Abstract
Study design
Prediction study.
Objectives
To investigate the prediction accuracy of the Downton fall risk index (DFRI) and a question of falls the previous year; further to examine the association between time to first fall and risk indicators for falls in wheelchair users and ambulatory persons with Spinal Cord Injury (SCI).
Setting
Two SCI centres in Norway and Sweden (Sunnaas Rehabilitation Hospital, Rehab Station Stockholm /Spinalis).
Methods
Two hundred and twenty-four persons with traumatic SCI, ≥1 year post-injury, ≥18 years participated. Prospective falls were reported by text messages every second week for one year. Sensitivity, specificity and time to first fall (Kaplan Meier) were investigated for DFRI and the question of falls in the previous year. DFRI ≥3 was defined as a high risk of falls. Cox survival analysis was used to calculate hazard ratios for functional independence, gait speed and fear of falling.
Results
The sensitivity was 36–57% for DFRI and 82–89% for the question of falls, while specificity was 74–83%, and 34–49%. For DFRI, time to first fall was shorter in the high-risk group, for both wheelchair users (p = 0.005) and ambulatory persons (p = 0.006). Falls previous year increased the hazard ratio of falls for wheelchair users (HR = 3.35, 95% CI = 1.86 to 6.02) but not for ambulatory persons.
Conclusions
Falls in the previous year showed a better predictive accuracy than DFRI due to the low sensitivity of DFRI. As previous falls had low specificity, it still remains difficult to predict falls in those who have not fallen yet.
Similar content being viewed by others
Introduction
During a lifetime with spinal cord injury (SCI) there is a high risk of secondary complications, and falls are an additional threat to health and independence. Knowledge regarding falls and SCI is increasing, showing that falls are common, and an incidence between 30 and 72% [1,2,3,4,5] over 6−12 months has been reported. Furthermore, there seem to be different factors contributing to falls in wheelchair users and ambulatory persons with SCI [1,2,3,4,5,6].
Since falls and related injuries can have severe consequences for the individual and may lead to great cost for the society, it is important to identify persons at risk of falling. In clinical settings, programmes for the prevention of falls often start with screening for fall risk. There are several fall risk assessments for different populations such as elderly people [7], as well as for people with a neurological diagnosis [8, 9]. Fall risk assessments often include different aspects, such as previous falls [7, 10], medication [10], mobility or physical function [7, 10], frequent toileting [7] and visual impairment [7, 10]. Moreover, these assessments are seldom developed for community dwelling people, and to our knowledge there are no established fall risk assessments designed for persons with SCI, and especially for non-elderly groups with a large proportion of wheelchair users.
The Downton Fall Risk Index (DFRI) [10, 11] is commonly used in the Nordic countries, and has shown predictive properties equivalent to other fall risk instruments [12, 13]. When validated for stroke patients in geriatric rehabilitation, a moderately high correlation was found between the predicted risk of falls and observed falls [14]. The sensitivity for prediction of falls shown previously in older people was 79 to 95%, and specificity was 24 to 40% [10, 15, 16].
Previous falls, a well-known risk factor for falls [1, 17], can either be used included in instruments such as Downton [10, 16], or as a single item question. Simple prediction models with age, sex, self-reported balance problems and previous falls have been reported as being equivalent to complex models [18].
Furthermore, staff assessment of the risk of falling has in some studies been shown to have a better prediction than instruments [7, 13], but not always [19]. Nevertheless, fall risk instruments, such as DFRI, are still used and are recommended in guidelines for the prevention of falls.
The primary aim in this study was to investigate the prediction accuracy of the Downton and a single item question of falls the previous year in wheelchair users and ambulatory persons with SCI. Secondly, the aim was to investigate the relation between time to first fall and factors related to falls in SCI [2, 3, 6] i.e., mode of mobility, functional independence, gait speed, general quality of life, fear of falling, and symptoms of depression.
Methods
This one-year longitudinal study is part of the Spinal Cord Injury Prevention of Falls Study (SCIP Falls). Data collection and sample have been thoroughly described earlier [2, 3, 6]. A fall was defined according to the Prevention of Falls Network Earth as “an unexpected event in which the participants come to rest on the ground, floor, or lower level”. The Standards for Reporting of Diagnostic Accuracy Studies (STARD) for reporting diagnostic accuracy [20] were used.
Participants
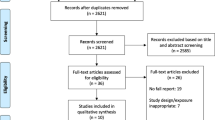
A consecutive sample of 224 persons with SCI was included after excluding 9 who were ill and 37 who declined to participate. Participants, (151 wheelchair users, 73 ambulatory), were enroled from Rehab Station Stockholm/Spinalis, Sweden and Sunnaas Rehabilitation Hospital, Norway at regular lifelong SCI follow up. Participant characteristics are displayed in Table 1, the Flowchart in Fig. 1. Of the 151 wheelchair users, 126 participants used light-weight wheelchairs, 16 used different types of power wheelchairs while the rest used “all-round or comfort” wheelchairs.
Persons ≥18 years of age, at least one year post traumatic SCI (American Spinal Cord Injury Impairment Scale [AIS] A-D), were included. Persons with motor complete injuries (AIS A and B) above C5 level and injuries below L5 were excluded. These criteria were chosen as persons with high tetraplegia have a very special situation and rely on help from other people. In the contrary, persons with lesions below L5 have very small reduction in their physical capacity and their situation differs in this way from most other persons with SCI. Seven persons dropped out.
Data collection procedure
The data collection consisted of a structured interview and clinical assessments as described earlier [2, 3, 6].
Falls were registered prospectively for one year with a text message (sms) delivered every second week with the question “Have you fallen the previous two weeks? (yes or no)”. If no answer was forthcoming, a reminder and a telephone follow-up were sent. A semi-structured telephone interview was performed when a fall was reported. Falls during sports were registered but excluded. All participants answered way above the pre-set criteria of at least 2/3 of the text-messages, except for the seven drop-outs. Hence, 217 persons completed the study. Seven participants reported falls mainly by email or telephone.
Outcome measures
DFRI [10], is an assessment based on 11 items: falls during the previous year (score 0/1), medication (maximum score 5), visual, hearing and limb impairment (maximum score 3), cognitive orientation (score 0/1), and ability to walk safely (score 0/1). The total sum (0‒11) is calculated, and a score of ≥3 is used to indicate a high risk of falls [10, 14].The instrument (14) is thoroughly described by Rosendahl (10), and their operational definitions were used.
The single item question of falls the previous year was assessed by a semi-structured interview. Follow-up questions were used in order to reduce recall bias (i.e.,”Have you fallen the previous year?”, How many times per month/week?”). Furthermore, medication was registered by a structured interview. Impaired vision was registered if a participant “with or without glasses, was not able to read a word in 5 mm block letters at reading distance” according to Rosendahl et al. [10]. Impaired hearing was registered if the participant “without hearing aid was not able to perceive a conversation in a normal voice at a distance of 1 m” [10]. Limb impairment was registered when paresis or sensory impairment was present [10]. All participants were considered to be cognitively oriented with respect to DFRI since they had to be capable to cooperate and manage the testing procedure and telephone follow-up.
Walking ability was considered safe, if the participant with or without walking aids, could “move easily and safely, when for example, opening and closing doors, meeting people in the hallway, and approaching a chair to sit down” [10]. There was no missing data regarding DFRI.
Functional independence was assessed with a Spinal Cord Independence Measure (SCIM) III mobility score. Symptoms of depression were defined as a depression subscale sum score ≥8 of the Hospital Anxiety and Depression Scale (HADS). General quality of life was assessed using the International Spinal Cord Injury Quality of Life Basic Data Set. Fear of falling (no/yes) was registered by interview. Maximal walking speed was measured with the 10 Metre Walk Test (10MWT).
Statistical analysis
Statistical analyses were performed using IBM-SPSS Statistics, version 22.0 (SPSS Inc., Chicago, IL, USA), and MedCalc Statistical Software version 16.4.3 (MedCalc Software Ostend, Belgium; https://www.medcalc.org; 2016). Non-parametric statistics with median and interquartile range (IQR), were used for those continuous variables not normally distributed. Dependent variable was number of reported falls, dichotomised as no falls or at least one fall. Differences between groups were analysed with Student t-test, Mann–Whitney U-test and Chi2 test (χ2). Fisher exact test was used for variables with <5 cases. Spearman’s rank correlation coefficient (rs) was used to investigate relations between variables.
Sensitivity and specificity for predicting falls were analysed for allocation to low and high-risk groups (DFRI) and for the question of falls during the previous year. The area under the Receiver Operator Characteristics (ROC) curve was calculated with a value >0.7 considered as sufficient [21]. After three, six, and twelve months specificity, sensitivity, positive and negative predictive values (PPV and NPV), and Prognostic Separation Index (PSEP) were calculated with 95% confidence intervals (CI).
Kaplan-Meier analysis with the Log Rank test for statistical significance was used to investigate the time difference to first fall between the groups with a low or high risk of falls (DFRI) and between those who had/had not fallen the previous year. Event-free time was based on the number of weeks from inclusion to first fall during follow-up (or censoring for drop-outs), and those who had not fallen were censored after 12 months. Cox regression analysis with hazard ratios (HR) and 95% CI was used to investigate the association between the DFRI score (total sum, low/high-risk groups, falls the previous year and separate items from previous studies of the same sample) [2, 3, 6], and time to first fall. Significant variables from previous studies [2, 3] were also analysed: general quality of life symptoms of depression, functional independence, fear of falling and maximal walking speed. Variables with p < 0.20 and with at least 5 cases that had fallen were investigated in a multivariate Cox regression analysis model where p-values ≤ 0.05 were considered significant. The possible confounders’ age and sex were included in the first Cox regression analysis.
The study was approved by the local ethics committee in Stockholm, Sweden (Dnr: 2012/830−31/2, 2013/391−32, 2014/364−32) and the Regional Ethics Committee for Medical Research Ethics in South East Norway in 2012 (Dnr: 2012/531). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
DFRI and the question of falls the previous year
The DFRI score ranged between 0 and 5 with a median of 2 (IQR = 1). Of the 224 participants 75 (34%) were defined as having a high risk of falls (sum score ≥3), corresponding to 44 (29%) of the wheelchair users and 31 (43%) of the ambulatory persons (Table 2). Falls during the previous year were reported by 170 (76%) of the participants, equal to 111 (74%) of the wheelchair users and 58 (80%) of the ambulatory persons.
Prospective falls
After three months 90 of 224 participants had fallen (40%), after six months another 39 (totally 58%), and after twelve months a total of 159 (71%). Significantly more participants in the DFRI high-risk group 65/75 (87%) had fallen after twelve months compared to 94/149 (63%) in the low risk group (p < 0.001). Corresponding numbers were 36/44 (82%) and 62/107 (58%) for wheelchair users (p = 0.005), and 29/31 (94%) and 32/42 (76%) for the ambulatory persons (p = 0.048).
Concerning the question of falls during the previous year, 24 of those 54 (44%) who had not fallen the previous year fell during the 12 months follow-up period, compared to 135/170 (79%) of those who had fallen the previous year (p < 0.001). For the wheelchair users the corresponding numbers were 27/53 (51%) and 85/98 (87%) (p < 0.001), and for the ambulatory persons 11/15 (73%) and 50/58 (86%) (p = 0.23). One person had at least two falls related to a change in psychotropic medication, and one person fell due to influenza; otherwise there were no known falls due to effects of medication or acute illness.
In general, the sensitivity was lower for the DFRI, 36–57%, than for the question of previous falls 82–89%, while specificity was higher, 74–83%, compared to 34–49% and there was little variation with time, Table 3.
For the DFRI, Kaplan–Meier analysis showed that the time to first fall was shorter in the high-risk group, compared to the low-risk group for both wheelchair users (Log Rank Mantel-Cox, p = 0.005), and ambulatory persons (p = 0.006) (Fig. 2a–b). Moreover, wheelchair users who had fallen during the previous year had a shorter time to first fall (Log Rank Mantel-Cox, p ≤ 0.001) contrary to the ambulatory persons (p = 0.073), (Fig. 2c–d).
a-d a, b. Kaplan–Meier graph on time to first fall (in weeks) for participants classified as having low or high risk of falls according to Downton Fall Risk Index, displayed for wheelchair users (a) and ambulatory persons (b). At baseline there were 44 of 151 wheelchair users, and 31 of 73 ambulatory participants classified as having high risk of falling. c, d. Kaplan-Meier graph on time to first fall (in weeks) for participants who reported falling or not the previous year, displayed for wheelchair users (c) and ambulatory persons (d). At baseline there were 112 of 151 wheelchair users, and 58 of 73 ambulatory participants who reported falling the previous year
Hazard ratios (HR) for fall predictors during the follow-up period (time to first fall)
In the high-risk DFRI group, both wheelchair users and ambulatory persons had increased HR compared to the low-risk group, HR = 1.77, 95% CI = 1.17 to 2.67, p = 0.007 respectively HR = 1.98, 95% CI 1.19 to 3.32, p = 0.009. For the question of falls during the previous year, there was a strong positive relationship between previous falls and falls during follow-up for wheelchair users (HR = 3.35, 95% CI = 1.86 to 6.02, p < 0.001) (Table 4a) but not for ambulatory persons (HR = 1.78, 95% CI = 0.92 to 3.44, p = 0.085) (Table 4b).
For wheelchair users, there were five significant variables (p < 0.05) with ≥5 participants per category: DFRI total score, DFRI group allocation, previous falls, HADS depression score and functional independence (SCIM) (Table 4a). For those with depressive symptoms, the HR for falls were increased (HR = 2.16, 95% CI = 1.24 to 3.79). Those with higher SCIM scores had a higher HR compared to those with lower (HR = 1.06, 95% CI = 1.01 to 1.11). HADS depression score and SCIM were moderately associated (Spearman’s Rho = −0.351; p = 0.002) [48]. They were used in a multivariate model where the HADS depression score ≥ 8 was associated with increased HR for falls (HR = 2.13, 95% CI = 1.22 to 3.72), and for each unit increase in SCIM score the HR increased by 6% (HR = 1.06, 95% CI = 1.01 to 1.11).
For the ambulatory persons, there were two significant variables (p < 0.05), DFRI total score and 10MWT. A higher DFRI score corresponded to increased HR for falls, (HR = 1.29, 95% CI = 1.04 to 1.62, p = 0.023). Furthermore, a longer time during 10MWT, equivalent to slower speed, increased the HR for falls (HR = 1.13, 95% CI = 1.01 to 1.27, p = 0.027) (Table 4b). These two where used in a multivariate model where only the DFRI total score remained significant (HR = 1.28, 95% CI = 1.03 to 1.60, p = 0.027). For several variables, it was not possible to calculate the HRs due to the distribution of participants causing low numbers (<5) per category.
Discussion
This study is to our knowledge one of the first investigating fall risk assessments for persons with SCI. It shows that the fall risk assessment according to DFRI had a lower sensitivity in predicting falls during the one-year prospective follow-up, while the question of falls during the previous year showed a greater ability to predict those who would fall. Symptoms of depression and higher functional independence were associated with higher HR for falls for the wheelchair users, while reduced maximum walking speed and DFRI total score increased the HR in ambulatory persons.
The sensitivity and specificity for DFRI were lower compared to other groups [10, 15, 16], probably explained as the use of medication was low, and visual and hearing impairments were rare, due to the relatively young age of the study group. The low specificity for the question of previous falls indicates that those who had not fallen during the previous year still risk falling in the future. Accordingly, the area under the ROC curve, (Table 3), was rather low (0.62–0.65) for DFRI, but for the question of falls during the previous year it was just above (0.71) the proposed acceptable level of 0.70 for wheelchair users, but not for ambulatory persons (0.58).
In general, sensitivity and specificity did not vary much with time for any of the fall risk assessments. As expected, the PPV increased with time, i.e., those who were classified as high-risk or had reported falls previous year did fall. Consequently, the NPV decreased, i.e., the proportion of those who were classified as low risk or had not fallen during the previous year, who did not fall during follow-up. Even though previous falls is a strong predictor for future falls, included in both methods and in other fall risk assessments [7], it remains difficult to find the first-time fallers.
Interestingly, it has been suggested by Vassallo et al. [13], that low predictive accuracy of a fall risk assessment is positive, i.e., if a patient with a high risk of falling does not fall, the fall preventive interventions seem to be correct, a so-called treatment paradox. They further suggest that prevention of falls should be based on targeting known risk factors instead of using risk classifications [13]. The use of fall risk instruments has also been criticised [22] as it might take valuable resources without adding enough clinical value, because even if they predict the risk of falls correctly, they capture the risk for just a short timeframe. However, the question of previous fall only takes a few minutes.
Moreover, the relation between time to first fall and factors related to falls in previous papers of the SCIP Falls study [2, 3, 6] were investigated. Due to the limited number and distribution of participants, the Cox regression analysis could not be performed for some variables. For the wheelchair users, a higher level of independence (higher SCIM value), was associated with higher HR for falls. This is possibly explained as people with lower levels of independence (often, but not always, reflecting a more severe SCI), have more supervision/assistance. Interestingly, there was no association between time to first fall and level of functional independence for the ambulatory persons in this study contrary to other studies with varying results concerning level of function and falls [4, 5]. Remarkably, the wheelchair users with symptoms of depression had double HR for time to first fall (2.16, 95% CI = 1.24 to 3.79), indicating that this is an area of clinical importance. The relation between depression and falls has, to our knowledge, not been studied in the SCI population. However, in persons with other neurological diagnoses [23], it has been related to increased fear of falling, and to risk of falls in elderly [24].
Study limitations
Despite the limited sample, the size is relatively large for this type of study in an SCI population. Inevitably, analysing participants separately depending on previous falls reduced the statistical power; but based on the high significant HR this method was chosen. Furthermore, any fall risk assessment is a snapshot that might change rapidly. Medication was self-reported since records might include medication no longer in use, which could cause an overestimate of the risk of falls. With such a long follow-up, there is risk of bias if the participants changed their behaviour due to the focus on falls, and thereby reduced the fall rate.
Clinical implications
Asking for previous falls might be more useful than using DFRI in order to capture fallers; but finding first-time fallers is difficult. DFRI showed a fair ability to discriminate the non-fallers, contrary to the question of previous falls. Since falls are common and difficult to predict, a wide use of fall prevention interventions is recommended as, there are usually no negative consequences for interventions such as home visits or improved technical aids.
Conclusion
Allocation to risk groups according to DFRI only captured those who did not fall, while screening for previous falls detects those who usually fall, and to a large extent will continue to do so. Predicting future falls in persons who have not fallen yet remains difficult.
Falls during the previous year showed better predictive accuracy than DFRI due to the low sensitivity of DFRI. As previous falls had low specificity, it still remains difficult to predict falls in those who have not fallen yet.
References
Nelson AL, Groer S, Palacios P, Mitchell D, Sabharwal S, Kirby RL, et al. Wheelchair-related falls in veterans with spinal cord injury residing in the community: a prospective cohort study. Arch Phys Med Rehabil. 2010;91:1166–73.
Butler Forslund E, Jorgensen V, Franzén E, Opheim A, Seiger Å, Ståhle A, et al. High incidence of falls and fall-related injuries in wheelchair users with spinal cord injury—a prospective study on risk indicators. J Rehabil Med. 2017;49:144–51.
Jorgensen V, Butler Forslund E, Opheim A, Franzén E, Wahman K, Hultling C, et al. Falls and fear of falling are predictors of future falls and related injuries in ambulatory individuals with spinal cord injury: a longitudinal observational study. J Physiother. 2017;2:108–13.
Srisim K, Saengsuwan J, Amatachaya S. Functional assessments for predicting a risk of multiple falls in independent ambulatory patients with spinal cord injury. J Spinal Cord Med. 2015;38:439–45.
Phonthee S, Saengsuwan J, Amatachaya S. Falls in independent ambulatory patients with spinal cord injury: incidence, associated factors and levels of ability. Spinal Cord. 2013;51:365–8.
Jorgensen V, Butler Forslund E, Franzen E, Opheim A, Seiger A, Stahle A, et al. Factors associated with recurrent falls in individuals with traumatic spinal cord injury: a multicenter study. Arch Phys Med Rehabil. 2016;97:1908–16.
Oliver D, Britton M, Seed P, Martin FC, Hopper AH. Development and evaluation of evidence based risk assessment tool (STRATIFY) to predict which elderly inpatients will fall: case-control and cohort studies. BMJ. 1997;315:1049–53.
Olsson E, Lofgren B, Gustafson Y, Nyberg L. Validation of a fall risk index in stroke rehabilitation. J Stroke Cerebrovasc Dis. 2005;14:23–8.
Ross A, Yarnall AJ, Rochester L, Lord S. A novel approach to falls classification in Parkinsons disease: development of the Fall-Related Activity Classification (FRAC). Physiotherapy. 2017;103:459–64.
Rosendahl E, Lundin-Olsson L, Kallin K, Jensen J, Gustafson Y, Nyberg L. Prediction of falls among older people in residential care facilities by the Downton index. Aging Clin Exp Res. 2003;15:142–7.
Downton JH, Andrews K. Prevalence, characteristics and factors associated with falls among the elderly living at home. Aging. 1991;3:219–28.
Scott V, Votova K, Scanlan A, Close J. Multifactorial and functional mobility assessment tools for fall risk among older adults in community, home-support, long-term and acute care settings. Age Ageing. 2007;36:130–9.
Vassallo M, Poynter L, Sharma JC, Kwan J, Allen SC. Fall risk-assessment tools compared with clinical judgment: an evaluation in a rehabilitation ward. Age Ageing. 2008;37:277–81.
Nyberg L, Gustafson Y. Using the Downton index to predict those prone to falls in stroke rehabilitation. Stroke. 1996;27:1821–4.
Vassallo M, Stockdale R, Sharma JC, Briggs R, Allen S. A comparative study of the use of four fall risk assessment tools on acute medical wards. J Am Geriatr Soc. 2005;53:1034–8.
Olsson Möller UKJ, Midlöv PEC, Jakobsson U. Predictive validity and cut-off scores in four diagnostic tests for falls—a study in frail older people at home. Phys Occup Ther Geriatr. 2012;30:189–201.
Guideline for the prevention of falls in older persons.. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. J Am Geriatr Soc. 2001;49:664–72.
Gadkaree SK, Sun DQ, Huang J, Varadhan R, Agrawal Y Comparison of simple vs. performance-based fall prediction models: data from the National Health and Aging Trends Study. Gerontol Geriatr Med. 2015;1–10. https://doi.org/10.1177/2333721415584850.
da Costa BR, Rutjes AWS, Mendy A, Freund-Heritage R, Vieira ER. Can falls risk prediction tools correctly identify fall-prone elderly rehabilitation inpatients? A systematic review and meta-analysis. PLoS One. 2012;7:e41061.
Cohen JF, Korevaar DA, Altman DG, Bruns DE, Gatsonis CA, Hooft L, et al. STARD 2015 guidelines for reporting diagnostic accuracy studies: explanation and elaboration. BMJ Open. 2016;6:e012799. https://doi.org/10.1136/bmjopen-2016-012799.
Plichta SBKE Munro’s statistical methods for health care research, 6th edition. Philadelphia: Wolters Kluwer Health, Lippincott Williams & Wilkins; 2013. p 265.
Oliver D. Falls risk-prediction tools for hospital inpatients. Time to put them to bed? Age Ageing. 2008;37:248–50.
Franzen E, Conradsson D, Hagstromer M, Nilsson MH. Depressive symptoms associated with concerns about falling in Parkinson’s disease. Brain Behav. 2016;6:e00524.
Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21:658–68.
Acknowledgements
The authors wish to express their gratitude to all participants and staff members at the spinal rehabilitation units at Rehab Station Stockholm/Spinalis, Sweden and Sunnaas Rehabilitation Hospital, Norway. Thanks to Anneli Olausson for help with patient inclusion, Ellen E. Schaanning for help with data collection, Lisbet Broman for assistance with data management, Wim Grooten for support during analysis, and Salomé Cronjé for her help with the manuscript.
Funding
We acknowledge financial support from Rehab Station Stockholm, Sunnaas Rehabilitation Hospital, Neuro Sweden, Praktikertjänst, the Promobilia Foundation, the Spinalis Foundation and the Doctoral School in Health Care Sciences at Karolinska Institutet.
Author contributions
EBF contributed in the planning of the project, data collection, data analysis, and was the main author of the manuscript. VJ contributed with data collection, planning of the project, data analysis, and of the revision of manuscript. KSR contributed with planning of the project, review of data analysis and revision of the manuscript. CH contributed with planning of the project and revision of analysis and the manuscript. KW contributed with planning of the project and data analysis, review of data analysis and revision of the manuscript. EF contributed with planning of the project and data analysis, review of data analysis and revision of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Butler Forslund, E., Jørgensen, V., Skavberg Roaldsen, K. et al. Predictors of falls in persons with spinal cord injury—a prospective study using the Downton fall risk index and a single question of previous falls. Spinal Cord 57, 91–99 (2019). https://doi.org/10.1038/s41393-018-0175-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-018-0175-y