Abstract
Whether peripheral immunity prospectively influences brain health remains controversial. This study aims to investigate the longitudinal associations between peripheral immunity markers with incident brain disorders. A total of 161,968 eligible participants from the UK Biobank were included. We investigated the linear and non-linear effects of peripheral immunity markers including differential leukocytes counts, their derived ratios and C-reactive protein (CRP) on the risk of dementia, Parkinson’s disease (PD), stroke, schizophrenia, bipolar affective disorder (BPAD), major depressive disorder (MDD) and anxiety, using Cox proportional hazard models and restricted cubic spline models. Linear regression models were used to explore potential mechanisms driven by brain structures. During a median follow-up of 9.66 years, 16,241 participants developed brain disorders. Individuals with elevated innate immunity markers including neutrophils, monocytes, platelets, neutrophil-to-lymphocyte ratio (NLR), and systemic immune-inflammation index (SII) had an increased risk of brain disorders. Among these markers, neutrophils exhibited the most significant correlation with risk of dementia (hazard ratio 1.08, 95% confidence interval 1.04–1.12), stroke (HR 1.06, 95% CI 1.03–1.09), MDD (HR 1.13, 95% CI 1.10–1.16) and anxiety (HR 1.07, 95% CI 1.04–1.10). Subgroup analysis revealed age-specific and sex-specific associations between innate immunity markers with risk of dementia and MDD. Neuroimaging analysis highlighted the associations between peripheral immunity markers and alterations in multiple cortical, subcortical regions and white matter tracts, typically implicated in dementia and psychiatric disorders. These findings support the hypothesis that neuroinflammation is important to the etiology of various brain disorders, offering new insights into their potential therapeutic approaches.
Similar content being viewed by others
Introduction
Neurological and psychiatric disorders are a group of chronic diseases that often cause impaired cognition, motor function, emotional regulation, and tactile function [1]. These disorders include neurological conditions like dementia, PD and stroke, as well as psychiatric conditions such as schizophrenia, BPAD, MDD and anxiety. and are the leading causes of global mortality and disability [2]. Neurological and psychiatric disorders can be caused by external stresses and internal genetic factors. Multiple modifiable factors involving various aspects of life have been identified as essential for the prevention of brain disorders. These factors mainly encompass maintaining healthy lifestyle habits and management of risk factors, which includes regular exercise, normal social interactions, balanced nutrition, quality sleep, avoidance of toxins, alcohol, and smoking, as well as effectively managing medical risk factors such as hypertension, hyperlipidemia, and diabetes [1]. As such, unraveling the underlying risk factors may provide insights into disease mechanisms and find potential therapeutic targets.
The immune system has a critical role in brain homeostasis, resilience and brain reserve, and the interaction between the immune system and brain is garnering growing interest across a broad range of neurological and psychiatric disorders [3,4,5]. The peripheral immune system comprises innate and adaptive immune systems. The components of the innate immune response mainly include monocytes, macrophages, neutrophils, dendritic cells, mast cells, and natural killer cells [6, 7]. On the other hand, the adaptive immune response involves B cells and T cells [7]. An effective way to assess peripheral immunity is by analyzing differential leukocyte counts obtained from peripheral blood. Moreover, ratios of leukocyte counts, including NLR, platelet-to-lymphocyte ratio (PLR), LMR, and SII, have been proposed as more effective measures to assess the strength of peripheral immunity [8]. CRP is a classical acute-phase reactant protein from the pentraxin family. It can remain elevated in chronic inflammatory conditions, and thus could be regarded as a marker of peripheral immunity [9]. Emerging evidence has shown the association between peripheral immunity and risk of dementia [10,11,12,13,14,15], PD [16,17,18,19,20,21,22], stroke [23], as well as schizophrenia [24,25,26,27], BPAD [28,29,30], and MDD [31, 32]. However, most studies focus on the association between CRP and incident brain disorders, there is limited and inconsistent evidence concerning the association between differential leukocytes and incident brain disorders. Furthermore, previous studies have been limited by relatively small sample sizes, short durations of follow-up, or insufficient statistical power to identify clinically significant associations.
In this study, we conducted a comprehensive analysis using data from the UK Biobank (UKB), a large prospective cohort study. We chose nine peripheral immunity markers which could represent peripheral immune status and readily accessible from peripheral blood. We aimed to investigate the relationships between these markers and the risk of seven incident brain disorders, including dementia, PD, stroke, schizophrenia, BPAD, MDD, and anxiety.
Methods
Participants
UKB is a large-scale longitudinal cohort database containing in-depth genetic and health information of 502,493 participants aged 37–73 years at baseline assessments recruited from 22 centers throughout the UK during 2006–2010 (https://www.ukbiobank.ac.uk/). Data covering lifestyles and health conditions, physical measures, biological samples, imaging, and genotyping were obtained from interviews, questionnaires and measurements [33]. The baseline assessment was followed by consecutive long-term follow-up. The database is linked to national health datasets, including primary care, hospital inpatient, death, and cancer registration data [33]. Ethics approval for the UKB study was obtained from the North West Multicenter Research Ethical Committee. All participants provided written informed consent. The present study was conducted under UKB application number 19542. Participants with baseline diagnoses of the seven brain disorders, with a follow-up duration of less than five years or below 55 years, were excluded from our study. Additionally, we excluded individuals with conditions that could impact peripheral immunity markers, including malignant neoplasms, blood and blood-forming organ diseases, autoimmune diseases, and chronic inflammatory conditions. Finally, 161,968 participants were included in the primary analysis.
Peripheral immunity markers
Blood samples were analyzed at the UKB central laboratory within 24 h of the blood draw. Peripheral blood cell counts were obtained from an automated, clinically validated Coulter LH 750. Quality control was carried out according to the manufacturer’s recommendations. More details were available in the UK Biobank online showcase and protocol (http://www.ukbiobank.ac.uk). Thirty-one parameters were reported by the instrument (details available in https://biobank.ndph.ox.ac.uk/showcase/ukb/docs/ haematology.pdf). Baseline count data of neutrophils, monocytes, platelets, and lymphocytes were extracted. Next, we calculated four ratios based on peripheral blood cell counts, including NLR (neutrophils/lymphocytes), PLR (platelets/lymphocytes), SII (neutrophil×platelets/lymphocytes), and LMR (lymphocytes/monocytes). In addition, the serum CRP concentration was measured by immunoturbidimetric-high sensitivity analysis on Beckman Coulter AU5800 at baseline, ranging from 0.08 to 79.96 mg/L. Peripheral immunity markers with corresponding data fields are listed in Table S1 in Additional files 1.
Covariates
Relevant covariates were measured at baseline (corresponding field ID was presented in Table S1 in Additional files 1). Demographic variables included age (years), sex (male or female), and ethnicity (white or non-white). Education was categorized as higher (college/university degree or other professional qualification) or lower. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured twice at an interval time for 5 min or more using IntelliSense blood pressure monitor model HEM-907XL (Omron) [34]. We performed the test for multi-collinearity of covariates and variance inflation factor (VIF) < 10 indicated no multi-colinearities (Table S2 in Additional files 1).
Brain disorders
The outcomes included seven brain disorders, namely neurological disorders (dementia, PD, and stroke) and psychiatric disorders (schizophrenia, BPAD, MDD, and anxiety). The brain disorders were verified and classified according to the corresponding three-character ICD-10 codes, extracted from first occurrences of health outcomes (Category 1712). The health outcomes were generated from self-report conditions, primary care records, hospital inpatient data, and death records obtained from the National Health Service (NHS). The UK Biobank website [35] provides further details about the data processing and linkage procedures [35]. All-cause dementia encompassed codes F00, F01, F02, F03, and G30, PD was identified by code G20, stroke by codes I60-I69, MDD by codes F32 and F33, schizophrenia by code F20.9, BPAD by code F31 and anxiety by codes F40 and F41. Follow-up duration was calculated from the date of the initial assessment (Field 53) to the earliest date of any incident brain disorder diagnosis, date of death (Field 40000), or the last available date extracted from hospital inpatient data (Field 41280-41281) or recorded by the general practitioners (Field 42040), whichever came first.
Brain imaging data
Brain magnetic resonance imaging (MRI) data from over 40,000 participants in the UK Biobank was collected using a standardized protocol on a 3 T Siemens Skyra scanner with a 32-channel head coil. The T1-weighted images were processed by the UK Biobank imaging team using FSL software. Various imaging-derived phenotypes (IDPs) were generated, including cortical volume, area and thickness, subcortical volume, fractional anisotropy (FA) and mean diffusivity (MD) measures. We included participants with peripheral immunity and MRI data, and excluded those with major brain disorders. In total, 40068 participants were included. The volume, area and thickness of 68 cortical regions, volume of 45 subcortical regions, the FA and MD values of the 48 white matter tracts were analyzed to investigate the associations between brain structure and peripheral immunity markers. Further details of imaging processing and quality control can be found in the provided open-access article [36].
Statistical analysis
The results for continuous variables are shown as mean and standard deviation (SD) (normal distribution), while categorical variables are shown as number and percentage. To compare the effect sizes between various exposures, the peripheral immunity markers were log-transformed and standardized to Z scores (Z = (value − mean)/SD). Hence, the hazard ratio (HR) reflects the predicted effect of per SD increment of the peripheral immunity markers. We assessed longitudinal associations between various peripheral immunity markers and the risk of seven brain disorders with multivariable Cox proportional hazard regression models. The number of days between the baseline visit and dementia occurrence was calculated and utilized for Cox regression analysis. Covariates including age, sex, ethnicity, education, SBP and DBP were adjusted. The P values were further corrected by false-discovery rate (FDR) (labeled as Q values) to avoid the inflation of false-positive results. Restricted cubic spline (RCS) analysis was further performed to explore the potential non-linear relationships between peripheral immunity markers and the risk of various brain disorders. The spline models were adjusted with the same set of covariates as in the Cox model. To assess the robustness of our findings, we further performed two sensitivity analyses: (1) exclusion of participants with the extreme values (>mean ± 3 SD) of all exposures, (2) imputing missing values for all relevant exposures and covariates using CART, as implemented in the ‘mice’ package in R (single imputation, seed = 123). In subgroup analyses, we explored differences for each exposure based on age (55–65 years, ≥65 years) at baseline assessment and sex (male, female). Finally, multiple linear regression models were used to explore the associations between peripheral immunity markers and brain morphometric measures after adjusting for the aforementioned covariates. All analyses were carried out using R version 4.0.2.
Results
Population characteristics
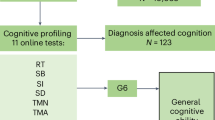
In this study, 161,968 participants were included, with an average age of 62.14 (SD = 4.07) years and 50.7% of them were women. A flow chart of study design was shown in Fig. 1. During a median follow-up of 9.66 years, 2958 individuals were diagnosed with dementia, 1193 with PD, 4815 with stroke, 51 with schizophrenia, 63 with BPAD, 3786 with MDD, and 4691 with anxiety. Table 1 presents the participants’ baseline demographic characteristics and peripheral immunity markers regarding brain health status. Compared to the control group, participants in the incident brain disorder group had characteristics such as older age, lower education levels, higher systolic blood pressure, and higher levels of innate immunity markers (Table 1).
Five hundred and two thousand four hundred and ninety-three participants aged 37–73 years were included for initial assessment, after excluding participants with baseline diagnoses of the seven brain disorders, with a follow-up duration of less than five years or below 55 years, with conditions that could impact peripheral immunity markers. Finally, 161,968 participants were included in the primary analysis.
Peripheral immunity markers and risk of brain disorders
We investigated the relationship between nine peripheral immunity markers and the incidence of seven brain disorders with the Cox model by adjusting for age at baseline, sex, ethnicity, education, SBP and DBP. Several markers, especially innate immunity markers, were associated with the risk of various brain disorders (Fig. 2).
The model was adjusted for age at baseline, sex, ethnicity, education, SBP and DBP. Exposures were log-transformed and standardized to Z score so that the HR represents the predicted effect of a one SD increment. Statistical significance at FDR-adjusted P (labeled as Q values) < 0.05. FDR, false discovery rate; HR hazard ratio, SD standard deviation, SBP systolic blood pressure, DBP diastolic blood pressure, PD Parkinson’s disease, MDD major depressive disorder, BPAD bipolar affective disorder.
In innate immunity category, higher neutrophils, the main element of innate immunity, were significantly associated with increased risk of incident dementia (HR 1.08, 95% CI: 1.04–1.12, p < 0.001), stroke (HR 1.06, 95% CI: 1.03–1.09, p < 0.001), MDD (HR, 1.13 95% CI: 1.10–1.16, p < 0.001), and anxiety (HR 1.07, 95% CI: 1.04–1.10, p < 0.001). In addition, a non-linear relationship was found between neutrophils and risk of incident dementia (p for non-linearity = 0.002; Fig. 3), stroke (p for non-linearity = 0.007; Fig. 3) and MDD (p for non-linearity = 0.014; Fig. 3). Elevated levels of NLR and SII, ratios of innate immunity to adaptive immunity, were observed to have similar results. Specifically, they were associated with an increased risk of dementia (HR 1.03, 95% CI: 1.01–1.05, p = 0.002 and HR 1.03, 95% CI: 1.01–1.05, p = 0.029, respectively), PD (HR 1.04, 95% CI: 1.02–1.06, p < 0.001 and HR 1.04, 95% CI: 1.01–1.06, p = 0.013, respectively), MDD (HR 1.03, 95% CI: 1.01–1.05, p = 0.002 and HR 1.04, 95% CI: 1.02–1.06, p < 0.001, respectively), and anxiety (HR 1.03, 95% CI: 1.01–1.04, p = 0.025 and HR 1.03, 95% CI: 1.01–1.05, p = 0.025, respectively). Additionally, the RCS model revealed a statistically significant non-linear relationship between NLR (p for non-linearity = 0.002, p for non-linearity < 0.001; Fig. 3) and SII (p for non-linearity = 0.024, p for non-linearity = 0.011; Fig. 3), with the risk of both dementia and PD. High monocyte count was found to be associated with an increased risk of stroke (HR 1.05, 95% CI: 1.03–1.07, p < 0.001), MDD (HR 1.04, 95% CI: 1.02–1.07, p < 0.001), and decreased risk of PD (HR 0.91, 95% CI: 0.85–0.98, p = 0.014). Levels of CRP were found to be associated with the risk of incident dementia (HR 0.95, 95% CI: 0.91–0.99, p = 0.029), stroke (HR 1.04, 95% CI: 1.01–1.07, p = 0.005) and MDD (HR 1.06, 95% CI: 1.03–1.08, p < 0.001). Moreover, a significant non-linear relationship between CRP and risk of dementia (p for non-linearity < 0.001; Fig. 3) and MDD (p for non-linearity = 0.001; Fig. 3) was observed. Low platelet count was associated with an increased risk of incident PD (HR 0.89, 95% CI: 0.84–0.95, p < 0.001), while higher platelet count was associated with an increased risk of incident MDD (HR 1.07, 95% CI: 1.04–1.10, p < 0.001).
Restricted cubic spline models fitted for Cox proportional hazards models was utilized, and 11 significant non-linear associations were identified. Two dashed vertical lines indicate 25% and 75% values of each exposure. Results were adjusted for age at baseline, sex, ethnicity, education, SBP and DBP. The colors blue, green, red, and purple represent each brain disorder fitting into PD, stroke, dementia, and MDD categories. HR hazard ratio, PD Parkinson’s disease, MDD major depressive disorder.
In the adaptive immunity category, increased adaptive immunity markers were associated with decreased risk of PD (HR 0.73, 95% CI: 0.66–0.82, p < 0.001 for lymphocytes and HR 0.78, 95% CI: 0.65–0.93, p = 0.013 for LMR) but increased risk of MDD (HR 1.03, 95% CI: 1.01–1.04, p < 0.001 for lymphocytes).
Sensitivity and subgroup analysis
Sensitivity analysis excluding the extreme values or imputing missing values did not significantly change the risk estimates. In subgroup analysis, HRs were generally in the same direction between peripheral immunity markers and multiple brain disorders (Table S3 in Additional files 1). In age-stratified subgroups, the associations between peripheral immunity markers and the risk of PD, stroke, anxiety, and BPAD incidence were consistent with the general population (Table S4 in Additional files 1). Interestingly, the association between peripheral immunity markers and MDD risk was significant only in participants aged 55 to 65, whereas the relationship between peripheral immunity markers and dementia risk was more pronounced in participants over 65 years (Table S4). In sex-stratified subgroups, the associations were generally more prominent in males than in females. Notably, significant associations were found between peripheral immunity markers and the risk of incident dementia exclusively in males (Table S5 in Additional files 1).
Association between peripheral immunity markers and brain structure
After FDR correction, results showed significant associations between innate immunity markers and multiple brain regions. Notably, neutrophils was associated with volumes of the insula (left hemisphere, P < 0.001, right hemisphere, P < 0.001), medial orbital frontal cortex (left hemisphere, P = 0.001, right hemisphere, P < 0.001), superior temporal gyrus (left hemisphere, P = 0.003, right hemisphere, P < 0.001), pars triangularis (left hemisphere, P < 0.001, right hemisphere, P = 0.022), precentral gyrus (left hemisphere, P < 0.001, right hemisphere, P < 0.006), posterior cingulate gyrus (left hemisphere, P = 0.034, right hemisphere, P = 0.001), as well as area and thickness of several cortical regions and multiple white matter tracts (Fig. 4; Tables S6–10 in Additional files 1).
Neutrophil (A), SII (B), platelet (C), NLR (D) are negatively associated with volume of cortical and subcortical structures (Bonferroni-corrected, P < 0.05). Models are adjusted for age at baseline, sex, ethnicity, education, SBP and DBP. T-value represents the correlation coefficient of the linear regression. SBP systolic blood pressure, DBP diastolic blood pressure, NLR neutrophils/lymphocytes ratio, SII systemic immune-inflammation index (neutrophils×platelets/lymphocytes).
Similarly, significant associations were identified between other innate immunity markers, including platelet, NLR and SII, with multiple cortical and subcortical regions implicated in dementia and psychiatric disorders (Fig. 4; Tables S8–10 in Additional files 1). In addition, these markers were observed to correlate with FA or MD values of white matter tracts, such as anterior corona radiate, anterior limb of internal capsule, cerebral peduncle, superior fronto-occipital fasciculus, and cingulum cingulate gyrus (Tables S6–7 in Additional files 1).
Discussion
Utilizing data from 161,968 participants in the UKB, we explored the associations between nine peripheral immunity markers and the risk of seven incident brain disorders. Our study yielded several noteworthy findings. Firstly, innate immunity markers including neutrophils, NLR, SII and CRP exhibited significant correlations with risk of various brain disorders, including dementia, PD, stroke, MDD, and anxiety. Secondly, multiple non-linear relationships were observed between peripheral immunity markers and incident brain disorders. Thirdly, subgroup analysis revealed that the relationship between peripheral immunity markers and risk of incident dementia is more pronounced in males and older individuals, whereas the relationship with the risk of incident MDD is more prominent among younger individuals. Lastly, neuroimaging analysis revealed the associations between peripheral immunity markers and alterations in multiple cortical, subcortical regions and white matter tracts, typically implicated in dementia and psychiatric disorders.
Our findings indicate that abnormal innate immunity is not specific to a particular disorder but could reflect an underlying pathological process that leads to brain dysfunction. The mechanisms by which innate immunity contributes to brain disorders are complicated. Under normal physiological conditions, leukocytes do not easily penetrate the blood-brain barrier (BBB) and are predominantly found near brain boundaries. On the flip side, peripheral cytokines can penetrate the brain via endothelial transporters, enabling them to impact brain functions by modulating neurotransmitters and neural activity [37]. In cases of chronic inflammation, the integrity of the BBB can be disrupted, facilitating the entry of circulating cytokines and leukocytes into the brain [38]. Evidence has shown that the peripheral neutrophils could release neutrophil extracellular traps (NETs) and contribute to the development and aggravation of lipopolysaccharide (LPS)-induced depressive behaviors in mice [39]. In transgenic models of AD, it has been observed that neutrophils extravasate from the bloodstream and accumulate in regions where amyloid-β (Aβ) deposits are present [40]. In individuals with AD, neutrophils have been observed to adhere to and intrude into brain venules and be present in the parenchyma [40]. Once peripheral inflammatory signals flow into the brain, microglia, the primary resident immune cells can be activated [41], thereby contributing to chronic neuroinflammation and neurodegeneration. Moreover, neutrophils also actively promote all stages of atherosclerosis by facilitating the recruitment of monocytes, activating macrophages, and exerting cytotoxic effects [42]. CRP could induce direct neuronal damage through pro-inflammatory responses [43], and act as a cardiovascular risk factor leading to the development of cerebral atherosclerosis [44, 45]. The gut-liver-brain axis has drawing much attention in exploring the association between peripheral immunity and brain disorders. Chronic gastrointestinal inflammation could lead to increased intestinal permeability, which is known as a leaky gut syndrome (LGS) [46]. The disruption of the intestinal barrier allows the leak of antigens from the digestive system into the bloodstream through the portal vein, subsequently activating liver immunity [47]. Meanwhile, systemic inflammation triggered by LGS could cause increased pro-inflammatory cytokines level, the excess of which is destructive to host cells, including cells of the CNS [48]. Peripheral immunity is also implicated in the relationship between psychosocial stress and neuropsychiatric diseases. There is now evidence that in experimental animals, different types of psychosocial stressors increase systemic and CNS levels of pro-inflammatory cytokines, including IL-1 and IL-6 [49, 50]. Moreover, in humans, psychosocial stress induced increase in pro-inflammatory cytokines coordinate stress-induced changes in peripheral blood immune cells, sparking inflammatory reactions and neurobehavioral changes [51, 52]. These may be the mechanistic explanations for the significant associations between innate immune dysfunction and the risk of various brain disorders, including dementia, stroke, depression and anxiety in our study.
As for neurodegenerative disorders, although many studies have identified changes in peripheral immunity markers in individuals with dementia [53,54,55,56,57,58], limited cohort studies have investigated the association between peripheral immunity markers and dementia incidence prospectively [10, 59, 60]. Several observational studies have evaluated the associations between plasma CRP levels and risk of dementia, and the results were inconclusive [12, 54, 61,62,63,64,65,66,67,68,69,70,71]. Our study, for the first time, investigated and discovered a non-linear relationship between CRP levels and incident dementia. Interestingly, contradictory results were yielded from Cox and RCS analysis regarding the association between CRP and risk of dementia. The reason may lie in the complex non-linear relationships between CRP levels and incident dementia, which cannot be captured adequately by a linear model. Consequently, the linear results may introduce errors, which could also be a contributing factor to the inconsistent findings observed in previous studies. A few studies reported the associations between alterations of neutrophils, lymphocytes, NLR, PLR, granulocyte-to-lymphocyte ratio (GLR), LMR, and SII with risk of dementia incidence [10, 59, 60]. Our results further corroborate previous findings. Remarkably, Our results also indicated pronounced sexual dimorphism. Importantly, neutrophils exhibit a statistically significant association with dementia in males (HR 1.10, p < 0.001) but not in females (HR 1.05, p = 0.249). Similarly, the NLR is significantly associated with dementia in males (HR 1.03, p = 0.001) but not in females (HR 1.01, p = 0.856). These observations suggest that immune system markers may play different roles in the pathogenesis of brain disorders between the sexes. Potential explanations may involve the influence of sex hormones on immune function. Estrogen is known to generally enhance immune responses, while testosterone exerts immunosuppressive effects [72]. These findings underscore the need to consider sex-specific responses in clinical risk assessment and potentially in the tailoring of therapeutic interventions. Regarding PD, three prospective studies examined the association between peripheral immunity markers and incident PD [16, 18, 73], our results showed consistency with two studies that reduced lymphocyte count was associated with an elevated risk of developing PD [16, 73]. Moreover, our research further extended the positive associations to platelet, NLR and LMR.
As for stroke, previous cross-sectional studies have investigated the association between peripheral immunity and stroke [74,75,76], but the prospective effect on stroke incidence has rarely been addressed. Only two studies explored the relationship between CRP and risk of stroke [23, 77]. Our results confirmed previous findings, and for the first time, provided evidence of associations between neutrophils and monocytes with risk of stroke incidence, which may offer new insights in the etiology and therapy of stroke.
As for psychiatric brain disorders, many cross-sectional studies showed an increased inflammatory response in individuals with MDD, anxiety, BPAD and schizophrenia [78,79,80,81]. Additionally, elevated CRP has been found to be correlated with increased depressive symptoms [81], symptom severity [82] and poorer treatment response in individuals with MDD [83, 84]. However, limited studies have reported associations between peripheral immunity markers and MDD incidence [32, 85]. Our study utilized more rigorous inclusion and exclusion criteria, such as excluding individuals with diseases that could potentially affect peripheral immune cells and excluding individuals with a follow-up period of less than 5 years, providing further confirmation of previous findings. Notably, this association was observed specifically in younger individuals, which may arise from variations in the inflammatory processes implicated in depression between younger adults and older adults [86, 87]. We did not observe any significant correlation between inflammatory factors and the risk of schizophrenia and bipolar disorder. Additional research is necessary to confirm these findings.
Since inflammation plays a prominent role in the development of different neuropsychiatric diseases, anti-inflammatory drugs are likely to improve symptoms. Evidence from recent meta-analyses suggests that adjunctive anti-inflammatory medication might be effective in the treatment of mood disorders [88, 89]. However, the results are inconsistent [90, 91]. Our findings provide evidence that early intervention on the systemic inflammation may be a promising therapy to reduce the risk of neuropsychiatric diseases.
Our study possesses several significant strengths. Firstly, we employed a longitudinal rather than cross-sectional approach to examine the relationships between nine peripheral immunity markers and the risk of seven prevalent neurological and psychiatric brain disorders. Secondly, brain imaging data in UKB offers us a chance to investigate the underlying mechanisms influenced by brain microstructural and macrostructural changes. Thirdly, our study benefits from substantial sample size and a prolonged follow-up duration, enhancing the statistical power and enabling us to capture long-term trends and outcomes. We also conducted a comprehensive assessment of various covariates, which allows for the control of potential confounding factors and strengthens the validity of our findings. Fourthly, our analysis using the RCS model identified crucial non-linear associations between immune markers and brain disorders that linear models did not capture. For instance, while the Cox regression analysis identified that higher neutrophil counts were linearly associated with an increased risk of incident dementia, stroke, and MDD, RCS allowed for the detection of non-linear trends in these associations (p for non-linearity = 0.002, 0.007, and 0.014, respectively). The U-shaped relationship observed between neutrophil counts and stroke or dementia indicates a potential optimal neutrophil count range, and deviations on either side could increase the risk for these disorders. Clinically, this could lead to the development of targeted therapies that aim to maintain neutrophil counts within a healthy range. Lastly, our findings gain credibility through the utilization of precise and validated diagnoses derived from hospital inpatient or primary care records. Our study has several limitations. Firstly, the sample of UKB was restricted to middle-aged and European ancestry participants, therefore the generalizability of our findings to broader populations may be limited. Secondly, potential confounding may still impact our findings even though we have performed extensive covariate correction. Thirdly, as an observational study, we cannot establish a causal relationship between peripheral immunity and the various brain disorders examined. Lastly, the assessment of peripheral immunity markers and confounding variables was only conducted at baseline, and we lack information on potential changes of these factors over time, which could have influenced our findings.
Conclusion
To date, our study stands out as the largest longitudinal study that comprehensively explores the association between peripheral immunity markers and incident brain disorders. The consistent findings of elevated innate immunity with increased risk of neurological and psychiatric disorders suggest that abnormal innate immunity is not specific to any particular brain disorder but may reflect a pathological process that leads to brain dysfunction. These findings support the hypothesis that neuroinflammation is important to the etiology of neurological and psychiatric disorders. More research is needed to further elucidate the specific neuroinflammatory mechanisms that give rise to specific disorders.
Availability of data and materials
The dataset supporting the conclusions of this article is available in the UK Biobank (https://biobank.ndph.ox.ac.uk/showcase/index.cgi) upon application.
References
Alchalabi T, Prather C. Brain health. Clin Geriatr Med. 2021;37:593–604.
WorldHealthOrganization. Optimizing brain health across the life course: WHO position paper. 2022. Available from: https://www.who.int/publications/i/item/9789240054561.
Furman D, Chang J, Lartigue L, Bolen CR, Haddad F, Gaudilliere B, et al. Expression of specific inflammasome gene modules stratifies older individuals into two extreme clinical and immunological states. Nat Med. 2017;23:174–84.
Bennett JM, Reeves G, Billman GE, Sturmberg JP. Inflammation-nature’s way to efficiently respond to all types of challenges: implications for understanding and managing “the Epidemic” of chronic diseases. Front Med (Lausanne). 2018;5:316.
Pape K, Tamouza R, Leboyer M, Zipp F. Immunoneuropsychiatry - novel perspectives on brain disorders. Nat Rev Neurol. 2019;15:317–28.
Heneka MT, Kummer MP, Latz E. Innate immune activation in neurodegenerative disease. Nat Rev Immunol. 2014;14:463–77.
Hemmer B, Kerschensteiner M, Korn T. Role of the innate and adaptive immune responses in the course of multiple sclerosis. Lancet Neurol. 2015;14:406–19.
Nost TH, Alcala K, Urbarova I, Byrne KS, Guida F, Sandanger TM, et al. Systemic inflammation markers and cancer incidence in the UK Biobank. Eur J Epidemiol. 2021;36:841–8.
Allin KH, Nordestgaard BG. Elevated C-reactive protein in the diagnosis, prognosis, and cause of cancer. Crit Rev Clin Lab Sci. 2011;48:155–70.
Zhang YR, Wang JJ, Chen SF, Wang HF, Li YZ, Ou YN, et al. Peripheral immunity is associated with the risk of incident dementia. Mol Psychiatry. 2022;27:1956–62.
Kim JW, Stewart R, Kang HJ, Bae KY, Kim SW, Shin IS, et al. Longitudinal associations between serum cytokine levels and dementia. Front Psychiatry. 2018;9:606.
Lewis NA, Knight JE. Longitudinal associations between C-reactive protein and cognitive performance in normative cognitive ageing and dementia. Age Ageing. 2021;50:2199–205.
Miwa K, Okazaki S, Sakaguchi M, Mochizuki H, Kitagawa K. Interleukin-6, interleukin-6 receptor gene variant, small-vessel disease and incident dementia. Eur J Neurol. 2016;23:656–63.
Higgins Tejera C, Ware EB, Hicken MT, Kobayashi LC, Wang H, Adkins-Jackson PB, et al. The mediating role of systemic inflammation and moderating role of race/ethnicity in racialized disparities in incident dementia: a decomposition analysis. medRxiv. 2023.
Baril AA, Beiser AS, Redline S, McGrath ER, Aparicio HJ, Gottlieb DJ, et al. Systemic inflammation as a moderator between sleep and incident dementia. Sleep. 2021;44:zsaa164.
Jensen MP, Jacobs BM, Dobson R, Bandres-Ciga S, Blauwendraat C, Schrag A, et al. Lower lymphocyte count is associated with increased risk of Parkinson’s disease. Ann Neurol. 2021;89:803–12.
Chen H, O’Reilly EJ, Schwarzschild MA, Ascherio A. Peripheral inflammatory biomarkers and risk of Parkinson’s disease. Am J Epidemiol. 2008;167:90–5.
Dommershuijsen LJ, Ruiter R, Erler NS, Rizopoulos D, Ikram MA, Ikram MK. Peripheral immune cell numbers and C-reactive protein in Parkinson’s disease: results from a population-based study. J Parkinsons Dis. 2022;12:667–78.
Bottigliengo D, Foco L, Seibler P, Klein C, Konig IR, Del Greco MF. A Mendelian randomization study investigating the causal role of inflammation on Parkinson’s disease. Brain. 2022;145:3444–53.
Phongpreecha T, Fernandez R, Mrdjen D, Culos A, Gajera CR, Wawro AM, et al. Single-cell peripheral immunoprofiling of Alzheimer’s and Parkinson’s diseases. Sci Adv. 2020;6:eabd5575.
Bartl M, Xylaki M, Bahr M, Weber S, Trenkwalder C, Mollenhauer B. Evidence for immune system alterations in peripheral biological fluids in Parkinson’s disease. Neurobiol Dis. 2022;170:105744.
Bartl M, Dakna M, Schade S, Otte B, Wicke T, Lang E, et al. Blood markers of inflammation, neurodegeneration, and cardiovascular risk in early Parkinson’s disease. Mov Disord: Off J Mov Disord Soc. 2023;38:68–81.
Karim MA, Kartsonaki C, Bennett DA, Millwood IY, Hill MR, Avery D, et al. Systemic inflammation is associated with incident stroke and heart disease in East Asians. Sci Rep. 2020;10:5605.
Campeau A, Mills RH, Stevens T, Rossitto LA, Meehan M, Dorrestein P, et al. Multi-omics of human plasma reveals molecular features of dysregulated inflammation and accelerated aging in schizophrenia. Mol Psychiatry. 2022;27:1217–25.
Notter T. Immunological processes in Schizophrenia pathology: potential biomarkers? Curr Top Behav Neurosci. 2018;40:389–410.
Trovao N, Prata J, VonDoellinger O, Santos S, Barbosa M, Coelho R. Peripheral biomarkers for first-episode psychosis-opportunities from the neuroinflammatory hypothesis of Schizophrenia. Psychiatry Investig. 2019;16:177–84.
Michel M, Schmidt MJ, Mirnics K. Immune system gene dysregulation in autism and schizophrenia. Dev Neurobiol. 2012;72:1277–87.
Sanchez-Autet M, Arranz B, Sierra P, Safont G, Garcia-Blanco A, de la Fuente L, et al. Association between neutrophil-lymphocyte ratio, platelet-lymphocyte ratio, and C-reactive protein levels and metabolic status in patients with a bipolar disorder. World J Biol Psychiatry. 2022;23:464–74.
Strawbridge R, Carter R, Saldarini F, Tsapekos D, Young AH. Inflammatory biomarkers and cognitive functioning in individuals with euthymic bipolar disorder: exploratory study. BJPsych Open. 2021;7:e126.
Queissner R, Pilz R, Dalkner N, Birner A, Bengesser SA, Platzer M, et al. The relationship between inflammatory state and quantity of affective episodes in bipolar disorder. Psychoneuroendocrinology. 2018;90:61–7.
Colasanto M, Madigan S, Korczak DJ. Depression and inflammation among children and adolescents: a meta-analysis. J Affect Disord. 2020;277:940–8.
Wainberg M, Kloiber S, Diniz B, McIntyre RS, Felsky D, Tripathy SJ. Clinical laboratory tests and five-year incidence of major depressive disorder: a prospective cohort study of 433,890 participants from the UK Biobank. Transl Psychiatry. 2021;11:380.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779.
White WB, Anwar YA. Evaluation of the overall efficacy of the Omron office digital blood pressure HEM-907 monitor in adults. Blood Press Monit. 2001;6:107–10.
UK Biobank first occurrences outcomes. Available from: https://biobank.ndph.ox.ac.uk/ukb/ukb/docs/first_occurrences_outcomes.pdf.
Alfaro-Almagro F, Jenkinson M, Bangerter NK, Andersson JLR, Griffanti L, Douaud G, et al. Image processing and quality control for the first 10,000 brain imaging datasets from UK Biobank. Neuroimage. 2018;166:400–24.
Banks WA. Blood-brain barrier transport of cytokines: a mechanism for neuropathology. Curr Pharm Des. 2005;11:973–84.
Varatharaj A, Galea I. The blood-brain barrier in systemic inflammation. Brain Behav Immun. 2017;60:1–12.
Kong Y, He G, Zhang X, Li J. The role of neutrophil extracellular traps in lipopolysaccharide-induced depression-like behaviors in mice. Brain Sci. 2021;11:1514.
Zenaro E, Pietronigro E, Della Bianca V, Piacentino G, Marongiu L, Budui S, et al. Neutrophils promote Alzheimer’s disease-like pathology and cognitive decline via LFA-1 integrin. Nat Med. 2015;21:880–6.
Delpech JC, Madore C, Nadjar A, Joffre C, Wohleb ES, Laye S. Microglia in neuronal plasticity: influence of stress. Neuropharmacology. 2015;96:19–28.
Silvestre-Roig C, Braster Q, Ortega-Gomez A, Soehnlein O. Neutrophils as regulators of cardiovascular inflammation. Nat Rev Cardiol. 2020;17:327–40.
Pasceri V, Willerson JT, Yeh ET. Direct proinflammatory effect of C-reactive protein on human endothelial cells. Circulation. 2000;102:2165–8.
Cleland SJ, Sattar N, Petrie JR, Forouhi NG, Elliott HL, Connell JM. Endothelial dysfunction as a possible link between C-reactive protein levels and cardiovascular disease. Clin Sci (Lond, Engl: 1979). 2000;98:531–5.
Torzewski J, Torzewski M, Bowyer DE, Frohlich M, Koenig W, Waltenberger J, et al. C-reactive protein frequently colocalizes with the terminal complement complex in the intima of early atherosclerotic lesions of human coronary arteries. Arterioscler Thromb Vasc Biol. 1998;18:1386–92.
Fukui H. Increased intestinal permeability and decreased barrier function: does it really influence the risk of inflammation? Inflamm Intest Dis. 2016;1:135–45.
Brescia P, Rescigno M. The gut vascular barrier: a new player in the gut-liver-brain axis. Trends Mol Med. 2021;27:844–55.
Goralczyk-Binkowska A, Szmajda-Krygier D, Kozlowska E. The microbiota-gut-brain axis in psychiatric disorders. Int J Mol Sci. 2022;23:11245.
Kubera M, Symbirtsev A, Basta-Kaim A, Borycz J, Roman A, Papp M, et al. Effect of chronic treatment with imipramine on interleukin 1 and interleukin 2 production by splenocytes obtained from rats subjected to a chronic mild stress model of depression. Pol J Pharm. 1996;48:503–6.
Moller M, Du Preez JL, Viljoen FP, Berk M, Emsley R, Harvey BH. Social isolation rearing induces mitochondrial, immunological, neurochemical and behavioural deficits in rats, and is reversed by clozapine or N-acetyl cysteine. Brain Behav Immun. 2013;30:156–67.
Song C, Kenis G, van Gastel A, Bosmans E, Lin A, de Jong R, et al. Influence of psychological stress on immune-inflammatory variables in normal humans. Part II. Altered serum concentrations of natural anti-inflammatory agents and soluble membrane antigens of monocytes and T lymphocytes. Psychiatry Res. 1999;85:293–303.
Dobbin JP, Harth M, McCain GA, Martin RA, Cousin K. Cytokine production and lymphocyte transformation during stress. Brain Behav Immun. 1991;5:339–48.
Kuyumcu ME, Yesil Y, Ozturk ZA, Kizilarslanoglu C, Etgul S, Halil M, et al. The evaluation of neutrophil-lymphocyte ratio in Alzheimer’s disease. Dement Geriatr Cogn Disord. 2012;34:69–74.
Koyama A, O’Brien J, Weuve J, Blacker D, Metti AL, Yaffe K. The role of peripheral inflammatory markers in dementia and Alzheimer’s disease: a meta-analysis. J Gerontol A Biol Sci Med Sci. 2013;68:433–40.
Rembach A, Watt AD, Wilson WJ, Rainey-Smith S, Ellis KA, Rowe CC, et al. An increased neutrophil-lymphocyte ratio in Alzheimer’s disease is a function of age and is weakly correlated with neocortical amyloid accumulation. J Neuroimmunol. 2014;273:65–71.
Chen SH, Bu XL, Jin WS, Shen LL, Wang J, Zhuang ZQ, et al. Altered peripheral profile of blood cells in Alzheimer disease: a hospital-based case-control study. Med (Baltim). 2017;96:e6843.
Kalelioglu T, Yuruyen M, Gultekin G, Yavuzer H, Ozturk Y, Kurt M, et al. Neutrophil and platelet to lymphocyte ratios in people with subjective, mild cognitive impairment and early Alzheimer’s disease. Psychogeriatrics. 2017;17:506–8.
Kara SP, Altunan B, Unal A. Investigation of the peripheral inflammation (neutrophil-lymphocyte ratio) in two neurodegenerative diseases of the central nervous system. Neurol Sci. 2022;43:1799–807.
Ramos-Cejudo J, Johnson AD, Beiser A, Seshadri S, Salinas J, Berger JS, et al. The neutrophil to lymphocyte ratio is associated with the risk of subsequent dementia in the Framingham Heart Study. Front Aging Neurosci. 2021;13:773984.
van der Willik KD, Fani L, Rizopoulos D, Licher S, Fest J, Schagen SB, et al. Balance between innate versus adaptive immune system and the risk of dementia: a population-based cohort study. J Neuroinflamm. 2019;16:68.
Kravitz BA, Corrada MM, Kawas CH. Elevated C-reactive protein levels are associated with prevalent dementia in the oldest-old. Alzheimers Dement. 2009;5:318–23.
Schmidt R, Schmidt H, Curb JD, Masaki K, White LR, Launer LJ. Early inflammation and dementia: a 25-year follow-up of the Honolulu-Asia Aging Study. Ann Neurol. 2002;52:168–74.
Engelhart MJ, Geerlings MI, Meijer J, Kiliaan A, Ruitenberg A, van Swieten JC, et al. Inflammatory proteins in plasma and the risk of dementia: the rotterdam study. Arch Neurol. 2004;61:668–72.
Hsu PF, Pan WH, Yip BS, Chen RC, Cheng HM, Chuang SY. C-reactive protein predicts incidence of dementia in an Elderly Asian Community Cohort. J Am Med Dir Assoc. 2017;18:277.e7–e11.
Hegazy SH, Thomassen JQ, Rasmussen IJ, Nordestgaard BG, Tybjaerg-Hansen A, Frikke-Schmidt R. C-reactive protein levels and risk of dementia—observational and genetic studies of 111,242 individuals from the general population. Alzheimers Dement. 2022;18:2262–71.
Haan MN, Aiello AE, West NA, Jagust WJ. C-reactive protein and rate of dementia in carriers and non carriers of Apolipoprotein APOE4 genotype. Neurobiol Aging. 2008;29:1774–82.
Darweesh SKL, Wolters FJ, Ikram MA, de Wolf F, Bos D, Hofman A. Inflammatory markers and the risk of dementia and Alzheimer’s disease: a meta-analysis. Alzheimers Dement. 2018;14:1450–9.
van Oijen M, Witteman JC, Hofman A, Koudstaal PJ, Breteler MM. Fibrinogen is associated with an increased risk of Alzheimer disease and vascular dementia. Stroke. 2005;36:2637–41.
Ravaglia G, Forti P, Maioli F, Chiappelli M, Montesi F, Tumini E, et al. Blood inflammatory markers and risk of dementia: The Conselice Study of Brain Aging. Neurobiol Aging. 2007;28:1810–20.
Sundelof J, Kilander L, Helmersson J, Larsson A, Ronnemaa E, Degerman-Gunnarsson M, et al. Systemic inflammation and the risk of Alzheimer’s disease and dementia: a prospective population-based study. J Alzheimers Dis. 2009;18:79–87.
Eriksson UK, Pedersen NL, Reynolds CA, Hong MG, Prince JA, Gatz M, et al. Associations of gene sequence variation and serum levels of C-reactive protein and interleukin-6 with Alzheimer’s disease and dementia. J Alzheimers Dis. 2011;23:361–9.
Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16:626–38.
Yazdani S, Mariosa D, Hammar N, Andersson J, Ingre C, Walldius G, et al. Peripheral immune biomarkers and neurodegenerative diseases: a prospective cohort study with 20 years of follow-up. Ann Neurol. 2019;86:913–26.
Wang L, Song Q, Wang C, Wu S, Deng L, Li Y, et al. Neutrophil to lymphocyte ratio predicts poor outcomes after acute ischemic stroke: a cohort study and systematic review. J Neurol Sci. 2019;406:116445.
Zhang R, Wu X, Hu W, Zhao L, Zhao S, Zhang J, et al. Neutrophil-to-lymphocyte ratio predicts hemorrhagic transformation in ischemic stroke: a meta-analysis. Brain Behav. 2019;9:e01382.
Lux D, Alakbarzade V, Bridge L, Clark CN, Clarke B, Zhang L, et al. The association of neutrophil-lymphocyte ratio and lymphocyte-monocyte ratio with 3-month clinical outcome after mechanical thrombectomy following stroke. J Neuroinflamm. 2020;17:60.
Emerging Risk Factors C, Kaptoge S, Di Angelantonio E, Lowe G, Pepys MB, Thompson SG, et al. C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet. 2010;375:132–40.
Fernandes BS, Steiner J, Molendijk ML, Dodd S, Nardin P, Goncalves CA, et al. C-reactive protein concentrations across the mood spectrum in bipolar disorder: a systematic review and meta-analysis. Lancet Psychiat. 2016;3:1147–56.
Yuksel RN, Ertek IE, Dikmen AU, Goka E. High neutrophil-lymphocyte ratio in schizophrenia independent of infectious and metabolic parameters. Nord J Psychiat. 2018;72:336–40.
Ozdin S, Usta MB. A comparison of inflammatory markers in manic and euthymic states of bipolar disorder. Nord J Psychiatry. 2021;75:124–9.
Singh D, Guest PC, Dobrowolny H, Vasilevska V, Meyer-Lotz G, Bernstein HG, et al. Changes in leukocytes and CRP in different stages of major depression. J Neuroinflamm. 2022;19:74.
Jeenger J, Sharma M, Mathur DM, Amandeep. Associations of number and severity of depressive episodes with C-reactive protein and Interleukin-6. Asian J Psychiatr. 2017;27:71–5.
Raison CL, Pikalov A, Siu C, Tsai J, Koblan K, Loebel A. C-reactive protein and response to lurasidone in patients with bipolar depression. Brain Behav Immun. 2018;73:717–24.
Zhou J, Zhou J, Sun Z, Feng L, Feng Y, Xiao L, et al. The association of C-reactive protein with responses to escitalopram antidepressant treatment in patients with major depressive disorder. J Affect Disord. 2022;306:32–8.
Zainal NH, Newman MG. Increased inflammation predicts nine-year change in major depressive disorder diagnostic status. J Abnorm Psychol. 2021;130:829–40.
Copeland WE, Shanahan L, Worthman C, Angold A, Costello EJ. Cumulative depression episodes predict later C-reactive protein levels: a prospective analysis. Biol Psychiat. 2012;71:15–21.
Duivis HE, Kupper N, Vermunt JK, Penninx BW, Bosch NM, Riese H, et al. Depression trajectories, inflammation, and lifestyle factors in adolescence: the TRacking Adolescents’ Individual Lives Survey. Health Psychol. 2015;34:1047–57.
Rosenblat JD, Kakar R, Berk M, Kessing LV, Vinberg M, Baune BT, et al. Anti-inflammatory agents in the treatment of bipolar depression: a systematic review and meta-analysis. Bipolar Disord. 2016;18:89–101.
Husain MI, Strawbridge R, Stokes PR, Young AH. Anti-inflammatory treatments for mood disorders: systematic review and meta-analysis. J Psychopharmacol. 2017;31:1137–48.
Hellmann-Regen J, Clemens V, Grozinger M, Kornhuber J, Reif A, Prvulovic D, et al. Effect of minocycline on depressive symptoms in patients with treatment-resistant depression: a randomized clinical trial. JAMA Netw Open. 2022;5:e2230367.
Husain MI, Chaudhry IB, Khoso AB, Husain MO, Hodsoll J, Ansari MA, et al. Minocycline and celecoxib as adjunctive treatments for bipolar depression: a multicentre, factorial design randomised controlled trial. Lancet Psychiat. 2020;7:515–27.
Acknowledgements
The authors gratefully thank all the participants and professionals contributing to the UK Biobank. This study was supported by grants from the National Natural Science Foundation of China (grant number 82071201 to JTY, 81971032 to LT, 82071997 to WC), Shanghai Municipal Science and Technology Major Project (grant number 2018SHZDZX01 to JTY), Research Start-up Fund of Huashan Hospital (grant number 2022QD002 to JTY), Excellence 2025 Talent Cultivation Program at Fudan University (grant number 3030277001 to JTY), the Shanghai Rising-Star Program (grant number 21QA1408700 to WC), and ZHANGJIANG LAB, Tianqiao and Chrissy Chen Institute, the State Key Laboratory of Neurobiology and Frontiers Center for Brain Science of Ministry of Education, Fudan University, and Qingdao Municipal Medical Research Guidance Program (2020-WJZD081, 2021-WJZD078). The grant funding bodies had no roles in design, conduct or data analysis of the study, nor in manuscript preparation and approval.
Author information
Authors and Affiliations
Contributions
XLZ and YXQ: study concept and design, data processing, statistical analysis, interpretation of the results, and writing the manuscript; LW: critical revision of the manuscript, YRZ: study concept and design, statistical analysis, interpretation of the results, and critical revision of the manuscript. JQL: statistical analysis and interpretation of the results, JFF and WC: interpretation of the results, and critical revision of the manuscript; YJT and LT: study concept and design, interpretation of the results, and critical revision of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhong, X., Qiang, Y., Wang, L. et al. Peripheral immunity and risk of incident brain disorders: a prospective cohort study of 161,968 participants. Transl Psychiatry 13, 382 (2023). https://doi.org/10.1038/s41398-023-02683-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-023-02683-0