Abstract
Study design
Single-centre, retrospective study of people with a spinal cord injury or disorder (PwSCI/D) and identified psychological need.
Objectives
To examine the effect of psychological need on rehabilitation outcomes.
Setting
National Spinal Injuries Centre (NSIC), Stoke Mandeville Hospital, Buckinghamshire Healthcare NHS Trust, United Kingdom.
Methods
Self-reported data from the Stoke Mandeville Spinal Needs Assessment Checklist (SMS-NAC) were used to examine identified psychological need (characterised by referral for psychological treatment, or scoring above clinical threshold in admission psychometric measures) on SCI rehabilitation outcome domains. Participants were grouped according to whether they were referred, not referred, scored above or below clinical threshold.
Results
234 participants were included (Mean age at injury (years) = 53, 70% Male, 29% tetraplegia, 38% paraplegia, 33% ASIA D). There was a significant improvement in outcome scores from admission to discharge across all domains irrespective of participant group, however individuals with identified psychological need scored lower across all rehabilitation domains than those without. While individuals with psychological need demonstrated longer rehabilitation stays, more frequent and longer discharge delays, they also showed comparatively greater rehabilitation improvements. Psychological screening measures were more effective at detecting psychological need than individuals identified via referral, and participants scoring above clinical threshold had poorest overall rehabilitation outcomes.
Conclusions
Individuals with psychological need have greater rehabilitation need and may require longer rehabilitation and benefit from additional discharge planning. Early, proactive psychometric screening can better facilitate improvements for delivering rehabilitation. Future research should consider specific contributing factors to psychological need, such as pre-existing mental health conditions or socio-demographic influences.
Similar content being viewed by others
Introduction
A spinal cord injury or disorder is a major life event, affecting both physical and social functioning, and resulting in unique psychological pressures in the process of adaptation [1, 2]. Persons with a spinal cord injury or disorder (PwSCI/D) often undertake specialised rehabilitation in Spinal Cord Injury Centres to acquire the physical skills and knowledge to meet the significant, numerous and varied challenges. Several personal factors including age, ethnicity and injury aetiology have been evidenced to influence rehabilitation availability and outcome [3,4,5,6].
Another significant factor influencing rehabilitation outcome is psychological wellbeing. Many PwSCI/D experience psychological difficulties after their injury, with diagnostic rates for mental health disorders ranging from 10% to one third of individuals [7]. Additionally, PwSCI/D repeatedly report the challenges of learning new skills and behaviours alongside the psycho-emotional upheaval to their activities, roles and sense of self following their injury [2, 8, 9]. Such psychological difficulties are inextricably linked to individuals’ physical health. Low mood, for example, is associated with increased pain, poorer physical health, increased mortality, and impairments to memory, concentration and energy [10], all of which may limit individuals’ engagement with rehabilitation and the acquisition of new skills and knowledge. Similarly, Heinemann et al. [11] found that individuals who required greater levels of emotion-focused psychological support during rehabilitation had comparatively lower motor function after rehabilitation.
Despite both the prevalence of psychological need for PwSCI/D and the potential ramifications for rehabilitation, research on this relationship has been limited. Thus far, although some examination of the role of psychological resources have been undertaken, such as self-efficacy or coping strategies in functional and health outcomes [1, 12,13,14], there remains little consideration of the influence of mood or adjustment more broadly upon rehabilitation outcome. One study, Kennedy et al. [15], examined the difference in outcomes and found that individuals with mental health disorders had more rehabilitation needs but made comparatively greater gains over time than those without. However, the sample size was small and did not account for individuals who may have developed psychological need secondary to their spinal cord injury.
It has been evidenced that individuals with long-term and comorbid psychological need, such as depression or anxiety, have worse healthcare outcomes, including longer treatment durations and increased rates of hospitalisation [16]. This is likely to be due to a range of causes, including greater risk of additional physical health conditions or reduced socio-economic resources restricting independence of people with mental health needs being met in the community [17]. However, there has only been limited consideration of psychological need on healthcare outcomes in the context of inpatient spinal cord injury rehabilitation. By examining this impact, it may be possible to minimise unnecessary costs and resource-consumption within services, as well as highlight areas where clinical best practice may need review.
A further concern is that examined rehabilitation outcomes are often limited to physical functionality, which means the effect of wider psychological variables on other rehabilitation goals, such as self-management and resumption of meaningful activities, remains unclear. Research into such components are essential to determine whether psychological screening measures are needed and enable better identification of need and achievement of rehabilitation goals.
Finally, there is little research examining the different methods through which psychological need is identified. Some nations have developed best practice guidelines about the provision of screening for psychological need using psychometric measures, and undertake patient follow-up for individuals who exceed a pre-determined score [18, 19], but this has yet to be done in the UK where clinical psychology Spinal Cord Injury Centre provision is highly variable. Most UK Spinal Cord Injury Centres’ clinical psychology services incorporate a referral system: individuals are most often referred by a member of their treating team (either with or without their knowledge), can self-refer or be referred by a family member at any point during admission.
Internationally, there is currently no standardised screening, associated treatment recommendations or the required psychologist workforce for intervention or services, although recommendations for routine screening for depression and anxiety is under development by ISCoS through an International Psychological Basic Data Set. Currently, many services across the world rely on local and practical considerations such as clinician availability. It is therefore relevant to investigate whether differences in rehabilitation outcome arise between those identified through psychological screening measures compared to those identified through referral.
Given the prevalence of psychological need within PwSCI/D, the potential interference of mood and adjustment on rehabilitation engagement and attainment, and the lack of standardisation regarding the method used to identify psychological need, the present study aimed to:
-
1.
Examine whether identified psychological need – characterised by referral for psychological treatment or scoring above clinical threshold on psychological screening measures – influences rehabilitation outcome (individuals’ attainment of skills and knowledge) and affects duration of admission.
-
2.
Explore whether identifying psychological need via referral compared to via psychometric screening measures present differences in rehabilitation outcomes.
It was hypothesised that individuals with identified psychological need would have poorer outcomes, with lower achieved scores on outcome measures, and longer length of hospital stay during rehabilitation. In line with previous research [15], it was hypothesised that those with psychological need would nevertheless make greater rehabilitation gains over time.
Methods
All adult PwSCI/D admitted for rehabilitation at a specialist Spinal Cord Injury Centre between February 2015 and January 2020 were considered for participation in the current study (N = 724), however only participants who completed a multidisciplinary rehabilitation outcome assessment at admission and discharge were included (N = 234). As outcome measures are completed routinely for all inpatients, except those with significant cognitive impairments, no other inclusion or exclusion criteria were applied. Of the 489 excluded participants, 71 had not completed any assessment, 408 had completed only an admission assessment, 7 had an incomplete pre-discharge assessment, 3 had an incomplete admission assessment, and 1 assessment had been completed by a paediatric inpatient. A range of systemic reasons for the reduced number of inpatients with only an admission assessment have been identified and this is part of a larger quality improvement project [20].
Outcome measures
The Stoke Mandeville Spinal Needs Assessment Checklist (SMS-NAC)
Theprimary outcome variable was the SMS-NAC [21], a spinal cord injury-specific, validated [22], multidisciplinary team-administered [23] self-report measure of an individual’s skill and knowledge across ten biopsychosocial domains: physical health, daily living activities, skin and posture management, bladder management, bowel management, mobility, wheelchair and equipment, community preparation, psychological health, and discharge coordination. The psychological health domain includes several assessments, such as caring responsibilities, sexual health, relationships and intimacy, as well as the widely used and validated Hospital Anxiety and Depression Scale (HADS) [24, 25] and the short form of the Appraisals of DisAbility: Primary and Secondary Scale (ADAPSS-sf) [26, 27]. For the purposes of the psychological health domain in the SMS-NAC, items for the HADS and ADAPSS-sf are reverse-coded such that lower scores indicate poorer psychological health. However, for the purposes of examining psychological need, HADS and ADAPSS-sf scores were re-reverse coded so that higher scores indicate greater need.
The SMS-NAC contains 328 items across the 10 domains: each item is scored 0–3, with higher scores indicating greater knowledge or verbal or physical independence in that task. Questions inappropriate to the individual’s level of injury are scored as not applicable. Individuals’ scores for each domain are calculated as a percentage of the maximum possible score and were used in the present analysis. For the purposes of this study, missing items in the SMS-NAC were scored as 0.
The SMS-NAC is administered twice as part of standard clinical practice: within 2 weeks of admission and 4 weeks prior to discharge. The SMS-NAC is regularly updated according to clinical practice: the current paper reports on the 2015 version [28]. An updated version was released in 2020 which included different psychological screening measures and additional sections [20].
Secondary outcome variables
Total Length of Rehabilitation was calculated as the difference in days between the participants’ admission date and their proposed discharge date. The multidisciplinary team and the inpatient agree a discharge date through a collaborative process at the second goal planning meeting. An inpatient remaining beyond this date is considered to have a ‘delayed discharge’. Delayed Discharge was defined as one or more days after participants’ proposed discharge date. Delays are most commonly due to discharge arrangements not being in place, or because the inpatient has become medically unfit (such as pressure injury or urinary tract infection). Length of Discharge Delay was calculated as the difference in days between participants proposed and final discharge date.
Psychological need groupings
Participants were categorised into four groups: ‘referred’, ‘not referred, ‘above clinical threshold’, below clinical threshold’. Participants who were ‘referred’ were those who received a referral for psychological treatment, and participants could have been referred at any point following their admission to hospital. Participants who were ‘above clinical threshold’ were those who received a ‘clinical flag’ by scoring 8 or above on the HADS and/or 22 or above on the ADAPSS-sf screening measures. Participants ‘not referred’ therefore did not receive a referral for psychological treatment, and participants ‘below clinical threshold’ therefore did not receive a clinical flag for either of the psychometric screening measures.
Data collection
Data for the primary outcome assessment, the SMS-NAC, was drawn from the Spinal Cord Injury Centre’s central database. Demographic data and dates relating to participants’ rehabilitation were drawn from inpatients’ electronic medical notes. Whether a participant was referred to the clinical psychology department was established by review of their electronic inpatient notes, cross-checking this against the clinical psychology department’s internal records to ensure all referrals were captured. Finally, whether a participant was coded as above or below clinical threshold at admission was established by examining the HADS and ADAPSS-sf scores on their admission SMS-NAC.
All applicable institutional and governmental regulations concerning the ethical use of human volunteers were adhered to in this study.
Analysis
One-way ANOVAs and Chi-Square tests of association were used to examine differences between the four psychological need groups: referred or not, above or below clinical threshold. To determine whether there was a main effect of psychological need group (referred versus not; above versus below clinical threshold) or time (admission versus discharge) on SMS-NAC scores, mixed 2 × 2 (time × psychological need group) ANOVAs were conducted for the main analysis, using each SMS-NAC domain score as the dependent variable. Interaction effects of time by psychological need group were also explored.
As a follow-up to the mixed ANOVA, which used the averaged admission and discharge scores and therefore may be skewed by significant differences at one time-point only, one-way ANOVAs were conducted separately for each SMS-NAC domain over time (admission and discharge) by psychological need group. Examining the effect of psychological need group may indicate whether degree of improvement across rehabilitation domains differs for those referred (versus not) and/or those scoring above clinical threshold (or below). Similarly, examining the effect of time may indicate whether rehabilitation outcomes improved from admission to discharge. One-way ANOVAs were also used to examine whether differences existed between psychological need groups on participants’ length of rehabilitation admission and length of discharge delay. Chi-square tests of association were conducted to examine whether there was an over-representation of delayed discharges between the groups. Significance was set at p < 0.05 for all tests; partial η2 of 0.01–0.059 was considered a weak effect, 0.06–0.139 a moderate effect, and ≥0.14 a strong effect.
Results
Due to the large proportion of excluded participants who had only completed an admission assessment (N = 408), mean admission scores for the psychological health domain were compared. Those with only an admission SMS-NAC (Mean = 64.48) were compared to those who had both an admission and discharge SMS-NAC (Mean = 63.51) in case of non-response bias. The results indicated that there was no significant difference in mean psychological health scores at admission between the groups (t = 0.970, p = 0.332).
Psychological need groupings
For included participants, descriptive statistics for the psychological need groupings are presented in Table 1, and demographics and descriptive statistics for SMS-NAC domain scores for each psychological need group are presented in Table 2. There was a significant over-representation of those with tetraplegia (A/B/C) among those referred (χ2 (2) = 6.439, p = 0.040) and those scoring above clinical threshold (χ2 (2) = 7.039, p = 0.030). There were no other significant differences between groups with respect to gender, ethnicity, cause of injury, age at injury or time from injury to admission.
SMS-NAC
Mean admission and discharge scores across the 10 SMS-NAC domains for each psychological need group are presented in Table 2.
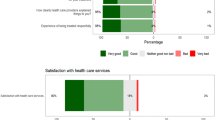
There was a strong significant increase in scores from admission to discharge across all groups for all domains of the SMS-NAC (Table 3). This indicates that PwSCI/D showed improvement in all areas of rehabilitation, independent of psychological need.
There was a weak-to-moderate main group effect for those referred versus those not referred in 5 of the 10 domains (physical health, activities of daily living, bowel management, wheelchair and equipment, and psychological health) (Table 3), with lower mean SMS-NAC scores for those referred. Results of the one-way ANOVA (Table 4) found a weak-to-moderate effect in the psychological health and activities of daily living domains at both admission and discharge; in the physical health and bowel management domains at admission only; and in the wheelchair and equipment domain at discharge only. At all time-points where an effect was found, those referred for psychological treatment scored significantly lower across rehabilitation domains than those not referred.
There was a weak-to-moderate main group effect for those above clinical threshold across all domains of the SMS-NAC (Table 3), with lower mean SMS-NAC scores for those scoring above clinical threshold. The one-way ANOVA (Table 4) found a weak-to-moderate effect in the physical health, activities of daily living, bladder management, bowel management, wheelchair and equipment, and discharge coordination domains at admission and discharge; in the community preparation domain at admission only; and the skin and posture management, and mobility domains at discharge only. The strongest effect was found in the psychological health domain between admission (η2 = 0.43) and discharge (η2 = 0.22). Once again, at all time-points where an effect was found, participants scoring above clinical threshold at admission scored significantly lower across rehabilitation domains than those scoring below clinical threshold.
There was no significant interaction effect of time (admission versus discharge) by referred versus not referred psychological need group for each domain. However, in 7 of the 10 domains those referred made greater improvements in rehabilitation outcome scores over time than those not referred. There was a weak but significant interaction effect of time (admission versus discharge) for those scoring above clinical threshold in the domains of daily living activities (F(1,232) = 6.76, p = 0.010, partial η2 = 0.03) and psychological health (F(1,232) = 8.64, p = 0.004, partial η2 = 0.04). With the exception of the mobility domain, those scoring above clinical threshold at admission made greater improvements in rehabilitation outcome scores over time than those scoring below clinical threshold.
SMS-NAC additional analyses
All participants were screened at admission and therefore were flagged as either above or below clinical threshold depending on their scores on the psychometric measures. However, as some participants were referred following their admission screening, there was a crossover between psychological need groupings (Table 1). Those referred would have also received varying levels of psychological intervention and frequency, as outlined by the services pathway [29]. Additional analyses were therefore undertaken to more closely examine the relationship between referral versus psychometric screening measures on total mean SMS-NAC scores by splitting participants into 3 new groups: ‘referred only’, ‘above threshold only’, and ‘neither referred or above threshold’ (Supplementary Table 1). Bartlett test of equal variance indicated non-significant variance between the 3 groups for total SMS-NAC admission scores (B = 1.62, p = 0.444) and total SMS-NAC discharge scores (B = 1.36, p = 0.506). Independent samples t-tests were therefore conducted for group comparisons. There was a significant difference between the ‘above threshold only’ and ‘neither referred or above threshold’ groups in mean total SMS-NAC score at both admission (t = 4.65, p < 0.001) and discharge (t = 4.22, p < 0.001), with those scoring ‘above threshold only’ demonstrating lower mean scores. Similarly, there was a significant difference between those ‘above threshold only’ and ‘referred only’ at admission (t = 2.47, p = 0.015) and discharge (t = 2.14, p = 0.035), with those scoring ‘above threshold only’ demonstrating lower mean score. While there was a non-significant difference between the ‘referred only’ and ‘neither referred or above threshold’ groups in mean total SMS-NAC score at admission (t = 1.96, p = 0.052), a significant difference emerged at discharge (t = 2.14, p = 0.034). This suggested similar mean SMS-NAC scores at admission between the two groups, but lower mean SMS-NAC scores for those ‘referred only’ at discharge. Mean difference in SMS-NAC score from admission to discharge, indicating rehabilitation outcome improvement, was greatest for the ‘above threshold only’ group and fewest for the ‘neither referred or above threshold’ group (Supplementary Table 1).
Length of rehabilitation
There was a weak but significant difference in length of rehabilitation between those referred and those not referred (F(1,232) = 4.60, p = 0.033, partial η2 = 0.02), and between those scoring above clinical threshold compared with those below (F(1,232) = 9.77, p = 0.002, partial η2 = 0.04). Participants referred for psychological treatment and also those participants scoring above clinical threshold at admission had significantly longer periods of rehabilitation than those not receiving treatment or scoring below clinical threshold.
Discharge delay
There was no significant difference in the distribution of delayed discharges between those referred and those not referred (χ2(1) = 0.17, p = 0.684). However, there was a significant difference between clinical threshold groups (χ2(1) = 10.04, p = 0.002), whereby there was an over-representation of inpatients with a delayed discharge among those who scored above clinical threshold at admission.
For delayed discharges, there was no significant difference between participants who were referred and those not referred in terms of the length of delay (F(1,232) = 2.44, p = .119, partial η2 = 0.01). However, those above clinical threshold at admission had significantly longer delays than those below clinical threshold at admission (F(1,232) = 5.08, p = 0.025, partial η2 = 0.02).
Discussion
Psychological need and rehabilitation outcomes
In accordance with the initial hypotheses, the present results indicate that individuals presenting with psychological need also have greater rehabilitation need.
Participants who were referred for psychological treatment and participants who scored above clinical threshold at admission were found to have lower attainment across various domains of the SMS-NAC, at both admission and discharge, than those not referred or scoring below clinical threshold. As the SMS-NAC is a self-report measure, this suggests that individuals presenting with psychological need consider themselves less knowledgeable and less independent during their rehabilitation. This could reflect perceptual biases resulting from mood disorders. For example, individuals with depression and anxiety often have lowered self-esteem and confidence, and cognitive distortions (such as ‘black-and-white’ thinking, or minimising positives) which result in a more negative view of themselves and their rehabilitation; indeed, the triad of negative attitudes towards the self, others and world is one of the defining characteristics of depression [30]. Similarly, in order to score above the ADAPSS-sf clinical threshold, individuals must demonstrate an inclination to negatively appraise their external situation (their SCI/D and the ‘manageability’ of their rehabilitation), their internal resources (such as knowledge and skills to adapt to SCI/D), or both [31]. Individuals with psychological need, as identified in the present study, may be more likely to underestimate their abilities and therefore obtain lower scores across the SMS-NAC domains.
The finding that those referred and those above clinical threshold had longer rehabilitation stays suggests that individuals with psychological need may require more time to achieve comparable rehabilitation outcome. It is possible that the physical effects of low mood, anxiety or appraisals reduce individuals’ rate of progress. Indeed, low mood has been found to increase pain levels [10] which can interfere with rehabilitation participation and engagement. Although there is less accumulated evidence about the effects of anxiety compared to depression on rehabilitation outcome, in a meta-analysis Le and Dorstyn [32] comment that ongoing fear of secondary life-threatening consequences such as autonomic dysreflexia may emerge during rehabilitation. Additionally, impairments to cognition or attention, which can result from mood disorders [33], may have impeded individuals’ attainment of new skills and information. Alternatively, individuals with psychological need may simply have greater rehabilitation need. This is increasingly likely given the current finding that participants with psychological need considered themselves less knowledgeable and independent by scoring lower in the self-reported rehabilitation outcome measure: they may therefore have more rehabilitation goals yet to achieve or they may benefit from a more individualised rehabilitation programme which takes into account their psychological health, such as integrating psychological treatment with other therapies to maximise gain.
Participants who scored above clinical threshold at admission were also more likely to have a delayed discharge and the delay was significantly longer. The results may have been skewed by an over-representation of individuals with tetraplegia among those who scored above clinical threshold, which may be related to the longer hospital stay required for the provision of care needs in addition to rehousing on discharge. However, although there was also an over-representation of individuals with tetraplegia among those referred, no significant differences were found for this group in relation to either likelihood of discharge delay or length of delay. This suggests that individuals who present with a significant number of depression or anxiety symptoms or who negatively appraise their injury via psychometric screening measures experience a greater number of challenges during discharge preparations which may include physical health or secondary health complications as a result of difficulties in managing their self-care. Indeed, it is currently understood that individuals with psychological needs are more likely to develop physical health conditions [17]. It is also possible that those with identified need, due to their lower self-perceived skills and independence, are more likely to resist discharge arrangements because they do not consider themselves prepared for discharge. This would be of particular clinical concern given the strain such situations can place on the relationships between inpatients, staff, commissioners and rehabilitation providers. Overall, the finding would appear to reinforce previous evidence that people with psychological needs require a greater length of time and more and/or different healthcare provision to enhance the accommodation of their psychological needs [17], even in the context of specialised rehabilitation centres.
Finally, as hypothesised, and in line with Kennedy et al. [15], individuals with identified psychological need made greater rehabilitation gains in almost all rehabilitation outcomes than those either not referred for psychological treatment or those who scored below clinical threshold, despite scoring lower in all rehabilitation domains at admission and independent of whether individuals received psychological support. Although psychological need appears to affect individuals’ speed and perception of rehabilitation improvement, potential for improvement remains and can therefore be maximised if psychological intervention is provided. Crucially, therefore, rehabilitation outcomes are not universally or inevitably poorer for those with identified psychological need.
Clinical implications
Methods for identifying psychological need
The current study sought to investigate whether differences existed between individuals who were ‘flagged’ via clinical psychometric screening measures compared to those who were referred for psychological treatment. It was found in both the main analyses and additional analyses that individuals identified via psychometric screening measures showed greater percentage improvement in SMS-NAC scores across the rehabilitation domains from admission to discharge than individuals identified via referral, which may indicate that screening measures are more effective at detecting psychological need than a referral process. The point at which psychological need is identified may contribute to this. As clinical threshold distinctions were drawn from participants’ admission scores, psychological state at admission may be more indicative of future rehabilitation outcomes than referral later in the rehabilitation process [13]. Proactively identifying psychological need via psychometric screening measures and actively providing identified individuals with psychological support is crucial to the aim of providing best care and ensuring individuals reach their rehabilitation potential.
Findings from the additional analyses also suggested that individuals scoring above clinical threshold who were not referred – and therefore did not receive psychological treatment – had poorest rehabilitation outcomes at both admission and discharge. This emphasises the efficacy of psychometric screening measures at identifying psychological need and, more importantly, the requirement for all inpatients with need to be provided with formal psychological assessment and treatment where identified in order to improve rehabilitation outcome.
Nevertheless, while the efficacy of psychometric screening measures at detecting psychological need has been evidenced, the value of referral should not be discredited. Rehabilitation outcome scores for those referred for psychological treatment were lower than individuals not identified as having psychological need at both admission and discharge. Importantly, individuals who were referred for psychological support did not improve as much from admission to discharge as those who had scored above clinical threshold and also demonstrated significantly lower outcome scores than individuals without identified psychological need. This may be explained by the complexity of psychological need which is driving the referrals, and may illustrate aspects of psychological need – such as complex relationship issues or more challenging mental health concerns – which cannot be detected from brief mood and adjustment screening measures [34].
Additionally, while it is important to screen for psychological need early in admission, it is equally important for health professionals to be alert for emerging psychological need throughout the rehabilitation process. Mental health problems are not linear; they may develop at any point in the rehabilitation process, and often from a complex interplay between personal, situational and interpersonal influences. It is therefore important for multidisciplinary teams to be sensitive to any changes in inpatients’ psychological health which may indicate the need to refer for intervention. The utility of each method for identifying psychological need – screening measures and a referral process – should be maximised to ensure that all individuals requiring support are identified.
Rehabilitation gain
Although the ability to improve during rehabilitation for individuals with psychological need was unaffected, they appear less able to recognise such improvements and to translate them into effective self-management. As long-term health conditions such as SCI/D are increasingly being addressed by healthcare services with a self-management model [35], it is essential for PwSCI/D to consider themselves knowledgeable and capable in managing their condition independently. Rehabilitation centres must therefore identify and respond to psychological need, not merely for individuals’ psychological wellbeing, but also for their long-term health.
Moreover, given the evidence suggesting that individuals with psychological need require longer rehabilitation to achieve their goals, screening early in admission will enable clinicians to more effectively support goal attainment. Proactively structuring rehabilitation for those with identified psychological need and/or allowing greater admission time may mitigate engagement difficulties and counter the potential for underestimation of skills and knowledge, and more effectively achieve self-management after discharge. Similarly, earlier and more extensive discharge planning may be required in order to meet additional needs or to compensate for limited resources. In both cases, this would likely reduce the frequency and length of delayed discharges, which would ultimately improve the effectiveness and efficiency of healthcare provision thus promoting lifelong health.
Limitations and future directions
While the present study is a valuable contribution to clinical understanding regarding the effect of psychological need on rehabilitation outcomes, there are some limitations which merit future investigation. Firstly, the analyses in this study only indicate that a relationship exists between psychological need and rehabilitation outcomes: further study is required to clarify this relationship and to determine potential causal links.
Secondly, the variables used in the present study to quantify psychological need were deliberately simplified to focus on the initial psychological indicators that clinicians may witness in practice. It would be valuable for future cross-sectional and longitudinal research to account for specific contributing factors to psychological need (such as pre-existing mental health disorders or socio-demographic factors, such as limited social support) and psychological changes during rehabilitation.
In addition, the data regarding identifying psychological need in this paper was a combination of both mood disorders and appraisals. Future research to tease out the relationship between these areas or the relative contribution of each on adjustment could enhance psychological treatments.
The current findings suggest that those with psychological need made comparatively greater improvements in rehabilitation outcomes than those without. However, a limitation of this finding is that some participants with identified psychological need would also have received psychological treatment, which may have influenced the degree of improvement in rehabilitation from admission to discharge. Controlling for this influence through clinical or diagnostic interview would validate whether referral or screening is more effective and would provide a less biased comparison for the degree and trajectory of improvement.
Crucially, some participants in the current study would have been included in more than one psychological need group for the main analysis, therefore weakening the validity of the results and any subsequent conclusions made. Additional analyses were undertaken to compensate for this confound, and the results from these analyses supported findings from the main analysis that scoring above clinical threshold in screening measures results in the poorest rehabilitation outcome but also comparatively the greatest improvements from admission to discharge. Despite this, it would be worthwhile for future studies to replicate the current study design while more effectively minimising confounding variables, particularly with regard to controlling for psychological need group and psychological treatment.
Conclusions
The present study indicated that PwSCI/D who require psychological support during rehabilitation have greater physical and psychosocial rehabilitation needs and may therefore require longer rehabilitation and more complex discharge planning. As such, early and proactive psychological screening is essential because those who were flagged but did not receive intervention had the poorest rehabilitation outcome. It was also shown that individuals with identified psychological need demonstrated similar, if not greater, improvements across rehabilitation domains than individuals not requiring psychological intervention, which reinforces that addressing psychological need can facilitate positive rehabilitation gain for all.
Data availability
The data used in the current study are part of a standard clinical database which contains identifiable patient information and are therefore not publicly available. Pseudonymised data can be made available upon reasonable request to Buckinghamshire Healthcare NHS Trust.
References
Kennedy P, Lude P, Taylor N. Quality of life, social participation, appraisals and coping post spinal cord injury: a review of four community samples. Spinal Cord. 2006;44:95–105.
Craig A, Tran Y, Guest R, Middleton J. Trajectories of self-efficacy and depressed mood and their relationship in the first 12 months following spinal cord injury. Arch Phys Med Rehabilitation. 2019;100:441–7.
Kennedy P, Kilvert A, Hasson L. Ethnicity and rehabilitation outcomes: the needs assessment checklist. Spinal Cord. 2015;53:334–9.
Kennedy P, Cox A, Mariani A. Spinal cord injuries as a consequence of falls: are there differential rehabilitation outcomes? Spinal Cord. 2013;51:209–13. https://doi.org/10.1038/sc.2012.124. Available from.
Kennedy P, Chessell ZJ. Traumatic versus non-traumatic spinal cord injuries: are there differential rehabilitation outcomes? Spinal Cord. 2013;51:579–83. https://doi.org/10.1038/sc.2013.27. Available from.
Kennedy P, Hasson L. An audit of demographics and rehabilitation outcomes in non-traumatic spinal cord injury. Spinal Cord. 2016;54:1020–4.
Bombardier C, Azuero C, Fann J, Kautz D, Richards J, Sabharwal S, et al. Management of mental health disorders, substance use disorders, and suicide in adults with spinal cord injury: clinical practice guideline for healthcare providers. Top Spinal Cord Inj Rehabilitation. 2020;27:152–224.
Whalley Hammell K. Experience of rehabilitation following spinal cord injury: a meta-synthesis of qualitative findings. Spinal Cord. 2007;45:260–74.
Nunnerley JL, Hay-Smith EJC, Dean SG. Leaving a spinal unit and returning to the wider community: an interpretative phenomenological analysis. Disabil Rehabilitation. 2013;35:1164–73.
Kennedy P, Hasson L. The relationship between pain and mood following spinal cord injury. J Spinal Cord Med. 2017;40:275–9.
Heinemann AW, Wilson CS, Huston T, Koval J, Gordon S, Gassaway J, et al. Relationship of psychology inpatient rehabilitation services and patient characteristics to outcomes following spinal cord injury: The SCIRehab Project. J Spinal Cord Med. 2012;35:578–92.
van Diemen T, Crul T, van Nes I, Geertzen JH, Post MW. Associations between self-efficacy and secondary health conditions in people living with spinal cord injury: a systematic review and meta-analysis. Arch Phys Med Rehabilitation. 2017;98:2566–77.
Kennedy P, Kilvert A, Hasson L. A 21-year longitudinal analysis of impact, coping, and appraisals following spinal cord injury. Rehabilitation Psychol. 2016;61:92–101.
Kennedy P, Lude P, Elfström ML, Smithson EF. Psychological contributions to functional independence: a longitudinal investigation of spinal cord injury rehabilitation. Arch Phys Med Rehabilitation. 2011;92:597–602. https://doi.org/10.1016/j.apmr.2010.11.016.
Kennedy P, Sherlock O, Sandu N. Rehabilitation outcomes in people with pre-morbid mental health disorders following spinal cord injury. Spinal Cord. 2009;47:290–4. https://doi.org/10.1038/sc.2008.116. Available from.
Siddiqui N, Dwyer M, Stankovich J, Peterson G, Greenfield D, Si L, et al. (2018). Hospital length of stay variation and comorbidity of mental illness: A retrospective study of five common chronic medical conditions. BMC Health Services Research, 18.
Public Health England. Health matters: reducing health inequalities in mental illness. 2018 [cited 2022 Feb 14]. Available from: https://www.gov.uk/government/publications/health-matters-reducing-health-inequalities-in-mental-illness/health-matters-reducing-health-inequalities-in-mental-illness.
Russell HF, Richardson EJ, Bombardier CH. Professional standards of practice for psychologists, social workers, and counselors in SCI rehabilitation. J Spinal Cord Med. 2016;39:127–45. https://doi.org/10.1080/10790268.2015.1119966.
Middleton JW, Perry KN, Craig A. A Clinical Perspective on the Need for Psychosocial Care Guidelines in Spinal Cord Injury Rehabilitation. Int J Phys Med Rehabilitation. 2014;2:1–6.
Duff J, Grant LC, Gilchrist H, Jones K. Building and sustaining inpatient-clinician collaboration in spinal cord injury rehabilitation: a case example using the stoke mandeville spinal needs assessment checklist (SMS-NAC) and goal planning programme. J Clin Med. 2022;11:3730 https://doi.org/10.3390/jcm11133730.
Kennedy P, Hamilton LR. The needs assessment checklist: a clinical approach to measuring outcome. Spinal Cord. 1999;37:136–9. http://www.stockton-press.co.uk/sc.
Berry C, Kennedy P. A psychometric analysis of the Needs Assessment Checklist (NAC). Spinal Cord. 2003;41:490–501.
Eaton R, Duff J, Wallace M, Jones K. The value of the whole picture: rehabilitation outcome measurement using patient self-report and clinician-based assessments after spinal cord injury. Spinal Cord. 2022;60:71–80.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scandinavica. 1983;67:361–70. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1600-0447.1983.tb09716.x.
Bombardier CH, Azuero CB, Fann JR, Kautz DD, Richards JS, Sabharwal S, et al. Management of mental health disorders, substance use disorders, and suicide in adults with spinal cord injury: Clinical practice guideline for healthcare providers. Top Spinal Cord Inj Rehabilitation. 2021;27:152–224. https://doi.org/10.46292/sci2702-152.
Dean RE, Kennedy P. Measuring appraisals following acquired spinal cord injury: a preliminary psychometric analysis of the appraisals of disability. Rehabilitation Psychol. 2009;54:222–31.
Eaton R, Jones K, Duff J. Cognitive appraisals and emotional status following a spinal cord injury in post-acute rehabilitation. Spinal Cord. 2018;12:1151–7. https://doi.org/10.1038/s41393-018-0151-6.
Kennedy P, Duff J. Stoke Mandeville Spinal Needs Assessment Checklist, version 2015. bht.nsicpsychology@nhs.net. Accessed 2015.
Mahali SC, Beshai S, Feeney JR, Mishra S (2020). Associations of negative cognitions, emotion regulation, and depression symptoms across four continents: International support for the cognitive model of depression. BMC Psychiatry, 20. Available from: https://doi.org/10.1186/s12888-019-2423-x.
Craig A, Duff J, Middleton J (2022). Spinal cord injuries. In Asmundson, GJG (Ed.) Comprehensive Clinical Psychology, 2nd edition, vol. 8. Elsevier, 301–28. https://doi.org/10.1016/B978-0-12-818697-8.00061-3.
Duff J, Angell B. Regaining A Sense Of Me: a single case study of SCI adjustment, applying the appraisal model and coping effectiveness training. Spinal Cord Ser Cases. 2021;7:11 https://doi.org/10.1038/s41394-020-00349-3.
Le J, Dorstyn D. Anxiety prevalence following spinal cord injury: a meta-analysis. Spinal Cord. 2016;54:570–8. https://doi.org/10.1038/sc.2016.15.
Marvel CL, Paradiso S. Cognitive and neurological impairments in mood disorders. Psychiatr Clin North Am. 2008;27:19–36.
Huston T, Gassaway J, Wilson C, Gordon S, Koval J, Schwebel A. The SCIRehab project: treatment time spent in SCI rehabilitation. Psychology treatment time during inpatient spinal cord injury rehabilitation. J Spinal Cord Med. 2011;34:196–204. https://doi.org/10.1179/107902611X12971826988219.
McIntyre A, Marrocco SL, McRae SA, Sleeth L, Hitzig S, Jaglal S, et al. A scoping review of self-management interventions following spinal cord injury. Top Spinal Cord Inj Rehabilitation. 2020;26:36–63.
Acknowledgements
Thank you to the patients and staff of the National Spinal Injuries Centre, Stoke Mandeville Hospital, Buckinghamshire Healthcare NHS Trust, for completion of the standard clinical outcome tool (SMS-NAC) which comprised this research.
Author information
Authors and Affiliations
Contributions
MW was responsible for study design, extracting and analysing the data, and writing the report. JD was responsible for the study design, contributed to the interpretation of results and writing of the report, and had oversight into the final version and submission of the research. LG contributed to analysing the data, writing the report and the submission of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The authors certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were adhered to during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Wallace, M., Duff, J. & Grant, L.C. The influence of psychological need on rehabilitation outcomes for people with spinal cord injury. Spinal Cord 61, 83–92 (2023). https://doi.org/10.1038/s41393-022-00864-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00864-0