Abstract
Background
The absence of nocturnal blood pressure dipping is associated with adverse cardiovascular outcomes in adults, and proteinuria is a risk factor for non-dipping in this population. Risk factors for non-dipping in children are largely unknown.
Methods
We retrospectively identified patients aged 5–19 years who underwent 24-h ambulatory blood pressure monitoring (ABPM) from August 2018 to January 2019 and had a spot urine protein-to-creatinine ratio (PCR) within 1 year of their ABPM. Dipping was defined as ≥10% reduction in systolic and diastolic blood pressure from day to night. Multivariable logistic and linear regression models evaluated the association of proteinuria with non-dipping.
Results
Among 77 children identified, 27 (35.1%) were non-dippers. Each two-fold higher urine PCR was associated with 38% higher odds of non-dipping, after adjusting for body mass index (BMI). Higher urine PCR was also associated with a lower diastolic dipping percentage by 1.33 (95% confidence interval 0.31–2.34), after adjusting for BMI, age, and estimated glomerular filtration rate.
Conclusions
Limitations of this study include its retrospective design and the time lapse between urine PCR and ABPM. Proteinuria appears to be associated with blood pressure non-dipping in children. This finding needs to be confirmed in prospective studies.
Impact
-
Our study demonstrates the association of proteinuria with non-dipping of blood pressure in children.
-
This association has been explored in adults, but to our knowledge, this is the first time it is evaluated in children referred for evaluation of elevated blood pressure.
-
Non-dipping is a modifiable risk factor for kidney function decline and cardiovascular disease in adulthood, and thus early identification in children is important. The association between proteinuria and non-dipping in children will allow us to more readily identify those at risk, with a future focus on interventions to modify blood pressure dipping patterns.
Similar content being viewed by others
Introduction
Along with the rising prevalence of hypertension in children, there has been a concomitant increase in the use of 24-h ambulatory blood pressure monitoring (ABPM) for diagnosis and treatment.1,2 Twenty-four-hour ABPM allows for the dynamic assessment of blood pressure including at night-time.3 In otherwise healthy children being evaluated for hypertension using ABPM, ~14% are found to lack the expected lower blood pressure at night, defined as “non-dippers.”3 The prevalence of non-dipping is much higher, at 39%, in children with chronic kidney disease (CKD).4 The exact pathophysiology of non-dipping remains unclear; however, non-dipping has been associated with increased nocturnal natriuresis.5
In adults, the absence of nocturnal blood pressure dipping is associated with adverse cardiovascular outcomes, including increased left ventricular hypertrophy (LVH) and mortality.6,7 In young adults who were followed for 10 years, inadequate systolic dipping was significantly associated with future subclinical coronary artery atherosclerosis.8 This is particularly important in pediatric populations, where few manifest clinical evidence of cardiovascular disease (CVD), yet identifying children at risk for future CVD may provide opportunities for primary prevention. Risk factors for non-dipping in adults include obesity, obstructive sleep apnea, and proteinuria.9,10,11 In children, prior studies identified obesity as a risk factor for non-dipping, but the relationship between proteinuria and non-dipping is unknown.3,12,13,14 Thus, the goal of this study was to describe the relationship between proteinuria and nocturnal non-dipping on 24-h ABPM in children. Based on the findings in adults, we hypothesized that greater proteinuria would be associated with nocturnal non-dipping in children, independent of obesity, kidney function, and other shared risk factors.
Methods
Data source
We conducted a retrospective, cross-sectional study in which we identified consecutive subjects aged 5–19 years who underwent 24-h ABPM at Rady Children’s Hospital in San Diego from August 2018 to January 2019. The study was approved by the Institutional Review Board at the University of California San Diego Health System (#200336).
Subject selection/methods
Subjects were included if they had either a urine protein or urine microalbumin and urine creatinine measurement within 1 year of their ABPM study. Exclusion criteria included age ≥20 years, inadequate ABPM study by which to define dipping patterns, as determined by the interpreting physician based on AHA criteria,1 as well as any known genetic tubular disease. Subjects underwent 24-h ABPM either as part of the evaluation for elevated blood pressure or for assessment of blood pressure control on anti-hypertensive therapy. Through chart review, we collected information, including age, sex, race, past medical history, birth history, prior diagnosis of hypertension, and current anti-hypertensives at the time of the ABPM. We also obtained the serum creatinine of closest proximity in timing to ABPM (within 3 years), and cardiac geometry data of closest proximity in timing to ABPM by echocardiography (within 2 years), including left ventricular mass index (LVMI in g/m2.7) and the presence of LVH.
Among the subset with missing urine protein-to-creatinine ratio (PCR), but available urine albumin and creatinine measurements (N = 7, 9.1%), we used the equation of Weaver et al.15 to transform the urine albumin to creatinine ratio to a urine PCR.
All ABPM studies were performed using a Spacelabs (Snoqualmie, WA) 90217 or 90227 monitor. The monitors had been placed by trained medical assistants or nursing staff at the time of the clinic visit. The appropriate cuff size was determined based on the “Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents” by the American Academy of Pediatrics.2 The monitor cycles every 20 min during wake times and every 30 mins during sleep to provide blood pressure readings. Patients and their families were asked to document an activity log, including sleep and wake times.
Dipping was defined as ≥10% reduction in mean systolic and diastolic blood pressure from day to night.1,2 Ambulatory hypertension was defined as a mean systolic or diastolic blood pressure ≥95th percentile for age, sex, and height during either the awake or sleep period, with all loads between 25 and 50%.1,16 Severe ambulatory hypertension was defined as a mean systolic or diastolic blood pressure ≥95th percentile for age, sex, and height during either the awake or sleep period, with at least one load >50%. Prehypertension was defined as a mean ambulatory blood pressure <95th percentile for age, sex, and height, with loads ≥25%.1,16 Mean systolic and diastolic 24-h indices were calculated by dividing the mean 24-h systolic or diastolic blood pressure by the 95th percentile for sex and height. LVH was defined as LVMI ≥95th percentile for age and sex.17 Estimated glomerular filtration rate (eGFR) for subjects <18 years of age was calculated by both the original Schwartz (Schwartz I) and bedside-Schwartz (Schwartz II) equations.18,19 Because cystatin C was unavailable in the majority of subjects, we were unable to calculate eGFR based on the creatinine-cystatin C-based CKiD equation. For subjects 18 years of age and older, eGFR was calculated by the Modification of Diet in Renal Disease (MDRD) four-variable equation.20 A diagnosis of CKD was assigned based on ICD-10 code, as documented in the electronic medical record.
Statistical analysis
Continuous variables were described as mean ± standard deviation. Means were compared using independent samples t test. Categorical variables were described by frequency and percent and compared using Pearson’s χ2 tests. Urine PCR (mg/mg) was log2 transformed to normalize the data. For our primary outcome of non-dipping, we utilized multivariable logistic regression models with the exposure of interest being log2 (PCR). We evaluated unadjusted and mutually adjusted models. Variables that were considered for adjustment included age, sex, body mass index (BMI) (kg/m2), and eGFR (Schwartz I or MDRD). We then employed backward selection to retain potential confounders in a final model, with a p value threshold for inclusion of <0.2. In the secondary analysis, we evaluated the association of log2 (PCR) with systolic and diastolic dipping (%) in multivariable linear regression models. Similarly, we employed backward selection to retain important confounders. A p value of <0.05 was considered significant. All statistical analyses were performed using IBM SPSS version 26 (Armonk, NY).
Results
General characteristics of subjects
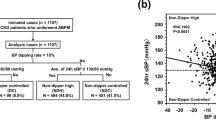
A total of 214 ABPM studies were completed between August 2018 and January 2019. Of these, one was a repeat ABPM on the same subject, and one subject with Lowe syndrome was excluded (tubular proteinuria). Twenty ABPMs were classified as inadequate quality by the interpreting physician. Of the remaining 192, 77 had a urine protein or urine microalbumin test within 1 year of the ABPM and were included in the study (Fig. 1). Two subjects had glomerular disease, one with immunoglobulin A (IgA) nephropathy and one with IgM nephropathy and nephrotic syndrome. Two subjects had secondary hypertension from Takayasu’s arteritis. The median time between ABPM and urine PCR was 25 days (interquartile range (IQR) −25 to +48), between ABPM and echocardiogram was 42 days (IQR −50 to +331,) and between ABPM and serum creatinine was 22 days (IQR −61 to +114).
The mean age of subjects was 14.2 ± 3.5 years. Females comprised 35.1% of the cohort. Nearly 57% of subjects were Hispanic and 5% were African American. The mean 24-h systolic blood pressure was 116.1 ± 13.2 mm Hg. The mean 24-h systolic blood pressure index was 0.92 ± 0.1. Mean eGFR (by Schwartz I or MDRD) was 152 ± 36.3 ml/min/1.73 m2, and median urine PCR was 0.07 [IQR 0.04, 0.12] mg/mg creatinine.
Among the 77 subjects, 27 were classified as non-dippers (35.1%). There were no significant differences in age, sex, race, anti-hypertensive use, or eGFR between dippers and non-dippers (Table 1). There was a trend towards higher BMI (mean difference 2.7 kg/m2, 95% confidence interval (CI) −0.41 to 5.84) and higher log2 (PCR) in non-dippers (mean difference 0.77, 95% CI −0.08 to 1.60). Non-dippers had a significantly higher LVMI (mean difference 6.9 g/m2.7, 95% CI 1.6–12.2) and significantly more LVH (30.4% vs. 5.1%, p = 0.01), as compared to dippers. There were no differences between dippers and non-dippers in regard to clinic blood pressure measurements.
Proteinuria and non-dipping
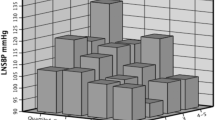
The distribution of log2 (PCR) by dipping status is shown in Fig. 2. The distribution was right skewed in non-dippers. Age, sex, eGFR, and blood pressure medication use were not found to be significant confounders in the analysis (p > 0.2). After backward selection, only log2 (PCR) and BMI were retained as covariates. In a model simultaneously adjusting for these two variables, a two-fold higher urine PCR was associated with 38% higher odds of non-dipping (1.38, 95% CI 1.01–1.88) and a 5 kg/m2 higher BMI was associated with 54% higher odds of non-dipping (1.54, 95% CI 1.00–2.29) (Table 2).
In the secondary analysis, a two-fold higher urine PCR was associated with a lower systolic dipping percentage by 0.72 (95% CI 0.002–1.44), after adjustment for BMI and sex (Table 3). Similarly, a two-fold higher urine PCR was associated with a lower diastolic dipping percentage by 1.33 (95% CI 0.31–2.34), after adjustment for BMI, age, and eGFR (Table 3). A grouped scatterplot of the correlation between systolic dipping percent and log2 (PCR) and diastolic dipping percent and log2 (PCR) is shown in Fig. 3. Diastolic dipping percentage appeared to associate more strongly with proteinuria than did systolic dipping percentage.
Discussion
We demonstrate that greater proteinuria is associated with non-dipping status in children who completed 24-h ABPM for either evaluation of elevated blood pressure or continued management of hypertension. In addition, our data corroborate prior studies showing that a higher BMI is associated with non-dipping.3,14 If associations in children mimic those seen in adults, then non-dipping on ABPM may identify children at higher risk for CKD progression and future CVD. Thus, identifying risk factors such as proteinuria may allow clinicians to better recognize children who may benefit from serial ABPM monitoring and more aggressive primary prevention strategies.
While little is known about non-dipping in children, it is known to be associated with adverse clinical outcomes in adults. In participants of the Jackson Heart Study, reverse dipping (higher systolic blood pressure at night than day) was associated with increased LVMI and higher prevalence of LVH, even after adjustment for mean daytime systolic blood pressure.21 Similar findings have been demonstrated in adult hemodialysis populations.22 Non-dipping has also been associated with a more rapid decline in kidney function in adults.23 Data pertaining to blood pressure dipping and its association with adverse clinical outcomes in the pediatric population is more limited. In a longitudinal study of adolescents with Type 1 diabetes mellitus, non-dipping was associated with hyperfiltration at a 2-year follow-up.24 In a small cross-sectional study of children with CKD, lower systolic blood pressure dipping was associated with lower eGFR.25 Non-dipping has also been associated with surrogate CVD biomarkers in children. An abnormal dipping pattern was associated with an increased likelihood of LVH in children with stages 3–5 CKD.26 In addition, in a cross-sectional study of healthy children, dipping patterns were a significant determinant of pulse wave velocity, independent of BMI and other risk factors.27,28 In 20 subjects with pediatric-onset systemic lupus erythematosus, isolated blood pressure non-dipping was associated with endothelial dysfunction and greater intima–media thickness.29 We add to these studies by demonstrating that proteinuria is associated with non-dipping in hypertensive children and adolescents. This is important as the identification of children with non-dipping may allow for early intervention, as dipping patterns may be modifiable. In adults, adjustment of the timing of anti-hypertensive medication from morning to evening resulted in lower night-time blood pressure, improved overall 24-h blood pressure, and reduced proteinuria.30,31 In a trial of adults with CKD and hypertension, night-time dosing of at least one anti-hypertensive medication significantly reduced the risk of CVD at a 5-year follow-up.32 Recently, a pilot study in pediatric kidney transplant recipients demonstrated that the addition of a short-acting blood pressure medication in the evening increased systolic dipping and restored normal dipping profile in 53% of non-dippers who received the intervention.33 Although this study only included transplant patients and evaluated additive therapy, it demonstrates that nocturnal dipping is modifiable in children. Thus, non-dipping is a modifiable risk factor for CVD, at least in adults, and further studies are needed to determine if it is in the pediatric population as well. Adjustment of the timing of anti-hypertensive therapy provides a feasible intervention that may induce normal dipping profiles in children, and larger, randomized controlled trials in the pediatric population are needed to determine if this will translate into improved clinical outcomes.
A clear understanding of the risk factors associated with non-dipping is important in identifying patients who would benefit from 24-h ABPM. In adults with resistant hypertension, microalbuminuria was more strongly associated with elevated night-time systolic blood pressure than with any other office or 24-h ABPM parameter.34 Likewise, a study by Afsar and Elsurer35 evaluated 24-h urinary albumin excretion (UAE) rates in hypertensive adults and found that non-dippers had higher UAE.35 Interestingly, those with both systolic and diastolic non-dipping had higher UAE than those with isolated systolic or diastolic non-dipping. Fewer studies have been done in children evaluating the association of proteinuria with non-dipping, and existing studies are limited to children with diabetes. In a prospective study that followed adolescents with type 1 diabetes mellitus, an increase in nocturnal systolic pressure was significantly associated with the development of microalbuminuria during follow-up.36 Only six of our participants had diabetes. Thus, to our knowledge, our study is the first to investigate the association of proteinuria with non-dipping in a more general pediatric cohort referred for evaluation of elevated blood pressure.
The pathophysiology of abnormal diurnal variation of blood pressure is not well understood, although a number of pathways might play a role. Overactivation of the sympathetic nervous system, an abnormal hormone profile (elevated catecholamines, renin, or aldosterone), and high dietary sodium load have all been proposed as potential mediators of this phenomenon.37 The mechanism underlying the association between proteinuria and non-dipping is similarly unclear. We hypothesize that proteinuria may identify persons with impaired excretion of daytime dietary sodium load. A decrease in the ability to effectively excrete sodium may lead to elevated nocturnal blood pressure as a compensation mechanism to enhance natriuresis overnight, if insufficient sodium is excreted during the daytime hours.38 This hypothesis requires further investigation.
Our study has important limitations. First, the sample size is small, which limits the statistical power to capture more subtle differences in demographics between dippers and non-dippers. Nonetheless, this study is relatively large compared to other ABPM studies in pediatric populations. Second, the cross-sectional design of our study prevents us from making any interpretations about causality. Third, the urine PCR was obtained within 1 year of ABPM date; given the time lapse between the collection of these data, there is potential for misclassification. Such misclassification would likely be non-differential with respect to dipping patterns, and thus would likely bias the results towards the null hypothesis. In addition, given the retrospective design of the study, we do not have serial measurements of urine PCR for each subject or data from 24-h urine collections, which is a source of information bias. Further prospective studies with simultaneous ABPM and 24-h urine protein collections are needed. Fourth, because of the nature of our question, we selected only subjects who had obtained either a urine protein or urine microalbumin test and included only children who were referred for ABPM measurements at our academic pediatric hospital, resulting in selection bias. Finally, our cohort is 57% Hispanic, so generalizability to other populations is limited, and results should be confirmed in other settings.
In conclusion, greater proteinuria is associated with non-dipping status in children. Prospective studies are needed to further delineate this relationship and allow for a better understanding of the pathophysiology. Given the significant impact of non-dipping on clinical outcomes in adults, the finding that non-dipping may be modifiable, and such modifications translate into a lower risk of CVD and mortality in adults, there is an urgent need to identify additional risk factors for non-dipping, its associations with clinical outcomes, and its ability to be modified in children. As both abnormal dipping patterns and higher urine PCR are strongly associated with adverse outcomes in adults, our results suggest that children found to have non-dipping should be evaluated with a urine PCR, and, conversely, those with proteinuria may benefit from 24-h ABPM evaluation.
References
Flynn, J. T. et al. Update: ambulatory blood pressure monitoring in children and adolescents. Hypertension 63, 1116–1135 (2014).
Flynn, J. T. et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140, e20171904 (2017).
Macumber, I. R., Weiss, N. S., Halbach, S. M., Hanevold, C. D. & Flynn, J. T. The association of pediatric obesity with nocturnal non-dipping on 24-hour ambulatory blood pressure monitoring. Am. J. Hypertens. 29, 647–652 (2016).
Mitsnefes, M. et al. Masked hypertension associates with left ventricular hypertrophy in children with CKD. J. Am. Soc. Nephrol. 21, 137–144 (2010).
Sachdeva, A. & Weder, A. B. Nocturnal sodium excretion blood pressure dipping, and sodium sensitivity. Hypertension 48, 527–533 (2006).
Cuspidi, C., Giudici, V., Negri, F. & Sala, C. Nocturnal nondipping and left ventricular hypertrophy in hypertension: an updated review. Expert Rev. Cardiovasc. Ther. 8, 781–792 (2010).
Liu, M. Non-dipping is a potent predictor of cardiovascular mortality and is associated with autonomic dysfunction in haemodialysis patients. Nephrol. Dial. Transplant. 18, 563–569 (2003).
Viera, A. J. et al. Nighttime blood pressure dipping in young adults and coronary artery calcium 10-15 years later: the coronary artery risk development in young adults study. Hypertension 59, 1157–1163 (2012).
De La Sierra, A. et al. Prevalence and factors associated with circadian blood pressure patterns in hypertensive patients. Hypertension 53, 466–472 (2009).
Crinion, S. J. et al. Nondipping nocturnal blood pressure predicts sleep apnea in patients with hypertension. J. Clin. Sleep Med. 15, 957–963 (2019).
Agarwal, R. & Light, R. P. GFR, proteinuria and circadian blood pressure. Nephrol. Dial. Transplant. 24, 2400–2406 (2009).
Framme, J. et al. 24-h Systolic blood pressure and heart rate recordings in lean and obese adolescents. Clin. Physiol. Funct. Imaging 26, 235–239 (2006).
Westerståhl, M. & Marcus, C. Association between nocturnal blood pressure dipping and insulin metabolism in obese adolescents. Int. J. Obes. 34, 472–477 (2010).
Westerståhl, M. et al. Nocturnal blood pressure non-dipping is prevalent in severely obese, prepubertal and early pubertal children. Acta Paediatr. 103, 225–230 (2014).
Weaver, R. G. et al. Estimating urine albumin-to-creatinine ratio from protein-to-creatinine ratio: development of equations using same-day measurements. J. Am. Soc. Nephrol. 31, 591–601 (2020).
Wühl, E., Witte, K., Soergel, M., Mehls, O. & Schaefer, F. Distribution of 24-h ambulatory blood pressure in children: normalized reference values and role of body dimensions. J. Hypertens. 20, 1995–2007 (2002).
Khoury, P. R., Mitsnefes, M., Daniels, S. R. & Kimball, T. R. Age-specific reference intervals for indexed left ventricular mass in children. J. Am. Soc. Echocardiogr. 22, 709–714 (2009).
Schwartz, G. J., Haycock, G. B., Edelmann, C. M. Jr. & Spitzer, A. A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58, 259–263 (1976).
Schwartz, G. J. et al. New equations to estimate GFR in children with CKD. J. Am. Soc. Nephrol. 20, 629–637 (2009).
Levey, A. S. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann. Intern. Med. 130, 461 (1999).
Abdalla, M. et al. Associations of blood pressure dipping patterns with left ventricular mass and left ventricular hypertrophy in blacks: The Jackson Heart Study. J. Am. Heart Assoc. 6, e004847 (2017).
Rahman, M., Griffin, V., Heyka, R. & Hoit, B. Diurnal variation of blood pressure; reproducibility and association with left ventricular hypertrophy in hemodialysis patients. Blood Press. Monit. 10, 25–32 (2005).
Davidson, M. B., Hix, J. K., Vidt, D. G. & Brotman, D. J. Association of impaired diurnal blood pressure variation with a subsequent decline in glomerular filtration rate. Arch. Intern. Med. 166, 846 (2006).
Lovshin, J. A. et al. Hyperfiltration, urinary albumin excretion, and ambulatory blood pressure in adolescents with type 1 diabetes mellitus. Am. J. Physiol. Ren. Physiol. 314, F667–F674 (2018).
Mitsnefes, M. M., Kimball, T. R. & Daniels, S. R. Office and ambulatory blood pressure elevation in children with chronic renal failure. Pediatr. Nephrol. 18, 145–149 (2003).
Gupta, D., Chaturvedi, S., Chandy, S. & Agarwal, I. Role of 24-h ambulatory blood pressure monitoring in children with chronic kidney disease. Indian J. Nephrol. 25, 355–361 (2015).
Correia-Costa, A. et al. Determinants of carotid-femoral pulse wave velocity in prepubertal children. Int. J. Cardiol. 218, 37–42 (2016).
Correia-Costa, L. et al. Association of myeloperoxidase levels with cardiometabolic factors and renal function in prepubertal children. Eur. J. Clin. Invest. 46, 50–59 (2016).
Chang, J. C. et al. Nocturnal blood pressure dipping as a marker of endothelial function and subclinical atherosclerosis in pediatric-onset systemic lupus erythematosus. Arthritis Res. Ther. 22, 129 (2020).
Zhao, P., Xu, P., Wan, C. & Wang, Z. Evening versus morning dosing regimen drug therapy for hypertension. Cochrane Database Syst. Rev. CD004184 (2011).
Glasser, S. P., Neutel, J. M., Gana, T. J. & Albert, K. S. Efficacy and safety of a once daily graded-release diltiazem formulation in essential hypertension. Am. J. Hypertens. 16, 51–58 (2003).
Hermida, R. C., Ayala, D. E., Mojón, A. & Fernández, J. R. Bedtime dosing of antihypertensive medications reduces cardiovascular risk in CKD. J. Am. Soc. Nephrol. 22, 2313–2321 (2011).
Sethna, C. B. et al. Restoration of nocturnal blood pressure dip and reduction of nocturnal blood pressure with evening anti-hypertensive medication administration in pediatric kidney transplant recipients: a pilot randomized clinical trial. Pediatr. Transplant. e13854 (2020).
Oliveras, A., Armario, P., Martell-Claros, N., Ruilope, L. M. & De La Sierra, A. Urinary albumin excretion is associated with nocturnal systolic blood pressure in resistant hypertensives. Hypertension 57, 556–560 (2011).
Afsar, B. & Elsurer, R. Urinary albumin excretion among nondipper hypertensive patients is closely related with the pattern of nondipping. J. Am. Soc. Hypertens. 4, 196–202 (2010).
Lurbe, E. et al. Increase in nocturnal blood pressure and progression to microalbuminuria in type 1 diabetes. N. Engl. J. Med. 347, 797–805 (2002).
Kanbay, M., Turgut, F., Erkmen Uyar, M., Akcay, A. & Covic, A. Causes and mechanisms of nondipping. Hypertension 30, 585–597 (2008).
Granger, J. P., Alexander, B. T. & Llinas, M. Mechanisms of pressure natriuresis. Curr. Hypertens. Rep. 4, 152–159 (2002).
Acknowledgements
This work was supported by the National Institutes of Diabetes and Digestive and Kidney Disease through Grants 5T32DK104717-04 (C.Y.B.), K23 DK114556 (P.S.G.), and K24 DK110427 (J.H.I.).
Author information
Authors and Affiliations
Contributions
C.Y.B, J.H.I., and P.S.G.: substantial contributions to conception and design, and analysis and interpretation of data. C.Y.B. and K.T.V.: acquisition of data. C.Y.B., K.T.V., C.E.C., F.B.G., J.H.I., and P.S.G.: drafting the article and revising it critically for important intellectual content, and final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Statement of consent
This retrospective, cross-sectional study was approved by the UCSD IRB (#200336). Consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bakhoum, C.Y., Vuong, K.T., Carter, C.E. et al. Proteinuria and nocturnal blood pressure dipping in hypertensive children and adolescents. Pediatr Res 90, 876–881 (2021). https://doi.org/10.1038/s41390-020-01315-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-01315-3
This article is cited by
-
Hypertension in Wilms tumor
Pediatric Nephrology (2024)