Abstract
Study design
Retrospective cohort study.
Objectives
To evaluate the effects of older age at the time of injury on the individuals’ survival and neurological recovery within the first year after acute traumatic spinal cord injury (tSCI).
Setting
United States.
Methods
This study included all participants enrolled into the First National Acute Spinal Cord Injury Study (NASCIS-1). Outcome measures included survival and neurological recovery (as assessed using the NASCIS motor and sensory scores) within the first year after tSCI. Data analyses of neurological recovery were adjusted for major potential confounders.
Results
The study included 39 females and 267 males with overall mean age of 31 years who mostly sustained cervical severe tSCI after motor vehicle accidents or falls. Survival rates among older individuals are significantly lower than among younger individuals within the first year following tSCI (p < 0.0001). Among who survived the first year of tSCI, there were no statistically significant difference between older survivors and younger survivors regarding motor and sensory recovery in the multiple regression analyses adjusted for major potential confounders.
Conclusions
The results of this retrospective study suggest that older age at the injury onset is associated with lower survival rate within the first year following tSCI. However, older individuals have similar potential to recover from their initial neurological impairment to younger individuals after tSCI. The results of this study combined to the recent literature underline the need for multidisciplinary team approach to the management of the elderly with acute SCI is essential to maximize their recovery.
Similar content being viewed by others
Introduction
Traumatic spinal cord injury (tSCI) can cause motor, sensory, and autonomic deficits to individuals and result in considerable economic burden to them and to society. The global incidence of tSCI varies from 6.2 to 174 per million inhabitants yearly, and its worldwide prevalence ranges from 50 to 906 per million inhabitants [1]. While tSCI has a relatively modest incidence, its burden is substantial. In Canada, the estimated lifetime costs per individual with tSCI vary from USD$ 1.17 million for incomplete paraplegia to USD$ 2.35 million for complete tetraplegia [2].
Aging population is a worldwide phenomenon that has had a considerable impact on the epidemiology of many diseases including tSCI. Several investigators documented an escalation of fall-related SCI in the geriatric population over the past decades, even though their prevalence appears to be unchanged due to the relatively higher mortality rates in the elderly after tSCI [3,4,5]. For the elderly who survives tSCI, there may follow many challenges with regards to secondary medical conditions in addition to their many pre-existing medical co-morbidities [6]. Caring for the older individuals with tSCI is relatively more expensive than, but similarly effective to, their younger counterparts [7]. While the mean total hospital costs for initial admission after acute spine trauma in the elderly is usually greater than in younger individuals, the former typically has significantly lower per diem total, fixed, direct, and indirect costs for management spine trauma than the latter [8]. The proportion of services utilized in the acute care hospital for caring for elderly patients with acute spine trauma were reportedly similar to their younger counterparts [8].
With this background, there has been an increasing interest in studying the impact of older age at the time of injury on the outcomes of individuals following acute tSCI. This retrospective cohort study examined the potentials effects of older age at the time of injury onset on the individuals’ survival and neurological recovery within the first year after tSCI using high-quality data from a prospectively accrued database.
Methods
The Institutional Ethics Board approved the use of database from the First National Acute Spinal Cord Injury Study (NASCIS-1) to address research questions other than the original aims of the clinical trial.
This retrospective cohort study included all 306 individuals who were enrolled in the NASCIS-1 trial, which was designed to compare the efficacy of a “high dose” of methylprednisolone (i.e., bolus of 1000 mg of MPSS and daily thereafter for 10 days) with a “standard dose” of MPSS (i.e., bolus of 100 mg and daily thereafter for 10 days) in the management of patients with acute tSCI [9]. All participants in the NASCIS-trial entered in the study between February 1979 and November 1981 in one of the nine hospitals from seven American states, including six specialized spinal cord centers. The chief and as senior neurosurgeon of the Department of Neurosurgery from each participating hospital were responsible for the study. The coordinating center was based in the Department of Epidemiology and Public Health at Yale Medical School (New Haven, CT). Individuals with acute tSCI at the age of 14 years or older were considered eligible for the NASCIS-1 trial and consecutively recruited to the NASCIS-1 trial. Individuals who were admitted in a participant center more than 48 h after the injury, and individuals with “severe comorbidities” or other specific reasons (“including a history of diabetes, severe vascular disease, concurrent infection, gastrointestinal tract bleeding and pregnancy”) were excluded. Inclusion and exclusion criteria are entirely documented elsewhere [9].
Baseline data
The NASCIS-1 database includes information on the individuals’ demographics (i.e., age at the time of tSCI; and sex), causes of tSCI (i.e., “fall”; “missile”; motor vehicle accident that includes “automobile accidents” and “motorcycle accidents”; “water related”, others that include “crush” and “unknown”; and “missing”), ethnic groups (i.e., “black”; “white”; and others including “Hispanics” and “Orientals”), level of consciousness at admission (i.e., “normal” and “abnormal”), and type of wound (i.e., “open” and “closed”).
The degree of severity of tSCI was classified from A (i.e., complete motor and sensory impairment) to E (i.e., complete return of all motor and sensory function, but still have abnormal reflexes) using Frankel grades, which has many similarities to the most currently used ASIA Impairment Scale [10]. The level of tSCI was classified as “tetraplegia/tetraparesis”, “paraplegia/paraparesis”, and “minor neurological deficits without specified level”.
Outcome measures
Survival data were analyzed for the first year after tSCI. The degree of impairment was assessed using the NASCIS motor and sensory scores in all individuals at admission in the emergency department and at 1-year post-tSCI. The NASCIS motor score was established by assessing motor function in 14 segments bilaterally, using a manual muscle scoring system as follows: (1) for normal function; (2) for reduced function but active movement against resistance; (3) for active movement with antigravity; (4) for active movement with antigravity; (5) for some trace of contraction; or (6) for no muscle contraction [9]. The NASCIS motor scores varied from 14 (all normal motor responses) to 84 (no contraction in any muscle) [9]. The NASCIS sensory score was determined by testing pinprick and light touch sensation in each dermatome from C2 to S5 bilaterally. Each sensory response was classified as (1) if normal response, (2) if decreased, or (3) if absent. Each sensory score varied from 29 (all normal sensory responses) to 87 (all absent sensory responses) [9].
Neurological recovery at 1 year after tSCI was determined by subtracting the baseline NASCIS score at admission from the follow-up NASCIS score at 1-year post-injury and, hence, a negative neurological recovery score represents improved function whereas a positive score characterizes decreased function.
Study groups and sensitivity analyses
Elderly group was primarily defined as individuals with 65 years of age or older at the time of tSCI onset. In a series of sensitivity analyses, other two threshold values were used to define elderly group as follows: (a) 55 years of age; and (b) 45 years of age.
Further sensitivity analyses were carried out imputing hypothetical data to replace missing data on the 1-year follow-up Frankel grades. In the “best scenario” sensitivity analysis, all cases with missing data were supposedly assumed to have improved at least one-degree improvement in the Frankel score from baseline to 1-year follow-up assessment. For the “worst scenario” sensitivity analyses, all cases with missing data were theoretically considered as they have had no improvement in the Frankel grade from the baseline to 1-year follow-up assessment.
Data analysis
Both age-related groups were statistically compared regarding their baseline data using Mann–Whitney U test (for continuous variables), and Fisher exact test or Chi-square test (for categorical variables).
Survival analysis was carried out using univariate analysis (Fisher exact test) and Kaplan–Meier curve with log-rank test.
Multiple regression analyses evaluated the potential effects of the older age on the neurological recovery (i.e., motor and sensory recovery) at 1 year after tSCI. Those multiple regression analyses were adjusted for major potential confounders including the individuals’ sex, ethnic group, level of SCI, cause of injury, type of wound, level of consciousness at admission, and total received dose of MPSS. Similarly, multiple regression analyses were used for neurological recovery (i.e., motor and sensory recovery) as the dependent variable, and age groups dichotomized into “older” (65 years of age or older) and “younger” individuals as independent variables. Those models were adjusted for the same major potential confounders as above listed.
Finally, multiple logistic analyses were used to evaluate whether improved neurological recovery (defined as at least one-grade improvement in the 1-year follow-up Frankel grading) was associated with age at the tSCI onset after adjusting for the same major potential confounders. Similar multiple logistic regression studies were performed for the “worst scenario” and “best scenario” sensitivity analyses.
Significance was assumed at p < 0.05. All data analyses were carried out using SAS software version 9.4.
Results
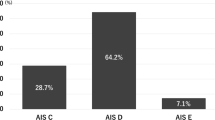
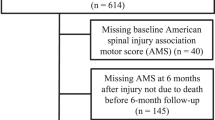
The study included 306 individuals (39 females and 267 males) with a mean age of 31 years (age range, 14–81 years) who sustained paraplegia (36.60%), tetraplegia (34.98%), tetraparesis (11.75%), paraparesis (6.23%), or minimal neurological deficit (10.28%). Of the 306 individuals with acute tSCI enrolled in the NASCIS-1 trial, there were 13 older individuals and 293 younger individuals who were statistically comparable regarding sex distribution, level and severity of tSCI, individuals’ level of consciousness at admission, and total received dose of MPSS in the acute stage after tSCI (Table 1). There was a trend toward a greater proportion of white individuals with open wounds after a tSCI caused by missile and water-related accidents among younger individuals, which did not reach statistical significance (Table 1).
Survival analysis
Using univariate analyses, the 1-year mortality rate among individuals with 65 years of age or older was significantly higher than among younger individuals after acute sSCI (53.85% versus 8.53%; P < 0.01). Similarly, the 1-year mortality rate among older individuals with 55 years of age or older was significantly greater than among younger individuals following acute tSCI (46.15% versus 7.14%; P < 0.01). Likewise, the 1-year mortality rate among individuals with 45 years of age or older was significantly higher than among younger individuals after acute tSCI (35.71% versus 4.80%; P < 0.01).
Survival analyses using Kaplan–Meier curve and log-rank test showed that the survival rate among individuals with 65 years of age or older was significantly lower than among young individuals within the first year after tSCI (P < 0.01; Fig. 1A). Similarly, survival rate among individuals with 55 years of age or older was significantly lower than among younger individuals within the first year following tSCI (P < 0.01; Fig. 1B). Likewise, survival rate among individuals with 45 years of age of older was significantly lower than among younger individuals within the first year after tSCI (P < 0.01; Fig. 1C).
Neurological recovery
Among survivors, older age at the tSCI onset (as a continuous variable) was significantly associated with better motor at 1 year after injury (P < 0.01; Fig. 2A), even after adjusting for major potential confounders (Table 2). In addition, there was a trend toward an association of older age with improved sensory recovery at 1 year after tSCI (P = 0.06; Fig. 2B), even after adjusting the model for major potential confounders (Table 2).
When the variable age at the tSCI onset was dichotomized, the results of the multiple regression analysis showed that older age (65 years of age or older) was not significantly associated with motor or sensory recovery at 1 year following acute tSCI (Table 3).
Finally, improved neurological recovery defined as at least one-grade enhancement in the Frankel grading from the baseline to the 1-year follow-up assessment was not adversely affected by individuals’ age at the tSCI onset in a multiple logistic regression analysis adjusted for major potential confounders (Table 4). Similar results would be obtained in the “worst scenario” sensitivity analysis when missing data on the 1-year follow-up Frankel grading was hypothetically assumed to be unchanged from the baseline assessment (Table 4). Nonetheless, the results of the “best scenario” analysis indicated that older age at the tSCI onset would be associated with significantly improved neurological recovery if hypothetically there was an improvement of at least one-grade in the 1-year follow-up Frankel grading in all cases with missing follow-up assessments (Table 4).
Discussion
The results of this retrospective cohort study indicated that survival rates among older individuals are significantly lower than among younger individuals within the first year following acute tSCI, regardless of the age threshold between 45 and 65 years at the tSCI onset. Among the survivors, older age as a continuous variable was associated with statistically significant greater motor recovery at 1 year after acute tSCI in the multiple regression analyses adjusted for major potential confounders. Of note, there was a trend toward an association between age and sensory recovery at 1 year after tSCI. Among those who survived the first year of tSCI, there were no statistically significant differences between survivors with 65 years of age or older at the injury onset and younger survivors with regards to motor and sensory recovery at 1 year following acute tSCI in the multiple regression analyses adjusted for major potential confounders. Using a multiple logistic regression analysis adjusted for major potential confounders, age at the tSCI onset was not significantly associated with at least one-grade neurological improvement using Frankel grading from the baseline to the 1-year follow-up assessment. Similar results would be obtained in the “worst scenario” sensitivity analysis, while the results of the “best scenario” sensitivity analyses suggested that age would be associated with better neurological outcomes if all missing data were putatively considered as there was at least one-grade neurological improvement.
Age and survival after acute traumatic spinal cord injury
The results of this study indicated that the mortality rates among older individuals were between 6.3 and 7.4-fold higher than younger individuals within the first year following acute tSCI, depending upon the age threshold used between 45 and 65 years. Those results are consistent with the worldwide literature regarding the effects of age on survival after tSCI. In a retrospective cohort study including 1995 cases of tSCI (1993–2003), Varma et al. reported that increasing age by 20 years with odds ratio of 1.2 was significantly associated with in-hospital mortality after adjusting for other covariates in the United States [11]. Using data from 499 individuals with tSCI who were enrolled in the NASCIS-3 trial (1991–1995), the results of another retrospective study indicated that older age at the time of injury was significantly associated with increased mortality rates at a hazard ratio of 1.05 [12]. The results of a retrospective study using data from the NASCIS-2 trial revealed that the mortality rate among elderly individuals was 9.6-fold higher than among younger individuals within the first year after acute tSCI [13]. In another retrospective cohort study including 595 individuals with tSCI (1997–2007), Sabre et al. documented that the relative risk of death within the first 2 years after tSCI increased by 5% for every year of age at the time of injury in Estonia [14]. Using data from the US Nationwide Inpatient Sample databases with 63,109 cases of acute tSCI (1993–2012), Jain et al. found that older age at the time of injury was associated with increased in-hospital mortality rates [3]. In a single-institution retrospective study including 665 cases of tSCI (1990–2012), the 2-, 5-, and 10-year survival rates were lower among individuals with 60 years of age or older than younger individuals after tSCI in Denmark [15]. Using data from the Swiss Spinal Cord Injury including 2421 individuals with tSCI (1990–2011), Chamberlain et al. also found that older age was associated with higher mortality following tSCI [16]. Using data from a Japanese nationwide trauma registry with 7622 cases of tSCI (2004–2015), Shibahashi et al. reported that older individuals at the time of injury were at a greater risk of in-hospital death than younger individuals [17]. Analyzing data from a Victorian State Trauma Registry with 706 cases of tSCI (2007–2016), Beck et al. documented that the mortality rates among individuals with 65 years of age or older at the time of injury were significantly higher than among younger individuals in Australia [18]. In a recently published population-based study using an administrative database (2006–2016), Li et al. found that individuals with 65 years of age or older had the greatest mortality rate among other age groups in China [19].
While there is a growing body of evidence suggesting that older age at the time of injury is associated with higher mortality after tSCI, the reasons for this association remain incompletely understood. In a prior retrospective analysis of 297 cases of tSCI from a single institution, pre-existing medical co-morbidities were found to be a major confounder, accounting for most of age-related variances in mortality after tSCI [20]. Ageistic attitudes have been recognized a significant source of age-related disparities in access to healthcare services and in health outcomes. In a cross-sectional observational study among nurses caring for patients with tSCI, fewer ageist attitudes were associated with a higher level of education and working in the rehabilitation setting when compared with working in the acute spine trauma center [21]. In another cross-sectional study comparing clinicians, neuroscientists, and allied-health professionals, females and clinicians showed more positive attitudes toward older people [22]. A recently published study using data from a participant institution in the Surgical Trial in Acute Spinal Cord Injury Study (STASCIS) revealed no significant age bias in the waiting time for each step in the surgical management of acute cervical tSCI [23]. Nonetheless, further investigations are required to examine the effects of ageism on outcomes after tSCI and to explore other potential reasons for those age-related differences in mortality following tSCI.
Age and neurological recovery after acute traumatic spinal cord injury
Among the survivors, older age as a continuous variable was associated with better motor recovery, and there was a trend toward better sensory recovery, at 1 year after acute tSCI after adjusting for major potential confounders. Potential explanations for a better neurological recovery in the older survivors when compared to younger survivors would include, for instance, discrepancies in the most common mechanism of injuries (e.g., lower-energy trauma such as fall versus higher-energy trauma such as motor vehicle accidents, respectively), the presence of associated body injuries (e.g., single-site trauma versus polytrauma, respectively), and underlying spine disease (e.g., pre-existing spinal canal stenosis in the older individuals). However, the elderly group showed no statistically significant differences regarding motor and sensory recovery when compared to younger individuals at 1 year following acute tSCI.
Those results challenge the presumption that elderly individuals typically have less favorable neurological outcomes after acute tSCI. This is congruent with the emerging evidence suggesting that the geriatric population has potential to recover as much as the younger individuals if they have access to proper acute and rehabilitation services. For instance, Lau et al. reported that a selected group of individuals with 70 years of age or older at the time of injury had similar neurological recovery to younger individuals after aggressive surgical and intensive care treatment for acute tSCI [24]. Using data from the NASCIS-2 trial, the results of a retrospective cohort study with 485 individuals with acute tSCI indicated that age at the time of injury was not significantly associated with motor and sensory outcomes at 6 weeks, 6 months, and 1-year post-tSCI after adjusting for major potential confounders [13]. Also, a neuroanatomical analysis of post-mortem spinal cord tissue (including 7 cases of tSCI and 5 control cases without history of CNS trauma or disease) revealed no significant age-related differences for extent of myelin degeneration or number of intact axons within sensory, motor, and autonomic spinal cord tracts following tSCI [13]. In another retrospective study using data from the NASCIS-3 trial (n = 499), older age at the time of injury was not significantly associated with motor recovery or changes in pain score, but older age was associated with better sensory recovery at 6 weeks, 6 months, and 1-year post-tSCI after adjusting for major potential confounders [12]. Yet, there was no significant correlation between individuals’ age at the time of injury and their degree of disability as assessed using Functional Independence Measure (FIM) at 1-year post-tSCI [12]. Similarly, the results of a pilot retrospective study (including 30 patients with tSCI or non-traumatic SCI) showed no significant association between their age at the time of injury and functional recovery (as assessed using FIM and Spinal Cord Independence Measure [SCIM]) during initial inpatient treatment in a tertiary rehabilitation center [25]. Moreover, the results of a unique histopathological and immunohistochemical study of post-mortem spinal cord tissue (including 64 cases of tSCI and 48 control cases without history of CNS trauma or disease) indicated that age at the tSCI onset did not adversely affect the cellular inflammatory response to, oligodendroglial apoptosis and axonal survival following tSCI [26].
Study limitations
This retrospective study examined a large dataset from the NASCIS-1 trial that included data on multiple relevant potential confounders. Nevertheless, there are limitations that should be taken into account when interpreting and applying the results of this study. First, the retrospective nature of the study did not allow inclusion of other potential confounders. For example, pre-existing medical co-morbidities could influence not only on survival but also recovery after acute tSCI [20]. In addition, polypharmacy and rehabilitation intensity can have an impact on the neurological outcomes following acute tSCI [27, 28]. Also, altered level of consciousness on admission due to concomitant traumatic brain injury could affect the neurological recovery after tSCI, even though this remains understudied. In this study, data on the level of consciousness were limited to two categories (i.e., “normal” and “abnormal”) which precluded an in-depth data analysis using Glasgow Coma Scale, for example. Second, the participants were enrolled in the NASCIS-1 trial between 1979 and 1981 when the standard of care could be different from the current guidelines in some aspects of the pre-hospital, acute spine care, and rehabilitation practices. For instance, maintenance of spinal cord perfusion by properly managing mean arterial pressure (≥85 mmHg), preoperative evaluation using MRI, and early decompression of spinal cord have lately become the best practices in the management of patients with acute tSCI [29, 30]. While those discrepancies in the management of individuals with acute tSCI could limit the application of those results in the current clinical practice, this study represented an unique opportunity to evaluate the effects of age at the injury time on outcomes of patients after acute tSCI who were managed four decades ago under different standard of care from the current practice guidelines. Third, the negative results in comparisons between older individuals (n = 13) and younger individuals (n = 293) could be due to a type-II error in the data analyses. However, the results from the multiple regression analyses using age at the tSCI onset as a continuous variable endorsed those negative results when adjusted for major potential confounders. Fourth, there were no available data in the NASCIS-1 database to clarify the reasons why elderly individuals had a higher mortality rate than younger individuals after tSCI. As above mentioned, pre-existing medical co-morbidities and ageistic attitudes can have an important impact on the survival after tSCI. Moreover, one could speculate that elderly individuals who died within the first year after tSCI had a different degree of neurological recovery from those elderly individuals who survived, which could influence the results of this study. While this information is not available in the NASCIS-1 database for a subgroup analysis, further data analysis suggested that the elderly individuals who died within the first year following tSCI had more severe tSCI than those ones who survived (motor complete tSCI: 100% versus 33.3%, respectively, p = 0.02) at admission. Notably, both subgroups were statistically comparable with regards to their level and cause of tSCI (p = 0.27 and p = 0.44, respectively). Finally, all participants in the NASCIS-1 trial received MPSS that could have a different age-related neuroprotective effect after acute tSCI.
Conclusions
The results of this retrospective cohort study suggest that older age at the injury onset is associated with lower survival rate within the first year following acute tSCI. However, older individuals have similar potential to recover from their initial neurological impairment to younger individuals after acute tSCI. Those results confirm the literature that has consistently documented higher mortality rates in the elderly population after tSCI, which underscore the need for further investigations to determine other causes for this age-related discrepancy in survival post-tSCI beyond pre-existing medical co-morbidities and the negative effects of ageism. Among the survivors, the results of the present study are relevant to the emerging evidence in the literature suggesting that elderly individuals have the potential to recover from neurological impairment after tSCI similarly to their younger counterparts. Those findings challenge the preconception that geriatric population would have less favorable neurological outcomes after tSCI and also reinforce the need for multidisciplinary team approach to the management of the elderly with acute SCI in order to maximize their recovery.
Data availibity
Data access should be directly requested to the Yale University that led the NASCIS-1 trial.
References
Furlan JC, Sakakibara BM, Miller WC, Krassioukov AV. Global incidence and prevalence of traumatic spinal cord injury. Can J Neurol Sci. 2013;40:456–64.
Krueger H, Noonan VK, Trenaman LM, Joshi P, Rivers CS. The economic burden of traumatic spinal cord injury in Canada. Chronic Dis Inj Can. 2013;33:113–22.
Jain NB, Ayers GD, Peterson EN, Harris MB, Morse L, O’Connor KC, et al. Traumatic spinal cord injury in the United States, 1993–2012. JAMA. 2015;313:2236–43.
Kattail D, Furlan JC, Fehlings MG. Epidemiology and clinical outcomes of acute spine trauma and spinal cord injury: experience from a specialized spine trauma center in Canada in comparison with a large national registry. J Trauma. 2009;67:936–43.
Devivo MJ. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord. 2012;50:365–72.
Krassioukov AV, Furlan JC, Fehlings MG. Medical co-morbidities, secondary complications, and mortality in elderly with acute spinal cord injury. J Neurotrauma. 2003;20:391–9.
Furlan JC, Craven BC, Fehlings MG. Surgical management of the elderly with traumatic cervical spinal cord injury: a cost-utility analysis. Neurosurgery. 2016;79:418–25.
Furlan JC, Fehlings MG, Craven BC. Economic impact of aging on the initial spine care of patients with acute spine trauma: from bedside to teller. Neurosurgery. 2019;84:1251–60.
Bracken MB, Collins WF, Freeman DF, Shepard MJ, Wagner FW, Silten RM, et al. Efficacy of methylprednisolone in acute spinal cord injury. JAMA. 1984;251:45–52.
Furlan JC, Fehlings MG, Tator CH, Davis AM. Motor and sensory assessment of patients in clinical trials for pharmacological therapy of acute spinal cord injury: psychometric properties of the ASIA Standards. J Neurotrauma. 2008;25:1273–301.
Varma A, Hill EG, Nicholas J, Selassie A. Predictors of early mortality after traumatic spinal cord injury: a population-based study. Spine. 2010;35:778–83.
Furlan JC, Fehlings MG. The impact of age on mortality, impairment, and disability among adults with acute traumatic spinal cord injury. J Neurotrauma. 2009;26:1707–17.
Furlan JC, Bracken MB, Fehlings MG. Is age a key determinant of mortality and neurological outcome after acute traumatic spinal cord injury? Neurobiol Aging. 2010;31:434–46.
Sabre L, Rekand T, Asser T, Korv J. Mortality and causes of death after traumatic spinal cord injury in Estonia. J Spinal Cord Med. 2013;36:687–94.
Noe BB, Stapelfeldt CM, Parner ET, Mikkelsen EM. Survival after traumatic spinal cord injury in Denmark: a hospital-based study among patients injured in 1990-2012. Spinal Cord. 2017;55:373–7.
Chamberlain JD, Gmunder HP, Hug K, Jordan X, Moser A, Schubert M, et al. Differential survival after traumatic spinal cord injury: evidence from a multi-center longitudinal cohort study in Switzerland. Spinal Cord. 2018;56:920–30.
Shibahashi K, Nishida M, Okura Y, Hamabe Y. Epidemiological state, predictors of early mortality, and predictive models for traumatic spinal cord injury: a multicenter nationwide cohort study. Spine. 2019;44:479–87.
Beck B, Cameron PA, Braaf S, Nunn A, Fitzgerald MC, Judson RT, et al. Traumatic spinal cord injury in Victoria, 2007–16. Med J Aust. 2019;210:360–6.
Li B, Qi J, Cheng P, Yin P, Hu G, Wang L, et al. Traumatic spinal cord injury mortality from 2006 to 2016 in China. J Spinal Cord Med. 2020:1–6 https://doi.org/10.1080/10790268.2019.1699355. (Online ahead of print).
Furlan JC, Kattail D, Fehlings MG. The impact of co-morbidities on age-related differences in mortality after acute traumatic spinal cord injury. J Neurotrauma. 2009;26:1361–7.
Furlan JC, Craven BC, Ritchie R, Coukos L, Fehlings MG. Attitudes towards the older patients with spinal cord injury among registered nurses: a cross-sectional observational study. Spinal cord. 2009;47:674–80.
Furlan JC, Fehlings MG. Attitudes toward the elderly with CNS trauma: a cross-sectional study of neuroscientists, clinicians, and allied-health professionals. J Neurotrauma. 2009;26:209–25.
Furlan JC, Craven BC, Fehlings MG. Is there any gender or age-related discrepancy in the waiting time for each step in the surgical management of acute traumatic cervical spinal cord injury? J Spinal Cord Med. 2019;42(sup1):233–41.
Lau D, Dalle Ore CL, Tarapore PE, Huang M, Manley G, Singh V, et al. Value of aggressive surgical and intensive care unit in elderly patients with traumatic spinal cord injury. Neurosurg Focus. 2019;46:E3.
Furlan JC, Hitzig SL, Craven BC. The influence of age on functional recovery of adults with spinal cord injury or disease after inpatient rehabilitative care: a pilot study. Aging Clin Exp Res. 2013;25:463–71.
Furlan JC, Liu Y, Dietrich WD 3rd, Norenberg MD, Fehlings MG. Age as a determinant of inflammatory response and survival of glia and axons after human traumatic spinal cord injury. Exp Neurol. 2020;332:113401.
Kitzman P, Cecil D, Kolpek JH. The risks of polypharmacy following spinal cord injury. J Spinal Cord Med. 2017;40:147–53.
Fehlings MG, Tetreault LA, Aarabi B, Anderson P, Arnold PM, Brodke DS, et al. A clinical practice guideline for the management of patients with acute spinal cord injury: recommendations on the type and timing of rehabilitation. Glob Spine J. 2017;7(3 Suppl):231S–238S.
Fehlings MG, Tetreault LA, Wilson JR, Aarabi B, Anderson P, Arnold PM, et al. A clinical practice guideline for the management of patients with acute spinal cord injury and central cord syndrome: recommendations on the timing (</=24 h Versus >24 h) of decompressive surgery. Glob Spine J. 2017;7(3 Suppl):195S–202S.
Fehlings MG, Martin AR, Tetreault LA, Aarabi B, Anderson P, Arnold PM, et al. A clinical practice guideline for the management of patients with acute spinal cord injury: recommendations on the role of baseline magnetic resonance imaging in clinical decision making and outcome prediction. Glob Spine J. 2017;7:221S–230S.
Acknowledgements
The author gratefully acknowledges Dr. Michael Bracken who kindly shared the NASCIS-1 database for this research study. This study was carried out without funding support.
Author information
Authors and Affiliations
Contributions
As the solo author, Dr. Julio Furlan was responsible for the study design, data analysis and interpretation, manuscript writing and revision. He is accountable for all aspects of this work.
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Ethical approval
The Institutional Ethics Board approved the use of database from the NASCIS-1 trial to address research questions other than the original aims of the NASCIS-1 trial. A Data Use Agreement between the Yale University and University Health Network was instituted in 2006.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Furlan, J.C. Effects of age on survival and neurological recovery of individuals following acute traumatic spinal cord injury. Spinal Cord 60, 81–89 (2022). https://doi.org/10.1038/s41393-021-00719-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-021-00719-0