Abstract
Study design
Focus group qualitative study.
Objectives
To explore factors affecting adherence to behaviours appropriate for the prevention of pressure injuries (PIs) in people with spinal cord injury (SCI) in Malaysia.
Setting
University Hospital, Malaysia
Methods
Four sets of focus group interviews were conducted, each with 5–10 participants, totalling 30 people with SCI. A trained interviewer used structured interviews designed to explore participants’ experiences of complying with recommended behaviours for the prevention of PIs. All interviews were digitally recorded, transcribed, and analysed utilising thematic analysis.
Results
The factors that affected participants’ adherence are classified into four main themes: (a) educational aspects, (b) internal drive, (c) social and environmental factors, and (d) post-SCI physiological changes.
Conclusions
This qualitative study provides initial exploratory evidence regarding the thoughts, experience, and opinions pertaining to PI preventive behaviours within the Malaysian SCI population. The emerging themes contribute to an in-depth understanding of the competency of the Malaysian healthcare system in PI prevention, personal and societal factors influenced by the socio-demographic backgrounds, and disease-related factors that influence the adherence to such preventive interventions.
Similar content being viewed by others
Introduction
Pressure injuries (PIs) are a debilitating post-SCI complication which are known to affect a person’s general health condition, psychological status, and function and community integration. Furthermore, they may be the cause of mortality due to the development of sepsis from infected ulcers [1, 2]. PIs are common complications [3, 4] following SCI. They constitute one of the most common causes of recurrent hospitalisation [5], thereby resulting in financial burden due to hospital costs and resulting unemployment [5, 6]. The prevalence of PIs in SCI populations across low and middle-income countries is highly variable, ranging from 26% to 46% [4]. As many as 95% of people with SCI will experience a PI during their lifetime [7]. The prevalence of such was 8% after 1 year, increasing to 9% after 2 years and 32% at 20 years post-SCI [8]. However, accurate measurement was difficult in such countries due to lack of reliable reporting as a result of health infrastructure constraints, difficulty in detecting stage 1 PIs and inability to capture data on mortality secondary to SCI-related complications [4, 9].
Various studies have been conducted to investigate the risks of PIs [2, 10]. Demographic risk factors including age, education level, ethnicity, economic status, and social-background have been identified as increasing the risk of developing PIs [10, 11]. Lower levels of adherence to PIs have been shown to contribute to a higher risk of PI occurrence [10, 12]. Differing demographic backgrounds, lifestyles, and personal values are also significant factors in determining adherence levels to PI preventive behaviours [12]. Further risks of occurrence include SCI related factors (level of injury, functional level, traumatic vs non-traumatic, previous history of PIs, autonomic dysreflexia, spasticity, contracture and incontinence), accessibility to healthcare systems and psychological factors [2, 10]. Identification of these risk factors has allowed us to understand the fundamental knowledge of PI formation and hence develop pro-active preventive interventions [2, 10]. However, these findings may not be generalizable; therefore, an in-depth understanding of the risks in different socio-economic backgrounds is necessary [13]. Malaysia is a multi-ethnic country with a marked diversity of culture, lifestyles, personal values and healthcare systems. To prevent PIs among people with SCI in Malaysia, there must first be an understanding of the local degree of PI knowledge, the competency of healthcare staff and infrastructure in preventing and managing PIs, and the individualized risk profiles and socio-environmental factors which might play significant roles in PI preventive interventions. An in-depth understanding of these factors will allow the development and implementation of effective PI preventive interventions specifically for the Malaysian SCI population.
Given the lack of prior research demonstrating adherence levels among the local SCI population and the uniqueness of Malaysia’s heterogeneous population, it is appropriate to deploy qualitative research as an initial exploratory tool. This will enable us to uncover the beliefs, opinions and experiences within the local SCI population, and explore the factors influencing adherence to PI preventive behaviours, thereby allowing relevant conclusions to be developed.
Methods
This study used a qualitative methodology to provide an accurate description and interpretation of experiences and factors affecting adherence during PI preventive behaviours.
Participants
Convenience sampling was used to select a total of thirty participants with SCI who were undergoing inpatient rehabilitation or attended the outpatient SCI rehabilitation clinic in the University Malaya Medical Centre, and who satisfied the inclusion and exclusion criteria. The inclusion criteria was as follows: (1) aged 18 years and above; (2) inability to walk except for therapeutic purposes; (3) traumatic and non-traumatic etiologies of SCI; (4) ability to manage skin regimen independently—as determined by a Spinal Cord Independence Measure (SCIM) score of 6 in the domain of mobility in bed and action; (5) proficiency in either Bahasa Melayu or English, and (6) at least three months post-injury. The exclusion criteria were: (1) concomitant brain injury with cognitive impairment as determined by the Mini Mental State Examination (MMSE) score of 24 or lower; (2) complete dependence on caregiver; (3) residence in nursing home; (4) non-traumatic etiology of SCI progressing in nature, such as metastatic diseases or HIV-associated myelopathy, and (5) signs and symptoms of depression based on Patient Health Questionnaire-9 with a score of 5 or above.
Data collection
Four focus group of 5–10 participants were conducted by one researcher (NMH). Demographic data regarding participants’ age, duration of SCI since onset (sub-acute or chronic) and years of experience in dealing with PIs were collected. The duration of each session ranged from 60 to 75 min. The demographic data and participants’ characteristics relevant to this study were gathered through a checklist-type questionnaire given to participants. The trained interviewer asked predetermined, open-ended questions pertaining to the experiences and factors that affected adherence to PI preventive behaviours. The development of the interview guide was based on the author’s experience in working with people who have SCI (see Supplementary Appendix 1 for interview guide). The questions were structured to cover the following: (1) level of knowledge pertaining to PIs; (2) adherence level to PI preventive behaviours; (3) factors that hindered PI preventive behaviours; (4) facilitating factors towards PI preventive behaviours, and (5) perceptions of PI preventive behaviour. Interviews were conducted until data saturation was reached, i.e., the point at which no new themes or issues arose within a category of data. The participants could freely discuss and exchange opinions on the topic with other participants. Group sessions were audiotaped and subsequently transcribed verbatim in the original language used in the interview (Bahasa Melayu).
Data analysis
A thematic analysis approach, as outlined by Braun and Clarke (2006), was employed to organise the data from the focus group discussion sessions [14]. Transcripts were read and re- read by two researchers (NMH and ANMY) to allow familiarisation with the data and identify emerging concepts and codes. The analysis focused on the factors, reasons and limitations that influenced adherence to PI preventive behaviours. Two researchers (NMH and ANMY) coded the data independently using an inductive approach and later reviewed the codes together, until sub-themes were formed based on commonality. The third researcher (JPE), an expert in qualitative research, reviewed the sub-themes to confirm interpretations and assist in their development. Further discussion between two researchers (NMH and JPE) were conducted to finalise the developed themes. Data interpretation and analysis were conducted in the original language used in the discussion. The verbatim transcripts were translated into English language only for publication purposes.
Data trustworthiness
To ensure data trustworthiness several steps, described by Shenton et al. (2004). were adopted [15]. NMH is a rehabilitation physician with 5 years’ experience in managing patients with SCI and is a novice qualitative researcher. JPE is a rehabilitation physician with a special interest in the field of spinal cord rehabilitation and is an experienced qualitative researcher. ANMY is a medical ethics expert with experience in qualitative research and data analysis. Steps were undertaken to ensure data validity; i.e., prolonged engagement with the participants by utilising informal ice-breaking sessions and a 30-min question and answer session regarding PIs care before the actual interview. These sessions enabled the researchers to gain the participants’ acquaintance and trust and provided a better understanding of the research field. Data triangulation was adopted by holding four focus group discussion sessions with different participants at different times. Data triangulation was achieved by two researchers analysing the verbatim independently, and later reviewing the same together to confirm interpretation, codes and themes. The researchers involved in the initial data analysis included one researcher with a SCI rehabilitation background and one without an SCI background to reduce potential bias during data interpretation. Further interpretation confirmation was conducted by an experienced qualitative researcher with a long-standing SCI rehabilitation background. The researchers also kept records of all analysis and reflexive notes and maintained the verbatim quotations throughout all stages of analysis.
Results
The demographic characteristics of the participants are presented in Table 1. Four broad categories were identified: educational aspects, internal drive, social and environmental factors, and post-SCI physiological changes. These themes reflect what and how these factors influence the level of adherence towards PI preventive behaviours among people living with SCI. The four broad categories are presented in Table 2. Each of the themes are discussed below. Illustrative quotes to support the themes are presented in Tables 3–14.
Educational aspects
Educational aspects refers to issues encountered during knowledge delivery pertaining to PI preventive interventions among people with SCI. This theme consists of two sub-themes, as depicted in Tables 3 and 4 with supportive quotes relevant to the sub-themes.
Source of information
Credibility, expertise and trustworthiness are important characteristics of an efficient knowledge provider. Most participants were exposed to PI information during their initial encounter with the healthcare providers (HCPs) following their SCI. The effectiveness of education was highly dependent upon the HCPs’ efficiency in conveying the information. Participants stated that the information was usually superficial, insufficient and sometimes incorrect. Some participants also stated that HCPs were incompetent in detecting PIs, hence less emphasis was placed on the preventive method. Flaws in the education given led to poor understanding of PI risks, which led to incompetency in performing the preventive behaviour. The education was most effective when given by a multi-disciplinary team of HCPs specialising in the care of SCI patients, as opposed to HCPs with less experience and specialisation in SCI and its complications, particularly in centres lacking specialty in rehabilitation medicine.
The participants also gained access to information from the internet and their peers. They reported that they could better digest, value and relate to the information conveyed by peers sharing similar conditions, than that from HCPs using existing guidelines, who were perceived as different and unable to understand the participants’ situations.
Self-management
The participants were also able to empower themselves with problem-solving skills and knowledge to manage problems or challenges encountered whilst practising PI preventive measures. These measures were tailored to their individual needs and ever-changing lifestyles and may not be addressed in the standard guidelines of PI preventive behaviours. This self-empowerment skill is one of the most crucial attributes in improving self-efficacy in performing PI preventive behaviours, hence maintaining and enhancing the adherence level. However, without proper guidance from the HCP, incorrect information regarding preventive measures may be accessed or improper behaviour adopted that may not align with medical recommendations.
Internal drive
Internal drive refers to inherent personal factors which influence preventive behaviours among SCI persons. This consists of four sub-themes, as depicted in Tables 5–8 with supportive quotes relevant to the sub-themes.
Responsibility toward family
Fulfilling duties towards family serves as an internal push or facilitator for adherence to the preventive behaviours. The participants feel that they need to stay healthy to fulfil their responsibilities as the head of the family or breadwinner or in managing the household. Thus, they were more ready to commit to preventive behaviours to avoid burdening their family with severe complications of PIs, which could affect family relationships, finances and the psychological state of the family.
Attitude
Negative or positive attitudes influence levels of adherence. Participants possessing apathetic or ‘couldn’t-care-less’ attitudes risk being ignorant of and losing interest in continuing preventive measures. Participants who were very diligent after SCI may become less diligent over time, perceiving the behaviours as troublesome. However, several participants who were consistent and disciplined, gradually became used to the routine and successfully developed good preventive habits. Most agreed that self-discipline and positive attitudes were crucial to maintaining adherence.
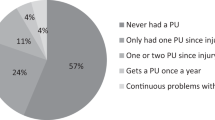
Experience of pressure injury
Several participants disclosed that their experience with PIs served as encouragement in adhering to preventive behaviours. Having first-hand experience of PIs or observing their peers struggling with the serious complications increased their understanding of the hazardous effect of taking the preventive matters lightly. The more severe PIs complication suffered, the more likely they were to adhere to the preventive acts. In contrast, a few participants perceived that the preventive measures had less beneficial effect; hence, they resorted to not performing them at all. This belief was driven by having little or no experience of PIs during the disease, as well as non-adherence to the preventive acts.
Mood
Motivation is influenced by the psychological status of those suffering from SCI. Downheartedness or low mood as a result of SCI, can lower a person’s motivation to perform the preventive behaviours as they are still in denial and more concerned about the chances of recovery following SCI. They have little or no or interest in learning about skin care, despite previous education regarding the disease.
Social and environmental factors
The third theme concerning “Social and Environmental Factors” describes external factors which influence adherence levels. Four main sub-themes were identified, as depicted in Tables 9–12 with relevant supportive quotes.
Social and ethical inappropriateness
Strict adherence to ensure the effectiveness of PI preventive measures requires people with SCI to perform these measures in all situations. This may result in humiliating situations occurring whilst performing pressure relief in public, such as passing flatus or unappealing smells arising from soaked PI dressings. Such scenarios deterred individuals from performing pressure relief. Society may perceive pressure relief as a peculiar act, mainly stemming from lack of understanding regarding the SCI impairment.
Physical & situational threat
A non-conducive environmental condition can hamper SCI sufferers from utilising preventive acts. Factors contributing to such difficulties included lack of facilities in workplaces, e.g., sick bays to accommodate employees with SCI. Poorly maintained amenities, such as cracked toilet bowls, may be hazardous to persons performing preventive measures. Other factors, including being trapped in unfavourable and unpredictable situations (e.g., stuck in traffic whilst riding a tricycle) also contributes to such problems. These situations not only hinder adherence but also increase the chances of further developing PIs.
Family support
Families play an important role as facilitators in preventive care. They provide support by offering assistance and affirmation, which serve as a constant reminder and help to fill any knowledge gaps and inefficiency in performing the preventive measures.
Societal attitude
Some participants reported that they perceived the preventive behaviours as a burden, which interfered with their daily lives. Being overly occupied with daily work, house chores and tasks tends to cause negligence towards self-care, which adversely affects adherence to preventive methods. It was also believed that by performing some preventive acts, they may be perceived as ineffective, inefficient, less-productive employees. It was deemed important for them to display a high-credibility appearance despite their disabilities, in order to keep their jobs.
Post- SCI physiological changes
Two sub-themes emerged regarding physiological changes following SCI, which influenced the adherence level (as depicted in Tables 13 and 14), with supportive quotes relevant to the sub-themes.
Pathological factors as facilitators
The identified facilitative pathological factors were pain and spasm over lower limbs when a person with SCI sat for too long. This served as an alarm or signal that it was time to perform pressure reliefs and prevent total abandonment of such behaviours. Paradoxically, having such signals may reduce the appropriate frequency of performing pressure reliefs that are recommended in the guideline.
Pathological factors as barriers
Pathological barriers towards preventive behaviours included truncal spasm, which usually occurs whilst performing pressure relief acts. This can be hazardous as it may cause falls, whereas orthostatic hypotension which occurs in acute SCI hinders one’s ability to be upright or move to perform the preventive actions. Concomitant fracture of the upper limb together with SCI also caused a hindrance due to pain. The presence of these physical barriers had deleterious implications in regards to PI preventive acts, decreasing adherence. Keeping safe and avoiding other medical hazards were sufferers’ utmost priority.
Discussion
This study explored factors influencing the level of adherence towards PI preventive behaviours. Many quantitative and qualitative studies investigating the risks of developing PIs, have indicated that poor adherence towards the preventive behaviours plays a role in PI occurrence [8,9,10, 16, 17]. This study allows an in-depth understanding of what and how those factors affect the adherence. Four broad themes emerged from this study: (1) Educational aspects; (2) Internal drive; (3) Social and environmental factors and, (4) Post-SCI Physiological changes. The results of this research overlapped with those of previous qualitative studies covering a range of behavioural components including motivation, education, psychological and biological aspects [13, 16, 18].
Education has been shown to be crucial to knowledge empowerment [2, 17]. To the best of our knowledge, limited or no prior research exists describing how PI education is conducted in our local setting. Hence, this study delves indirectly into the shortfalls of education intervention within our healthcare system. Based on our experience of managing SCI patients, education about PIs is often conducted at the bedside by the HCPs during the acute phase, usually taking place in the surgical ward or sometimes in a hospital without specialised rehabilitation medical services. The quality of this education very much depends on the competency of the HCPs, as shown in our study [19, 20]. Structured PI prevention programs often begin during the active inpatient rehabilitation admission, by specialised multi-disciplinary rehabilitation teams trained in post-SCI care, during the sub-acute phase. However, not all hospitals are fortunate enough to have this service. This education is usually confined to the recommendations in the basic manual to avoid information overload which may overwhelm the patient and takes place during the initial phase, emphasising the core principles of PI prevention methods regarding skin care, pressure reliefs, equipment and a healthy lifestyle. Peers are not usually involved in the formal education as they are not trained. Education is rarely extended to the community; if occurring at all it is held in isolation, is uncoordinated and with a lack of supervision. Hence, certain psychosocial aspects are poorly addressed, despite their evident importance as shown in this study.
Analysing the shortfalls in the education system assists us in determining how the education intervention should be improved. All HCPs dealing with SCI patients should be educated about the risks of PIs and preventive method steps, especially when dealing with patients during the acute phase [17, 20]. Knowledge evaluation should be conducted among HCPs from time to time to ensure that their competency is at a high level [21]. SCI patients’ education should be structured as recommended in the evidence-based guidelines, especially in the early stages that address many dimensions of PI prevention [2, 22]. The content of the education should not only encompass traditional medical models, but also behavioural approaches which promote self-management [17, 22]. A systematic review which explored the content of skincare self-management intervention for people with SCI, utilised a Behaviour Change Technique (BCT) components to code the intervention content. It had revealed that 65 out of 93 BCTs were not coded to any interventions, implying that many components of behavioural science remain unexplored despite their potential impact on skincare [22]. Our findings address this disparity by providing an in-depth understanding of factors that influence these BCT components, including credible source, behavioural practice, action planning, feedback on behaviour, social support, commitment, habit formation, prompt/cues, body changes and social and environmental consequences [22]. These findings may assist clinicians in developing relevant educational content and preventive methods which are appropriate to end-users. Other necessary elements are the experience and knowledge-sharing, which may be achieved by conducting group sharing sessions moderated by a trained HCP, enabling cross-over of knowledge and enhanced problem-solving skills. HCPs have a role as “gatekeeper” to ensure that the information shared is in line to the medical recommendations. This may also allow the HCPs to increase their understanding of issues which might arise once the participants return to their community. Hence, a more individualised approach to giving relatable recommendations beyond medical perspectives and standard guidelines is achieved. This also promotes self-management, assisting patients to learn, consistently apply and incorporate the recommendations into their daily lives effectively [2]. The education interventions should be effectively targeted and matched to different groups of needs and different phases of SCI [2, 23].
Peer influence has been shown to be a critical factor and should be integrated into the community outreach programme. This might provide more behavioural approaches outside the conventional medical framework [2, 17]. The Peer Information Network was an evaluation project of peer support conducted in America [24]. 24 peer advisors were trained, operating through community centres to promote independence for people living with disabilities. However, the project encountered multiple downfalls in implementation; low recruitment; high loss to follow-up of subjects, and lack of control over peer-advisor training [2]. Learning from these pitfalls we propose a peer-match buddy system, in which online profiles of a potential peers are outlined, from which the person with SCI can choose the peer deemed most compatible with their own clinical characteristics, lifestyle, personal values and personality traits. Thus, an opportunity is provided to develop a close, long-lasting mentorship bond and individualised guidance. Hence, loss of follow-up might be reduced and a role model of effective empowerment formed [25]. Ideally, this system should be initiated during the early rehabilitation phase, so that good attitudes can be instilled, and psychological aspects supported. Regress or deviation of motivation or attitude can be detected earlier by peers and addressed. Peers should be trained to ensure the dissemination of correct information. This study provides additional information regarding the challenges and obstacles pertaining to preventive behaviours relevant to our community, which can be used to prepare the peers with strategies to tackle such problems.
In previous literature, pathological implications post SCI, such as pain, has been found to negatively affect mood, function and quality of life [26]. Moderate-to-severe pain impairs weight-shifting and mobility which leads to increased risk of PIs development [26]. Interestingly, several participants admitted that pain was a facilitative factor which served as a reminder or indicator that it was time to perform pressure relief acts. However, this behaviour deviates from the recommended standard practice [1, 2]. Further study is warranted to explore the effectiveness and implications of such practice [1, 2]. Strikingly, despite similarities with prior studies which focused on the complications of non-adherence towards preventive behaviour, a noteworthy implication of performing preventive behaviours was identified; passing flatus, unappealing smells and receiving awkward stares from people around whilst performing pressure relief are perceived as socially and ethically inappropriate. These acts, which may give rise to embarrassment, are rarely discussed and may lead to abandonment of the preventive practices. This indicates that shortfalls in certain preventive acts exist which may not be suitable in some circumstances.
This study also reveals that certain preventive steps are not well adapted to certain lifestyle or biological changes. Our local approach is very traditional and conventional. Perhaps we might start to incorporate technological advancement to local preventive methods, e.g., electrical stimulation [27], dynamic weight-shifting technology and power weight-lifting or tilting wheelchairs [28]. The expense of such equipment limits their usage in our preventive intervention. This study hopes to motivate local innovators to produce sophisticated versatile equipment that is affordable, and more importantly, able to solve pertinent issues of the preventive behaviours.
Limitations of the study
The advantages of using focus group discussion allowed us to achieve maximal variation, provide a wider range of information and promote interactivity [29]. The recommendation that preventive behaviours should be initiated early post-injury [2] and the evidence indicating that SCIs possess different sets of PI risks at different stages, rationalises the combining of inpatient and outpatient participants during the discussion sessions. [30, 31].
It is worthwhile to note some limitations of this study in interpreting the results. This study may not represent all populations of SCI in the country, as the interview was more focused on those independent of skin care regimen. The results may be influenced by selective memory and inability to recall events. Nonetheless, the themes were identified repeatedly across the study sample, hence increasing the reliability of the study outcomes. Future research could focus on the education needs pertaining to PI preventive behaviours, utilising in-depth semi-structured interviews. The interviews should be conducted among HCPs (HCPs or peers), people with SCI and their care takers. This will expand the context and rigorous information pertaining to what is lacking from different perspectives of both providers and recipients of the education.
Conclusion
This qualitative study provides an initial exploratory analysis regarding the thoughts, experience and opinion pertaining to PI prevention among the heterogeneous Malaysian SCI population. It contributes to an in-depth understanding of the competency of the Malaysian healthcare system in PI preventive management, personal and societal factors influenced by the socio-demographic backgrounds, and disease-related factors which affect adherence to preventive intervention. We believe that our study has provided the necessary evidence to urge that requisite actions or strategies be taken to improve current states of practice in our healthcare landscape.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
[No author listed] Consortium for Spinal Cord Medicine Clinical Practice Guidelines. Pressure ulcer prevention and treatment following spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med. 2001;24:S40.
Houghton PE, Campbell K Canadian best practice guidelines for the prevention and management of pressure ulcers in people with Spinal Cord Injury: a resource handbook for clinicians. Ontario Neurotrauma Foundation; 2013.
Chen Y, DeVivo MJ, Jackson AB. Pressure ulcer prevalence in people with spinal cord injury: age-period-duration effects. Arch Phys Med Rehabilit. 2005;86:1208–13.
Zakrasek EC, Creasey G, Crew JD. Pressure ulcers in people with spinal cord injury in developing nations. Spinal Cord. 2015;53:7–13.
Allman RM, Goode PS, Burst N, Bartolucci AA, Thomas DR. Pressure ulcers, hospital complications, and disease severity: impact on hospital costs and length of stay. Adv Ski wound care. 1999;12:22–30.
DeJong G, Tian W, Hsieh CH, Junn C, Karam C, Ballard PH, et al. Rehospitalization in the first year of traumatic spinal cord injury after discharge from medical rehabilitation. Arch Phys Med Rehabilit. 2013;94:S87–97.
Rintala DH, Garber SL, Friedman JD, Holmes SA. Preventing recurrent pressure ulcers in veterans with spinal cord injury: impact of a structured education and follow-up intervention. Arch Phys Med Rehabilit. 2008;89:1429–41.
Chen D, Apple DF Jr, Hudson LM, Bode R. Medical complications during acute rehabilitation following spinal cord injury—current experience of the Model Systems. Arch Phys Med Rehabilit. 1999;80:1397–401.
Garber SL, Rintala DH, Hart KA, Fuhrer MJ. Pressure ulcer risk in spinal cord injury: predictors of ulcer status over 3 years. Arch Phys Med Rehabilit. 2000;81:465–71.
Marin J, Nixon J, Gorecki C. A systematic review of risk factors for the development and recurrence of pressure ulcers in people with spinal cord injuries. Spinal Cord. 2013;51:522–7.
Saunders LL, Krause JS, Peters BA, Reed KS. The relationship of pressure ulcers, race, and socioeconomic conditions after spinal cord injury. J Spinal Cord Med. 2010;33:387–95.
Ghaisas S, Pyatak EA, Blanche E, Blanchard J, Clark F, PUPS II Study Group. Lifestyle changes and pressure ulcer prevention in adults with spinal cord injury in the pressure ulcer prevention study lifestyle intervention. Am J Occup Ther. 2015;69:6901290020p1–0.
Jackson J, Carlson M, Rubayi S, Scott MD, Atkins MS, Blanche EI, et al. Qualitative study of principles pertaining to lifestyle and pressure ulcer risk in adults with spinal cord injury. Disabil Rehabilit. 2010;32:567–78.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3:77–101.
Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Educ Inf. 2004;22:63–75.
Langemo DK, Melland H, Hanson D, Olson B, Hunter S. The lived experience of having a pressure ulcer: a qualitative analysis. Adv Ski Wound Care. 2000;13:225.
Hsieh J, Benton B, Titus L, Gabison S, McIntyre A, Wolfe D, et al. Skin Integrity and Pressure Injuries Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, et al. editors. Spinal Cord Injury Rehabilitation Evidence. Version 7.0; 2020.
Clark FA, Jackson JM, Scott MD, Carlson ME, Atkins MS, Uhles-Tanaka D, et al. Data-based models of how pressure ulcers develop in daily-living contexts of adults with spinal cord injury. Arch Phys Med Rehabilit. 2006;87:1516–25.
Dalvand S, Ebadi A, Gheshlagh RG. Nurses’ knowledge on pressure injury prevention: a systematic review and meta-analysis based on the Pressure Ulcer Knowledge Assessment Tool. Clin Cosmet Investig Dermatol. 2018;11:613.
Kaddourah B, Abu-Shaheen AK, Al-Tannir M. Knowledge and attitudes of health professionals towards pressure ulcers at a rehabilitation hospital: a cross-sectional study. BMC Nurs. 2016;15:17.
Zanini C, Lustenberger N, Essig S, Gemperli A, Brach M, Stucki G, et al. Outpatient and community care for preventing pressure injuries in spinal cord injury. A qualitative study of service users’ and providers’ experience. Spinal Cord 2020;58:882–91.
Baron JS, Sullivan KJ, Swaine JM, Aspinall A, Jaglal S, Presseau J, et al. Self-management interventions for skin care in people with a spinal cord injury: part 2—a systematic review of use of theory and quality of intervention reporting. Spinal Cord. 2018;56:837–46.
Schubart JR, Hilgart M, Lyder C. Pressure ulcer prevention and management in spinal cord-injured adults: analysis of educational needs. Adv Ski Wound Care. 2008;21:322–9.
Steele LL, Ferguson-Pell MW, Paeglow TN, Stevens FG, Davis K Peer information network: an evaluation of peer counselling in the prevention of pressure sores among persons with spinal cord injury. Preliminary report. New York State Prevention Program Special Project. Personal communication.
Cesario J, Hibbard MR A Community Based Peer Mentoring Program For Individuals With Spinal Cord Injury Program Manual.
Mehta S, Teasell RW, Loh E, Short C, Wolfe DL, Benton B, Blackport D, et al. Pain Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, et al. editors. Spinal Cord Injury Rehabilitation Evidence. Version 7.0; 2019; pp. 1–101.
Smit CA, Zwinkels M, Van Dijk T, De Groot S, Stolwijk-Swuste JM, Janssen TW. Gluteal blood flow and oxygenation during electrical stimulation-induced muscle activation versus pressure relief movements in wheelchair users with a spinal cord injury. Spinal Cord. 2013;51:694–9.
Connolly SJ, Miller WC, Trenholm K, Titus L, Moir S, Coulson S, et al. Wheeled mobility and seating equipment for the spinal cord injured individual. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, et al, eds. Spinal Cord Injury Rehabilitation Evidence, 2010. Version 7.0. http://www.scireproject.com/. Accessed May 10, 2020.
Leung FH, Savithiri R. Spotlight on focus groups. Can Fam Phys. 2009;55:218–9.
Gelis A, Dupeyron A, Legros P, Benaim C, Pelissier J, Fattal C. Pressure ulcer risk factors in persons with SCI: part I: acute and rehabilitation stages. Spinal Cord. 2009;47:99–107.
Gelis A, Dupeyron A, Legros P, Benaim C, Pelissier J, Fattal C. Pressure ulcer risk factors in persons with spinal cord injury part 2: the chronic stage. Spinal Cord. 2009;47:651–61.
Acknowledgements
Sa’adah Binti Muhamad Amin, Occupational Therapist, Universiti Malaya Medical Center. Atika Suhada Mistee, Physiotherapist, Universiti Malaya Medical Center. Chua Siew Chin, Rehabilitation Nurse, Universiti Malaya Medical Center. University Malaya for funding this study under the University of Malaya Research Grant (PO019–2016A)
Funding
The University of Malaya funded this study under the University of Malaya Research Grant (PO019–2016A).
Author information
Authors and Affiliations
Contributions
NMH is the corresponding author responsible for designing the review protocol, writing the protocol and report, conducting the search, screening potentially eligible studies, leading the process of extracting, coding, analysing data, interpreting results, updating reference lists and creating’Summary of findings’ tables. She is also responsible for summarising the whole research protocol, findings and interpretation into a written manuscript with the assistance of the other co-authors. ANMY has experience in qualitative study and was actively involved in the verbatim transcription, coding and thematic analysis alongside the lead researcher. She was also involved in the data interpretation. She assisted the lead researcher with the reference list. JPE contributed and gave her expert advice in qualitative study protocol, assisting the data coding, thematic analyses and data interpretation together with the lead researcher. She also contributed to the re-structuring of the manuscript. NH contributed in advising on the focus of the study and the recruitment of participants. She also assisted in proofreading the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics
This study was approved by the Institution’s Medical Research Ethics Committee (20164–2377).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Mohamad Hashim, N., Yusof, A.N.M., Engkasan, J.P. et al. Factors affecting adherence to behaviours appropriate for the prevention of pressure injuries in people with spinal cord injury from Malaysia: a qualitative study. Spinal Cord 59, 777–786 (2021). https://doi.org/10.1038/s41393-020-00586-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-00586-1


