) infiltration and immunoglobulin M (IgM) paraproteinaemia [1]. While a watch-and-wait approach is appropriate for asymptomatic patients, treatment is indicated when clinical manifestations arise due to the IgM paraprotein or LPL infiltrate [2]. Major classes of agents commonly used for the treatment of WM include monoclonal antibodies, alkylating agents, proteasome inhibitors, and Bruton Tyrosine Kinase inhibitors (BTKi) [3].
Rituximab is a key component of WM treatment, and has been evaluated in combination with bortezomib [4, 5], dexamethasone and bortezomib (BDR) [6, 7]; dexamethasone and cyclophosphamide (DRC) [8], bortezomib cyclophopshamide dexamethasone(B-DRC) [9], and bendamustine (BR) [10,11,12]. The BTKi ibrutinib was shown to be an effective therapy for newly diagnosed WM and is approved by the Food and Drug Administration for this indication [13]. While oral administration and a favourable toxicity profile have made ibrutinib an attractive option, fixed-duration treatment with chemo-immunotherapy remains a valid alternative [2, 14].
The rarity of WM and the paucity of randomised trials (RCTs) comparing chemo-immunotherapy and BTKi-based treatment has resulted in uncertainty regarding the optimal therapy for treatment-naïve WM patients. In this systematic review and meta-analysis, our objective was to compare the efficacy and safety of rituximab-based chemo-immunotherapy and BTKi-based regimens for newly diagnosed WM from all comparative and non-comparative trials.
Methods
A systematic literature review was performed according to the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [15]. A study protocol was written a priori and registered with PROSPERO (Registration number: 283550).
We performed literature searches of the following electronic databases: Medline and Medline In-process (using the PubMed platform), Embase (using the Elsevier Platform), and The Cochrane Library from January 2007 to March 2023. The rationale for the period of the search strategy was that the key trials of rituximab-based chemo-immunotherapy and BTKi therapy were published after 2006. We also searched ClinicalTrials.gov and the International Clinical Trials Registry Platform (http://www.who.int/ctrp/en/.) to identify ongoing, discontinued and completed clinical trials: There was no limit on language or geographical perspective. Briefly, the population studied was treatment-naïve WM patients, and the interventions included rituximab-based chemo-immunotherapy or BTKi-based regimens. Detailed inclusion and exclusion criteria are presented in Supplementary Tables S1 and S2.
The study selection process was performed in the following two phases: Level 1 screening: titles and abstracts of studies identified from the electronic databases and the internet searches were reviewed by two researchers (SDM, WLC), independently and in parallel, to determine eligibility according to the criteria in Supplementary Table S1. Level 2 screening: Full texts of studies selected at level 1 were obtained and reviewed by two researchers (SDM, WLC), independently and in parallel, to determine eligibility according to the criteria in Supplementary Table S2. Where there was disagreement about study relevance at either stage of screening, consensus was reached with a third member of the study team (MS).
The results of the systematic literature review were summarised qualitatively and quantitatively as appropriate. The outcomes of interest were: response rates based on International Waldenstrom Macroglobulinaemia Working Group (IWWM) criteria [16] (Supplementary Table S3), time to achievement of partial response or complete response, rates of relapse, progression-free survival (PFS), overall survival (OS), treatment-related complications, and quality-of-life scores. Where outcomes were reported as dichotomous data in trials, we calculated the risk ratios (RR) and 95% confidence interval (CI) for meta-analysis using Review Manager software (version 5.4). Evidence from single-arm studies was summarised using descriptive summary statistics. Continuous measures were expressed in the form of mean (standard deviation).
Where the demographics of the study populations and inclusion/exclusion were relatively similar between the single-arm cohort studies, a meta-analysis of proportions (expressed as a percentage), with their 95% CI, was performed using the software Comprehensive Meta-analysis (version 3.3). To establish the variance of raw proportions, a Freeman-Tukey transformation was applied. To incorporate heterogeneity (anticipated among the included studies), transformed proportions were combined using DerSimonian-Laird random effects models.
In order to assess whether effect sizes were consistent across the included studies, heterogeneity was quantified. The test for heterogeneity was performed using the I2 statistic, which provides a magnitude of variability, where 0% indicates that any variability is due to chance, whilst higher I2 values (>50%) indicate increasing levels of unexplained variability. Where we have judged that the included trials are too clinically heterogeneous to warrant a formal meta-analysis, we presented the results of the included trials in a narrative format instead of performing a meta-analysis. All the studies were evaluated with the critical appraisal tools by the Joanna Briggs Institute or the Centre for Reviews and Dissemination (Table 1).
Results
Results of the search
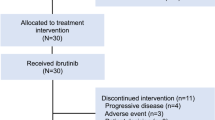
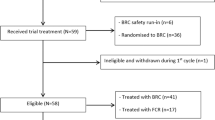
The searches yielded 736 distinct references. Of these, 16 records were duplicates, therefore 720 titles and abstracts were eligible for screening. After removing irrelevant and clearly ineligible studies, we assessed the full texts of 93 studies for eligibility. Finally, 61 studies were excluded, and 30 publications that reported results from 11 unique trials were included in this systematic review and meta-analysis (Fig. 1).
Study characteristics
Of the 30 publications reporting on 11 trials, four were phase III RCTs [9,10,11, 13], and seven were phase II single-arm studies. The comparisons in the RCTs included the following interventions: BR versus R-CHOP (1 trial), BR versus R-CHOP or R-CVP (1 trial); I-R versus rituximab (I trial); and B-DRC versus DRC (1 trial). All 11 studies used the World Health Organisation (WHO) criteria for diagnosis of WM [1] and IWWM criteria for response definitions (Supplementary Table S3) [16]. The sample sizes of the studies ranged from 23 to 261, with a male predominance and a median age of patients ranging from 58 to 70 years. Details of the included studies are summarised in Table 2. All relevant outcome measures were reported in most studies except for quality-of-life measures, which were not reported in most trials.
Meta-analysis
Rituximab-based chemo-immunotherapy regimens
Response rates and time to best response
Rates of complete response (CR) and very good partial response (VGPR) based on IWWM criteria were reported in all 11 trials that were included. When the response rate was reported by more than one study, proportions were pooled from both RCTs and single-arm trials to find the estimates (Fig. 2 and Supplementary Fig. S1). The response category near CR (nCR) was reported in only one trial [4]. The combined CR, VGPR and nCR rates in patients given rituximab-based chemo-immunotherapy regimens were 47% (95% CI 34–60%) with bortezomib bendamustine rituximab (BBR); 46% (95% CI 30–63%) with BR; 33% (95% CI 24–40%) with BDRC; 30% with BDR; 25% with R-CHOP; 15% with DRC and 8% with bortezomib rituximab.
A comparison of regimens showed that bendamustine-based therapies (BR and BBR) had a higher probability of achieving a CR or VGPR than other regimens (Fig. 3). Two RCTs (Rummel et al., 2013 [10], Flinn et al., 2014 [17]) compared BR versus R-CHOP or R-CHOP/R-CVP respectively and the pooled evidence shows that response rates were higher with BR; however, the risk difference was not statistically significant (RD 0.06, 95% CI −0.02 to 0.14). Similar results were observed with one RCT that compared B-DRC to DRC (Buske et al., 2023 [9]). The evidence suggests that patients in the B-DRC arm had higher rates of CR or VGPR than those in the DRC group, although the difference observed was not statistically significant (RD 0.12, 95% CI −0.01 to 0.24).
Overall pooled major response (combined CR, VGPR, PR) rates for each regimen were as follows: BBR (89%), BR (83%), BDR (82%), Bortezomib, Rituximab (66%), DRC (81%), BDRC (85%) and RCHOP (91%) (Supplementary Fig. S4). PR rates for each regimen (pooled values for regimens evaluated in more than one trial) were as follows: BR (44%), BBR (42%) BDR (54%), Bortezomib, Rituximab (58%), DRC (71%), BDRC (53%) and RCHOP (66%) (Supplementary Figs. S2 and S3).
The median time to best response was 6.8 months for DRC [18] and five [19] to 15 months [6] for BDR. Median time to best response was not reported in the trials evaluating BR. The median time to first response was 1.4 to 3 months for BDR [6, 19] and 3.3 months for B-DRC [9]. As the time to response data were not consistently reported across trials, a meaningful comparison between regimens was not possible in this case.
Progression-free survival
Two-year pooled PFS rates for each regimen were as follows: BR (89%), BBR (89%), BDR (69%), Bortezomib, Rituximab (66%), DRC (69%), Bortezomib-DRC (81%) (Fig. 4). Evidence from one trial evaluating the BBR regimen reported a PFS of 75% at 3 years [12]. Five-year PFS was reported for three regimens: BDRC (63%), BR (74%) and DRC (32%) (Supplementary Fig. S5). These data suggest that Bendamustine-based regimens result in better PFS at 3- and 5- years compared to other rituximab-based chemo-immunotherapy regimens.
Overall survival
The duration of follow-up and reporting of OS varied across trials. However, 2-year OS rates were reported by six trials and the available data were combined when two or more trials reported this outcome to evaluate the pooled estimate. The 2-year OS rates reported were as follows: BR (97%), BDR (80%), DRC (91%), BDRC (94%) (Supplementary Fig. S6).
Comparing BTK inhibitor-based regimens with rituximab-based immuno-chemotherapy
The major response rate for patients treated with IR was 73%, and the median time to best response was 3 months (range 1–46 months) [20]. The combined CR and VGPR rate for IR was 26% (95% CI 17–35%) compared to 47% (95% CI 34–60%) for BBR; 46% (95% CI 30–63%) with BR; and 33% (95% CI 24–40%) with BDRC (Fig. 2). IR resulted in 2-year PFS (Fig. 4) and OS (Supplementary Fig. S6) of 82% and 90%, respectively [20] which is comparable to the rituximab-based immuno-chemotherapy regimens overall.
Outcomes based on MYD88 and CXCR4 mutational status
Outcomes based on MYD88/CXCR4 mutational status were not reported in most trials. A phase II trial of BR showed no significant difference in response rates or PFS based on MYD88 or CXCR4 mutational status [21]. It is however noteworthy that the numbers of patients in each mutational category were small, and none of the MYD88/CXCR4 double mutant patients progressed, while two of six double wild type patients did. The INNOVATE trial also reported similar response rates and PFS in patients treated with IR across mutational subtypes [13, 20]. It is noteworthy that responses to the BDRC regimen also appeared to be independent of MYD88/CXRC4 mutational status [9].
Treatment-related adverse effects
In terms of toxicities, IR was associated with more grade 3 and 4 cardiac/vascular toxicities, including hypertension and arrhythmias [13, 20]. Bortezomib-containing regimens were associated with an increased incidence of peripheral neuropathy, with approximately 20% and 10% of patients experiencing at least grade 2 and grade 3-4 neuropathy, respectively [4, 6, 7, 19]. It is noteworthy that more recent studies using subcutaneous bortezomib reported a lower incidence of peripheral neuropathy (10% grade 1 and 2% grade 3) [9]. Chemotherapy-based regimens, such as DRC, were associated with a higher incidence of haematological toxicity than those using bortezomib and ibrutinib. Of note, 20% of patients receiving DRC [8, 18] and 29% of those receiving BR [10, 11] experienced grade 3-4 neutropenia, compared to approximately 12% in those receiving bortezomib-based treatments [4, 6, 7, 19] and 10% of those receiving IR [13, 20].
Discussion
We present the first systematic review and meta-analysis comparing first-line treatment regimens for WM in the BTKi era. Current practice recommendations by the IWWM [2] suggest the use of either rituximab-based chemo-immunotherapy, rituximab combined with proteasome inhibitors, or BTKi, in symptomatic, treatment-naïve patients with WM. In this systematic review, evidence from comparative and non-comparative studies suggests that among the options recommended by the IWWM, bendamustine-based regimens may result in improved response rates and PFS compared to BTKi- and bortezomib-based regimens. It is noteworthy that OS did not differ significantly between the treatment groups, which may be a function of the effective second-line therapies available.
A comparison of treatment regimens for WM had previously been attempted by Santos Lozano et al. [22]. This study did not however include the key RCTs evaluating BR and was performed before the advent of BTKi. More recent studies by Khurshid et al. [23] and Zheng et al. [24] also did not include BTKi in their comparison of treatment options. Of these, Khurshid et al. [23] focused exclusively on purine analogues in combination with rituximab and did not include bendamustine-containing regimens. Zheng et al. [24] found that rituximab, in combination with either proteasome inhibitors or alkylating agents, yielded the best outcome, with overall response rates of 86% in both groups. A meta-analysis comparing first and second-generation BTKi in newly diagnosed and relapsed WM has also been performed, suggesting they are of similar efficacy but differ in their toxicity profiles [25]. A retrospective multi-centre comparison of treatment-naïve WM patients showed that BR resulted in improved response rates but not prolonged survival compared to ibrutinib [26]. These findings are concordant with our analysis.
Unlike previous studies, we did not include purine analogue-based therapy in our analysis as these regimens are not part of the first-line treatment recommendations by the IWWM [2]. We also did not include second-generation proteasome inhibitors or novel anti-CD20 antibodies such as ofatumumab and obinutuzumab for the same reason.
The identification of MYD88 and CXCR4 mutations has been shown to have prognostic and therapeutic implications, resulting in the latest IWWM recommendations that treatment (especially for BTKi) be adapted based on mutational status [2]. The majority of data supporting the impact of mutational status on therapeutic outcomes are in relapsed WM [27]. Results from ongoing studies are eagerly awaited in the first-line setting.
Although this would have provided valuable information for our analysis, we were unable to compare the efficacy of treatment regimens based on mutational status, as most trials did not report this data. It is interesting that the activity of the B-DRC, BR and IR regimens in treatment-naïve WM appears to be independent of MYD88/CXCR4 mutational status. The number of patients in the genomic analyses was however small, and the studies were not powered to answer this question [9, 13, 21]. Nevertheless, these results bring into question the role of MYD88 and CXCR4 mutations as biomarkers of response to therapy. Future studies stratifying patients by mutational subtype will be crucial to address this important question.
We were not able to compare the PFS in patients achieving a CR or VGPR with those achieving a PR as we do not have access to individual patient data from the trials. This would have been an interesting analysis to determine if the depth of response correlates with PFS. Another major limitation of our study, as it was with previous systematic reviews, is the heterogeneity among the existing trials, not just in terms of trial design but also with regard to the reporting of results. Key outcome measures such as PFS, time to next treatment and time to achievement of response were not consistently reported in the published studies, and those that are reported are limited by varying duration of follow-up. As a result, it was not possible to perform a quantitative meta-analysis of these outcome measures. We pooled the clinical trials based on treatment groups; heterogeneity was identified within most groups, likely due to variations in the trial design. Furthermore, the genomic subtypes (based on MYD88 and CXCR4 mutational status) of patients were not reported in several trials, resulting in heterogeneity among the patient characteristics in the studies that are included in this review.
The advanced age of the typical WM patient, as well as the chronic, incurable nature of the disease, means that quality of life (QOL) and treatment-related toxicities are very important considerations when making treatment decisions. Despite the availability of several objective measures of QOL [28], these were not consistently assessed in most studies and is a key area to improve on in future WM trials.
The rapidly expanding treatment arsenal for WM holds great promise for patients [29]. Novel BTKi such as acalabrutinib, zanubrutinib and tirabrutinib are showing promising results, and it remains to be seen how they compare to ibrutinib, especially in MYD88 L265P wild-type patients [30]. Recent RCTs suggest that the novel BTKi have a favourable toxicity profile (cardiac and gastrointestinal toxicity in particular) compared to ibrutinib, although their efficacy appears similar [31].
With regard to bortezomib-based regimens, the incidence of neuropathy is an important consideration, given that even mild grade 1 neuropathies are chronic and often impair QOL. Second-generation proteasome inhibitors (carfilzomib, ixazomib) [32] are emerging as highly effective, neuropathy-sparing agents and will be an important consideration for the future. It is also noteworthy that lenalidomide [33] and everolimus [34] have been shown in small studies to be effective, while the results of ongoing studies are awaited. BCL2 inhibition using venetolcax is under active investigation for WM [35] and is likely to play an important role in the treatment of WM in the near future. The inclusion of these agents as monotherapy or in combination with anti-CD20 monoclonal antibodies in future trials promises interesting results that could change practice.
In conclusion, evidence from this review suggests that BR yields higher response rates compared to the other first-line treatment options recommended by the IWWM. Given the efficacy and favourable toxicity profile of the novel BTKi, these may also be considerations for front-line therapy in the near future. The future of WM treatment is however likely to involve a genomically stratified treatment approach. Collaborative, international clinical trials comparing BR against other front-line treatment options in patients stratified by MYD88 and CXCR4 mutational status are called for to definitively identify the optimal first-line treatment for WM.
Data availability
Data may be shared upon reasonable request by contacting the corresponding author, Dr. Sanjay de Mel, at Sanjay_widanalage@nuhs.edu.sg.
References
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. Classification of tumours of haematopoietic and lymphoid tissues. Revised 4th ed. In: Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al., editors. Lyon: IARC; 2017.
Castillo JJ, Advani RH, Branagan AR, Buske C, Dimopoulos MA, D’Sa S, et al. Consensus treatment recommendations from the tenth International Workshop for Waldenström Macroglobulinaemia. Lancet Haematol. 2020;7:e827–e37.
Gertz MA. Waldenström macroglobulinemia treatment algorithm 2018. Blood Cancer J. 2018;8:40.
Ghobrial IM, Xie W, Padmanabhan S, Badros A, Rourke M, Leduc R, et al. Phase II trial of weekly bortezomib in combination with rituximab in untreated patients with Waldenstrom macroglobulinemia. Am J Hematol. 2010;85:670–4.
Agathocleous A, Rohatiner A, Rule S, Hunter H, Kerr JP, Neeson SM, et al. Weekly versus twice weekly bortezomib given in conjunction with rituximab, in patients with recurrent follicular lymphoma, mantle cell lymphoma and Waldenström macroglobulinaemia. Br J Haematol. 2010;151:346–53.
Treon SP, Ioakimidis L, Soumerai JD, Patterson CJ, Sheehy P, Nelson M, et al. Primary therapy of Waldenström macroglobulinemia with bortezomib, dexamethasone, and rituximab: WMCTG clinical trial 05-180. J Clin Oncol. 2009;27:3830–5.
Dimopoulos MA, García-Sanz R, Gavriatopoulou M, Morel P, Kyrtsonis MC, Michalis E, et al. Primary therapy of Waldenstrom macroglobulinemia (WM) with weekly bortezomib, low-dose dexamethasone, and rituximab (BDR): long-term results of a phase 2 study of the European Myeloma Network (EMN). Blood. 2013;122:3276–82.
Dimopoulos MA, Anagnostopoulos A, Kyrtsonis MC, Zervas K, Tsatalas C, Kokkinis G, et al. Primary treatment of Waldenstrom macroglobulinemia with dexamethasone, rituximab, and cyclophosphamide. J Clin Oncol. 2007;25:3344–9.
Buske C, Dimopoulos MA, Grunenberg A, Kastritis E, Tomowiak C, Mahé B, et al. Bortezomib-dexamethasone, rituximab, and cyclophosphamide as first-line treatment for Waldenström’s macroglobulinemia: a prospectively randomized trial of the European Consortium for Waldenström’s Macroglobulinemia. J Clin Oncol. 2023;41:2607–16.
Rummel MJ, Niederle N, Maschmeyer G, Banat GA, von Grünhagen U, Losem C, et al. Bendamustine plus rituximab versus CHOP plus rituximab as first-line treatment for patients with indolent and mantle-cell lymphomas: an open-label, multicentre, randomised, phase 3 non-inferiority trial. Lancet. 2013;381:1203–10.
Flinn IW, van der Jagt R, Kahl B, Wood P, Hawkins T, MacDonald D, et al. First-line treatment of patients with indolent non-Hodgkin lymphoma or mantle-cell lymphoma with bendamustine plus rituximab versus R-CHOP or R-CVP: results of the BRIGHT 5-year follow-up study. J Clin Oncol. 2019;37:984–91.
Luminari S, Goldaniga MC, Cesaretti M, Orsucci L, Tucci A, Pulsoni A, et al. Bendamustine and rituximab combination in untreated indolent non follicular B-cell non-Hodgkin’s lymphomas. A phase II study from the Fondazione Italiana Linfomi (INFL09). Blood. 2013;122:3049.
Dimopoulos MA, Tedeschi A, Trotman J, García-Sanz R, Macdonald D, Leblond V, et al. Phase 3 trial of ibrutinib plus rituximab in Waldenström’s macroglobulinemia. N Engl J Med. 2018;378:2399–410.
Gertz MA. Waldenström macroglobulinemia: 2021 update on diagnosis, risk stratification, and management. Am J Hematol. 2021;96:258–69.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Leblond V, Kastritis E, Advani R, Ansell SM, Buske C, Castillo JJ, et al. Treatment recommendations from the Eighth International Workshop on Waldenstrom’s Macroglobulinemia. Blood. 2016;128:1321–8.
Flinn I.W, Thompson D.S, Boccia R.V, Miletello G., Lipman A, Flora D, et al. Bendamustine, bortezomib and rituximab produces durable complete remissions in patients with previously untreated, low grade lymphoma. Br J Haematol. 2018;180:365–373.
Paludo J, Abeykoon JP, Kumar S, Shreders A, Ailawadhi S, Gertz MA, et al. Dexamethasone, rituximab and cyclophosphamide for relapsed and/or refractory and treatment-naïve patients with Waldenstrom macroglobulinemia. Br J Haematol. 2017;179:98–105.
Gavriatopoulou M, García-Sanz R, Kastritis E, Morel P, Kyrtsonis MC, Michalis E, et al. BDR in newly diagnosed patients with WM: final analysis of a phase 2 study after a minimum follow-up of 6 years. Blood. 2017;129:456–9.
Buske C, Tedeschi A, Trotman J, García-Sanz R, MacDonald D, Leblond V, et al. Ibrutinib plus rituximab versus placebo plus rituximab for Waldenström’s macroglobulinemia: final analysis from the randomized phase III iNNOVATE study. J Clin Oncol. 2022;40:52–62.
Laribi K, Poulain S, Willems L, Merabet F, Le Calloch R, Eveillard JR, et al. Bendamustine plus rituximab in newly-diagnosed Waldenström macroglobulinaemia patients. A study on behalf of the French Innovative Leukaemia Organization (FILO). Br J Haematol. 2019;186:146–9.
Santos-Lozano A, Morales-Gonzalez A, Sanchis-Gomar F, Cristi-Montero C, Fiuza-Luces C, Pareja-Galeano H, et al. Response rate to the treatment of Waldenström macroglobulinemia: a meta-analysis of the results of clinical trials. Crit Rev Oncol Hematol. 2016;105:118–26.
Khurshid Q, Dar AJ, Mirza MA, Ahmad ME, Jaan A, Aamir S, et al. A systemic review on efficacy of ibrutinib-based regimens for the treatment of Waldenstrom macroglobulinemia. Blood. 2020;136:8–9.
Zheng YH, Xu L, Cao C, Feng J, Tang HL, Shu MM, et al. Rituximab-based combination therapy in patients with Waldenström macroglobulinemia: a systematic review and meta-analysis. Onco Targets Ther. 2019;12:2751–66.
Abushukair H, Syaj S, Ababneh O, Qarqash A, Schinke C, Thanendrarajan S, et al. First- versus second-generation Bruton tyrosine kinase inhibitors in Waldenström’s macroglobulinemia: a systematic review and meta-analysis. Am J Hematol. 2022;97:942–50.
Abeykoon JP, Kumar S, Castillo JJ, D’Sa S, Kastritis E, Durot E, et al. Bendamustine rituximab (BR) versus ibrutinib (Ibr) as primary therapy for Waldenström macroglobulinemia (WM): an international collaborative study. J Clin Oncol. 2022;40:7566. (16_suppl)
Treon SP, Xu L, Hunter Z. MYD88 mutations and response to ibrutinib in Waldenström’s macroglobulinemia. N Engl J Med. 2015;373:584–6.
Marandino L, La Salvia A, Sonetto C, De Luca E, Pignataro D, Zichi C, et al. Deficiencies in health-related quality-of-life assessment and reporting: a systematic review of oncology randomized phase III trials published between 2012 and 2016. Ann Oncol. 2018;29:2288–95.
Treon SP, Xu L, Guerrera ML, Jimenez C, Hunter ZR, Liu X, et al. Genomic landscape of Waldenström macroglobulinemia and its impact on treatment strategies. J Clin Oncol. 2020;38:1198–208.
Ntanasis-Stathopoulos I, Gavriatopoulou M, Fotiou D, Dimopoulos MA. Current and novel BTK inhibitors in Waldenström’s macroglobulinemia. Ther Adv Hematol. 2021;12:2040620721989586.
Tam CS, Opat S, D’Sa S, Jurczak W, Lee HP, Cull G, et al. A randomized phase 3 trial of zanubrutinib vs ibrutinib in symptomatic Waldenström macroglobulinemia: the ASPEN study. Blood. 2020;136:2038–50.
Kastritis E, Dimopoulos MA. Proteasome inhibitors in Waldenström macroglobulinemia. Hematol Oncol Clin North Am. 2018;32:829–40.
Treon SP, Soumerai JD, Branagan AR, Hunter ZR, Patterson CJ, Ioakimidis L, et al. Lenalidomide and rituximab in Waldenstrom’s macroglobulinemia. Clin Cancer Res. 2009;15:355–60.
Ghobrial IM, Witzig TE, Gertz M, LaPlant B, Hayman S, Camoriano J, et al. Long-term results of the phase II trial of the oral mTOR inhibitor everolimus (RAD001) in relapsed or refractory Waldenstrom macroglobulinemia. Am J Hematol. 2014;89:237–42.
Castillo JJ, Allan JN, Siddiqi T, Advani RH, Meid K, Leventoff C, et al. Venetoclax in previously treated Waldenström macroglobulinemia. J Clin Oncol. 2022;40:63–71.
Flinn IW, van der Jagt R, Kahl BS, Wood P, Hawkins TE, Macdonald D, et al. Randomized trial of bendamustine-rituximab or R-CHOP/R-CVP in first-line treatment of indolent NHL or MCL: the BRIGHT study. Blood. 2014;123(19):2944–52.
Dimopoulos MA, Roussou M, Kastritis E, Hadjiharissi E, Kyrtsonis M-C, Symeonidis A, et al. Primary Treatment of Waldenstrom’s Macroglobulinemia with Dexamethasone, Rituximab and Cyclophosphamide (DRC): Final Analysis of a Phase II Study. Blood. 2012;120(21):438.
Funding
No funding support was received for the conduct of this study.
Author information
Authors and Affiliations
Contributions
SDM, ADJ and MS conceptualised the study. IJYW, WLC, VC, SDM and MS wrote the protocol. WLC and SDM screened for and selected the included articles. WLC extracted the data. MS performed the analysis. WLC, SDM and MS wrote the original draft of the manuscript. WJC, MP, EHLC, YLC, ADJ and JL reviewed the manuscript. All authors agree with the submitted work and acknowledge that no other authors meeting the authorship criteria have been left out. MS, WLC and SDM had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chan, WL., Chong, V.C.L., Wee, I.J.Y. et al. Efficacy and safety of front-line treatment regimens for Waldenstrom macroglobulinaemia: a systematic review and meta-analysis. Blood Cancer J. 13, 140 (2023). https://doi.org/10.1038/s41408-023-00916-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41408-023-00916-5