Abstract
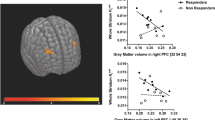
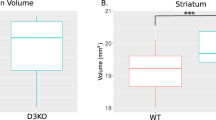
Dysregulation of dopamine systems has been considered a foundational driver of pathophysiological processes in schizophrenia, an illness characterized by diverse domains of symptomatology. Prior work observing elevated presynaptic dopamine synthesis capacity in some patient groups has not always identified consistent symptom correlates, and studies of affected individuals in medication-free states have been challenging to obtain. Here we report on two separate cohorts of individuals with schizophrenia spectrum illness who underwent blinded medication withdrawal and medication-free neuroimaging with [18F]-FDOPA PET to assess striatal dopamine synthesis capacity. Consistently in both cohorts, we found no significant differences between patient and matched, healthy comparison groups; however, we did identify and replicate robust inverse relationships between negative symptom severity and tracer-specific uptake widely throughout the striatum: [18F]-FDOPA specific uptake was lower in patients with a greater preponderance of negative symptoms. Complementary voxel-wise and region of interest analyses, both with and without partial volume correction, yielded consistent results. These data suggest that for some individuals, striatal hyperdopaminergia may not be a defining or enduring feature of primary psychotic illness. However, clinical differences across individuals may be significantly linked to variability in striatal dopaminergic tone. These findings call for further experimentation aimed at parsing the heterogeneity of dopaminergic systems function in schizophrenia.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Snyder SH, Banerjee SP, Yamamura HI, Greenberg D. Drugs, neurotransmitters, and schizophrenia. Science 1974;184:1243.
Masri B, Salahpour A, Didriksen M, Ghisi V, Beaulieu J-M, Gainetdinov RR, et al. Antagonism of dopamine D2 receptor/β-arrestin 2 interaction is a common property of clinically effective antipsychotics. Proc Natl Acad Sci USA. 2008;105:13656.
Lieberman JA, Kane JM, Alvir J. Provocative tests with psychostimulant drugs in schizophrenia. Psychopharmacology 1987;91:415–33.
Bertolino A, Breier A, Callicott JH, Adler C, Mattay VS, Shapiro M, et al. The relationship between dorsolateral prefrontal neuronal N-acetylaspartate and evoked release of striatal dopamine in schizophrenia. Neuropsychopharmacology 2000;22:125–32.
Abi-Dargham A, van de Giessen E, Slifstein M, Kegeles LS, Laruelle M. Baseline and amphetamine-stimulated dopamine activity are related in drug-naive schizophrenic subjects. Biol Psychiatry. 2009;65:1091–3.
Laruelle M, Abi-Dargham A, Gil R, Kegeles L, Innis R. Increased dopamine transmission in schizophrenia: Relationship to illness phases. Biol Psychiatry. 1999;46:56–72.
Abi-Dargham A, Gil R, Krystal J, Baldwin RM, Seibyl JP, Bowers M, et al. Increased striatal dopamine transmission in schizophrenia: Confirmation in a second cohort. Am J Psychiatry. 1998;155:761–7.
Breier A, Su TP, Saunders R, Carson RE, Kolachana BS, de Bartolomeis A, et al. Schizophrenia is associated with elevated amphetamine-induced synaptic dopamine concentrations: evidence from a novel positron emission tomography method. Proc Natl Acad Sci USA. 1997;94:2569–74.
Laruelle M, Abi-Dargham A, van Dyck CH, Gil R, D’Souza CD, Erdos J, et al. Single photon emission computerized tomography imaging of amphetamine-induced dopamine release in drug-free schizophrenic subjects. Proc Natl Acad Sci USA. 1996;93:9235–40.
Thompson JL, Urban N, Slifstein M, Xu X, Kegeles LS, Girgis RR, et al. Striatal dopamine release in schizophrenia comorbid with substance dependence. Mol Psychiatry. 2013;18:909–15.
Reith J, Benkelfat C, Sherwin A, Yasuhara Y, Kuwabara H, Andermann F, et al. Elevated dopa decarboxylase activity in living brain of patients with psychosis. Proc Natl Acad Sci USA. 1994;91:11651.
Hietala J, Syvälahti E, Kuoppamäki M, Hietala J, Syvälahti E, Haaparanta M, et al. Presynaptic dopamine function in striatum of neuroleptic-naive schizophrenic patients. Lancet. 1995;346:1130–1.
Lindström LH, Gefvert O, Hagberg G, Lundberg T, Bergström M, Hartvig P, et al. Increased dopamine synthesis rate in medial prefrontal cortex and striatum in schizophrenia indicated by L-(β-11C) DOPA and PET. Biol Psychiatry. 1999;46:681–8.
Hietala J, Syvälahti E, Vilkman H, Vuorio K, Räkköläinen V, Bergman J, et al. Depressive symptoms and presynaptic dopamine function in neuroleptic-naive schizophrenia. Schizophrenia Res. 1999;35:41–50.
Meyer-Lindenberg A, Miletich RS, Kohn PD, Esposito G, Carson RE, Quarantelli M, et al. Reduced prefrontal activity predicts exaggerated striatal dopaminergic function in schizophrenia. Nat Neurosci. 2002;5:267–71.
Gefvert O, Lindström LH, Waters N, Waters S, Carlsson A, Tedroff J. Different corticostriatal patterns of L-DOPA utilization in patients with untreated schizophrenia and patients treated with classical antipsychotics or clozapine. Scand J Psychol. 2003;44:289–92.
McGowan S, Lawrence AD, Sales T, Quested D, Grasby P. Presynaptic dopaminergic dysfunction in schizophrenia: A positron emission tomographic [18F]Fluorodopa study. Arch Gen Psychiatry. 2004;61:134–42.
Howes OD, Montgomery AJ, Asselin M-C, Murray RM, Valli I, Tabraham P, et al. Elevated striatal dopamine function linked to prodromal signs of schizophrenia. Arch Gen Psychiatry. 2009;66:13–20.
Nozaki S, Kato M, Takano H, Ito H, Takahashi H, Arakawa R. et al. Regional dopamine synthesis in patients with schizophrenia using L-[β-11C]DOPA PET. Schizophrenia Res.2009;108:78–84.
Dao-Castellana M-H, Paillère-Martinot M-L, Hantraye P, Attar-Lévy D, Rémy P, Crouzel C, et al. Presynaptic dopaminergic function in the striatum of schizophrenic patients. Schizophrenia Res. 1997;23:167–74.
Elkashef AM, Doudet D, Bryant T, Cohen RM, Li S-H, Wyatt RJ. 6-18F-DOPA PET study in patients with schizophrenia. Psychiatry Res: Neuroimaging. 2000;100:1–11.
Shotbolt P, Stokes PR, Owens SF, Toulopoulou T, Picchioni MM, Bose SK, et al. Striatal dopamine synthesis capacity in twins discordant for schizophrenia. Psychological Med. 2011;41:2331–8.
Demjaha A, Murray RM, McGuire PK, Kapur S, Howes OD. Dopamine synthesis capacity in patients with treatment-resistant schizophrenia. Am J Psychiatry. 2012;169:1203–10.
Kim E, Howes OD, Veronese M, Beck K, Seo S, Park JW, et al. Presynaptic dopamine capacity in patients with treatment-resistant schizophrenia taking clozapine: An [18F]DOPA PET study. Neuropsychopharmacology 2017;42:941–50.
Jauhar S, McCutcheon R, Borgan F, Veronese M, Nour M, Pepper F, et al. The relationship between cortical glutamate and striatal dopamine in first-episode psychosis: A cross-sectional multimodal PET and magnetic resonance spectroscopy imaging study. Lancet Psychiatry. 2018;5:816–23.
McCutcheon RA, Jauhar S, Pepper F, Nour MM, Rogdaki M, Veronese M, et al. The topography of striatal dopamine and symptoms in psychosis: An integrative positron emission tomography and magnetic resonance imaging study. Biol Psychiatry: Cogn Neurosci Neuroimaging. 2020;5:1040–51.
Kay SR, Flszbein A, Opfer LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophrenia Bull. 1987;13:261–76.
Jauhar S, Nour MM, Veronese M, Rogdaki M, Bonoldi I, Azis M, et al. A test of the transdiagnostic dopamine hypothesis of psychosis using positron emission tomographic imaging in bipolar affective disorder and schizophrenia. JAMA Psychiatry. 2017;74:1206–13.
First M, Gibbon M, Spitzer R, Williams J User’s Guide for the SCID-I for DSM-IV Axis I Disorders - Research Version. New York: Biometrics Research; 1996.
Eisenberg DP, Yankowitz L, Ianni AM, Rubinstein DY, Kohn PD, Hegarty CE, et al. Presynaptic dopamine synthesis capacity in schizophrenia and striatal blood flow change during antipsychotic treatment and medication-free conditions. Neuropsychopharmacology 2017;42:2232–41.
Wallwork RS, Fortgang R, Hashimoto R, Weinberger DR, Dickinson D. Searching for a consensus five-factor model of the positive and negative syndrome scale for schizophrenia. Schizophrenia Res. 2012;137:246–50.
Patlak CS, Blasberg RG. Graphical evaluation of blood-to-brain transfer constants from multiple-time uptake data. Generalizations. J Cereb Blood Flow Metab. 1985;5:584–90.
Tohka J, Reilhac A. Deconvolution-based partial volume correction in Raclopride-PET and Monte Carlo comparison to MR-based method. NeuroImage. 2008;39:1570–84.
Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel RR. What does the PANSS mean? Schizophrenia Res. 2005;79:231–8.
Leucht S, Corves C, Arbter D, Engel RR, Li C, Davis JM. Second-generation versus first-generation antipsychotic drugs for schizophrenia: A meta-analysis. Lancet. 2009;373:31–41.
Carpenter WT Jr, Heinrichs DW, Alphs LD. Treatment of negative symptoms. Schizophrenia Bull. 1985;11:440–52.
Swerdlow NR, Bhakta SG, Talledo J, Benster L, Kotz J, Lavadia M, et al. Lessons learned by giving amphetamine to antipsychotic-medicated schizophrenia patients. Neuropsychopharmacology 2019;44:2277–84.
Sabe M, Kirschner M, Kaiser S. Prodopaminergic drugs for treating the negative symptoms of schizophrenia: Systematic review and meta-analysis of randomized controlled trials. J Clin Psychopharmacol. 2019;39:658–64.
Shukla DK, Chiappelli JJ, Sampath H, Kochunov P, Hare SM, Wisner K, et al. Aberrant frontostriatal connectivity in negative symptoms of schizophrenia. Schizophrenia Bull. 2019;45:1051–9.
Radua J, Schmidt A, Borgwardt S, Heinz A, Schlagenhauf F, McGuire P, et al. Ventral striatal activation during reward processing in psychosis: A neurofunctional meta-analysis. JAMA Psychiatry. 2015;72:1243–51.
Jauhar S, Veronese M, Nour MM, Rogdaki M, Hathway P, Turkheimer FE, et al. Determinants of treatment response in first-episode psychosis: an [18F]-FDOPA PET study. Mol Psychiatry. 2019;24:1502–12.
Jauhar S, McCutcheon R, Borgan F, Veronese M, Nour M, Pepper F, et al. The relationship between cortical glutamate and striatal dopamine in first-episode psychosis: a cross-sectional multimodal PET and magnetic resonance spectroscopy imaging study. Lancet Psychiatry. 2018;5:816–23.
Kumakura Y, Cumming P, Vernaleken I, Buchholz H-G, Siessmeier T, Heinz A, et al. Elevated [18F]Fluorodopamine turnover in brain of patients with schizophrenia: An [18F]Fluorodopa/Positron emission tomography study. J Neurosci. 2007;27:8080.
Eisenberg DP, Kohn PD, Hegarty CE, Ianni AM, Kolachana B, Gregory MD, et al. Common variation in the DOPA Decarboxylase (DDC) gene and human striatal DDC activity in vivo. Neuropsychopharmacology 2016;41:2303–8.
Maharjan S, Serova L, Sabban EL. Transcriptional regulation of tyrosine hydroxylase by estrogen: Opposite effects with estrogen receptors α and β and interactions with cyclic AMP. J Neurochemistry. 2005;93:1502–14.
Criswell SR, Perlmutter JS, Videen TO, Moerlein SM, Flores HP, Birke AM, et al. Reduced uptake of [18F]FDOPA PET in asymptomatic welders with occupational manganese exposure. Neurology 2011;76:1296.
Allen GFG, Neergheen V, Oppenheim M, Fitzgerald JC, Footitt E, Hyland K, et al. Pyridoxal 5′-phosphate deficiency causes a loss of aromatic l-amino acid decarboxylase in patients and human neuroblastoma cells, implications for aromatic l-amino acid decarboxylase and vitamin B6 deficiency states. J Neurochemistry. 2010;114:87–96.
Acknowledgements
We would like to thank the research volunteers for their generous participation in this study, the staff of the NIH PET Center for their assistance in data acquisition, the nursing staff and multidisciplinary care team on the 7SE-S Inpatient Clinical Research Unit for their support of inpatient care, the CTNB Recruitment Team for their help with participant recruitment, and the CTNB administrative and research staff for their facilitation of this work. Some of this work utilized the computational resources of the NIH HPC Biowulf cluster (http://hpc.nih.gov).
Funding
This research was supported by the Intramural Research Program, National Institute of Mental Health, NIH, Bethesda, MD, 20892. Project ZIAMH002652 (NCT00001247, NCT00024622). All authors report no financial conflict of interest with regard to this paper.
Author information
Authors and Affiliations
Contributions
DPE and KFB were involved in the conception and design of the study. DPE drafted the paper, and all authors have substantially revised it critically for intellectual content. All authors have contributed to data acquisition, analysis, or interpretation of the data. All authors have reviewed and approved the final version of this article.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Eisenberg, D.P., Kohn, P.D., Hegarty, C.E. et al. Clinical correlation but no elevation of striatal dopamine synthesis capacity in two independent cohorts of medication-free individuals with schizophrenia. Mol Psychiatry 27, 1241–1247 (2022). https://doi.org/10.1038/s41380-021-01337-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-021-01337-1