Abstract
Study design
This is a retrospective longitudinal study.
Objectives
To explore the relative impact and contribution of using both the Spinal Cord Independence Measure III (SCIM) and Stoke Mandeville Spinal Needs Assessment Checklist (SMS-NAC) to assess rehabilitation outcome following an acute spinal cord injury (SCI).
Setting
The study was performed at National Spinal Injuries Centre (NSIC), Stoke Mandeville Hospital, Buckinghamshire Healthcare NHS Trust, Aylesbury, UK.
Methods
A patient self-report SMS-NAC and clinician-rated SCIM were administered on admission and discharge from the NSIC as part of standardised care. This paper presents a retrospective analysis of the rehabilitation outcomes of 195 people with spinal cord injury (PwSCI) following their first admission.
Results
In both measures, PwSCI improved from admission to discharge. Individuals with higher SCI obtained lower scores in both measures, at both admission and discharge. The SMS-NAC demonstrated the greatest increase in knowledge and skill for PwSCI who had higher and more complete injuries. On the SCIM, PwSCI who had lower and less complete injuries demonstrated the greatest increase in outcome.
Conclusions
Overall, both measures demonstrated responsiveness to change during SCI rehabilitation and enable clinicians to systematically determine areas to focus rehabilitation effort. The relative strengths and contribution to delivering person-centred care for each are identified. The SMS-NAC enables clinicians to record, for people with higher injuries, their subjective self-report of skill and knowledge gains from rehabilitation that may be missed with other measures. Consequently, using both is encouraged in appreciation of the value of recording verbal (instructional) independence as well as functional (physical) independence.
Similar content being viewed by others
Introduction
Formal measures that assess and monitor individuals’ progress through rehabilitation are increasingly utilised by clinicians as good clinical practice to demonstrate outcomes [1], and are a means of informing service-users, clinicians and policy makers about effectiveness and influencing service development [2]. Furthermore, rehabilitation measures that offer valid meaningful change can be a clinical intervention in and of itself, rather than solely an outcome tool, and aids services’ engagement of users to understand their changed health condition, set goals, support the development of self-management and facilitate adjustment [1]. Within spinal cord injury (SCI) rehabilitation, a range of measures exist that evaluate an individual’s progress with significant variation between them in the domains assessed and practical aspects of administration, training and cost [3]. Understanding the effectiveness of SCI-specific measures is vital for informing selection and application; this needs to go beyond a measure’s psychometric properties and should also consider clinical efficacy, particularly specificity to reflect the complex nature of rehabilitation progress across level and completeness of SCI.
Due to the complex nature of SCI, and diverse demands of living in the community, a biopsychosocial rehabilitation model is most commonly adopted by specialist spinal cord injury centres (SCICs). This incorporates physical, social and psychological domains to encourage individuals to gain as much independence as possible [4], and skills and knowledge from a range of clinical specialties and disciplines [5]. Outcome measures therefore need to have breadth, as well as specificity, and include physical health, functional tests, as well as tools to monitor psychological adjustment, mood and participation [6]. Through SCI rehabilitation, individuals learn to comprehend their changed health needs and in turn develop a vast array of new skills to live life well. Measures therefore need to also include ways to capture self-management skills and the knowledge progress that occurs during rehabilitation, which interacts with the significant psychological and social adjustment necessitated by injury.
Increasingly, SCI settings have adopted an inclusive person-centred approach to rehabilitation, which includes the individual in setting their goals in partnership with the clinical team [6, 8,9,10]. Equipping individuals with a role in managing their condition, facilitating a sense of control, self-efficacy and empowerment in enacting long-term change, has been found to improve adherence, satisfaction with care and greater physical gains and psycho-social adjustment during and after rehabilitation [7, 8, 10,11,12]. Consequently, outcome measures should also be able to reflect the individual’s values and priorities, and serve to involve and inform people with spinal cord injury (PwSCI), in order to develop self-management skills as part of a holistic, biopsychosocial and interdisciplinary rehabilitation [13, 14].
Rehabilitation outcome at the National Spinal Injuries Centre (NSIC) at Stoke Mandeville Hospital involves a clinician-administered Spinal Cord Independence Measure (SCIM) [15] and patient self-report assessment, the Stoke Mandeville Spinal Needs Assessment Checklist (SMS-NAC) [16,17,18,19], to measure progress and develop a process map for rehabilitation [16, 18, 19]. The former is a scale developed to assess functional independence following SCI, whilst the latter is a self-report measure that engages the patient in understanding their range of changed functional health needs, with the individual rating their knowledge and skill in a variety of SCI self-management domains. The current research aims to explore both measures and outcome across levels and completeness of SCI, to gain understanding of their clinical utility and establish a more comprehensive picture of rehabilitation progress. Moreover, given the two measures are administered concurrently, understanding the relative benefits for each assessment may lead to greater tracking of inpatient progress, enabling rehabilitation amendments to account for individual and demographic variation in outcome [20, 21].
Method
Outcome measures at the National Spinal Injuries Centre
The NSIC at Stoke Mandeville Hospital administers two distinct SCI-specific rehabilitation outcome measures in routine clinical practice to inform inpatient service-users of their starting point, needs, progress and outcomes through rehabilitation.
Spinal Cord Independence Measure III (SCIM) [22]
The SCIM is an internationally recognised measure for SCI functional assessment, used within research and rehabilitation provision [1, 23]. The SCIM includes 19 items over four domains: (a) self-care (6 items, scored 0–20); (b) respiration and sphincter management (4 items, scored 0–40); (c) mobility, room and toilet (3 items, scored 0–10); and (d) mobility, indoors and outdoors (6 items, scored 0–30). A total SCIM score is also calculated, summing the subscale scores. The higher the score on an item, the less assistance, aids or medical compromise for the task assessed to be accomplished with, meaning the higher the score, the greater the observed independence. All questions must be answered, with no N/A answers possible. Newly injured SCI inpatients were scored on the observational SCIM on admission and discharge by a multidisciplinary (MDT) meeting involving medical and nursing staff, physiotherapist, occupational therapists, clinical psychologists and case managers.
Stoke Mandeville Spinal Needs Assessment Checklist (SMS-NAC) [16, 17]
As part of the MDT goal planning framework, the evidence-based SMS-NAC was developed by Kennedy and Hamilton following user consultation and has been regularly updated according to clinical practice [17]; the current paper reports on the 2015 version, using data from 2015 to 2020. It structures a person’s skill acquisition, knowledge and rehabilitation progress across ten biopsychosocial domains: physical health (54 items), daily living activities (33 items), skin and posture management (21 items), bladder management (29 items), bowel management (16 items), mobility (28 items), wheelchair and equipment (32 items), community preparation (36 items), psychological health (40 items, including the Hospital Anxiety and Depression Scale [24], the short form of the Appraisals of DisAbility: Primary and Secondary Scale [25], the PMSnac [26]) and discharge coordination (39 items). Subtopics and items within each domain are organised hierarchically, so that items come in the order that they would be addressed during rehabilitation. In mobility, for example, ‘transfers’ is followed by ‘wheelchair skills’, which is followed by ‘ambulation’; within transfers, transfers to/from a bed comes before transfers to/from a car.
All items are scored from 0 to 3, with higher scores indicating full independence in or knowledge of that task. Independence on the SMS-NAC refers to both physical independence, in which the individual requires no other assistance from another person to physically complete a task, or verbal independence, whereby the PwSCI requires the physical assistance of at least one other person to complete a task, but has full knowledge and ability to instruct another person in that task. This means people with all levels and completeness of SCI are able to reach optimal rehabilitation outcome, achieving 100% on this scale, and enables them to visually understand their improvements across time and rehabilitation [4]. The SMS-NAC assesses both physical and verbal knowledge and skills concurrently, with each interchangeable in their contribution toward the final score, enabling the PwSCI to specify their skill level and knowledge item by item. For example, someone with a C5/6 SCI may be physically independent in upper body dressing and instruct others to dress their lower body (demonstrating verbal independence). Not all questions are appropriate to be answered by all patients. Some questions can therefore be answered with ‘N/A’, which is scored as fully independent. A percentage score is calculated for each domain, taking the sum total scored by an individual as a percentage of the maximum possible score for that domain.
The measure’s reliability and validity has been examined and approved for use in this population, and on the basis of psychometric properties and clinical utility the SMS-NAC has historically been recognised as one of the best international outcome measures [7, 27]. It is administered on admission to provide a framework for rehabilitation goal and target setting, and repeated prior to discharge to demonstrate learning and progress for users and clinicians, and identify remaining goals. The ten domains map directly onto the Goal Planning Programme, providing a measure that directly relates to person-centred goal setting [16, 18].
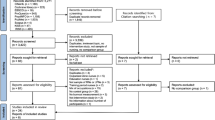
Sample
Participants included in the current study were 195 newly injured SCI inpatients participating in rehabilitation at a specialist SCIC between February 2015 and January 2020. Both the SCIM and SMS-NAC are completed twice as part of standard clinical care, at admission (within 2 weeks of admission or mobilisation, whichever was soon) and at discharge (6–4 weeks prior to discharge). They are administered routinely for all adult inpatients, except for adults with significant cognitive impairments. Only inpatients who completed both measures were included in the current review. There were no other inclusion or exclusion criteria. A total of 721 patients were admitted for rehabilitation in this period, with 526 excluded in turn for having no NAC data (n = 71), having only one NAC (n = 408), then finally for having only one SCIM (n = 44) or incomplete NAC data (n = 3).
Statistics
After summary descriptives were produced for participant demographics (Table 1), a series of Mixed ANOVAs with Bonferroni post-hoc tests were used to answer the primary research question. Mixed 2 × 3 ANOVAs (2 timepoints of admission and discharge × 3 injury groupings as described in Table 1) were performed to examine whether participants’ scores in the SCIM and SMS-NAC changed significantly over time, and whether scores in either measure were affected by injury characteristics. The change in scores over time was important to consider as one mark of responsiveness for rehabilitation outcome measures is their ability to detect change over time. Any differences in scores by injury characteristics would also elucidate the clinical utility of the measures over the full population of PwSCI. One-way ANOVAs were also run for each SMS-NAC and SCIM domain (including SCIM Total) at admission and discharge separately, split by level of injury, to clarify the main effect of group in the mixed ANOVA (which was based on the average group scores, taking the average of admission and discharge scores). This examined whether group differences existed consistently at both admission and discharge, or whether there was a significant difference between groups at only a single point in time, distorting the average. All ANOVAs were performed separately for all ten domains of the SMS-NAC, all four domains of the SCIM and total SCIM score. This enabled more detailed examination of both the ability of the measures to assess individuals’ improvement across the full range of rehabilitation, and also how the two measures might complement each other in rehabilitation outcome measurement by developing a more detailed picture of both measures. Significance was set at p < 0.05 for all tests; partial η2 of 0.01–0.059 was considered a weak effect, 0.06–0.139 a moderate effect and ≥0.14 a strong effect.
Results
Data from 195 inpatients were included in the analysis. Sample demographics and injury characteristics are displayed in Table 1. There was no significant difference between injury groupings in gender, ethnicity, cause of injury, age at injury or time between injury and rehabilitation admission. There was a significant difference between injury groupings in time in hospital (F (2,194) = 25.012, p < 0.001), whereby those with tetraplegia (A/B/C) stayed significantly longer than both other groups. The appropriateness of an ANCOVA to control for this difference was considered. However, upon examining the data, it was found that there was little to no relationship of time in hospital and the dependent variables for those with tetraplegia (A/B/C). Therefore, the assumption of homogeneity of regression was not met. Moreover, given the finding that those with significantly different stays had the least effect of length of stay on their outcomes, there did not seem a statistical rationale for including time in hospital as a covariate. Consequently, it was judged acceptable to continue with the ANOVA.
Improvement over time
In both the SMS-NAC and SCIM there was a strong and significant increase in scores from admission to discharge indicating a main effect of time for all SMS-NAC and SCIM domains, and the SCIM total score (Table 2). This indicated that PwSCI, regardless of level and completeness of injury, showed improvement in all areas during rehabilitation. Mean admission and discharge scores for each injury group across the ten SMS-NAC domains and five SCIM sub- and total scores are presented in Table 3.
In the SMS-NAC, there was an average increase of 60% across all domains. Discharge coordination saw the greatest increase (95%) and psychological health the least (13%). All domains except psychological health demonstrated an increase of more than 20%. In the SCIM, scores increased from admission to discharge by a mean of 67%, ranging from 47% (respiration and sphincter management) to 94% (mobility (room and toilet).
Level of injury group differences
In nine domains of the SMS-NAC, excluding mobility, and in all sub- and total scores of the SCIM, there was a significant main effect of level of injury (Table 2), though the effect sizes ranged from weak (partial η2 = 0.05 for SMS-NAC psychological health, the smallest effect size) to strong (partial η2 = 0.52 for SCIM self-care, the largest effect size). This indicates that there were weak to strong differences between rehabilitation scores obtained (taking the average of admission and discharge scores) based on injury level.
The trends identified in Bonferroni post-hoc tests are given in Table 4 (for full results, see Supplementary Table 1). In the SMS-NAC, main effect differences followed four main trends. In the domains of physical health, wheelchair and equipment, community preparation, psychological health and discharge coordination, people with tetraplegia (A/B/C) scored significantly lower than both people with paraplegia (A/B/C) and people with incomplete (D) injuries; there was no significant difference between the scores of those with paraplegia (A/B/C) and those with incomplete (D) injuries. In the domains of bladder and bowel management, people with tetraplegia (A/B/C) scored significantly lower than people with paraplegia (A/B/C), who scored significantly lower than people with incomplete (D) injuries. In skin management, people with tetraplegia (A/B/C) and people with paraplegia (A/B/C) scored significantly lower than people with incomplete (D) injuries; there was no significant difference between the scores of people with tetraplegia (A/B/C) and people with paraplegia (A/B/C). In activities of daily living, people with tetraplegia (A/B/C) scored significantly lower than people with incomplete (D) injuries, who scored significantly lower than people with paraplegia (A/B/C). There were no significant differences between individuals’ scores in mobility.
In the SCIM domain of self-care, people with tetraplegia (A/B/C) scored significantly lower than both people with paraplegia (A/B/C) and people with incomplete (D) injuries; there was no significant difference between the scores of those with paraplegia (A/B/C) and those with incomplete (D) injuries. In all other sub-scores and the total score of the SCIM, people with tetraplegia (A/B/C) scored significantly lower than people with paraplegia (A/B/C), who scored significantly lower than people with incomplete (D) injuries. For full results, see Supplementary Table 2.
One-way ANOVAs
As in the mixed ANOVA, there were significant between-group differences in all domains of the SMS-NAC except mobility, and in all domains and total of the SCIM. As an important extension to the mixed ANOVA, it was found that these between-group differences occurred in all domains at both admission and discharge. Table 4 summarises the patterns of group differences found when Bonferroni post-hoc tests were conducted (for full results, see Supplementary Tables 1 and 2). Of particular note was the finding that the scores obtained by people with tetraplegia (A/B/C) (Table 3) were in all cases significantly lower than the scores of at least one other group, and in most cases were significantly lower than the scores of all other PwSCI. There were fewer significant differences between the scores of people with paraplegia (A/B/C) and people with incomplete (D) injuries in the SMS-NAC (compared to the SCIM), and at discharge (compared to admission). Of the observed instances in which people with paraplegia (A/B/C) obtained greater scores than people with incomplete (D) injuries (Table 3), only one was found to be a significant difference.
Degree of improvement by level and completeness of injury
SMS-NAC
In four domains (physical health, skin and posture management, bladder management and bowel management), a moderately strong, significant interaction effect was found (partial η2 ranged from 0.06 to 0.13, p < 0.01), meaning the amount of improvement over time for the PwSCI was impacted by their level and completeness of injury (Table 5).
Bonferroni post-hoc tests were run to compare the group differences in change of score from admission to discharge. In physical health, people with tetraplegia (A/B/C) made significantly greater gains over time than both people with paraplegia (A/B/C) and people with incomplete (D) injuries. There was no significant difference between people with paraplegia (A/B/C) and individuals with incomplete (D) injuries. In skin and posture, bladder and bowel management domains, both people with tetraplegia (A/B/C) and people with paraplegia (A/B/C) made significantly greater gains over time than individuals with incomplete (D) injuries. There was no significant difference between people with tetraplegia (A/B/C) and people with paraplegia (A/B/C).
SCIM
In all domains and total SCIM (except for self-care), a weak to moderately strong, significant interaction effect was found (partial η2 ranged from 0.05 to 0.08, p < 0.01) (Table 5).
Bonferroni post-hoc tests were run to compare the group differences in change of score from admission to discharge. In respiration and sphincter management, those with tetraplegia (A/B/C) made significantly smaller gains than those with incomplete (D) injuries, who made significantly smaller gains than people with paraplegia (A/B/C). In mobility (indoors and outdoors), both those with tetraplegia (A/B/C) and those with paraplegia (A/B/C) made significantly smaller gains over time than individuals with incomplete (D) injuries. There was no significant difference between people with tetraplegia (A/B/C) and people with paraplegia (A/B/C). In mobility (room and toilet), and in SCIM total score, those with tetraplegia (A/B/C) made significantly smaller gains over time than those with paraplegia (A/B/C). There was no significance difference between individuals with incomplete (D) injuries, and both people with tetraplegia (A/B/C) and people with paraplegia (A/B/C).
In both the SMS-NAC and SCIM, PwSCI improved by different degrees during their rehabilitation depending on their injury level and completeness. However, differing patterns were observed: in the SCIM, people with high, complete injuries evidenced relatively fewer rehabilitation gains than other PwSCI; in those domains of the SMS-NAC where an effect was found, it followed the opposite trend.
Discussion
Overall, the results indicate the clinical benefit of using both the SCIM and SMS-NAC. It was found that both demonstrated significant improvements for all levels and completeness of SCI across all domains from admission to discharge. This evidences the SCIM and SMS-NAC’s clinical utility, validity and efficacy as tools able to assess a variable and complex pattern of social, psychological and physical change seen in individuals with a full range of SCI. Furthermore, both measures demonstrated sensitivity to differences between injury groupings in both overall scores and patterns of improvement, critical for meaningfully constructed rehabilitation. The relative findings of the measures, in patterns of improvement and the complimentary nature of this in line with their conceptual differences, further reinforces the validity of using multiple measures in tandem.
Utility of measures
Both measures were evidently sensitive to change over time: across all domains of the SCIM and SMS-NAC, scores increased from admission to discharge. The authors note that psychological health scores on the SMS-NAC appeared to show comparatively less improvement than other sub-scores. It is possible that scores remain comparatively more stable in the psychological health domain due to the nature of the questions: unlike other domains, the psychological health section includes a number of questions for which the answer is unlikely to change, for example whether the individual is a carer for a vulnerable adult. However, relatively little change in scores might also be due to fluctuations in mood, which does not necessarily progress in a linear fashion with rehabilitation: in particular, other studies have indicated that mood can decline in the weeks immediately prior to discharge, or for psychological symptoms to rise after an initial delay post-injury [28,29,30]. Nonetheless, the consistent improvement across all SCIM and SMS-NAC domains demonstrates the ability of the measures to capture change over time.
Both measures also demonstrate sensitivity to group differences and differences in the needs and abilities of different injury profiles. This is important for rehabilitation outcome measures, as it enables rehabilitation settings to deliver personalised care and provide more meaningful information about development for the individual [9, 11, 17]. In particular, both measures appear to capture a greater scope of rehabilitation need for individuals of higher injury levels: in all cases across the two measures, people with complete tetraplegia obtained lower scores than those with complete paraplegia and individuals with incomplete injuries. In the SCIM, this is likely due to the measures’ intention to assess physical functional independence; therefore, individuals with complete, high-level injuries obtain lower scores. In the SMS-NAC, the lower scores for people with higher injuries likely reflect the greater number of questions for this injury level, and that N/A items receive a full score in the SMS-NAC. For example, in the physical health domain, questions regarding respiratory management and autonomic dysreflexia knowledge are applicable only to those with injuries above T6; consequently, individuals with injuries below T6 are more likely to score the maximum for this section than those with injuries above. As such, the present results reflect both measures’ ability to detect the increased scope and complexity of rehabilitation for people with higher SCI, indicating their utility for effecting a responsive rehabilitation for individuals of different injury profiles and needs.
Finally, the present results also highlight key differences between the two measures, which reinforce the value of using both in tandem. In particular, though both the SCIM and the SMS-NAC found that the degree of improvement demonstrated over time differed depending on injury characteristics, the trends of these differences were reversed between the measures. Specifically, in the four domains of the SMS-NAC where an effect was found, those with high-level, complete injuries made the greatest improvements over time, whilst the SCIM found the smallest improvements demonstrated by individuals of this injury group. It is possible that the finding of greatest improvement for people with complete tetraplegia, and least improvement for people with incomplete injuries is less an interaction of time and injury, and simply to do with injury level and completeness, whereby those with incomplete injuries have less room for improvement as a result of scoring with less impairments initially. For example, it is possible that many items in the skin, bladder and bowel domains are redundant for individuals with incomplete injuries, who may be able to stand rather than require regular pressure relief, or who may not need additional bladder or bowel management methods; therefore, their scope for improvement would be reduced. Further research to clarify this would be valuable. However, it is nonetheless a significant finding from the present results that the two measures demonstrate opposite trends in degree of improvements, highlighting a conceptual difference between the measures that reinforces the value of using both in conjunction. The SCIM was designed to focus on functional assessment to define rehabilitation progress; consequently, in keeping with other research findings, those with incomplete injuries demonstrated a greater functional improvement over time [31,32,33]. The SMS-NAC, by contrast, is a measure of self-management, assessing knowledge as well as functional ability and considering verbal as well as physical independence. Consequently, the SMS-NAC is able to capture an increase in the knowledge and verbalised instructional skill of these individuals, resulting in people with complete tetraplegia making the greatest gains over time in select domains of the SMS-NAC.
Both the physical, functional improvement assessed by the SCIM and the self-management assessed by the SMS-NAC are important facets of rehabilitation for measures to address. There is increasing evidence that an individual’s perception of their control has been shown to predict subsequent life satisfaction following traumatic SCI and be associated with positive adjustment [34, 35], and that effective self-management is critical to long-term outcomes for chronic conditions [12]. The ability of the SMS-NAC to assess individual self-management (via verbalised independence) is a significant strength of this measure and enables it to be used as a self-management tool connected with goal setting for people with higher-level SCI. Moreover, the present results found that the SMS-NAC enabled people with the greatest identified need at admission to have the greatest capacity for improvement by discharge, thus reinforcing that the SMS-NAC can more fully represent the progress and outcome of individuals with higher and more complete injuries. This is particularly relevant as the demographics of PwSCI shift, with an increase in the age of PwSCI and fall-related aetiology [36]. For such individuals, with cervical injuries or additional needs associated with ageing, developing verbal instructional skills to convey how to do an activity will be essential in increasing their independence and improving long-term health outcome. Consequently, it is valuable to use both measures concurrently as, alongside their conceptual difference, this study demonstrates that this increases sensitivity and breadth needed for individually tailored rehabilitation.
Clinical implications
First, there appears to be a relatively lower ceiling on rehabilitation attainment at the point of discharge for individuals with higher level injuries. The fact that this is the case even in the SMS-NAC, where the inclusion of verbal independence should theoretically enable those with high-level injuries to achieve the same scores by discharge as those with lower-level injuries, is striking. It may be that the present results highlight the more limited opportunities of people with higher level injuries to translate their skills to community practice before discharge, which may mean they are less confident in their ability to translate skills learned in rehabilitation to community living. For example, they may have fewer opportunities to go out because of more difficulties arranging care, transportation, etc., and have less practice instructing care-givers outside of the SCIC. Such individuals may therefore obtain lower scores on the SMS-NAC as they perceive themselves to be less confident and independent. There is therefore perhaps an area for clinical improvement in the relative lack of preparation for discharge for individuals with higher level injury, suggested by the lower ceiling of rehabilitation gains found for this group.
Second, in the majority of SCIM and SMS-NAC scores, people with paraplegia scored lower than people with incomplete injuries. The fact that people with paraplegia (A/B/C) score higher than people with incomplete (D) injuries in the SMS-NAC domain of activities of daily living, and the SCIM domain of self-care, is therefore interesting. For the most part, it would appear that individuals are advantaged first by incompleteness of injury, then by lower level of injury; evidently, however, in some areas of rehab it is primarily the level of injury, and thus the degree and nature of body parts affected by the injury, that affects outcomes. For example, it is possible that these specific findings are related to hand function. The incomplete (D) injury grouping includes people with high as well as low injury levels, and thus this group might be considered to represent individuals with marginally more impaired hand function than those with paraplegia (A/B/C), where hand function is entirely intact. As both activities of daily living and self-care are the domains most directly assessing tasks of hand function, this may explain why people with paraplegia (A/B/C) in these areas score higher than individuals with incomplete (D) injuries. Consequently, the present results highlight the clinical importance of approaching different areas of rehabilitation as potentially affected by different aspects of the SCI, either the level or the completeness.
Limitations and future research
The limitations of the current study are that the sample has been selected from, and measures administered within, a single rehabilitation setting; findings may therefore lack generalisability. Moreover, the standardisation of administering the assessments may differ between spinal centres. Further research on wider samples, across a broader spectrum of rehabilitation contexts would be advantageous. A further limitation is the lack of consensus on ‘clinically meaningful change’ for PwSCI detected by assessments. Thus, more research needs to establish the ecological validity of changes on both measures with individuals own lived experiences of SCI. Finally, a large proportion of PwSCI admitted for rehabilitation did not have both measures completed at both timepoints. Though in large part this is due to clinical pressures, in particular the availability of trained staff to complete the measures and the length of patients’ admissions, it is also possible that clinical considerations such as the physical wellness of patients affected whether measures were completed. As such, although the final sample was judged sufficient for statistical analysis, it is possible that the results are not entirely representative of the full SCIC.
It was also observed that demographic differences existed between the injury groupings. For example, there was great variation between each three groups in the length of time between injury and rehabilitation admission. This was judged to be due to both acute care needs (those with higher-level injuries staying in acute care centres for longer before transferring to the rehabilitation centre than those with lower-level injuries) and limited rehabilitation needs (those with low level, very incomplete injuries, such as those with Cauda Equina Syndrome, often being discharged to the community for long periods before SCIC rehabilitation). Such group differences were not considered likely to affect the present results. In particular, it was judged that these differences in time elapsed suggested that participants would have reached similar rehabilitation start points by admission, with greater or lesser time in acute care or the community to enable this. However, the findings highlight that there may be demographic, as well as functional, characteristics of different injury profiles that warrant further research, particularly in influencing rehabilitation outcomes.
Finally, the present results give an initial indication of the utility of the SCIM and SMS-NAC in a rehabilitation context. Further research could valuably consider the utility of these measures beyond the rehabilitation environment, for example in examining community need after discharge or before admission, as would be particularly relevant for those individuals evidenced in the present sample to have a long delay before admission. Similarly, extending the timeframe of analysis beyond rehabilitation would allow for examination of the predictive utility of the measures, which would further inform use of them clinically.
Conclusion
Many rehabilitation outcome measures exist for use within an SCI population. Standardising use of these measures offers an opportunity to establish a common language accessible to newly injured inpatients, their families and clinical professionals, and impact, as well as promote, a consistent approach and cross-comparison of service effectiveness. The current study highlights the relevance of using both the SCIM and SMS-NAC as efficacious, sensitive and complimentary rehabilitation outcome measures. In line with previous research, both measures demonstrate a significant change over the course of SCI rehabilitation, reinforcing their validity in assessing rehabilitation progress, for individuals with all injury levels and injury completeness. Moreover, both demonstrate sensitivity to differences according to injury level. Due to the heterogeneous nature of SCI population, having measures capable of assessing difference, in order to provide rehabilitation most appropriate to the needs and strengths of individuals with different injury profiles, is essential. Finally, the study reinforces the use of both the MDT-led functional assessment (SCIM) and inpatient self-reported outcome (SMS-NAC) in tandem, for both the patterns held in common and the patterns of difference.
Data availability
The datasets generated and/or analysed during the current study are part of a standard clinical database that contains patient identifiable information and are therefore not publicly available. Pseudonymised data can be made available on reasonable request to Buckinghamshire Healthcare NHS Trust.
References
Alexander MS, Anderson KD, Biering-Sorensen F, Blight AR, Brannon R, Bryce TN, et al. Outcome measures in spinal cord injury: recent assessments and recommendations for future directions. Spinal Cord. 2009;47:582–91. https://doi.org/10.1038/sc.2009.18.
Chan CW, Miller WC, Querée M, Noonan VK, Wolfe DL, SCIRE Research Team The development of an outcome measures toolkit for spinal cord injury rehabilitation: création d’une trousse de mesures des résultats pour la réadaptation des personnes ayant subi une lésion de la moelle épinière. Can J Occup Ther. 2017;84:119–29. https://doi.org/10.1177/0008417417690170.
Stevens A, Beurskens A, Köke A, van der Weijden T. The use of patient-specific measurement instruments in the process of goal-setting: a systematic review of available instruments and their feasibility. Clin Rehabil. 2013;27:1005–19. https://doi.org/10.1177/0269215513490178.
Byrnes M, Beilby J, Ray P, McLennan R, Ker J, Schug S. Patient-focused goal planning process and outcome after spinal cord injury rehabilitation: quantitative and qualitative audit. Clin Rehabil. 2012;26:1141–9. https://doi.org/10.1177/0269215512442669.
Coulter A, Entwistle VA, Eccles A, Ryan S, Shepperd S, Perera R. Personalised care planning for adults with chronic or long‐term health conditions. Cochrane Database Syst Rev. 2015;2015:CD010523 https://doi.org/10.1002/14651858.CD010523.pub2.
Wade DT. What is rehabilitation? An empirical investigation leading to an evidence-based description. Clin Rehabil. 2020;34:571–83. https://doi.org/10.1177/0269215520905112.
Berry C, Kennedy P. A psychometric analysis of the Needs Assessment Checklist (SMS-NAC). Spinal Cord. 2003;41:490–501. https://doi.org/10.1038/sj.sc.3101460.
Stucki G, Cieza A, Melvin J. The international classification of functioning, disability and health: a unifying model for the conceptual description of the rehabilitation strategy. J Rehabil Med. 2007;39:279–85. https://doi.org/10.2340/16501977-0041.
Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff (Millwood). 2001;20:64–78. https://doi.org/10.1377/hlthaff.20.6.64.
Eaton S, Roberts S, Turner B. Delivering person centred care in long term conditions. BMJ. 2015;350:h181. https://doi.org/10.1136/bmj.h181.
van Diemen T, Scholten EW, van Nes IJ, Geertzen JH, Post MW, SELF-SCI Group. Self-management and self-efficacy in patients with acute spinal cord injuries: protocol for a longitudinal cohort study. JMIR Res Protoc. 2018;7:e68 https://doi.org/10.2196/resprot.8054.
Schmittdiel J, Mosen DM, Glasgow RE, Hibbard J, Remmers C, Bellows, J. Patient Assessment of Chronic Illness Care (PACIC) and improved patient-centered outcomes for chronic conditions. J Gen Intern Med. 2008;23:77–80. https://doi.org/10.1007/s11606-007-0452-5.
Yoshida KK, Self HM, Renwick RM, Forma LL, King AJ, Fell LA. A value-based practice model of rehabilitation: consumers’ recommendations in action. Disabil Rehabil. 2015;37:1825–33. https://doi.org/10.3109/09638288.2014.981301.
van Diemen T, van Nes I, van Laake-Geelen C, Spijkerman D, Geertzen J, Post M. Learning self-care skills after spinal cord injury: a qualitative study. Submitted for publication.
Catz A, Itzkovich M, Agranov E, Ring H, Tamir A. SCIM–Spinal Cord Independence Measure: a new disability scale for patients with spinal cord lesions. Spinal Cord. 1997;35:850–6. https://doi.org/10.1038/sj.sc.3100504.
Duff J, Evans MJ, Kennedy P. Goal planning: a retrospective audit of rehabilitation process and outcome. Clin Rehabil. 2004;18:275–86. https://doi.org/10.1191/0269215504cr720oa.
Kennedy P, Duff J. Stoke Mandeville Spinal Needs Assessment Checklist, version 2015. bht.nsicpsychology@nhs.net. Accessed 2015.
Kennedy P, Hamilton LR. The needs assessment checklist: a clinical approach to measuring outcome. Spinal Cord. 1999;37:136–9. https://doi.org/10.1038/sj.sc.3100745.
Goodwin-Wilson C, Watkins M, Gardner-Elahi C. Developing evidence-based process maps for spinal cord injury rehabilitation. Spinal Cord. 2010;48:122–7. https://doi.org/10.1038/sc.2009.94.
Kennedy P, Hasson L. An audit of demographics and rehabilitation outcomes in non-traumatic spinal cord injury. Spinal Cord. 2016;54:1020–4. https://doi.org/10.1038/sc.2016.12.
Kennedy P, Kilvert A, Hasson L. Ethnicity and rehabilitation outcomes: the needs assessment checklist. Spinal Cord. 2015;53:334–9. https://doi.org/10.1038/sc.2015.14.
Itzkovich M, Gelernter I, Biering-Sorensen F, Weeks C, Laramee MT, Craven BC, et al. The Spinal Cord Independence Measure (SCIM) version III: reliability and validity in a multi-center international study. Disabil Rehabil. 2007;29:1926–33. https://doi.org/10.1080/09638280601046302.
Itzkovich M, Shefler H, Front L, Gur-Pollack R, Elkayam K, Bluvshtein V, et al. SCIM III (Spinal Cord Independence Measure version III): reliability of assessment by interview and comparison with assessment by observation. Spinal Cord. 2018;56:46–51. https://doi.org/10.1038/sc.2017.97.
Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
Dean RE, Kennedy P. Measuring appraisals following acquired spinal cord injury: a preliminary psychometric analysis of the appraisals of disability. Rehabil Psychol. 2009;54:222–31. https://doi.org/10.1037/a0015581.
Kennedy P, Scott-Wilson U, Sandhu N. The psychometric analysis of a brief and sensitive measure of perceived manageability. Psychol Health Med. 2009;14:454–65. https://doi.org/10.1080/13548500903012848.
Dawson J, Shamley D, Jamous MA. A structured review of outcome measures used for the assessment of rehabilitation interventions for spinal cord injury. Spinal Cord. 2008;46:768–80. https://doi.org/10.1038/sc.2008.50.
Kennedy P, Rogers BA. Anxiety and depression after spinal cord injury: a longitudinal analysis. Arch Phys Med Rehabil. 2000;81:932–7. https://doi.org/10.1053/apmr.2000.5580.
Bonanno G, Kennedy P, Galatzer-Levy IR, Lude P, Elfström M. Trajectories of resilience, depression, and anxiety following spinal cord injury. Rehabil Psychol. 2012;57:236–47. https://doi.org/10.1037/a0029256.
Craig A, Tran Y, Guest R, Middleton J. Trajectories of self-efficacy and depressed mood and their relationship in the first 12 months following spinal cord injury. Arch Phys Med Rehabil. 2019;100:441–7. https://doi.org/10.1016/j.apmr.2018.07.442.
Anderson K, Aito S, Atkins M, Biering-Sørensen F, Charlifue S, Curt A, et al. Functional recovery measures for spinal cord injury: an evidence-based review for clinical practice and research. J Spinal Cord Med. 2008;31:133–44. https://doi.org/10.1080/10790268.2008.11760704.
Catz A, Itzkovich M, Agranov E, Ring H, Tamir A. The Spinal Cord Independence Measure (SCIM): sensitivity to functional changes in subgroups of spinal cord lesion patients. Spinal Cord. 2001;39:97–100. https://doi.org/10.1038/sj.sc.3101118. PMID: 11402366.
Wirth B, van Hedel HJ, Kometer B, Dietz V, Curt A. Changes in activity after a complete spinal cord injury as measured by the Spinal Cord Independence Measure II (SCIM II). Neurorehabil Neural Repair. 2008;22:279–87. Erratum in: Neurorehabil Neural Repair. 2008;22:769.
Chase BW, Cornille TA, English RW. Life satisfaction among persons with spinal cord injuries. J Rehabil. 2000;66:14–20.
Schmitt MM, Elliott TR. Verbal learning ability and adjustment to recent-onset spinal cord injury. Rehabil Psychol. 2004;49:288–94. https://doi.org/10.1037/0090-5550.49.4.288.
McCaughey EJ, Purcell M, McLean AN, Fraser MH, Bewick A, Borotkanics RJ, et al. Changing demographics of spinal cord injury over a 20-year period: a longitudinal population-based study in Scotland. Spinal Cord. 2016;54:270–6. https://doi.org/10.1038/sc.2015.167.
Acknowledgements
Thanks to the patients and staff of the National Spinal Cord Injuries Centre, Stoke Mandeville Hospital, Buckinghamshire Healthcare NHS Trust, for completion of the standard clinical outcome tools (SMS-NAC and SCIM) that facilitated this research.
Funding
The data used in this study are part of routine clinical practice outcome measurement and analysis; as such, no additional funding was required.
Author information
Authors and Affiliations
Contributions
RE was responsible for designing the research protocol, identifying eligible participants, extracting data, and writing the report. JD was responsible for designing the research protocol, contributed to interpreting the results, and writing the report. MW contributed to the identification of eligible participants, and was responsible for extracting and analysing data, interpreting results, and writing the report. KJ contributed to designing the research protocol and provided feedback on the report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The authors certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Eaton, R., Duff, J., Wallace, M. et al. The value of the whole picture: rehabilitation outcome measurement using patient self-report and clinician-based assessments after spinal cord injury. Spinal Cord 60, 71–80 (2022). https://doi.org/10.1038/s41393-021-00677-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-021-00677-7