Abstract
Study design
Prospective cohort study with two times of measurement.
Objective
To assess the relationship between use of assistive devices for walking (at baseline) and the number of annual fall-related injuries (at follow-up) among a cohort of ambulatory adults with spinal cord injury (SCI).
Setting
Medical University in the Southeastern United States.
Methods
There were 622 ambulatory adults who met the eligibility criteria, 317 of whom completed both baseline and follow-up assessments. The participants completed a mailed self-report assessment (SRA) that measured self-reported number of fall-related injuries in the previous year, and the use of orthopedic equipment (assistive devices) for walking, including cane(s), crutches, walker, and braces, was assessed at both baseline and follow-up.
Results
The percentage of at least one self-reported fall-related injury decreased from 22% at baseline to 13% at the follow-up. Walker and cane use at baseline was significantly associated with fall-related injuries at follow-up. Participants using one walking device related to 194% greater number of fall injures, and using multiple device related to 730% greater number of fall injures than those who used no devices. We also found walker users were associated with 214% greater number of fall injures, while cane users were associated with 160% greater number of fall injures.
Conclusions
The probability of fall-related injury remained high among persons who are ambulatory after SCI. Health care professionals should be aware of the balance between the goal of ambulation and the potential increased risk of fall-related injuries associated with assistive device use.
Similar content being viewed by others
Introduction
Traumatic spinal cord injury (SCI) results in motor and sensory impairments below the neurologic level of injury, often significantly impacting activities such as ambulation. Return to walking is often reported as one of the main goals after SCI, and significant emphasis has been placed on rehabilitation interventions to improve functional walking outcomes [1,2,3]. However, while functional walking is associated with numerous benefits, ambulatory individuals with SCI may also be at an increased risk of experiencing falls [4, 5]. It is important to identify the types of assistive devices and other circumstances that relate to future falls.
According to SCI Model Systems data, the majority of ambulatory individuals (82.2%) report using assistive devices (e.g., cane, walker, crutches, braces, or orthotics), and use is increased as time since injury increases [6]. Other population-based cohorts of adults with SCI in the United States have found that roughly 66% of ambulatory adults use at least one assistive device, though longitudinal use has not been assessed [7, 8]. These assistive devices, used alone or in combination, can improve balance and mobility, but studies also found some devices usage might be associated with increased risk of falls [9, 10].
While studies on the relationship between assistive devices and falls are abundant, there is paucity of research on the effects of assistive devices on fall-related injuries, which are severe results of falls and lead to high health care utilization and excessive mortality. They are the most common unintentional injuries among ambulatory individuals with SCI. A recent study indicated participants who were independent in ambulation were 64% more likely to be involved in a fall-related injury than nonambulatory participants, and those who needed assistance for ambulation were 201% more likely to be injured related to a fall [11]. Saunders et al. [12] found that self-reported use of one crutch or cane was associated with increased risk of falls resulting in injuries. However, the limited literature was based on cross-sectional analysis, and evidence of fall-related injuries changing over time was lacking.
Longitudinal research is needed to better understand the relationships between assistive device use and fall-related injuries controlling for demographic and injury characteristics. Our purpose is to use data from a prospective cohort study to identify the relationship of device utilization and future fall-related injuries among ambulatory participants with SCI. The prospective cohort design makes our study unique in the research area in that it provides us the opportunity to identify the fall-related injuries prevalence over time by following up a cohort of chronic SCI, and it builds the temporal order to assess the impacts of assistive device use (walker, crutch, cane, and brace) on future fall-related injuries. It is a necessary step in developing the basis for future causal modeling of fall-related injuries.
Methods
Participants
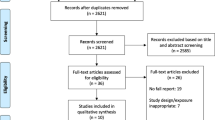
After obtaining approval from the institutional review board, participants were recruited from the South Carolina Spinal Cord Injury Surveillance System Registry (SCISSR) starting in 2011. The SCISSR is a population-based registry of traumatic SCI occurring in South Carolina (SC), covering all 62 acute care nonfederal hospitals in SC. They have a statutory requirement to report uniform billing discharge data to the state, and SCISSR used the billing data to select traumatic SCI cases according to the definition of the Centers for Disease Control and Prevention (i.e., International Classification of Diseases, 9th Revision codes: 806 and 952). SCISSR also randomly selected medical charts and verified the data quality, which found the data 99% accurate and complete [13]. All participants met the following criteria at the baseline: at least 18 years of age, 1-year post injury, treated acutely for SCI in SC, and traumatic SCI with residual neurologic impairment impeding full recovery. A total of 1160 participants completed the baseline self-reported assessment (SRA) between 2011 and 2018. After the initial baseline enrollment, the SC SCI Outcomes Database performed annual follow-up through the first 5 years post injury and then every 5 years thereafter. We excluded 538 who reported they were not able to walk at all or always used a wheelchair at home. The baseline sample included 622 ambulatory participants. Among them, 317 completed at least one follow-up measure. If a participant completed more than one follow-up measure, we used their most recent one to maximize the sample size for the longitudinal analyses. Their mean (SD) length of time between baseline and the most recent follow-up was 25 (16) months. Our longitudinal analyses used these 317 participants as the final study sample.
Procedures
At baseline, potential participants were sent introductory letters by mail to describe the study and alert them that materials would be forthcoming. The actual instruments of questionnaire were sent 4–6 weeks later. For those who did not respond to the first mailing, follow-up phone calls and then a second mailing were sent. Participants were offered $50 remuneration for completing the SRA. Similar procedures were utilized at the annual follow-up for participants who were within the first 5 years post injury. The follow-up started approximately one and half years after completion of the baseline SRA. Follow-up remuneration was $40.
Measures
The primary outcome measure was self-reported number of fall-related injuries at participants’ most recent follow-up, assessed by asking the following question, “In the past year, how many falls have you had that resulted in an injury serious enough to receive medical care in a clinic, emergency room, or hospital?” All the independent variables were measured at both baseline and follow-up by using the same data collection method. The use of assistive devices for walking (walker, crutch, cane(s), and brace(s)) was assessed in relation to fall-related injuries. Participants responded to the following questions: “(1) Do you use a standard or rolling walker to assist you in walking? (2) Do you use crutches to assist you in walking? (3) Do you use a cane(s) to assist you in walking? (4) Do you use short-leg braces when you walk? (5) Do you use long-leg braces when you walk?” For each device variable, we dichotomized the response (yes and no). The injury levels were grouped to cervical, thoracic, lumbar, and sacral levels. In the analyses, we combined the lumbar and sacral as other levels used for comparison reference group. Other covariates included years post injury, age, gender (male and female), race/ethnicity (non-Hispanic Black and others), and self-perceived body weight (overweight, underweight, and average weight).
Analyses
All analyses were conducted using SAS 9.4. Descriptive statistics were generated for all independent variables measured at baseline, and we also compared the whole baseline sample (n = 622) with the final study sample (n = 317). Then we did bivariate comparison between study participants with at least one fall-related injury and those without fall-related injury using Chi-square test. Since the number of fall-related injuries was a nonnegative integer with highly skewed distribution, we considered using the Poisson regression for the multivariate analyses. However, we found issues with over-dispersion using the Poisson regression models. Thus, the final multivariate analyses used the negative binomial regression model, which is a generalization of the Poisson model [14, 15]. We developed two negative binomial regression models using the number of fall-related injuries at the follow-up as the dependent variable: the first model focused on the different types of devices, and the second model explored the impacts of one device usage and multiple devices usage (using two or more different types of devices). The independent variables measured at baseline were used in the two models.
Results
Table 1 summarizes the participant characteristics and baseline assistive device use for 622 participants who have completed the baseline measurement and 317 participants study sample who completed both baseline and follow-up. We did not find substantial differences between the two samples at baseline. At baseline, 44% used at least one assistive device among 622 participants (including 28.5% using only one device, and 15.4% using multiple devices), and 48% used at least one assistive device among the 317 participants who completed the follow-up measure (including 30.3% using only one device, and 17.4% using multiple devices). Table 1 also presented the device usage for 317 participants at the follow-up (column 3). The percentage of walker users decreased from 22% at the baseline to 18% at the follow-up, and the percentage of brace users declined from 12 to 8%. The percentage of multiple assistive devices usage also dropped from 17% at the baseline to 13% at the follow-up.
Among 317 participants, the mean (SD) for fall-related injuries at baseline was 0.49 (1.41), ranging from 0 to 15 injuries. At baseline, 77 (22%) participants had at least one fall-related injury. At their most recent follow-up, the mean (SD) was 0.31 (1.11), ranging from 0 to 10 injuries, and there were 41 (13%) who had at least one fall-related injury. Table 2 compared the independent variables between those with at least one fall-related injury and those without fall-related injury at the follow-up. It indicated that participants using walker, cane, brace, or using multiple devices at the baseline were more likely to have fall-related injury at the follow-up.
The first negative binomial regression model (Table 3) used the baseline independent variables in temporal relationship with the fall-related injuries measured at follow-up. This longitudinal analysis indicated the relationships of walker and cane use with future fall-related injuries. Using a walker at baseline was associated with 214% greater number of fall-related injuries at follow-up (RR = 3.14) comparing with those who did not use a walker, while using a cane was related to 160% greater number of fall-related injuries (RR = 2.60) at follow-up comparing with those who did not use a cane. However, none of the other covariables was statistically significant. We did additional analyses to compare walker users to participants who did not use assistive device at all controlling for same demographic, injury characteristics and weight status, and the rate ratio (RR) increased to 5.67. The similar analyses applied to cane users and participants using no device, and the RR increased to 4.43.
Our second negative binomial regression model (Table 4) found one assistive device usage was associated with 194% greater number of fall-related injuries at follow-up (RR = 2.94), and the multiple assistive device usage was associated with 730% greater number of fall-related injuries (RR = 8.30) comparing with those who did not use walking device.
Discussion
The unique contribution of this study is the identification of the relationships between assistive device use and future fall-related injuries among ambulatory adults with SCI. It provides much stronger evidence of relationship between device use and falls when compared with existing cross-sectional studies. By establishing the association of the baseline factors related to equipment use with future fall-related injuries, this study is a prelude for building for the development of causal models.
We found baseline walker use was associated with a greater number of fall-related injuries at follow-up compared to other assistive devices. This finding may be related to higher walker use among individuals with more mobility limitations as the walker provides the most stability of all assistive devices. The increased number of fall-related injuries may be associated with the individual’s physical condition (e.g., frailty), other personal and environmental considerations, or use patterns. For instance, people who use walking devices also tend to be single, have lower income, are less educated, and are generally in poorer health [16].
In line with earlier results suggesting cane use is associated with a greater risk of falls among those with SCI [9, 12] and a high number of fall-related injuries in the general population [10, 16, 17], we found that baseline cane use was associated with increased risk of future fall-related injuries. The cane, which provides the least stability, may be used by individuals with a higher level of function, but it may not provide adequate stability when a loss of balance or misstep occurs.
In the first negative binomial model, the crutch usage and brace usage were not significantly associated with fall-related injury number, partly because smaller group of participants used them. However, most of the crutch users (83%) and brace users (79%) in our study were multiple devices users. Since multiple devices usage was highly related to fall-related injury (RR = 8.30), we should be cautious about the risk associated with crutch usage and brace usage as well. We also observed the percentage of having at least one fall-related injury dropped from 22% at baseline to 13% at the follow-up. One possible explanation is some participants became nonambulatory or had declined ambulatory ability at follow-up, and therefore had less fall-related injury. In our data, there were 6 participants became nonambulatory, and 19 participants unable to walk 10 m at the follow-up. Meanwhile, the percentage of multiple devices usage at the follow-up decreased to 13%, which might also contribute to the decrease of fall-related injury.
Methodologic considerations
The study included both strengths and limitations. The longitudinal data allow us to evaluate the relationship between baseline assistive devices equipment use and fall-related injuries at follow-up. However, this should not be interpreted as cause and effect. Particular caution must be used in interpreting the relationship between devices, such as a walker, or other safety measures and falls. Many other characteristics that are confounded with devices could account for the findings, so it is important for clinicians to be aware of the elevated risk of future falls, while not directly attempting to draw causality from the findings. However, the findings may be used to guide the search for causal links between equipment use and falls by helping to identify the minimal set of factors that may relate to future falls. Models of causality must consider equipment use to be both an indicator of function (i.e., certain types of function will lead to recommended use of different supported devices) and a potential contributor to fall-related injuries.
Second, use of a state-based population cohort is a distinct strength, as it reduces the likelihood of bias related to selective participation based on urban–rural status, ability to pay, and even severity of injury. Clinical facilities, including specialty hospitals, typically located in urban centers, may be more likely to admit individuals who can pay for services, and they are more likely to admit more severe cases of SCI (i.e., fewer ambulatory). That said, the participants likely were representative of people with SCI who have less severe complications that allow them to ambulate.
On the other hand, several limitations exist. First, the follow-up rate was 51%, which might lead to selection bias. Second, the outcome is based on a single estimation of falls. Future causal modeling will need to include the actual number of events leading to falls (i.e., the fall itself) to determine whether different devices are associated with differential risk of falls, with some devices more likely to lead to injuries. Third, similarly, our modeling does not include a detailed assessment of function which may be a more direct causative factor of fall-related injuries. It may therefore be that the devices themselves are basically a proxy measure for function, with a greater number of devices use by those who are more impaired. Under this circumstance, it would be important to note that the presence or need for multiple devices is a red flag that the individual will be at greater risk of future falls. Fourth, all data are self-report with unknown recall bias, which is inherent to all self-report data collection. Lastly, many participants were excluded because they were not ambulatory, which limited the statistical power to consider more independent variables in the multivariate analyses.
Future research
The relationship between walking devices and fall-related injuries is more complicated than what we have analyzed with the limitations in our current data, but our study built the first steppingstone to identify their longitudinal association. Continued research is necessary to understand better the personal characteristics of those who sustain serious fall-related injuries, as well as the circumstances in which these falls occur. This might help to resolve the conflicting evidence from the literature [9]. We need to work toward identification of causal paths, rather than merely identifying temporal relationships between variables. The current findings suggested that causal studies would benefit from identification of assistive device utilization which provides tips of functional limitations that may lead to fall-related injuries. We also need additional prospective cohort studies which include more detailed neurological (motor and sensory) and functional assessments which may precipitate the use and need for assistive devices. Increased education for the users on device fitting as well as research on the development of effective fall prevention strategies may help decrease the risk of falls and fall-related injuries among those who use assistive devices.
Conclusions
The probability of at least one fall-related injury decreased from 22% at baseline to 13% at the follow-up among adults with SCI who were ambulatory at baseline. However, the consequences of these injuries were severe, resulting in medical care in a clinic, emergency room, or hospital. Because walking devices usage was associated with increased risk of fall-related injury, health care professionals and caregivers should be aware of the balance between promoting ambulation after SCI and taking more precautions about the risks of fall-related injury for those who are ambulatory and use assistive devices.
Data availability
The data sets generated and/or analyzed during the current study are not publicly available due to the privacy concerns of study participants and are not standardized to be in a publicly interpretable format.
References
Behrman AL, Ardolino EM, Harkema SJ. Activity-based therapy: from basic science to clinical application for recovery after spinal cord injury. J Neurol Phys Ther. 2017;41:S39–45.
Morawietz C, Moffat F. Effects of locomotor training after incomplete spinal cord injury: a systematic review. Arch Phys Med Rehabilit. 2013;94:2297–308.
Mehrholz J, Harvey LA, Thomas S, Elsner B. Is body-weight-supported treadmill training or robotic-assisted gait training superior to overground gait training and other forms of physiotherapy in people with spinal cord injury? A systematic review. Spinal Cord. 2017;55:722–9.
Khan A, Pujol C, Laylor M, Unic N, Pakosh M, Dawe J, et al. Falls after spinal cord injury: a systematic review and meta-analysis of incidence proportion and contributing factors. Spinal Cord. 2019;57:526–39.
Wirz M, van Hedel HJA. Balance, gait, and falls in spinal cord injury. Handb Clin Neurol. 2018;159:367–84.
NSCISC. Annual statistical report. Birmingham, AL: University of Alabama; 2018.
Saunders LL, Krause JS, DiPiro ND, Kraft S, Brotherton S. Ambulation and complications related to assistive devices after spinal cord injury. J Spinal Cord Med. 2013;36:652–9.
Brotherton SS, Saunders LL, Krause JS, Morrisette DC. Association between reliance on devices and people for walking and ability to walk community distances among persons with spinal cord injury. J Spinal Cord Med. 2012;35:156–61.
Brotherton S, Krause JS, Nietert P. A pilot study of factors associated with falls in individuals with incomplete spinal cord injury. J Spinal Cord Med. 2007;30:243–50.
Bateni H, Maki BE. Assistive devices for balance and mobility: benefits, demands, and adverse consequences. Arch Phys Med Rehabilit. 2005;86:134–45.
Cao Y, DiPiro N, Li C, Roesler J, Krause JS. Behavioral factors and unintentional injuries after spinal cord injury. Arch Phys Med Rehabilit. 2020;101:412–7.
Saunders LL, DiPiro N, Krause JS, Brotherton S, Kraft S. Risk of fall related injuries among ambulatory participants with spinal cord injury. Top Spinal Cord Inj Rehabilit. 2013;19:259–66.
Cao Y, Selassie AW, Krause JS. Risk of death after hospital discharge with traumatic spinal cord injury: a population-based analysis, 1998–2009. Arch Phys Med Rehabilit. 2013;94:1054–61.
Cameron AC, Trivedi PK. Regression analysis of count data. New York: Cambridge Press; 1998.
Allison P. Logistic regression using SAS: theory and application. 2nd ed. Cary, NC: SAS Institute; 2012.
Stevens JA, Thomas K, Teh L, Greenspan AI. Unintentional fall injuries associated with walkers and canes in older adults treated in U.S. emergency departments. J Am Geriatr Soc. 2009;57:1464–9.
Bateni H, Heung E, Zettel J, McLlroy WE, Maki BE. Can use of walkers or canes impede lateral compensatory stepping movements? Gait Posture. 2004;20:74–83.
Funding
The contents of this publication were developed under grants from the South Carolina Spinal Cord Injury Research Fund (SCSCIRF) grants SCIRF 2017 SI-02, SCIRF 09–001, and from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) grant 90RT5003. NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this publication do not necessarily represent the policy of the SCSCIRF, NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government or the state of South Carolina.
Author information
Authors and Affiliations
Contributions
YC was the principal investigator and was responsible for the analyses, research methods and results sections, and contributed to the discussion and conclusion sections. NDD was responsible for the introduction and literature review, as well as contributing to the discussion and conclusion sections. SSB contributed to the introduction, discussion, and conclusion sections. JSK was responsible for the discussion and conclusion sections, and contributed to the overall development and editing of the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cao, Y., DiPiro, N.D., Brotherton, S.S. et al. Assistive devices and future fall-related injuries among ambulatory adults with spinal cord injury: a prospective cohort study. Spinal Cord 59, 747–752 (2021). https://doi.org/10.1038/s41393-020-00572-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-00572-7