Abstract
N-methyl-D-aspartate receptor (NMDAR) hypofunction is hypothesised to underlie psychosis but this has not been tested early in illness. To address this, we studied 40 volunteers (21 patients with first-episode psychosis and 19 matched healthy controls) using PET imaging with an NMDAR selective ligand, [18F]GE-179, that binds to the ketamine binding site to index its distribution volume ratio (DVR) and volume of distribution (VT). Hippocampal DVR, but not VT, was significantly lower in patients relative to controls (p = 0.02, Cohen’s d = 0.81; p = 0.15, Cohen’s d = 0.49), and negatively associated with total (rho = −0.47, p = 0.04), depressive (rho = −0.67, p = 0.002), and general symptom severity (rho = −0.74, p < 0.001). Exploratory analyses found no significant differences in other brain regions (anterior cingulate cortex, thalamus, striatum and temporal cortex). These findings are consistent with the NMDAR hypofunction hypothesis and identify the hippocampus as a key locus for relative NMDAR hypofunction, although further studies should test specificity and causality.
Similar content being viewed by others
Introduction
Schizophrenia is a chronic mental illness with a lifetime prevalence of 1% [1]. It has been ranked the third most disabling illness worldwide [2]. Several lines of evidence indicate that the pathophysiology of schizophrenia and related psychotic disorders involves N-methyl-D-aspartate receptor (NMDAR) hypofunction [3,4,5,6,7]. This hypothesis was initially proposed in the 1990s [8, 9] on the basis of observations that ketamine and phencyclidine (PCP) induced the full range of schizophrenia-like symptoms (positive, negative and cognitive) when given to healthy participants; and evidence that these compounds worsen symptoms in patients with schizophrenia [10,11,12]. Ketamine and PCP show uncompetitive NMDAR antagonism through binding to an intrachannel binding site to block the active channel [13].
Genome-wide association studies have identified genetic variants related to the structure and function of the NMDAR that are associated with schizophrenia, including GRIN2A and serine racemase (SRR) [14]. Mice with reduced NMDAR expression display schizophrenia-like phenotypes [15,16,17]. There is also evidence from post-mortem studies that the NMDAR density is reduced in the hippocampus of humans with schizophrenia [18]. While these studies indicate the NMDAR is altered in schizophrenia, the only in vivo imaging study of the NMDAR in schizophrenia to date used [123I]CNS-1261, a single-photon emission tomography (SPECT) radioligand, selective for the intrachannel ketamine/PCP binding site [19, 20]. This study found a lower ratio of tracer binding in the left hippocampus to that in the whole brain in antipsychotic-free patients relative to healthy participants. Moreover, the hippocampal binding ratio was negatively correlated with total and negative symptom severity in antipsychotic-treated patients. However, as the study was conducted in chronic patients, it is unknown if NMDAR alterations are present early in the illness or if they may be secondary to the effects of illness chronicity.
In view of this, we investigated the in vivo availability of NMDAR in patients with first-episode psychosis (FEP). We hypothesized that patients would show lower NMDAR availability in the hippocampus relative to matched healthy controls; and that NMDAR availability would be negatively correlated with symptom severity. In addition, as NMDAR availability has been found to be reduced in patients with epilepsy receiving antidepressants for depressive symptoms [21], we tested whether there was an association between NMDAR availability and depressive symptom severity.
Methods
Ethics statement
Approval was obtained by the West London & GTAC Research Ethics Committee (REC reference: 16/LO/0130) and the Administration of Radioactive Substances Advisory Committee. Volunteers demonstrated capacity and provided written informed consent to participate. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines for case-control studies.
Participants
Data were collected from November 7, 2016 until August 2, 2019. Patients were recruited from FEP services in London, United Kingdom. Inclusion criteria were as follows: a diagnosis of a DSM-IV psychotic disorder according to the Structured Clinical Interview of DSM-IV-TR Axis I Disorders-Patient Edition [22], fulfilling criteria for having the first episode of psychosis [23], and less than 5 years’ illness duration. For comparison, a sample of healthy controls matched on age (+/−3 years) and sex were included. Inclusion criteria were as follows: no current or lifetime history of Axis I Disorder as determined by the Structural Clinical Interview of DSM-IV-TR Axis I Disorders-Patient Edition [22].
Exclusion criteria for all volunteers were as follows: history of significant head trauma (such as loss of consciousness >1 min or requiring hospital admission), dependence on illicit substances or alcohol, positive urine drug test (SureScreen Diagnostics, Derby, UK) for any illicit substances that might affect NMDAR (e.g. stimulants) on the day of scanning, medical comorbidity (other than minor illnesses), current use (no use within 3 months) of any of the following drugs which may interfere with NMDAR; antidepressants [21], mood stabilizers [24,25,26], benzodiazapines [27]; and contraindications to scanning (such as pregnancy) (see eMethods 1 in the Supplement for full exclusion criteria).
Medication status
Participants with psychosis were classified as antipsychotic-free if they had been free from antipsychotic treatment for at least 6 weeks for oral or 6 months for depot formulations [28]. Antipsychotic-naive was defined as having had no antipsychotic treatment at all.
In total n = 32 patients were screened for eligibility, n = 25 were deemed eligible, and n = 21 were included in the study. N = 36 healthy volunteers were screened for eligibility as controls, n = 34 were deemed eligible, and n = 19 were included in the study. Participants who were deemed eligible, but were not included in the study, withdrew following screening prior to scanning.
The final sample included n = 40 individuals, including n = 19 healthy controls and n = 21 patients (n = 12 antipsychotic-free and n = 9 treated with antipsychotics).
Measures
Clinical and demographic variables
Current age and illness duration were recorded. Clinical symptom severity was determined using the Positive and Negative Syndrome Scale (PANSS) [29]. Psychotropic medication histories were recorded, urine drug screens were performed, and equivalent chlorpromazine doses were calculated using the method reported by Leucht et al. [30].
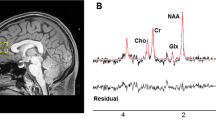
Neuroimaging
All participants underwent a dynamic, continuous 90-min simultaneous PET-MR acquisition after a bolus injection of [18F]GE-179 (mean [SD], 140.31 [9.04] MBq) with a Siemens 3T Biograph mMR PET/MR hybrid scanner (Siemens, Erlangen, Germany). In parallel to PET/MR imaging, continuous arterial sampling using an MR compatible blood sampler (http://www.swisstrace.ch/blood-sampler-twilite.html) was performed for the first 16 min followed by 6 discrete samples (see eMethods 2 in the Supplement for the full acquisition protocol). A T1-weighted structural Magnetization Prepared Rapid Gradient-Echo (MP-RAGE) image was acquired for co-registration (see eMethods 3 in the Supplement for the sequences). At the end of the session, a separate low dose CT scan (140 kV, 10 mA, helical acquisition) of the subject’s head was acquired on a GE Discovery DST 710 PET/CT (GE Healthcare, Chicago, Illinois, USA), and used for tissue attenuation correction during the PET image reconstruction. This additional CT scan was required because, at the time of the study starting, MRI based methods for attenuation correction had not been validated.
The person conducting the image analysis was blinded to the group status of the volunteers. NMDAR availability was determined as the [18F]GE-179 volume of distribution (VT, mL/cm3) calculated using the standard 2-tissue compartmental modelling method with a metabolite-corrected arterial plasma input function, consistent with previous [18F]GE-179 brain PET studies [31] (see eMethods 4–9 in the Supplement for more information on PET image analysis and model validation). Prior to kinetic modelling, all the individual PET data underwent the same image processing pipeline to measure and correct for subject motion, segment brain tissues and extract [18F]GE-179 tracer activity in the main regions of interest. For comparison with previous results [19], PET analysis was performed using the distribution volume ratio (DVR), calculated for the aforementioned regions as follows: region of interest VT/VT. The hippocampus was the primary region of interest given the prior findings of Pilowsky et al. [19] and evidence implicating it in the pathophysiology of psychotic and cognitive symptoms [18, 32, 33]. Exploratory analyses were conducted in the following additional ROIs: the anterior cingulate cortex (ACC), thalamus, striatum, and temporal lobe. These regions were chosen because prior studies have shown that patients with schizophrenia show glutamatergic dysfunction in these regions [18, 34]. Further exploratory analyses were completed to compare hippocampal DVR and VT across subgroups (antipsychotic-free patients, antipsychotic-treated patients and healthy controls). To determine if volumetric group differences influenced our findings, hippocampal volumes were compared across groups (eMethod 7).
Exploratory voxel-wise analyses were also conducted to determine if there were alterations in brain regions outside of the regions of interest using [18F]GE-179 VT parametric maps derived using the Logan graphical approach [35]. The main outputs from the image analysis were manually quality controlled (QC) by an experienced PET modeller (MV), blinded to subject status (for full description see eMethods 4 PET image analysis in the Supplement). Participants were excluded on the basis that there were still obvious artefacts on the motion corrected images and TACs (e.g. frame misalignment and signal drops in particular frames (for full description see eMethods 4 PET image analysis in the Supplement). Scans which failed QC were not included in the statistical analysis.
Statistical analysis
Statistical Product and Service Solutions (SPSS) version 22 (IBM Corp) was used for all statistical analyses and the significance level was set to p < 0.05 (two-tailed). Data normality was assessed using the Shapiro–Wilk test. Categorical clinical, demographics, and experimental variables were compared across groups using χ2 tests; and continuous variables were assessed using independent samples t-tests and Mann–Whitney tests for parametric and non-parametric data, respectively.
To determine whether hippocampal tracer uptake was lower in patients as compared to controls, an independent samples t-test was used. Mann–Whitney tests were used to analyze DVR data as they were non-normally distributed. To explore if there were effects in other regions, independent t-tests and Mann–Whitney tests were again used to identify if other areas known to be involved in schizophrenia had different tracer uptake. Independent t-tests and Mann–Whitney tests were also used for exploratory analyses to compare hippocampal DVR and VT across subgroups (antipsychotic-free patients, antipsychotic-treated patients and healthy controls) and to compare hippocampal volumes between the patient and healthy control groups. None of the exploratory analyses (additional ROIs or patient subgroup analyses) were corrected for multiple comparisons as they were exploratory. Effect sizes were summarised as Cohen’s d, and calculated using the difference in means between groups and the pooled standard deviation of the patient and control groups. The coefficient of variation was calculated for the VT and DVR of the hippocampus and other exploratory regions, in both patient and control groups, by calculating the ratio of the standard deviation to the mean (see eTable 1).
To investigate our hypothesis that tracer uptake was negatively associated with symptom severity, Pearson’s or Spearman’s correlation coefficients were calculated for normally and non-normally distributed data respectively, including PANSS total symptom severity as the independent variable, and tracer DVR or VT as the dependent variables. We also performed secondary analyses to explore if there were relationships with the general, positive, and negative subscales, using Bonferroni corrections to adjust for multiple comparisons in these exploratory analyses. We used the same approach to test our exploratory hypothesis that NMDAR availability would be negatively associated with depressive symptoms, using the score on the depressive item of the PANSS. Spearman’s correlation coefficients were calculated to determine if there were associations between hippocampal DVR and antipsychotic dose and hippocampal volume [36]. To further determine whether volume effects affected the results we performed a one-way ANOVA with hippocampal DVR as the dependent variable and group (patient or control) as the independent variables with hippocampal volume as the covariate.
Results
Demographics and experimental variables
A total of n = 40 individuals participated in the study, including n = 19 healthy controls and n = 21 patients (n = 12 antipsychotic-free and n = 9 treated with antipsychotics). One healthy control was excluded due to a malfunction of the arterial line, and two patients were excluded due to a positive urine test for cocaine (n = 1), or QC failure (n = 1). A total of n = 37 individuals (n = 18 healthy controls and n = 19 patients, of whom n = 11 were antipsychotic-free) were included in the final analysis.
No significant group differences were found for age (t35 = 0.93, p = 0.36) (Table 1), hippocampal, or whole-brain tissue volume (see eTable 1 and eResults 1 in the Supplement), cumulative movement, input function, injected mass, injected activity, or molar activity (see eTable 2 in the Supplement).
Tracer uptake in hippocampus
The hippocampal DVR data were not normally distributed (p < 0.03). Hippocampal DVR was significantly lower in the patient sample (Mean Rank = 14.84) compared to healthy controls (Mean Rank = 23.39; Mann–Witney test: U = 92.00; z = −2.40, p = 0.02; Cohen’s d = 0.81; Fig. 1). The coefficients of variation in hippocampal DVR for the patient and control groups were 7.5% and 7.1%, respectively. We conducted sensitivity analyses to determine if hippocampal volume could influence our findings. These showed that there was no correlation between hippocampal volume and hippocampal DVR (rho −0.14, p = 0.4), and there was still a significant effect of group on hippocampal DVR when hippocampal volume was included as a covariate (F(1,34) = 5.8, p = 0.02).
NMDAR availability measured by positron emission tomographic (PET) imaging was significantly lower in the hippocampus in patients with first-episode psychosis when DVR was measured (A) but not when VT was measured (B). Data are expressed as mean (SD) of the distribution volume ratio (DVR) (A) and distribution volume (VT) (B) of [18F]GE-179.
When antipsychotic-free patients were compared with healthy controls, there was no significant difference in hippocampal DVR (Mann–Witney test: U = 68.00; z = −1.39 p = 0.17; eFigure 1 in Supplementary Material). However, hippocampal DVR was significantly lower in the patient group taking antipsychotics relative to healthy controls Mann–Witney test: U = 24.00; z = −2.67, p = 0.006; eFigure 1 in Supplementary Material). There was no significant difference between antipsychotic-free and treated patient groups (Mann–Witney test: U = 24.00; z = −1.65 p = 0.10; eFigure 1 in Supplementary Material). Furthermore, there was no significant correlation between antipsychotic dose and hippocampal DVR (rho = −0.16, p = 0.71).
Volume of distribution data were normally distributed (p = 0.63). While in absolute terms hippocampal VT was lower in the patient group (Cohen’s d = 0.49), there was no statistically significant effect of group on VT in the hippocampus (t35 = 1.49, p = 0.15; Fig. 1). The coefficients of variation in VT for the patient and control groups were 22.7% and 18.2%, respectively. There were no significant differences in the comparisons between patients subgrouped on the basis of antipsychotic treatment and controls (antipsychotic-free vs healthy controls (t27 = −0.75, p = 0.46; eFigure 2 in Supplementary Material), antipsychotic-treated vs healthy controls (t24 = −1.94, p = 0.06; eFigure 2 in Supplementary Material), antipsychotic-free vs antipsychotic-treated (t17 = 0.94, p = 0.36; eFigure 2 in Supplementary Material).
Tracer uptake in additional brain areas and whole brain
Figure 2 shows mean parametric maps of VT of [18F]GE-179 for controls and patients, showing widespread uptake of the tracer throughout grey matter, in line with the expected distribution of NMDAR [31]. There was no significant effect of group on VT or DVR of [18F]GE-179 when investigated in the exploratory ROIs (the ACC, thalamus, striatum or temporal lobe; see eTable 1 and eResults 2 in the Supplement). Similarly, the voxel-wise analysis did not identify significant group differences in the VT of [18F]GE-179 in the hippocampus or other brain regions between patients and controls (see eResults 3 in the Supplement). There was no significant effect of group on VT in the whole brain (t35 = 0.60, p = 0.56, Cohen’s d = 0.20).
NMDAR availability and symptoms
There was a significant negative association between PANSS total symptom severity and hippocampal DVR (rho = −0.47, p = 0.04; Fig. 3). In addition, there was a significant negative association between hippocampal DVR and PANSS general symptom severity (rho = −0.74, p < 0.001; Fig. 4), but not with positive (rho = −0.41, p = 0.08), or negative (rho = 0.35, p = 0.14) symptom severity. Hippocampal DVR was also negatively associated with the depression item of the PANSS scale (rho = −0.67, p = 0.002; Fig. 5). The negative correlation between both general symptom severity and depression item with hippocampal DVR survived Bonferroni correction (αcorrected = 0.05/5 = 0.01).
The association between hippocampal VT, and PANSS scores, was assessed using Pearson’s correlation. The relationship between VT and total PANSS was not significant (r = −0.43, p = 0.06; eFigure 3 in Supplementary Material), along with positive PANSS (r = −0.30, p = 0.21), and negative PANSS (r = 0.08, p = 0.76). However, there was a significant negative correlation between hippocampal VT and general PANSS (r = −0.53, p = 0.02, eFigure 4 in Supplementary Material), and the depression item of the PANSS (r = −0.56, p = 0.01, eFigure5 in Supplementary Material).
Discussion
We found a significantly lower DVR of the NMDAR selective radiotracer, [18F]GE-179, in the hippocampus in patients with schizophrenia compared to healthy controls. In absolute terms, the hippocampal VT values of [18F]GE-179 were also lower in schizophrenia compared to controls, but this difference was not statistically significant. VT values showed more than double the variability seen with DVR (coefficients of variation for the hippocampus in healthy controls were 18.2% and 7.1%, respectively). Thus, the greater noise in the VT measure may have contributed to the lack of a significant difference in this measure in the hippocampus compared to the DVR.
This is the first in vivo study using an NMDAR selective radiotracer in patients with first-episode schizophrenia and builds upon the one previous in vivo study of NMDAR availability that used a SPECT tracer in older patients with chronic schizophrenia (illness duration mean (S.D) = 15.23 (9.21) years) [19]. In keeping with the present findings, they found a significant reduction in the DVR of [123I]CNS-1261 in the left hippocampus relative to the whole brain in medication-free patients (n = 5) compared to healthy controls. Our study findings are consistent with these, and, importantly, extend them to first-episode patients, indicating that alterations in NMDAR availability in the hippocampus are evident early in the development of the disorder. However, similar to our study, the SPECT study did not find a difference in NMDAR availability as measured by the VT in patients relative to healthy controls, although they did report a global reduction in [123I]CNS-1261 VT in patients treated with clozapine (n = 9) [20].
Our findings are also consistent with post-mortem data which provide evidence for lower hippocampal availability of NMDAR in patients with schizophrenia measured using MK801 binding [37], and lower hippocampal NR1 mRNA and protein levels in the hippocampus in schizophrenia patients relative to healthy controls [38]. As the NR1 subunits are essential components of the NMDAR, they can be used as a measure of NMDAR number more reliably than measurements of other subunits [39].
Strengths and limitations
A strength of our study is that the patients were predominantly antipsychotic-free FEP patients, and the sample size was more than double that of the SPECT study in chronic patients [19]. One important consideration is that the VT and DVR do not differentiate between specific and non-specific binding. As such, we cannot exclude the possibility that there was an alteration in non-specific binding contributing to the group differences in DVR. [18F]GE-179 has nanomolar affinity for the PCP site of the NMDAR ligand-gated ion channel and low affinity for other CNS receptors, indicating that its binding is likely to largely reflect NMDAR [40]. However, in vivo studies have been mixed. A study that used a blocking agent to investigate the specific binding of [18F]GE-179 in rodents and primates did not find evidence of specificity to NMDAR [41]. However, this study co-administered anaesthetic agents which may also alter the availability of the target sites, complicating interpretation of the findings as tracer binding could have been altered by anaesthetic agents used in the control group [41,42,43]. Notwithstanding this, a recent study found that electrical stimulation designed to activate NMDAR induced significant increases in the uptake of [18F]GE-179, and also that the NMDAR antagonist, ketamine, blocked this increase in uptake, indicating [18F]GE-179 binds to NMDAR and is sensitive to changes in NMDAR activity [44]. This provides evidence that the tracer we used is specific to the NMDAR, and sensitive to manipulations that activate NMDAR. However, it should be noted that in contrast to this study, in our study subjects were at rest. Future studies using activation paradigms or cognitive tasks would be useful to investigate the impact of receptor activation on specific binding in patients. There have also been studies in awake animals and humans using similar arylguanidine-based ligands to the one we used, such as CNS 5161 [45] and GMOM [46]. These studies have shown reductions in tracer uptake by NMDAR binding site antagonists. Using ketamine to block binding to the NMDAR, Van der Doef et al. reported a reduction in mean [11C]GMOM inhibitory constant (Ki) of 70% +/−12 in the hippocampus, indicating specific binding in vivo in the absence of the use of an NMDAR-modulating anaesthetic [46]. While these studies suggest that a large proportion of our signal is likely to be specific to the NMDAR, blocking studies in humans are required to determine how much of [18F]GE-179 tracer uptake is specific to the NMDAR in patients. However, this will be challenging because it would require giving patients a substantial dose of an NMDAR blocker such as ketamine, which can induce potent psychoactive effects in patients, which participants may find hard to tolerate while being scanned.
It is important to recognize that partial volume effects can potentially contribute to the lower hippocampal DVR values in patients. However, hippocampal and whole-brain volumes were not significantly different between the groups, and there was no correlation between hippocampal DVR and hippocampal volume; nor did our results change when hippocampal volume was added into the analysis as a covariate. These analyses suggest that volume effects are not a major factor in our finding of lower hippocampal DVR. There were also no significant differences in cumulative movement between patients and controls, indicating that partial volume effects or excess movement are unlikely to be major contributors to the group differences in DVR. It is possible that our findings were influenced by environmental risk factors for psychosis as we did not match our groups based on parental socio-economic status.
Interpretation and implications for understanding the pathophysiology of psychosis
As DVR is relative to tracer uptake in the brain, it is also possible that lower hippocampal DVR reflects greater uptake in other brain regions in schizophrenia. However, if this were the case then VT values would be higher in other brain regions in schizophrenia, which was not the case, and there is no consistent post-mortem evidence of globally increased NMDAR levels in schizophrenia [18]. Indeed, post-mortem studies in schizophrenia show lower brain levels of NMDAR in the hippocampus [18], cortex [47,48,49] and thalamus [50, 51] relative to controls. Thus, taken together with post-mortem findings of lower NMDAR levels [37, 38] the most parsimonious explanation for our findings is that first-episode patients with schizophrenia have lower hippocampal NMDAR density compared to healthy volunteers. However, as [18F]GE-179 binds to the NMDAR intrachannel phencyclidine binding site when the channel is open, another possibility is that a reduction in channel opening/receptor activity contributed to our results [21]. Recently, [18F]GE-179 has shown to have increased uptake following deep brain stimulation (DBS) of the hippocampus, without significant changes in cerebral blood flow, showing that the tracer is sensitive to a stimulus that leads to NMDAR activation [40]. Notwithstanding this, in either case the net result would be lower hippocampal NMDAR signalling, consistent with hypotheses that there is NMDA hypofunction in schizophrenia, which would be expected to alter excitation-inhibition balance to impair hippocampal function [52]. Our findings also add to other evidence for the involvement of the hippocampus in the pathophysiology of schizophrenia [53,54,55,56,57].
When we conducted exploratory subgroup analyses, we found that, there was no significant difference in hippocampal DVR between antipsychotic-free patients and healthy controls, although DVR was lower in absolute terms in patients. In contrast, the antipsychotic-treated patients had significantly lower hippocampal DVR compared to healthy controls. It should be recognized that these analyses are exploratory and the study was not designed or powered to detect differences in subgroups. Nevertheless, this could suggest either an effect of antipsychotic treatment on NMDAR or that patient subgroups show differences in NMDAR availability. The antipsychotics used by our patient group have very low affinities (Ki >1000 nM) for the tracer’s binding site on the NMDAR (the PCP binding site: Aripiprazole Ki >4000 nM, Olanzapine Ki >10,000 nM, Risperidone Ki >10,000 nM) [58] (https://pdsp.unc.edu/databases/kidb.php). There are no data on the Ki for Lurasidone on NMDAR but there is evidence that Lurasidone only has a weak affinity for NMDAR [59] and only one patient was treated with this. Furthermore, there was no correlation between antipsychotic dose and hippocampal DVR. Thus, it is unlikely that the results we see are due to the direct action of the medication on the receptor. All the patients treated with antipsychotics continued to be symptomatic despite adequate treatment perhaps suggesting a poor response to dopamine targeting medications. There is evidence that poor treatment responders have less significant abnormalities in their dopamine system and greater glutamate dysfunction [28, 60,61,62]. Our finding may, thus, suggest that NMDAR abnormalities are more marked in patients who show poor response to antipsychotic treatment. It would be useful to test this in a future study.
There was a negative association between hippocampal DVR and PANSS total symptoms, in agreement with prior findings in chronic patients treated with antipsychotic medication [19]. We found no significant associations with positive or negative subscales, in contrast to Pilowsky et al. who found a negative association with negative symptom severity. We cannot exclude the possibility that there is a weaker relationship with these symptoms. Nevertheless, this finding indicates that hippocampal NMDAR alterations may not be directly linked to psychotic symptoms, consistent with models that these arise from hyperdopaminergia [5, 63], albeit this may be secondary to NMDAR dysfunction in the hippocampus [64,65,66,67]. Preclinical models of psychosis suggest that hippocampal NMDAR hypofunction results in increased glutamatergic activity in pathways that project from the hippocampus to lead to increased mesostriatal dopaminergic activity, which is thought to result in psychosis [68, 69]. Interactions between the NMDAR and serotonin system may also contribute to psychosis [67].
It is also possible that glutamate dysfunction in other areas has a greater role in the induction of symptoms. There is evidence to suggest that glutamate levels in the ACC are related to greater severity of psychotic symptoms at first presentation [70]. Furthermore, a recent study found that thalamic glutamate levels in antipsychotic-naive patients were significantly negatively correlated with a percent change in symptoms after antipsychotic treatment [62].
The lack of a strong direct relationship between DVR and psychotic symptom severity may explain why it has proven challenging to develop antipsychotic medications targeting the NMDAR, such as glycine site modulators [71], inhibitors of glycine reuptake [72], positive allosteric modulation of NMDAR subunits [73], and other aspects of glutamatergic function for schizophrenia [73]. We found a significant inverse association between DVR and the general symptom subscale, which includes items covering cognitive symptoms. Preclinical studies show hippocampal NMDAR plays a key role in learning and memory [74, 75]. There is also evidence that NMDAR blockers, such as ketamine, induce cognitive impairments in patients with psychosis and healthy controls, and cognitive impairments are seen in chronic ketamine users [76,77,78,79]. Furthermore, there is evidence that patients with schizophrenia have impairments in cortical plasticity which can be improved with NMDAR enhancers such as D-serine [80]. These lines of evidence indicate that lower NMDAR could contribute to cognitive impairments in schizophrenia. However, further work is needed to determine if lower NMDAR availability is associated with cognitive impairments. Moreover, our exploratory analysis also demonstrated an inverse relationship between PANSS depressive symptom severity and hippocampal VT and DVR of [18F]GE-179, extending a prior finding that NMDAR tracer binding was globally reduced in patients with epilepsy who received treatment for depression [21], to show a direct association with depressive symptoms for the first time, as far as we are aware. This finding also adds to other evidence indicating a role for NMDAR in the pathophysiology of depressive symptoms, potentially more generally than just in schizophrenia. However, it is not clear how this fits with findings that treatment with NMDAR antagonist drugs, such as esketamine and ketamine, induces rapid antidepressant effects [81, 82]. A future study in patients with major depressive disorders would be useful to test this.
Conclusions
Our findings indicate that patients with first-episode psychosis show lower hippocampal NMDAR availability relative to other brain regions. This is consistent with patients showing either lower activity and/or density of NMDAR in the hippocampus relative to the whole brain; and the hypothesis that NMDA hypofunction in the hippocampus plays a key role in the pathophysiology of schizophrenia. Furthermore, we find that lower relative hippocampal NMDAR availability is associated with greater total symptom severity. Further studies are needed to determine the role of the NMDAR in the development of symptoms.
References
McCutcheon RA, Reis Marques T, Howes, OD. Schizophrenia—an overview. JAMA Psychiatry. 2020;77:201–10. https://doi.org/10.1001/jamapsychiatry.2019.3360.
Ustün TB, Rehm J, Chatterji S, Saxena S, Trotter R, Room R, et al. Multiple-informant ranking of the disabling effects of different health conditions in 14 countries. Lancet. 1999;354:111–5.
Howes O, McCutcheon R, Stone J. Glutamate and dopamine in schizophrenia: an update for the 21st century. J Psychopharmacol. 2015;29:97–115.
Coyle JT. The glutamatergic dysfunction hypothesis for schizophrenia. Harv Rev Psychiatry. 1996;3:241–53.
McCutcheon RA, Krystal JH, Howes OD. Dopamine and glutamate in schizophrenia: biology, symptoms and treatment. World Psychiatry. 2020;19:15–33.
Rotaru DC, Lewis DA, Gonzalez-Burgos G. The role of glutamatergic inputs onto parvalbumin-positive interneurons: relevance for schizophrenia. Rev Neurosci. 2012;23:97–109.
Lisman JE, Coyle JT, Green RW, Javitt DC, Benes FM, Heckers S, et al. Circuit-based framework for understanding neurotransmitter and risk gene interactions in schizophrenia. Trends Neurosci. 2008;31:234–42.
Olney JW, Farber NB. Glutamate receptor dysfunction and schizophrenia. Arch Gen Psychiatry. 1995;52:998.
Olney JW, Newcomer JW, Farber NB. NMDA receptor hypofunction model of schizophrenia. J Psychiatr Res. 1999;33:523–33.
Javitt DC, Zukin SR. Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry. 1991;148:1301–8.
Krystal JH, Perry EB,Jr, Gueorguieva R, Belger A, Madonick SH, Abi-Dargham A. et al. Comparative and interactive human psychopharmacologic effects of ketamine and amphetamine. Arch Gen Psychiatry. 2005;62:985–94.
Beck K, Hindley G, Borgan F, Ginestet C, McCutcheon R, Brugger S, et al. Association of ketamine with psychiatric symptoms and implications for its therapeutic use and for understanding schizophrenia: a systematic review and meta-analysis. JAMA Netw Open. 2020;3:e204693–e204693.
Zorumski CF, Izumi Y, Mennerick S. Ketamine: NMDA receptors and beyond. J Neurosci. 2016;36:11158–64.
Schizophrenia Working Group of the Psychiatric Genomics, C. Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511:421–7.
Belforte JE, Zsiros V, Sklar ER, Jiang Z, Yu G, Li Y, et al. Postnatal NMDA receptor ablation in corticolimbic interneurons confers schizophrenia-like phenotypes. Nat Neurosci. 2010;13:76–83.
Korotkova T, Fuchs EC, Ponomarenko A, von Engelhardt J, Monyer H. NMDA receptor ablation on parvalbumin-positive interneurons impairs hippocampal synchrony, spatial representations, and working memory. Neuron. 2010;68:557–69.
Moghaddam B, Krystal JH. Capturing the angel in “angel dust”: twenty years of translational neuroscience studies of NMDA receptor antagonists in animals and humans. Schizophr Bull. 2012;38:942–9.
Rubio MD, Drummond JB, Meador-Woodruff JH. Glutamate receptor abnormalities in schizophrenia: implications for innovative treatments. Biomol Ther. 2012;20:1–18.
Pilowsky LS, Bressan RA, Stone JM, Erlandsson K, Mulligan RS, Krystal JH, et al. First in vivo evidence of an NMDA receptor deficit in medication-free schizophrenic patients. Mol Psychiatry. 2006;11:118–9.
Bressan RA, Erlandsson K, Stone JM, Mulligan RS, Krystal JH, Ell PJ, et al. Impact of schizophrenia and chronic antipsychotic treatment on [123I]CNS-1261 binding to N-methyl-D-aspartate receptors in vivo. Biol Psychiatry. 2005;58:41–46.
McGinnity CJ, Koepp MJ, Hammers A, Riaño Barros DA, Pressler RM, Luthra S, et al. NMDA receptor binding in focal epilepsies. J Neurol Neurosurg Psychiatry. 2015;86:1150–7.
First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV-TR axis I disorders. New York State Psychiatric Institute; 2002.
Breitborde NJK, Srihari VH, Woods SW. Review of the operational definition for first-episode psychosis. Early Interv Psychiatry. 2009;3:259–65.
O'donnell T, Rotzinger S, Ulrich M, Hanstock CC, Nakashima TT, Silverstone PH. Effects of chronic lithium and sodium valproate on concentrations of brain amino acids. Eur Neuropsychopharmacol. 2003;13:220–7.
Zeise ML, Kasparow S, Zieglgänsberger W. Valproate suppresses N-methyl-d-aspartate-evoked, transient depolarizations in the rat neocortex in vitro. Brain Res. 1991;544:345–8.
Basselin M, Chang L, Bell JM, Rapoport SI. Chronic lithium chloride administration attenuates brain NMDA receptor-initiated signaling via arachidonic acid in unanesthetized rats. Neuropsychopharmacology. 2006;31:1659–74.
Van Sickle B, Cox A, Schak K, John Greenfield L, Tietz E. Chronic benzodiazepine administration alters hippocampal CA1 neuron excitability: NMDA receptor function and expression. Neuropharmacology. 2002;43:595–606.
Jauhar S, Veronese M, Nour MM, Rogdaki M, Hathway P, Turkheimer FE, et al. Determinants of treatment response in first-episode psychosis: an 18F-DOPA PET study. Mol Psychiatry. 2019;24:1502–12.
Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–76.
Leucht S, Samara M, Heres S, Patel MX, Woods SW, Davis JM. Dose equivalents for second-generation antipsychotics: the minimum effective dose method. Schizophr Bull. 2014;40:314–26.
McGinnity CJ, Hammers A, Riaño Barros DA, Luthra SK, Jones PA, Trigg W, et al. Initial evaluation of 18F-GE-179, a putative PET Tracer for activated N-methyl D-aspartate receptors. J Nucl Med. 2014;55:423–30.
Grace AA. Dysregulation of the dopamine system in the pathophysiology of schizophrenia and depression. Nat Rev Neurosci. 2016;17:524–32.
Bliss TVP, Collingridge GL. A synaptic model of memory: long-term potentiation in the hippocampus. Nature. 1993;361:31–39.
Merritt K, Egerton A, Kempton MJ, Taylor MJ, McGuire PK. Nature of glutamate alterations in schizophrenia. JAMA Psychiatry. 2016;73:665–74.
Logan J, Fowler JS, Volkow ND, Wolf AP, Dewey SL, Schlyer DJ. et al. Graphical analysis of reversible radioligand binding from time—activity measurements applied to [N-11C-methyl]-(−)-cocaine PET studies in human subjects. J Cereb Blood Flow Metab.1990;10:740–7.
Marques TR, Ashok AH, Angelescu I, Borgan F, Myers J, Lingford-Hughes A, et al. GABA-A receptor differences in schizophrenia: a positron emission tomography study using [11C]Ro154513. Mol Psychiatry. 2020;1–10. https://doi.org/10.1038/s41380-020-0711-y.
Beneyto M, Kristiansen LV, Oni-Orisan A, McCullumsmith RE, Meador-Woodruff JH. Abnormal glutamate receptor expression in the medial temporal lobe in schizophrenia and mood disorders. Neuropsychopharmacology. 2007;32:1888–902.
Vrajová M, Stastný F, Horácek J, Lochman J, Serý O, Peková S. et al. Expression of the hippocampal NMDA receptor GluN1 subunit and its splicing isoforms in schizophrenia: postmortem study. Neurochem Res.2010;35:994–1002.
Paoletti P, Neyton J. NMDA receptor subunits: function and pharmacology. Curr Opin Pharmacol. 2007;7:39–47.
Vibholm AK, Landau AM, Alstrup A, Jacobsen J, Vang K, Munk OL, et al. Activation of NMDA receptor ion channels by deep brain stimulation in the pig visualised with [18F]GE-179 PET. Brain Stimul. 2020;13:1071–8.
Schoenberger M, Schroeder FA, Placzek MS, Carter RL, Rosen BR, Hooker JM. et al. In vivo [18F]GE-179 brain signal does not show NMDA-specific modulation with drug challenges in rodents and nonhuman primates. ACS Chem Neurosci. 2018;9:298–305.
McGinnity CJ, Årstad E, Beck K, Brooks DJ, Coles JP, Duncan JS, et al. Comment on ‘In vivo [18F]GE-179 brain signal does not show NMDA-specific modulation with drug challenges in rodents and nonhuman primates’. ACS Chem Neurosci. 2019;10:768–72.
Sander CY, Schoenberger M, Hooker JM. Response to Comment on ‘In vivo [18F]GE-179 brain signal does not show NMDA-specific modulation with drug challenges in rodents and nonhuman primates’. ACS Chem Neurosci. 2019;10:773–5.
Vibholm AK, Landau AM, Møller A, Jacobsen J, Vang K, Munk OL, et al. NMDA receptor ion channel activation detected in vivo with [18F]GE-179 PET after electrical stimulation of rat hippocampus. J Cereb Blood Flow Metab. 2020;271678X20954928:1301–1312. https://doi.org/10.1177/0271678X20954928.
Biegon A, Gibbs A, Alvarado M, Ono M, Taylor S. In vitro and in vivo characterization of [3H]CNS-5161—a use-dependent ligand for the N-methyl-d-aspartate receptor in rat brain. Synapse. 2007;61:577–86.
Van Der Doef TF, Golla S, Klein PJ, Oropeza-Seguias GM, Schuit RC, Metaxas A, et al. Quantification of the novel N-methyl-d-aspartate receptor ligand [11 °C]GMOM in man. J Cereb Blood Flow Metab. 2016;36:1111–21.
Sokolov BP. Expression of NMDAR1, GluR1, GluR7, and KA1 glutamate receptor mRNAs is decreased in frontal cortex of “neuroleptic-free” schizophrenics: evidence on reversible up-regulation by typical neuroleptics. J Neurochem. 2002;71:2454–64.
Humphries C, Mortimer A, Hirsch S, de Belleroche J. NMDA receptor mRNA correlation with antemortem cognitive impairment in schizophrenia. Neuroreport. 1996;7:2051–5.
Beneyto M, Meador-Woodruff JH. Lamina-specific abnormalities of NMDA receptor-associated postsynaptic protein transcripts in the prefrontal cortex in schizophrenia and bipolar disorder. Neuropsychopharmacology. 2008;33:2175–86.
Ibrahim HM, Hogg AJ Jr, Healy DJ, Haroutunian V, Davis KL, Meador-Woodruff JH. Ionotropic glutamate receptor binding and subunit mRNA expression in thalamic nuclei in schizophrenia. Am J Psychiatry. 2000;157:1811–23.
Clinton SM, Haroutunian V, Davis KL, Meador-Woodruff JH. Altered transcript expression of NMDA receptor-associated postsynaptic proteins in the thalamus of subjects with schizophrenia. Am J Psychiatry. 2003;160:1100–9.
Kehrer C, Maziashvili N, Dugladze T, Gloveli T. Altered excitatory-inhibitory balance in the NMDA-hypofunction model of schizophrenia. Front Mol Neurosci. 2008;1:6.
Heckers S, Konradi C. Hippocampal pathology in schizophrenia. In: Swerdlow NR, editor. Behavioral neurobiology of schizophrenia and its treatment. Springer Berlin Heidelberg; 2010. p. 529–53. https://doi.org/10.1007/7854_2010_43.
Heckers S. Neuroimaging studies of the hippocampus in schizophrenia. Hippocampus. 2001;11:520–8.
Heckers S, Konradi C. GABAergic mechanisms of hippocampal hyperactivity in schizophrenia. Schizophr Res. 2015;167:4–11.
Heckers S, Konradi C. Hippocampal neurons in schizophrenia. J. Neural Transm. 2002;109:891–905.
Borgan F, Laurikainen H, Veronese M, Marques TR, Haaparanta-Solin M, Solin O, et al. In vivo availability of cannabinoid 1 receptor levels in patients with first-episode psychosis. JAMA Psychiatry. 2019;76:1074–84.
Kaar SJ, Natesan S, McCutcheon R, Howes OD. Antipsychotics: mechanisms underlying clinical response and side-effects and novel treatment approaches based on pathophysiology. Neuropharmacology. 2020;172:107704.
Ishibashi T, Horisawa T, Tokuda K, Ishiyama T, Ogasa M, Tagashira R, et al. Pharmacological profile of lurasidone, a novel antipsychotic agent with potent 5-hydroxytryptamine 7 (5-HT7) and 5-HT1A receptor activity. J Pharmacol Exp Ther. 2010;334:171–81.
Demjaha A, Egerton A, Murray RM, Kapur S, Howes OD, Stone JM, et al. Antipsychotic treatment resistance in schizophrenia associated with elevated glutamate levels but normal dopamine function. Biol Psychiatry. 2014;75:e11–e13.
Mouchlianitis E, Bloomfield MA, Law V, Beck K, Selvaraj S, Rasquinha N, et al. Treatment-resistant schizophrenia patients show elevated anterior cingulate cortex glutamate compared to treatment-responsive. Schizophr Bull. 2016;42:744–52.
Bojesen KB, Ebdrup BH, Jessen K, Sigvard A, Tangmose K, Edden R, et al. Treatment response after 6 and 26 weeks is related to baseline glutamate and GABA levels in antipsychotic-naïve patients with psychosis. Psychol Med. 2020;50:2182–93.
Glenthoj BY, Mackeprang T, Svarer C, Rasmussen H, Pinborg LH, Friberg L, et al. Frontal dopamine D 2/3 receptor binding in drug-naive first-episode schizophrenic patients correlates with positive psychotic symptoms and gender. Biol Psychiatry. 2006;60:621–9.
Grace AA. Phasic versus tonic dopamine release and the modulation of dopamine system responsivity: a hypothesis for the etiology of schizophrenia. Neuroscience. 1991;41:1–24.
Floresco SB, Todd CL, Grace AA. Glutamatergic afferents from the hippocampus to the nucleus accumbens regulate activity of ventral tegmental area dopamine neurons. J Neurosci. 2001;21:4915–22.
Lisman JE, Pi HJ, Zhang Y, Otmakhova NA. A thalamo-hippocampal-ventral tegmental area loop may produce the positive feedback that underlies the psychotic break in schizophrenia. Biol Psychiatry. 2010;68:17–24.
Kokkinou M, Irvine EE, Bonsall DR, Natesan S, Wells LA, Smith M, et al. Reproducing the dopamine pathophysiology of schizophrenia and approaches to ameliorate it: a translational imaging study with ketamine. Mol Psychiatry. 2020. https://doi.org/10.1038/s41380-020-0740-6.
Grace AA, Gomes FV. The circuitry of dopamine system regulation and its disruption in schizophrenia: insights into treatment and prevention. Schizophr Bull. 2019;45:148–57.
Modinos G, Allen P, Grace AA, McGuire P. Translating the MAM model of psychosis to humans. Trends Neurosci. 2015;38:129–38.
Egerton A, Broberg BV, Van Haren N, Merritt K, Barker GJ, Lythgoe DJ, et al. Response to initial antipsychotic treatment in first episode psychosis is related to anterior cingulate glutamate levels: a multicentre 1 H-MRS study (OPTiMiSE). Mol Psychiatry. 2018;23:2145–55.
Buchanan RW, Javitt DC, Marder SR, Schooler NR, Gold JM, McMahon RP, et al. The cognitive and negative symptoms in schizophrenia trial (CONSIST): the efficacy of glutamatergic agents for negative symptoms and cognitive impairments. Am J Psychiatry. 2007;164:1593–602.
Beck K, Javitt DC, Howes OD. Targeting glutamate to treat schizophrenia: lessons from recent clinical studies. Psychopharmacology. 2016;233:2425–8.
Goff DC. Drug development in schizophrenia. Curr Opin Psychiatry. 2015;28:207–15.
Morris RGM, Anderson E, Lynch GS, Baudry M. Selective impairment of learning and blockade of long-term potentiation by an N-methyl-D-aspartate receptor antagonist, AP5. Nature. 1986;319:774–6.
Martin SJ, Grimwood PD, Morris RGM. Synaptic plasticity and memory: an evaluation of the hypothesis. Annu Rev Neurosci. 2000;23:649–711.
Rowland LM, Astur RS, Jung RE, Bustillo JR, Lauriello J, Yeo RA. Selective cognitive impairments associated with NMDA receptor blockade in humans. Neuropsychopharmacology. 2005;30:633–9.
Newcomer JW, Farber NB, Jevtovic-Todorovic V, Selke G, Melson AK, Hershey T, et al. Ketamine-induced NMDA receptor hypofunction as a model of memory impairment and psychosis. Neuropsychopharmacology. 1999;20:106–18.
Cheng WJ, Chen CH, Chen CK, Huang MC, Pietrzak RH, Krystal JH, et al. Similar psychotic and cognitive profile between ketamine dependence with persistent psychosis and schizophrenia. Schizophr Res. 2018;199:313–8.
Malhotra AK, Pinals DA, Adler CM, Elman I, Clifton A, Pickar D, et al. Ketamine-induced exacerbation of psychotic symptoms and cognitive impairment in neuroleptic-free schizophrenics. Neuropsychopharmacology. 1997;17:141–50.
Kantrowitz JT, Epstein ML, Beggel O, Rohrig S, Lehrfeld JM, Revheim N, et al. Neurophysiological mechanisms of cortical plasticity impairments in schizophrenia and modulation by the NMDA receptor agonist D-serine. Brain. 2016;139:3281–95.
McGirr A, Berlim MT, Bond DJ, Fleck MP, Yatham LN, Lam RW. A systematic review and meta-analysis of randomized, double-blind, placebo-controlled trials of ketamine in the rapid treatment of major depressive episodes. Psychol Med. 2015;45:693–704.
Zanos P, Gould TD. Mechanisms of ketamine action as an antidepressant. Mol Psychiatry. 2018;23:801–11.
Acknowledgements
KB has received funding from the Royal College of Psychiatrists, Rosetrees Trust and Stoneygate Trust. MV is funded by the National Institute for Health Research Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London, and by the Wellcome Trust Digital Award 215747/Z/19/Z. CJM was supported by the Medical Research Council MR/N013042/1 and subsequently by the Wellcome Trust/Engineering and Physical Sciences Research Council (EPSRC) Centre for Medical Engineering WT 203148/Z/16/Z and the Engineering and Physical Sciences Research Council Centre for Doctoral Training in Medical Imaging EP/L015226/1. JD’s work was supported by the Wellcome/EPSRC Centre for Medical Engineering WT 203148/Z/16/Z. RM received funding from NIHR. NS was funded by a grant from the Medical Research Council, MR/K022733/1 (awarded to FT). TP’s work is supported by the NIHR and Maudsley Charity. TS’s work was funded by departmental funding Wellcome-EPSRC, Grant/Award Number: WT 203148/Z/16/Z. FT has received MRC funding MR/K022733/1. AH is funded by King’s College London. ODH has received funding from the Medical Research Council-UK no. MC_U120097115, Maudsley Charity no. 66, Brain and Behavior Research Foundation, and Wellcome Trust no. 094849/Z/10/Z grants to ODH and the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. This research was funded in whole, or in part, by the Wellcome Trust 094849/Z/10/Z. For the purpose of open access, the author has applied a CC BY public copyright licence to any Author Accepted Manuscript version arising from this submission. The views expressed are those of the author(s) and not necessarily those of H Lundbeck A/s, the NHS/NIHR or the Department of Health.
Author information
Authors and Affiliations
Contributions
Conceptualisation: KB and ODH. Data curation: KB. Formal analysis: KB, MV, BS, CJM, FB, JD, JS, AH and ODH. Funding acquisition: KB and ODH. Investigation: KB, AA, JD, RAD, SJK, NS, TP, SJ and TS. Project administration: KB, AA and ODH. Resources: KB, AH and ODH. Software: MV. Supervision: AH, FT and ODH. Validation: MV. Visualisation: KB, MV and AA. Writing – original draft: KB. Writing – review and editing: all authors.
Corresponding authors
Ethics declarations
Competing interests
KB, AA, BS, JD, NS, TS and FT declare no competing interests. MV has received consulting honoraria from GSK. CJM has received fees from GE Healthcare Ltd but neither he nor any of his family have ever been employed by the organisation; nor does he or any of his family have holdings/a financial stake in GE Healthcare Ltd. SK received travel expenses for a scientific meeting from Autifony Ltd. RM has received honoraria for lectures from Otsuka and is an investigator on research funded by Neurocrine.TP has received honoraria for lectures from Lundbeck, Otsuka, and Sunovion. In the last 3 years, JMS has been PI on research studies sponsored by Takeda and Protexin. He has received an honorarium from Janssen for attending an advisory board meeting. SJ has received honoraria for educational talks given for Sunovian. KCL has received honoraria for educational talks SJ has given for Lundbeck. SJ is Co PI on a drug trial for Alkermes. FB became an employee at COMPASS Pathways plc after completion of this work. This work is unrelated to COMPASS Pathways plc. AH has received honoraria or consultation fees from Imperial Innovations and is a shareholder in Imperial Innovations. ODH is a part-time employee of H Lundbeck A/s (obtained post after completion of this project) and has received investigator-initiated research funding from and/or participated in advisory/speaker meetings organised by Angellini, Autifony, Biogen, Boehringer-Ingelheim, Eli Lilly, Heptares, Global Medical Education, Invicro, Jansenn, Lundbeck, Neurocrine, Otsuka, Sunovion, Rand, Recordati, Roche and Viatris/Mylan. Neither Dr Howes or his family have holdings/a financial stake in any pharmaceutical company. Dr Howes has a patent for the use of dopaminergic imaging.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Beck, K., Arumuham, A., Veronese, M. et al. N-methyl-D-aspartate receptor availability in first-episode psychosis: a PET-MR brain imaging study. Transl Psychiatry 11, 425 (2021). https://doi.org/10.1038/s41398-021-01540-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-021-01540-2
This article is cited by
-
Schizophrenia: from neurochemistry to circuits, symptoms and treatments
Nature Reviews Neurology (2024)
-
Neuroimaging glutamatergic mechanisms differentiating antipsychotic treatment-response
Scientific Reports (2023)
-
Cognitive impairment in schizophrenia: aetiology, pathophysiology, and treatment
Molecular Psychiatry (2023)
-
Hippocampal circuit dysfunction in psychosis
Translational Psychiatry (2022)