Abstract
Innovative breakthroughs in nanotechnology are having a substantial impact in healthcare, especially for brain diseases where effective therapeutic delivery systems are desperately needed. Nanoparticle delivery systems offer an unmatched ability of not only conveying a diverse array of diagnostic and therapeutic agents across complex biological barriers, but also possess the ability to transport payloads to targeted cell types over a sustained period. In substance use disorder (SUD), many therapeutic targets have been identified in preclinical studies, yet few of these findings have been translated to effective clinical treatments. The lack of success is, in part, due to the significant challenge of delivering novel therapies to the brain and specific brain cells. In this review, we evaluate the potential approaches and limitations of nanotherapeutic brain delivery systems. We also highlight the examples of promising strategies and future directions of nanocarrier-based treatments for SUD.
Similar content being viewed by others
Introduction
Substance use disorder (SUD) is a devastating brain disease that inflicts enormous emotional and economic cost to the individual, families, and society [1, 2]. Despite the clinical importance of limiting the development of drug craving and relapse, relatively few pharmacological treatments for SUD have received FDA approval within the last 20 years [3, 4], and currently there are no approved medications for cocaine, methamphetamine, and cannabis use disorders. Although researchers have identified many validated targets in preclinical studies [5], most large pharmaceutical companies show little interest in developing and testing novel SUD treatments [6]. Another major factor that limits therapeutic innovation for SUD and other neuropsychiatric disorder is the lack of methods to safely and effectively deliver therapeutic molecules to the brain. The brain is protected by the blood-brain barrier (BBB), which excludes large-molecule therapeutics and the vast majority of small-molecule drugs [7]. Furthermore, brain regions that drive drug craving and relapse are anatomically and functionally heterogeneous, creating a growing need for treatments that target specific cell types [8]. Thus, improvements in neurotherapeutic delivery systems are required to effectively treat SUD.
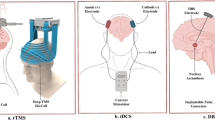
For many years in neuroscience research, the use of viral vectors has been the primary method to label and manipulate specific brain cells and circuits [9]. While viruses are excellent tools to study the brain in preclinical SUD models, limitations such as inadequate brain penetration following systemic delivery, constitutive expression, potential immune response, and cargo size restrictions have diminished the clinical utility of viral vectors as a SUD therapeutic [10]. On the other hand, non-toxic, biocompatible nanocarrier systems have emerged as a potential strategy to address the challenges of brain delivery that have hindered the advancement of many SUD treatments. As a putative therapeutic approach for SUD, nanoparticle delivery systems have several advantages, including 1) diverse therapeutic delivery applications (nucleic acid-based agents, peptides, proteins, small molecules, etc.), 2) tunable release rate lasting several days, 3) biocompatible and relatively low toxicity, 4) brain penetrating properties due to small size and stealth coating, and 5) adaptable to surface modifications for cell type-specific delivery [11] (Fig. 1). Additionally, several nanoparticle formulations have recently received FDA approval, further supporting their safety and efficacy in a variety of diseases [12]. In this review, we highlight advances in brain-targeted nanoparticle technologies and discuss ongoing and future directions of nanoparticle delivery systems for the treatment of SUD. Importantly, non-nanoparticle therapeutic delivery techniques such as new viral vectors [13, 14], genetically modified skin grafts [15], and ultrasound-mediated drug delivery [16] are also promising treatment strategies for SUD, and these and other approaches are summarized in previously published manuscripts [17,18,19,20].
Types of nanoparticles for brain delivery
Polymeric nanoparticles
Biodegradable polymeric nanoparticles have diverse drug delivery capabilities making them well suited for brain-targeted applications [21] (Fig. 1). Formulated from natural and synthetic polymers, polymeric nanoparticles are able to encapsulate therapeutics agents ranging from small molecules to biologic macromolecules [22]. An advantage of polymeric nanoparticles is that the polymer composition and surface properties may be adjusted to control the release rate and promote cell type-specific delivery of the therapeutic contents [23, 24]. In preclinical models, multiple polymeric nanoformulations have been successfully tested for brain delivery applications, including but not limited to polyamidoamine (PAMAM), Poly-lactic-co-glycolic acid (PLGA), polylactic acid (PLA), polylactic acid hyperbranched polyglycerol (PLA-HPG), and chitosan [25,26,27,28]. PAMAM-bound siRNAs, for example, showed greater efficacy and accumulation in the brain compared to the free siRNA [29]. FDA-approved PLGA nanoparticles are also capable of crossing the blood-brain barrier and are remarkably safe as the polymers are broken down to lactic acid and co-glycolic acids—natural metabolites of glycolysis [30]. For brain targeted applications, one preclinical study revealed that PLGA nanoparticles coated with polysorbate 80 and poloxamer 188 significantly improved central nervous system (CNS) delivery [31]. With improved sustained-release properties, PLA and PLA-HPG nanoparticles [32, 33] are being investigated as a potential delivery system for Alzheimer’s disease treatments [34, 35]. To improve brain biodistribution, other researchers have found that conjugating trans-activating transcriptor (TAT) peptide to PLA nanoparticles dramatically increased brain uptake in mice [36]. Several other surface modifications to polymeric nanoparticles have also been shown to increase brain delivery of the therapeutic cargo [37,38,39].
Although polymeric nanoparticles have many positive characteristics for brain delivery, they are not without limitations. For example, the accumulation of polymeric nanoparticles in the liver before the treatment reaches the brain may reduce the therapeutic effect [39, 40]. Uptake by the reticuloendothelial system may also lead to rapid clearance from systemic circulation [40]. Increased clearance and lower distribution may require higher and/or more frequent doses, which may result in unwanted side effects. Nevertheless, polymeric nanoparticles have proven to be versatile in nature, given the ability to encapsulate various types of payloads that can potentially penetrate the blood-brain barrier.
Liposomes
Liposomes are nanovesicles composed of phospholipids that produce a lipid bilayer with a hydrophilic aqueous inner core. Liposomes are able to encapsulate and deliver a variety of therapeutic cargo including hydrophilic and hydrophobic drugs, nucleic acids, peptides, and proteins [41,42,43,44] (Fig. 1). The recent success of the Moderna and Pfizer/BioNTech COVID-19 mRNA vaccines, which utilize liposomal delivery systems, has given considerable prominence to this nanoparticle class. Similar liposomal technologies have also been used for brain delivery. For example, nucleic acid-based therapeutics have been delivered to the brain with surface-modified liposomes in animals [45]. In brain delivery experiments, polyethylene-glycol conjugated liposomes were observed to have a greater therapeutic effect than free drug in rats [46]. In clinical studies, Doxil, a liposomal drug formulation for cancer, has been shown to effectively treat glioblastoma [47], and other liposome-based formulations are being investigated for the treatment of Alzheimer’s disease [48]. Although liposomes are versatile in nature, they also carry some downsides in their delivery properties. For example, nonspecific uptake and binding to serum proteins occurs in the bloodstream, requiring high doses to be used for efficacy [49]. Ligand conjugation can increase the binding of liposomes to specific tissues. As example of this approach, Costa and colleagues used liposomes conjugated to chlorotoxin for a more efficient brain targeted therapeutic delivery in mice [50]. Overall, liposomal formulations have strong potential in brain delivery given their ability to mimic membrane properties and cross the blood-brain barrier.
Solid lipid nanoparticles
Solid lipid nanoparticles (SLNs) are nanocarriers consisting of a lipid core matrix stabilized by an emulsifier, but do not use a bilayer system as in liposomes [51]. SLNs have been favored for drug delivery due to their optimal release profiles and longer shelf life compared to liposome formulations [52]. An attractive characteristic of SLNs is their small size, which may allow them to cross the blood-brain barrier more efficiently than other nanodelivery systems [53]. As SLNs are composed from physiologically similar lipids, they have potentially fewer toxic liabilities [54]. Improved brain targeting with SLNs has been achieved by conjugating ligands to the surface and adding specific coatings to increase brain uptake. For example, coating SLNs with bovine serum albumin was shown to increase transport to the brain in preclinical studies [55]. However, SLNs do have some limitations. Due to their small size, SLNs are subject to rapid release and low loading [56]. Nevertheless, SLNs have the potential to be major aids in brain delivery applications due to their safety profile and controlled release properties.
Gold nanoparticles
Gold nanoparticles have been successfully used for therapeutic brain delivery in preclinical studies [57]. Gold nanoparticles contain an inner inorganic layer surrounded by a nonpolar organic monolayer that stabilizes the inner core and interacts with the environmental targets [58]. This approach enhances solubility and protects the inner core from degradation. The main difference between gold nanoparticles and the previously discussed delivery systems is that the payload binds to the surface of the gold core instead of encapsulation [59]. Gold nanocarriers are capable of delivering a wide range of therapeutics range from antibiotics to DNA, due to their ability to conjugate to a diverse set of molecules [60, 61]. Like other nanoparticle systems, gold nanoparticles are adaptable to surface modifications allowing for brain and/or cell type-specific targeting [62]. With their small size (<100 nm), gold nanoparticles have been shown to cross the blood-brain barrier in multiple preclinical studies [63, 64]. However, in some experiments, unmodified, highly charged gold nanoparticles have been shown to induce an immune response in the brain, which may limit their therapeutic potential as a SUD treatment [65] (Fig. 1). To address this potential liability, surface modifications that alter the positive charge of the gold nanoparticles have been shown to minimize the potential toxic side effects [66].
Nanoparticle-based treatments for SUD
Small molecule drugs
Nanoparticles have the potential to bolster the therapeutic efficacy and utility of many FDA-approved small molecule treatments for SUD and SUD-related overdoses (Table 1). For example, naloxone is widely used to reverse opioid-induced respiratory depression, but because of its low oral bioavailability [67], it is typically administered intramuscularly, intranasally, or intravenously. Additionally, naloxone, when acutely administered, has a shorter half-life than many abused opioids, which may lead to renarcotization and a recurrence of opioid-induced respiratory depression [68]. To address these issues, researchers developed polymeric nanoparticles bound to naloxone (NP-naloxone) and demonstrated that this formulation greatly increased the oral bioavailability of naloxone and offered better protection from opioid overdose in animals by producing a sustained naloxone release [69]. Furthermore, this nanoparticle-based approach has the potential to decrease incidences of opioid antagonist-induced withdrawal, a common drawback of traditional naloxone dosage forms. Unlike some parenteral naloxone formulations, this orally administered NP-naloxone formulation possessed a long duration of action in mice (≥ 24 hours), while maintaining the quick onset of action properties. Consistent with the previous studies, other naloxone-bound nanoparticle formulations were shown to competitively displace morphine from the mu-opioid receptor and selectively block morphine’s antinociceptive effects in opiate-dependent mice without causing precipitated opioid withdrawal symptoms [70]. More recently, intranasal delivery of naloxone-loaded lipid nanoparticles was found to be effective at reversing opioid-induced overdose in rats, while also showing greater brain biodistribution compared to naloxone alone [71]. Additional preclinical studies are needed to determine if these nanoparticle formulations are also effective at reversing the actions of other, highly potent opioids (e.g., fentanyl) and whether these naloxone formulations have the potential to reduce drug-seeking and -taking behaviors in animal models of SUD. Furthermore, small molecules that act through non-opioidergic pathways have also been shown to reduced opioid-induced respiratory depression in animals [72], and additional studies are needed to determine if nanoparticle formulations have the potential to improve the pharmacokinetic properties, efficacy, and cell type-specific delivery of these small molecules.
While the previous section focused on nanoformulations for the reversal of opioid-induced respiratory depression, nanoparticle-bound small molecules are also being utilized for long-term SUD treatment. For example, naltrexone is a potent opioid receptor antagonist that attenuates the reinforcing effects of opioids and reduces alcohol craving and intake in humans [73, 74], but because of its poor oral bioavailability and relatively short duration of action, daily oral medication is typically required [75]. As daily medication noncompliance is a major issue associated with naltrexone and other SUD treatments [76], researchers as early as the mid-1970s began to develop sustained release, injectable polymer formulations for opioid receptor antagonists [77,78,79]. This line of research eventually lead to the FDA-approved, long-acting intramuscular injection form of naltrexone-bound PLGA nanoparticles (Vivitrol®) for the treatment of alcohol and opioid dependence [80,81,82]. Although Vivitrol® improved noncompliance issues associated with oral naltrexone, patients must return for treatment once a month, which again contributes to high attrition rates [83]. For longer sustained release of naltrexone (>1 month), polymer pellet implants [84,85,86], microspheres [87, 88], and nanogel [89] formulations are currently undergoing preclinical and/or clinical testing.
In other preclinical studies, Masoumi and EsmaeiliIn (2020) developed a nanoparticle formulation containing rifampin and buprenorphine as a potential treatment for opioid dependence. Rifampin is a potent inducer of numerous cytochrome P450 enzymes and will effectively decrease the serum concentrations of many substrates (i.e., opioids), and buprenorphine is a mixed agonist–antagonist opioid receptor modulator that reduces symptoms of opioid withdrawal and craving [90]. However, this approach might be problematic from a clinical prospective, as rifampin has been shown to alter buprenorphine metabolism [91], potentially causing withdrawal symptoms. Other lipid nanoparticles containing buprenorphine have also been investigated in pain studies [92] but have yet to be tested in SUD models. Overall, using nanoparticle formulations to promote the sustained release of small molecule SUD treatments is an effective strategy to increase patient compliance and clinical outcomes. Going forward, researchers are encouraged to investigate the ability of nanoformulations to improve the effectiveness of other small molecules that have shown promise in preclinical and clinical SUD studies.
Vaccines
Vaccines are a promising approach for the treatment of SUD [93]. SUD vaccines work by initiating the production of drug-specific antibodies that rapidly bind to the drug of abuse. This mechanism reduces the ability of the drug to cross the blood-brain barrier and thus attenuates the rewarding effects of the abused substance. In recent years, multiple nicotine vaccines have been tested in clinical trials but have failed to significantly alter smoking cessation [94]. The failure of these conjugate nicotine vaccines is likely due to their suboptimal intrinsic properties, such as insufficient recognition and internalization by immune cells, low bioavailability, and rapid degradation, all of which contribute to poor immunological efficacy [95]. To address these shortcomings, Zhao and colleagues developed a lipid-polymeric nanoparticle-based nicotine vaccine and found that it had improved cellular uptake by dendritic cells and immunogenicity in mice compared to conjugate vaccines [96]. In other preclinical studies, researchers demonstrated that the immunogenicity and pharmacokinetic efficacy of the nicotine nanovaccine, called NanoNicVac, could be improved by modulating the nanoparticle size, hapten density and localization, carrier proteins, adjuvants, and release rate [97,98,99] (Table 1). With these improvements, NanoNicVac was found to reduce brain levels of nicotine by 71% in mice [99]. Consistent with the previous studies in mice, the nicotine nanoparticle vaccine, SEL-068, effectively reduced the discriminative-stimulus effects of nicotine in nonhuman primates [100]. Importantly, these findings with nicotine have the potential to be applied to nanoparticle-based vaccines for other drugs of abuse.
Immunopharmacotherapy for cocaine use disorder is another emerging area of research [101]. Previous studies have shown that conjugate cocaine vaccines yielded a modest level of anticocaine antibodies and reduced cocaine seeking in multiple animal models [101,102,103]. However, because cocaine has poor immunogenic properties, improved strategies are needed ensure a robust and sustained anti-cocaine antibody response. By conjugating a cocaine analog to a nanoparticle carrier with major histocompatibility complex (MHC) II-binding moieties, researchers were able to generate a prompt, persistent, and high-affinity anti-cocaine antibody response in animals [104]. Using this nanoparticle approach, brain levels of cocaine were reduced by 80% in mice, and in behavioral studies, conditioned place preference for cocaine was significantly attenuated in nanoparticle-treated mice. Together, these studies demonstrate that nanoparticles significantly improve the effectiveness of SUD vaccines in animal models.
While SUD vaccines have shown promise in animal studies, first-generation vaccines for nicotine and cocaine have failed to demonstrate efficacy in phase III clinical trials [105, 106]. From these initial clinical studies, several ongoing challenges for SUD vaccines have been identified, some of which may be addressed by using nanoparticle delivery systems. For example, in SUD vaccine clinical studies, only a subset of individuals achieved sufficient drug-specific antibody levels [107]. Nanocarrier systems have the potential to alleviate this issue, as nanoparticle-based vaccines exhibited improved immunogenicity and pharmacokinetic efficacy for drugs of abuse and other targets in animals compared to conjugate vaccines [97, 108, 109], but human studies are needed to determine if these effects are translatable. To further improve SUD vaccine efficacy in humans, additional research with conjugate and nanoparticle-based vaccines should focus on understanding the factors that contribute to individual variability in immune response following vaccination (e.g., age, sex genetics, immune system health, history/pattern of drug use, vaccine regimen, antibody selectivity and affinity for the target drug, etc.). This information will help clinicians identify the subset of patients that are most likely benefit from SUD vaccines. Finally, the clinically tested SUD vaccines do not address polysubstance use or the likelihood of a person substituting one drug of abuse for another to circumvent the vaccine. Given the elevated prevalence of polysubstance use [110] and that many drugs of abuse are now laced with synthetic opioids, the development of multivalent vaccines will be essential to improve clinical outcomes. In animal studies, bivalent vaccines that target different opioids have demonstrated effectiveness in initial experiments [111,112,113], and multivalent nanoparticle vaccines have shown promise in other disease models [114, 115] but have not been tested in SUD-related experiments. Conceivably, the surface geometry of multiple antigen-displaying nanoparticles can be fine-tuned allowing for improved immunogenicity across multiple drugs of abuse. Overall, the clinical data indicates that SUD vaccines may be effective in reducing relapse in the subset of patients that are highly motivated to quit but are less useful in promoting abstinence in active drug users, as these subjects may increase their drug intake to saturate the antibody response [106]. Although nanoparticle delivery systems may improve the immunogenicity and pharmacokinetic efficacy of SUD vaccines, SUD vaccines will likely need to be combined with standard medication-assisted therapy to achieve optimal clinical outcomes.
Nucleic Acids
Remarkable progress has been made in the past few years with FDA approvals of antisense drugs targeting messenger RNA for disease treatment [116]. However, the delivery of nucleic acid-based therapeutics to the brain remains a significant challenge in neuroscience research. In SUD-related preclinical studies, investigators have successfully utilized nanoparticle delivery systems to manipulate addiction-related gene targets (Table 1). For example, using gold nanorod-siRNA complexes, gene expression of dopamine- and cAMP-regulated neuronal phosphoprotein (DARPP-32), an important target involved in drug-induced neuroplasticity, was effectively silenced in dopaminergic cultured neurons without signs of cytotoxicity [117]. The gold nanorod-siRNA complexes also permeated an in vitro BBB model to a greater degree than free (naked) siRNA. In animal studies, gold nanorod-DARPP-32 siRNA complexes caused sustained knockdown of DARPP-32 and reduced opioid withdrawal symptoms when injected into the periaqueductal gray area [118]. Using gold nanorod-siRNA complexes, long-term gene silencing of DARP-32 (14 days) has also been reported in the rat hippocampus [119]. While more research is needed to explore the potential of nanoparticle-mediated siRNA delivery in addiction models, promising results have been reported in animal models of traumatic brain injury [120], Alzheimer’s Disease [121, 122], and Huntington’s disease [123] using siRNA-loaded nanoparticles.
Because drugs of abuse alter a multitude of gene networks in the brain’s reward system, treatment strategies that have the ability to counteract these numerous adaptations are needed. Emerging evidence indicates that microRNA (miR)-based approaches are ideal for reversing or normalizing the extensive maladaptive neuroplasticity caused by repeated drug use [124]. For example, miR-212 levels are significantly altered in the striatum of rats with a history of cocaine use, and viral-mediated manipulation of this and other miRs in the brain decreased cocaine self-administration [125,126,127]. In humans, several other miRs are also altered in the brain following chronic drug use [128, 129], an indication that miRs are potentially important targets for clinical intervention.
microRNAs can be manipulated using anti-miRs, a single-stranded oligonucleotide with a complementary sequence to mature miRNA that binds to and inhibits the targeted miR, or by miR mimics that act as a replacement strategy to increase miR functional activity [130]. From a therapeutic standpoint, however, delivery of naked miR mimics or anti-miRs is not a viable option due to their short half-life under physiological conditions and their inability to penetrate the blood-brain barrier [131]. Chemical modifications to anti-miRs, such as locked nucleic acids (LNA) or peptide nucleic acids (PNA) have improved the stability of anti-miRs and miR mimics in in vivo applications [132], but even with these modifications, miR-based therapeutics have a limited ability to enter the brain. Encapsulating anti-miRs and miR mimics into nanoparticles is an alternative approach that addresses the shortcomings of miR-based therapeutics. For example, when injected systemically, rabies virus glycoprotein (RVG)-labeled nanoparticles were shown to effectively delivery miR-124a oligomers to the mouse brain [133]. Using Neuromag® anti-miR-134 nanocomplex, expression of miR-134 was reduced by 50% in the rat striatum 7 days post-intracerebroventricular injection [134]. Although these initial proof of concept studies are encouraging, nanoparticle-mediated brain delivery of anti-miRs and miR mimics has been primarily confined to brain cancer [135,136,137] and stroke studies [138]. Going forward, researchers are encouraged to test the effectiveness of nanoparticle-mediated delivery of siRNAs and microRNAs in sophisticated SUD models.
Peptides and Proteins
With low metabolic stability and a diminished ability to cross the blood-brain barrier, peptide and protein-based therapeutics for SUD have had limited clinical applications. In preclinical studies, nanoparticle delivery systems have been shown to address some of these pharmacokinetic liabilities (Table 1). For example, the endogenous opioid peptide leucine-enkephalin (LENK) plays an important role in SUD and pain processing but has a short half-life under physiological conditions [139]. By encapsulating LENK in nanoparticles, Godfrey and colleagues demonstrated that LENK entered the brain to a greater degree than the free form of LENK and produced tolerance-free analgesia in multiple pain assays [140]. Other studies have also shown that LENK-loaded nanoparticles increased brain uptake and antinociceptive effects following intranasal and systemic administration [141, 142]. Improved brain delivery of oxytocin and substance P have also been achieved following nanoparticle encapsulation, but these formulations have yet to be tested in SUD models [143, 144].
Similar to peptides, proteins, such as, brain-derived neurotropic factor (BDNF) and glial cell line-derived neurotrophic factor (GDNF) are potential therapeutic agents for the treatment for SUD [145]. By binding to magnetic nanoparticles, BDNF was shown to cross an in vitro model of the blood-brain barrier to a greater degree than free BDNF and increase dendritic spine density [146]. In other studies, GDNF-conjugated nanoparticles, when injected into the rat striatum, reduced acquisition of cocaine self-administration, but did not alter other behaviors, such as water self-administration [147]. Taken together, these findings indicate that nanoparticles represent a safe and feasible strategy for more efficient brain delivery of peptides and proteins.
Gene editing technologies
With the development of CRISPR-Cas9 systems, there has been a growing interest in using gene-editing techniques to study the underlying mechanisms of SUD. However, due to the large size of Cas9 ribonucleoprotein and the low stability of single guide RNAs (sgRNA), protecting these molecules from degradation during delivery has been a challenge [148]. Although truncated Cas9 ribonucleoproteins have been developed (e.g., Staphylococcus aureus Cas9, saCas9) [149], packaging the genetic material of Cas9, sgRNAs, and reporters into a single virus remains problematic [150]. Furthermore, viral-mediated constitutive expression of saCas9 and sgRNA in neuronal cells may result in unintended consequences [151]. To address these issues, researchers recently demonstrated that CRISPR-Gold (Cas9 packaged into gold nanoparticles) was able to safely edit genes in neurons, astrocytes, and microglia when injected into the mouse brain [152]. In the same report, CRISPR-Gold was successfully used to edit the metabotropic glutamate receptor 5 (mGluR5) gene in the mouse striatum and improve behavioral symptoms in a mouse model of amyotrophic lateral sclerosis. Tissue-specific gene editing has also been demonstrated following systemic administration of nanoparticle-encapsulated CRISPR-Cas9 [153], but further work is needed to determine if these Cas9- and sgRNA-bound nanoparticles are also able to cross the blood-brain barrier. From a therapeutic standpoint, modulation of gene expression levels, rather than gene knockout, is likely a more attractive treatment approach for SUD. In a technique called CRISPR activation and interference (CRISPRa and CRISPRi), a catalytically inactive Cas9 is fused to a transcription activator or repressor domain, and when combined with sgRNAs, this method allows for gene-specific activation or repression [154]. Though viral-mediated expression of CRISPRa/i has been demonstrated in the brain following an intracranial injection [155, 156], future studies are needed to determine if nanoparticle-mediated delivery of CRISPRa/i into the brain is an achievable approach in animal models of SUD.
Outlook of nanoparticle-based treatments for SUD
With the use of nanotechnology, brain delivery of many small molecules, biologics, and nucleic acids-based treatments is now possible. By encapsulating poorly water-soluble drugs and protecting nucleic acids and proteins from enzymatic degradation, nanoparticles ensure that the payload enters the brain and remains functional upon delivery. With surface modifications, nanocarriers can reduce the toxicity of treatments by targeting disease-associated brain cells while reducing exposure to healthy tissues [157]. The controlled release kinetics of nanoparticles formulations, combined with their capacity to delivery diverse therapeutics, may also reduce the total number of doses needed, potentially improving patient compliance and clinical outcomes. Despite these benefits, few SUD researchers have tested nanocarrier systems in sophisticated preclinical animal models of SUD. Access to nanoparticle formulations is likely one factor that has restricted such studies. While viral vector core facilities and vendors are widely available and utilized by neuroscience and SUD researchers, nanoparticle core facilities are less abundant. As a result, SUD researchers may not fully appreciate the capabilities of nanocarrier systems as an alternative approach to viral vectors. Thus, further collaborations between nanomedicine and SUD investigators are necessary to unlock the therapeutic potential of nanoparticle products for SUD.
Although a tremendous number of advancements in nanocarrier systems have been made in recent years, many unanswered questions remain regarding their potential clinical utility for SUD. For example, what class of nanoparticles is the best for brain delivery in SUD models? To date, most SUD-related studies administered nanoparticles directly into the brain or tested the nanoparticles in an in vitro blood-brain barrier model, which limits our understanding of its translatable potential. In other brain disease models, multiple classes of nanoparticles have been found to enter the brain following a systemic injection [158,159,160,161]. However, to our knowledge, there have been few head-to-head comparisons of brain delivery between the different classes and/or formulations of nanoparticles. Secondly, what is the best route of delivery? In preclinical studies, intranasal delivery of drug-bound nanoparticles showed superior pharmacokinetic qualities and CNS bioavailability when directly compared to intravenous delivery [162]. Thus, nose-to-brain delivery of nanoparticles may be a preferred approach for future SUD-related studies.
Finally, what surface modifications are likely to increase brain uptake and/or cell type-specific delivery? Thus far, the majority of studies have focused on disrupting the blood-brain barrier to improve nanotherapeutic delivery. For example, as a strategy to reduce brain efflux of therapeutic agents, Gomes and colleagues demonstrated that nanoparticles containing siRNAs for P-glycoprotein (P-gp) efflux transporters increased drug permeability of an in vitro blood-brain barrier model [163]. In preclinical studies, other researchers have utilized ultrasound to disrupt the blood-brain barrier, allowing brain region-specific uptake of nanoparticle-bound treatments [164, 165]. Nanoparticles containing ligands (e.g., transferrin, insulin, leptin, low-density lipoprotein) that bind to receptors on the circulation side of the blood-brain barrier is another approach that has been shown to facilitate transport across the blood-brain barrier via receptor-mediated transcytosis [166]. For cell-type-specific targeting, Tat and RVG-bound nanoparticles have been shown to facilitate uptake in neurons, while quantum dot formulations have been found to selectively target microglia in preclinical experiments [167,168,169]. Last, drug-induced changes in the brain’s microenvironment is an important factor to consider when designing nanoparticles for SUD treatment. For example, blood-brain barrier permeability and integrity may differ depending on the drug(s) abused and the duration of drug use [170], generating additional opportunities or barriers for nanomedicine products.
To move the field forward, more testing and validation is needed using clinically relevant routes of administration (e.g., intravenous, intramuscular, intranasal, intrathecal) in sophisticated SUD models (e.g., operant self-administration, reinstatement, behavioral economic procedures). Additionally, SUD researchers should determine what surface modifications to nanoparticles may increase cell type and/or tissue-specific uptake. Such an approach has the potential to limit side effects following systemic administration. As sustained release nanoformulations are a proven strategy to increase compliance and efficacy in SUD patients, researchers should also identify other small molecules-based therapies that may benefit from nanoparticle delivery systems. Finally, SUD researchers are encouraged to closely examine what nanoparticle delivery strategies have had success in other neurological models and investigate whether similar formulations have potential usefulness in SUD. Continued efforts to address these questions may reveal promising nanotherapeutic avenues for SUD.
References
Daley DC. Family and social aspects of substance use disorders and treatment. J Food Drug Anal. 2013;21:S73–6.
Florence C, Luo F, Rice K. The economic burden of opioid use disorder and fatal opioid overdose in the United States, 2017. Drug Alcohol Depend. 2021;218:108350.
Douaihy AB, Kelly TM, Sullivan C. Medications for substance use disorders. Soc Work Public Health. 2013;28:264–78.
Sartor GC. Epigenetic pharmacotherapy for substance use disorder. Biochem Pharm. 2019;168:269–74.
Chiamulera C, Padovani L, Corsi M. Drug discovery for the treatment of substance use disorders: novel targets, repurposing, and the need for new paradigms. Curr Opin Pharm. 2017;35:120–4.
van Gerven J, Cohen A. Vanishing clinical psychopharmacology. Br J Clin Pharm. 2011;72:1–5.
Pardridge WM. The blood-brain barrier: bottleneck in brain drug development. NeuroRx. 2005;2:3–14.
Salery M, Trifilieff P, Caboche J, Vanhoutte P. From Signaling Molecules to Circuits and Behaviors: Cell-Type-Specific Adaptations to Psychostimulant Exposure in the Striatum. Biol Psychiatry. 2020;87:944–53.
Nectow AR, Nestler EJ. Viral tools for neuroscience. Nat Rev Neurosci. 2020;21:669–81.
Kimura S, Harashima H. Current Status and Challenges Associated with CNS-Targeted Gene Delivery across the BBB. Pharmaceutics. 2020;12:E1216.
Ross KA, Brenza TM, Binnebose AM, Phanse Y, Kanthasamy AG, Gendelman HE, et al. Nano-enabled delivery of diverse payloads across complex biological barriers. J Control Release. 2015;219:548–59.
Anselmo AC, Mitragotri S. Nanoparticles in the clinic: An update. Bioeng Transl Med. 2019;4:e10143.
Koshimizu Y, Isa K, Kobayashi K, Isa T. Double viral vector technology for selective manipulation of neural pathways with higher level of efficiency and safety. Gene Ther. 2021;28:339–50.
Segel M, Lash B, Song J, Ladha A, Liu CC, Jin X, et al. Mammalian retrovirus-like protein PEG10 packages its own mRNA and can be pseudotyped for mRNA delivery. Science. 2021;373:882–9.
Kong Q, Li Y, Yue J, Wu X, Xu M. Reducing alcohol and/or cocaine-induced reward and toxicity via an epidermal stem cell-based gene delivery platform. Mol Psychiatry. 2021;26:5266–76.
Wu S-Y, Sanchez CS, Samiotaki G, Buch A, Ferrera VP, Konofagou EE. Characterizing Focused-Ultrasound Mediated Drug Delivery to the Heterogeneous Primate Brain In Vivo with Acoustic Monitoring. Sci Rep. 2016;6:37094.
Meng Y, Hynynen K, Lipsman N. Applications of focused ultrasound in the brain: from thermoablation to drug delivery. Nat Rev Neurol. 2021;17:7–22.
Terstappen GC, Meyer AH, Bell RD, Zhang W. Strategies for delivering therapeutics across the blood-brain barrier. Nat Rev Drug Disco. 2021;20:362–83.
Dong X. Current Strategies for Brain Drug Delivery. Theranostics. 2018;8:1481–93.
Pardridge WM. Blood-brain barrier delivery of protein and non-viral gene therapeutics with molecular Trojan horses. J Control Release. 2007;122:345–8.
Gomes MJ, Fernandes C, Martins S, Borges F, Sarmento B. Tailoring Lipid and Polymeric Nanoparticles as siRNA Carriers towards the Blood-Brain Barrier – from Targeting to Safe Administration. J Neuroimmune Pharm. 2017;12:107–19.
Fonseca C, Simões S, Gaspar R. Paclitaxel-loaded PLGA nanoparticles: preparation, physicochemical characterization and in vitro anti-tumoral activity. J Controlled Release. 2002;83:273–86.
Budhian A, Siegel SJ, Winey KI. Controlling the in vitro release profiles for a system of haloperidol-loaded PLGA nanoparticles. Int J Pharmaceutics. 2008;346:151–9.
Iwasaki Y, Maie H, Akiyoshi K. Cell-Specific Delivery of Polymeric Nanoparticles to Carbohydrate-Tagging Cells. Biomacromolecules. 2007;8:3162–8.
Gothwal A, Kumar H, Nakhate KT, Ajazuddin, Dutta A, Borah A, et al. Lactoferrin Coupled Lower Generation PAMAM Dendrimers for Brain Targeted Delivery of Memantine in Aluminum-Chloride-Induced Alzheimer’s Disease in Mice. Bioconjugate Chem. 2019;30:2573–83.
Jose S, Sowmya S, Cinu TA, Aleykutty NA, Thomas S, Souto EB. Surface modified PLGA nanoparticles for brain targeting of Bacoside-A. Eur J Pharm Sci. 2014;63:29–35.
Song E, Gaudin A, King AR, Seo Y-E, Suh H-W, Deng Y, et al. Surface chemistry governs cellular tropism of nanoparticles in the brain. Nat Commun. 2017;8:15322.
Fazil M, Md S, Haque S, Kumar M, Baboota S, Sahni JK, et al. Development and evaluation of rivastigmine loaded chitosan nanoparticles for brain targeting. Eur J Pharm Sci. 2012;47:6–15.
Kim I-D, Shin J-H, Kim S-W, Choi S, Ahn J, Han P-L, et al. Intranasal Delivery of HMGB1 siRNA Confers Target Gene Knockdown and Robust Neuroprotection in the Postischemic Brain. Mol Ther. 2012;20:829–39.
Seju U, Kumar A, Sawant KK. Development and evaluation of olanzapine-loaded PLGA nanoparticles for nose-to-brain delivery: in vitro and in vivo studies. Acta Biomaterialia. 2011;7:4169–76.
Kulkarni SA, Feng S-S. Effects of surface modification on delivery efficiency of biodegradable nanoparticles across the blood-brain barrier. Nanomed (Lond). 2011;6:377–94.
Hu K, Li J, Shen Y, Lu W, Gao X, Zhang Q, et al. Lactoferrin-conjugated PEG-PLA nanoparticles with improved brain delivery: in vitro and in vivo evaluations. J Controlled Release. 2009;134:55–61.
Saucier-Sawyer JK, Deng Y, Seo Y-E, Cheng CJ, Zhang J, Quijano E, et al. Systemic delivery of blood–brain barrier-targeted polymeric nanoparticles enhances delivery to brain tissue. J Drug Target. 2015;23:736–49.
Zhang C, Wan X, Zheng X, Shao X, Liu Q, Zhang Q, et al. Dual-functional nanoparticles targeting amyloid plaques in the brains of Alzheimer’s disease mice. Biomaterials. 2014;35:456–65.
Sánchez-López E, Ettcheto M, Egea MA, Espina M, Cano A, Calpena AC, et al. Memantine loaded PLGA PEGylated nanoparticles for Alzheimer’s disease: in vitro and in vivo characterization. J Nanobiotechnology. 2018;16:32.
Rao KS, Reddy MK, Horning JL, Labhasetwar V. TAT-conjugated nanoparticles for the CNS delivery of anti-HIV drugs. Biomaterials. 2008;29:4429–38.
Geldenhuys W, Mbimba T, Bui T, Harrison K, Sutariya V. Brain-targeted delivery of paclitaxel using glutathione-coated nanoparticles for brain cancers. J Drug Target. 2011;19:837–45.
Tosi G, Costantino L, Rivasi F, Ruozi B, Leo E, Vergoni AV, et al. Targeting the central nervous system: in vivo experiments with peptide-derivatized nanoparticles loaded with Loperamide and Rhodamine-123. J Control Release. 2007;122:1–9.
Vergoni AV, Tosi G, Tacchi R, Vandelli MA, Bertolini A, Costantino L. Nanoparticles as drug delivery agents specific for CNS: in vivo biodistribution. Nanomedicine. 2009;5:369–77.
Costantino L, Boraschi D. Is there a clinical future for polymeric nanoparticles as brain-targeting drug delivery agents? Drug Disco Today. 2012;17:367–78.
Dos Santos Rodrigues B, Oue H, Banerjee A, Kanekiyo T, Singh J. Dual functionalized liposome-mediated gene delivery across triple co-culture blood brain barrier model and specific in vivo neuronal transfection. J Control Release. 2018;286:264–78.
Ouyang C, Choice E, Holland J, Meloche M, Madden TD. Liposomal cyclosporine. Characterization of drug incorporation and interbilayer exchange. Transplantation. 1995;60:999–1006.
Chatin B, Mével M, Devallière J, Dallet L, Haudebourg T, Peuziat P, et al. Liposome-based Formulation for Intracellular Delivery of Functional Proteins. Mol Ther - Nucleic Acids. 2015;4:e244.
Kim JH, Shin DH, Kim J-S. Preparation, characterization, and pharmacokinetics of liposomal docetaxel for oral administration. Arch Pharm Res. 2018;41:765–75.
Yang Z-Z, Li J-Q, Wang Z-Z, Dong D-W, Qi X-R. Tumor-targeting dual peptides-modified cationic liposomes for delivery of siRNA and docetaxel to gliomas. Biomaterials. 2014;35:5226–39.
Hu Y, Gaillard PJ, Rip J, de Lange ECM, Hammarlund-Udenaes M. In Vivo Quantitative Understanding of PEGylated Liposome’s Influence on Brain Delivery of Diphenhydramine. Mol Pharmaceutics. 2018;15:5493–5500.
Gabizon A, Isacson R, Libson E, Kaufman B, Uziely B, Catane R, et al. Clinical Studies of Liposome-Encapsulated Doxorubicin. Acta Oncologica. 1994;33:779–86.
Zheng X, Shao X, Zhang C, Tan Y, Liu Q, Wan X, et al. Intranasal H102 Peptide-Loaded Liposomes for Brain Delivery to Treat Alzheimer’s Disease. Pharm Res. 2015;32:3837–49.
Kuznetsova NR, Vodovozova EL. Differential binding of plasma proteins by liposomes loaded with lipophilic prodrugs of methotrexate and melphalan in the bilayer. Biochem Mosc. 2014;79:797–804.
Costa PM, Cardoso AL, Mendonça LS, Serani A, Custódia C, Conceição M, et al. Tumor-targeted Chlorotoxin-coupled Nanoparticles for Nucleic Acid Delivery to Glioblastoma Cells: A Promising System for Glioblastoma Treatment. Mol Ther - Nucleic Acids. 2013;2:e100.
Jenning V, Thünemann AF, Gohla SH. Characterization of a novel solid lipid nanoparticle carrier system based on binary mixtures of liquid and solid lipids. Int J Pharmaceutics. 2000;199:167–77.
Cavalli R, Caputo O, Gasco MR. Solid lipospheres of doxorubicin and idarubicin. Int J Pharmaceutics. 1993;89:R9–12.
Singh I, Swami R, Pooja D, Jeengar MK, Khan W, Sistla R. Lactoferrin bioconjugated solid lipid nanoparticles: a new drug delivery system for potential brain targeting. J Drug Target. 2016;24:212–23.
Garud A, Singh D, Garud N. Solid Lipid Nanoparticles (SLN): Method, Characterization and Applications. Int Curr Pharm J. 2012;1:384–93.
Agarwal A, Majumder S, Agrawal H, Majumdar S, P. Agrawal G. Cationized Albumin Conjugated Solid Lipid Nanoparticles as Vectors for Brain Delivery of an Anti-Cancer Drug. Curr Nanosci. 2011;7:71–80.
Müller RH, Radtke M, Wissing SA. Nanostructured lipid matrices for improved microencapsulation of drugs. Int J Pharmaceutics. 2002;242:121–8.
Prades R, Guerrero S, Araya E, Molina C, Salas E, Zurita E, et al. Delivery of gold nanoparticles to the brain by conjugation with a peptide that recognizes the transferrin receptor. Biomaterials. 2012;33:7194–205.
Tkachenko AG, Xie H, Coleman D, Glomm W, Ryan J, Anderson MF, et al. Multifunctional gold nanoparticle-peptide complexes for nuclear targeting. J Am Chem Soc. 2003;125:4700–1.
Duncan B, Kim C, Rotello VM. Gold nanoparticle platforms as drug and biomacromolecule delivery systems. J Controlled Release. 2010;148:122–7.
Wu R, Peng H, Zhu J-J, Jiang L-P, Liu J. Attaching DNA to Gold Nanoparticles With a Protein Corona. Front Chem. 2020;8:121.
Saha B, Bhattacharya J, Mukherjee A, Ghosh A, Santra C, Dasgupta AK, et al. In Vitro Structural and Functional Evaluation of Gold Nanoparticles Conjugated Antibiotics. Nanoscale Res Lett. 2007;2:614.
Schäffler M, Sousa F, Wenk A, Sitia L, Hirn S, Schleh C, et al. Blood protein coating of gold nanoparticles as potential tool for organ targeting. Biomaterials. 2014;35:3455–66.
Cheng Y, Dai Q, Morshed RA, Fan X, Wegscheid ML, Wainwright DA, et al. Blood-brain barrier permeable gold nanoparticles: an efficient delivery platform for enhanced malignant glioma therapy and imaging. Small. 2014;10:5137–50.
Sela H, Cohen H, Elia P, Zach R, Karpas Z, Zeiri Y. Spontaneous penetration of gold nanoparticles through the blood brain barrier (BBB). J Nanobiotechnol. 2015;13:71.
Schaeublin NM, Braydich-Stolle LK, Schrand AM, Miller JM, Hutchison J, Schlager JJ, et al. Surface charge of gold nanoparticles mediates mechanism of toxicity. Nanoscale. 2011;3:410.
Xing X, Ma W, Zhao X, Wang J, Yao L, Jiang X, et al. Interaction between Surface Charge-Modified Gold Nanoparticles and Phospholipid Membranes. Langmuir. 2018;34:12583–9.
Smith K, Hopp M, Mundin G, Bond S, Bailey P, Woodward J, et al. Low absolute bioavailability of oral naloxone in healthy subjects. Int J Clin Pharm Ther. 2012;50:360–7.
Rzasa Lynn R, Galinkin JL. Naloxone dosage for opioid reversal: current evidence and clinical implications. Ther Adv Drug Saf. 2018;9:63–88.
Madison CA, Arora M, Kumar MNVR, Eitan S. Novel Oral Nanoparticle Formulation of Sustained Release Naloxone with Mild Withdrawal Symptoms in Mice. ACS Chem Neurosci. 2020;11:1955–64.
Lewter LA, Johnson MC, Treat AC, Kassick AJ, Averick S, Kolber BJ. Slow-sustained delivery of naloxone reduces typical naloxone-induced precipitated opioid withdrawal effects in male morphine-dependent mice. J Neurosci Res. 2020;100:339–52.
Hasan N, Imran M, Kesharwani P, Khanna K, Karwasra R, Sharma N, et al. Intranasal delivery of Naloxone-loaded solid lipid nanoparticles as a promising simple and non-invasive approach for the management of opioid overdose. Int J Pharm. 2021;599:120428.
Imam MZ, Kuo A, Smith MT. Countering opioid-induced respiratory depression by non-opioids that are respiratory stimulants. F1000Res. 2020;9:F1000 Faculty Rev-91.
O’Malley SS, Krishnan-Sarin S, Farren C, Sinha R, Kreek MJ. Naltrexone decreases craving and alcohol self-administration in alcohol-dependent subjects and activates the hypothalamo-pituitary-adrenocortical axis. Psychopharmacol (Berl). 2002;160:19–29.
Sudakin D. Naltrexone: Not Just for Opioids Anymore. J Med Toxicol. 2016;12:71.
Goonoo N, Bhaw-Luximon A, Ujoodha R, Jhugroo A, Hulse GK, Jhurry D. Naltrexone: a review of existing sustained drug delivery systems and emerging nano-based systems. J Control Release. 2014;183:154–66.
de Weert-van Oene GH, Burger H, Grobbee DE, Schrijvers AJP. Identification of patients at high risk of noncompliance in substance dependence treatment. Eur Addict Res. 2007;13:74–80.
Abrahams RA, Ronel SH. Biocompatible implants for the sustained zero-order release of narcotic antagonists. J Biomed Mater Res. 1975;9:355–66.
Chiang CN, Hollister LE, Kishimoto A, Barnett G. Kinetics of a naltrexone sustained-release preparation. Clin Pharm Ther. 1984;36:704–8.
Krupitsky EM, Blokhina EA. Long-acting depot formulations of naltrexone for heroin dependence: a review. Curr Opin Psychiatry. 2010;23:210–4.
Comer SD, Sullivan MA, Hulse GK. Sustained-release naltrexone: novel treatment for opioid dependence. Expert Opin Investig Drugs. 2007;16:1285–94.
Bartus RT, Emerich DF, Hotz J, Blaustein M, Dean RL, Perdomo B, et al. Vivitrex, an injectable, extended-release formulation of naltrexone, provides pharmacokinetic and pharmacodynamic evidence of efficacy for 1 month in rats. Neuropsychopharmacology 2003;28:1973–82.
Garbutt JC, Kranzler HR, O’Malley SS, Gastfriend DR, Pettinati HM, Silverman BL, et al. Efficacy and tolerability of long-acting injectable naltrexone for alcohol dependence: a randomized controlled trial. JAMA. 2005;293:1617–25.
Kranzler HR, Wesson DR, Billot L, DrugAbuse Sciences Naltrexone Depot Study Group. Naltrexone depot for treatment of alcohol dependence: a multicenter, randomized, placebo-controlled clinical trial. Alcohol Clin Exp Res. 2004;28:1051–9.
Kunøe N, Lobmaier P, Vederhus JK, Hjerkinn B, Hegstad S, Gossop M, et al. Naltrexone implants after in-patient treatment for opioid dependence: randomised controlled trial. Br J Psychiatry. 2009;194:541–6.
Olsen L, Christophersen AS, Frogopsahl G, Waal H, Mørland J. Plasma concentrations during naltrexone implant treatment of opiate-dependent patients. Br J Clin Pharm. 2004;58:219–22.
Tiihonen J, Krupitsky E, Verbitskaya E, Blokhina E, Mamontova O, Föhr J, et al. Naltrexone implant for the treatment of polydrug dependence: a randomized controlled trial. Am J Psychiatry. 2012;169:531–6.
Akala EO, Wiriyacoonkasem P, Pan G. Studies on in vitro availability, degradation, and thermal properties of naltrexone-loaded biodegradable microspheres. Drug Dev Ind Pharm. 2011;37:673–84.
Pagar KP, Vavia PR. Naltrexone-loaded poly[La-(Glc-Leu)] polymeric microspheres for the treatment of alcohol dependence: in vitro characterization and in vivo biocompatibility assessment. Pharm Dev Technol.2014;19:385–94.
Asadi H, Rostamizadeh K, Salari D, Hamidi M. Preparation and characterization of tri-block poly(lactide)-poly(ethylene glycol)-poly(lactide) nanogels for controlled release of naltrexone. Int J Pharm. 2011;416:356–64.
Masoumi S, Esmaeili A. New method of creating hybrid of buprenorphine loaded rifampin/polyethylene glycol/alginate nanoparticles. Int J Biol Macromol. 2020;159:204–12.
Hagelberg NM, Fihlman M, Hemmilä T, Backman JT, Laitila J, Neuvonen PJ, et al. Rifampicin decreases exposure to sublingual buprenorphine in healthy subjects. Pharm Res Perspect. 2016;4:e00271.
Wang J-J, Liu K-S, Sung KC, Tsai C-Y, Fang J-Y. Lipid nanoparticles with different oil/fatty ester ratios as carriers of buprenorphine and its prodrugs for injection. Eur J Pharm Sci. 2009;38:138–46.
Xu A, Kosten TR. Current status of immunotherapies for addiction. Ann NY Acad Sci. 2021;1489:3–16.
Bremer PT, Janda KD. Conjugate Vaccine Immunotherapy for Substance Use Disorder. Pharm Rev. 2017;69:298–315.
Pentel PR, LeSage MG. New directions in nicotine vaccine design and use. Adv Pharm. 2014;69:553–80.
Zhao Z, Hu Y, Harmon T, Pentel P, Ehrich M, Zhang C. Rationalization of a nanoparticle-based nicotine nanovaccine as an effective next-generation nicotine vaccine: A focus on hapten localization. Biomaterials 2017;138:46–56.
Zhao Z, Hu Y, Hoerle R, Devine M, Raleigh M, Pentel P, et al. A nanoparticle-based nicotine vaccine and the influence of particle size on its immunogenicity and efficacy. Nanomedicine 2017;13:443–54.
Zhao Z, Harris B, Hu Y, Harmon T, Pentel PR, Ehrich M, et al. Rational incorporation of molecular adjuvants into a hybrid nanoparticle-based nicotine vaccine for immunotherapy against nicotine addiction. Biomaterials 2018;155:165–75.
Zhao Z, Hu Y, Harmon T, Pentel P, Ehrich M, Zhang C. Effect of Adjuvant Release Rate on the Immunogenicity of Nanoparticle-Based Vaccines: A Case Study with a Nanoparticle-Based Nicotine Vaccine. Mol Pharm. 2019;16:2766–75.
Desai RI, Bergman J. Effects of the Nanoparticle-Based Vaccine, SEL-068, on Nicotine Discrimination in Squirrel Monkeys. Neuropsychopharmacology. 2015;40:2207–16.
Wee S, Hicks MJ, De BP, Rosenberg JB, Moreno AY, Kaminsky SM, et al. Novel cocaine vaccine linked to a disrupted adenovirus gene transfer vector blocks cocaine psychostimulant and reinforcing effects. Neuropsychopharmacology. 2012;37:1083–91.
Kantak KM, Collins SL, Lipman EG, Bond J, Giovanoni K, Fox BS. Evaluation of anti-cocaine antibodies and a cocaine vaccine in a rat self-administration model. Psychopharmacol (Berl). 2000;148:251–62.
Kantak KM, Collins SL, Bond J, Fox BS. Time course of changes in cocaine self-administration behavior in rats during immunization with the cocaine vaccine IPC-1010. Psychopharmacol (Berl). 2001;153:334–40.
Lowell JA, Dikici E, Joshi PM, Landgraf R, Lemmon VP, Daunert S, et al. Vaccination against cocaine using a modifiable dendrimer nanoparticle platform. Vaccine. 2020;38:7989–97.
Kosten TR, Domingo CB, Shorter D, Orson F, Green C, Somoza E, et al. Vaccine for cocaine dependence: a randomized double-blind placebo-controlled efficacy trial. Drug Alcohol Depend. 2014;140:42–47.
Truong TT, Kosten TR. Current status of vaccines for substance use disorders: A brief review of human studies. J Neurol Sci. 2021;434:120098.
Martell BA, Orson FM, Poling J, Mitchell E, Rossen RD, Gardner T, et al. Cocaine vaccine for the treatment of cocaine dependence in methadone-maintained patients: a randomized, double-blind, placebo-controlled efficacy trial. Arch Gen Psychiatry. 2009;66:1116–23.
Zhao Z, Powers K, Hu Y, Raleigh M, Pentel P, Zhang C. Engineering of a hybrid nanoparticle-based nicotine nanovaccine as a next-generation immunotherapeutic strategy against nicotine addiction: A focus on hapten density. Biomaterials. 2017;123:107–17.
Sahdev P, Ochyl LJ, Moon JJ. Biomaterials for nanoparticle vaccine delivery systems. Pharm Res. 2014;31:2563–82.
Moss HB, Chen CM, Yi H-Y. Early adolescent patterns of alcohol, cigarettes, and marijuana polysubstance use and young adult substance use outcomes in a nationally representative sample. Drug Alcohol Depend. 2014;136:51–62.
Hwang CS, Smith LC, Natori Y, Ellis B, Zhou B, Janda KD. Efficacious Vaccine against Heroin Contaminated with Fentanyl. ACS Chem Neurosci. 2018;9:1269–75.
Hwang CS, Smith LC, Natori Y, Ellis B, Zhou B, Janda KD. Improved Admixture Vaccine of Fentanyl and Heroin Hapten Immunoconjugates: Antinociceptive Evaluation of Fentanyl-Contaminated Heroin. ACS Omega. 2018;3:11537–43.
Natori Y, Hwang CS, Lin L, Smith LC, Zhou B, Janda KD. A chemically contiguous hapten approach for a heroin-fentanyl vaccine. Beilstein J Org Chem. 2019;15:1020–31.
Chiba S, Frey SJ, Halfmann PJ, Kuroda M, Maemura T, Yang JE, et al. Multivalent nanoparticle-based vaccines protect hamsters against SARS-CoV-2 after a single immunization. Commun Biol. 2021;4:597.
Ueda G, Antanasijevic A, Fallas JA, Sheffler W, Copps J, Ellis D, et al. Tailored design of protein nanoparticle scaffolds for multivalent presentation of viral glycoprotein antigens. Elife. 2020;9:e57659.
Akinc A, Maier MA, Manoharan M, Fitzgerald K, Jayaraman M, Barros S, et al. The Onpattro story and the clinical translation of nanomedicines containing nucleic acid-based drugs. Nat Nanotechnol. 2019;14:1084–7.
Bonoiu AC, Mahajan SD, Ding H, Roy I, Yong K-T, Kumar R, et al. Nanotechnology approach for drug addiction therapy: gene silencing using delivery of gold nanorod-siRNA nanoplex in dopaminergic neurons. Proc Natl Acad Sci USA. 2009;106:5546–50.
Ignatowski TA, Aalinkeel R, Reynolds JL, Nair BB, Sykes DE, Gleason CPK, et al. Nanotherapeutic approach for opiate addiction using DARPP-32 gene silencing in an animal model of opiate addiction. J Neuroimmune Pharm. 2015;10:136–52.
Bonoiu AC, Bergey EJ, Ding H, Hu R, Kumar R, Yong K-T, et al. Gold nanorod–siRNA induces efficient in vivo gene silencing in the rat hippocampus. Nanomed (Lond). 2011;6:617–30.
Kwon EJ, Skalak M, Lo Bu R, Bhatia SN. Neuron-Targeted Nanoparticle for siRNA Delivery to Traumatic Brain Injuries. ACS Nano. 2016;10:7926–33.
Zhang C, Gu Z, Shen L, Liu X, Lin H. In vivo Evaluation and Alzheimer’s Disease Treatment Outcome of siRNA Loaded Dual Targeting Drug Delivery System. Curr Pharm Biotechnol. 2019;20:56–62.
Wang P, Zheng X, Guo Q, Yang P, Pang X, Qian K, et al. Systemic delivery of BACE1 siRNA through neuron-targeted nanocomplexes for treatment of Alzheimer’s disease. J Control Release. 2018;279:220–33.
Sava V, Fihurka O, Khvorova A, Sanchez-Ramos J. Enriched chitosan nanoparticles loaded with siRNA are effective in lowering Huntington’s disease gene expression following intranasal administration. Nanomedicine. 2020;24:102119.
Doura MB, Unterwald EM. MicroRNAs Modulate Interactions between Stress and Risk for Cocaine Addiction. Front Cell Neurosci. 2016;10:125.
Sadakierska-Chudy A, Frankowska M, Miszkiel J, Wydra K, Jastrzębska J, Filip M. Prolonged Induction of miR-212/132 and REST Expression in Rat Striatum Following Cocaine Self-Administration. Mol Neurobiol. 2017;54:2241–54.
Im H-I, Hollander JA, Bali P, Kenny PJ. MeCP2 controls BDNF expression and cocaine intake through homeostatic interactions with microRNA-212. Nat Neurosci. 2010;13:1120–7.
Hollander JA, Im H-I, Amelio AL, Kocerha J, Bali P, Lu Q, et al. Striatal microRNA controls cocaine intake through CREB signalling. Nature. 2010;466:197–202.
Bali P, Kenny PJ. MicroRNAs and Drug Addiction. Front Genet. 2013;4:43.
Lewohl JM, Nunez YO, Dodd PR, Tiwari GR, Harris RA, Mayfield RD. Up-regulation of microRNAs in brain of human alcoholics. Alcohol Clin Exp Res. 2011;35:1928–37.
van Rooij E, Kauppinen S. Development of microRNA therapeutics is coming of age. EMBO Mol Med. 2014;6:851–64.
Lee SWL, Paoletti C, Campisi M, Osaki T, Adriani G, Kamm RD, et al. MicroRNA delivery through nanoparticles. J Control Release. 2019;313:80–95.
Lennox KA, Behlke MA. Chemical modification and design of anti-miRNA oligonucleotides. Gene Ther. 2011;18:1111–20.
Hwang DW, Son S, Jang J, Youn H, Lee S, Lee D, et al. A brain-targeted rabies virus glycoprotein-disulfide linked PEI nanocarrier for delivery of neurogenic microRNA. Biomaterials. 2011;32:4968–75.
Titze de Almeida SS, Horst CH, Soto-Sánchez C, Fernandez E, Titze de Almeida R. Delivery of miRNA-Targeted Oligonucleotides in the Rat Striatum by Magnetofection with Neuromag®. Molecules. 2018;23:E1825.
Sukumar UK, Bose RJC, Malhotra M, Babikir HA, Afjei R, Robinson E, et al. Intranasal delivery of targeted polyfunctional gold-iron oxide nanoparticles loaded with therapeutic microRNAs for combined theranostic multimodality imaging and presensitization of glioblastoma to temozolomide. Biomaterials. 2019;218:119342.
Seo Y-E, Suh H-W, Bahal R, Josowitz A, Zhang J, Song E, et al. Nanoparticle-mediated intratumoral inhibition of miR-21 for improved survival in glioblastoma. Biomaterials. 2019;201:87–98.
Costa PM, Cardoso AL, Custódia C, Cunha P, Pereira de Almeida L, Pedroso de Lima MC. MiRNA-21 silencing mediated by tumor-targeted nanoparticles combined with sunitinib: A new multimodal gene therapy approach for glioblastoma. J Control Release. 2015;207:31–39.
Hao R, Sun B, Yang L, Ma C, Li S. RVG29-modified microRNA-loaded nanoparticles improve ischemic brain injury by nasal delivery. Drug Deliv. 2020;27:772–81.
Marquez P, Baliram R, Gajawada N, Friedman TC, Lutfy K. Differential involvement of enkephalins in analgesic tolerance, locomotor sensitization, and conditioned place preference induced by morphine. Behav Neurosci. 2006;120:10–15.
Godfrey L, Iannitelli A, Garrett NL, Moger J, Imbert I, King T, et al. Nanoparticulate peptide delivery exclusively to the brain produces tolerance free analgesia. J Control Release. 2018;270:135–44.
Kumar M, Pandey RS, Patra KC, Jain SK, Soni ML, Dangi JS, et al. Evaluation of neuropeptide loaded trimethyl chitosan nanoparticles for nose to brain delivery. Int J Biol Macromol. 2013;61:189–95.
Feng J, Lepetre-Mouelhi S, Gautier A, Mura S, Cailleau C, Coudore F, et al. A new painkiller nanomedicine to bypass the blood-brain barrier and the use of morphine. Sci Adv. 2019;5:eaau5148.
Oppong-Damoah A, Zaman RU, D’Souza MJ, Murnane KS. Nanoparticle encapsulation increases the brain penetrance and duration of action of intranasal oxytocin. Horm Behav. 2019;108:20–29.
Li J, Du Y, Jiang Z, Tian Y, Qiu N, Wang Y, et al. Y1 receptor ligand-based nanomicelle as a novel nanoprobe for glioma-targeted imaging and therapy. Nanoscale 2018;10:5845–51.
Koskela M, Bäck S, Võikar V, Richie CT, Domanskyi A, Harvey BK, et al. Update of neurotrophic factors in neurobiology of addiction and future directions. Neurobiol Dis. 2017;97:189–200.
Pilakka-Kanthikeel S, Atluri VSR, Sagar V, Saxena SK, Nair M. Targeted brain derived neurotropic factors (BDNF) delivery across the blood-brain barrier for neuro-protection using magnetic nano carriers: an in-vitro study. PLoS One. 2013;8:e62241.
Green-Sadan T, Kuttner Y, Lublin-Tennenbaum T, Kinor N, Boguslavsky Y, Margel S, et al. Glial cell line-derived neurotrophic factor-conjugated nanoparticles suppress acquisition of cocaine self-administration in rats. Exp Neurol. 2005;194:97–105.
Nishiyama J. Genome editing in the mammalian brain using the CRISPR-Cas system. Neurosci Res. 2019;141:4–12.
Ran FA, Cong L, Yan WX, Scott DA, Gootenberg JS, Kriz AJ, et al. In vivo genome editing using Staphylococcus aureus Cas9. Nature. 2015;520:186–91.
Cota-Coronado A, Díaz-Martínez NF, Padilla-Camberos E, Díaz-Martínez NE. Editing the Central Nervous System Through CRISPR/Cas9 Systems. Front Mol Neurosci. 2019;12:110.
Charlesworth CT, Deshpande PS, Dever DP, Camarena J, Lemgart VT, Cromer MK, et al. Identification of preexisting adaptive immunity to Cas9 proteins in humans. Nat Med. 2019;25:249–54.
Lee B, Lee K, Panda S, Gonzales-Rojas R, Chong A, Bugay V, et al. Nanoparticle delivery of CRISPR into the brain rescues a mouse model of fragile X syndrome from exaggerated repetitive behaviours. Nat Biomed Eng. 2018;2:497–507.
Wei T, Cheng Q, Min Y-L, Olson EN, Siegwart DJ. Systemic nanoparticle delivery of CRISPR-Cas9 ribonucleoproteins for effective tissue specific genome editing. Nat Commun. 2020;11:3232.
Konermann S, Brigham MD, Trevino AE, Joung J, Abudayyeh OO, Barcena C, et al. Genome-scale transcriptional activation by an engineered CRISPR-Cas9 complex. Nature. 2015;517:583–8.
Kampmann M. CRISPR-based functional genomics for neurological disease. Nat Rev Neurol. 2020;16:465–80.
Colasante G, Qiu Y, Massimino L, Di Berardino C, Cornford JH, Snowball A, et al. In vivo CRISPRa decreases seizures and rescues cognitive deficits in a rodent model of epilepsy. Brain. 2020;143:891–905.
Farokhzad OC, Langer R. Impact of nanotechnology on drug delivery. ACS Nano. 2009;3:16–20.
Karatas H, Aktas Y, Gursoy-Ozdemir Y, Bodur E, Yemisci M, Caban S, et al. A nanomedicine transports a peptide caspase-3 inhibitor across the blood-brain barrier and provides neuroprotection. J Neurosci. 2009;29:13761–9.
Roney C, Kulkarni P, Arora V, Antich P, Bonte F, Wu A, et al. Targeted nanoparticles for drug delivery through the blood-brain barrier for Alzheimer’s disease. J Control Release. 2005;108:193–214.
Trapani A, De Giglio E, Cafagna D, Denora N, Agrimi G, Cassano T, et al. Characterization and evaluation of chitosan nanoparticles for dopamine brain delivery. Int J Pharm. 2011;419:296–307.
He H, Yao J, Zhang Y, Chen Y, Wang K, Lee RJ, et al. Solid lipid nanoparticles as a drug delivery system to across the blood-brain barrier. Biochem Biophys Res Commun. 2019;519:385–90.
Yadav S, Gattacceca F, Panicucci R, Amiji MM. Comparative Biodistribution and Pharmacokinetic Analysis of Cyclosporine-A in the Brain upon Intranasal or Intravenous Administration in an Oil-in-Water Nanoemulsion Formulation. Mol Pharm. 2015;12:1523–33.
Gomes MJ, Kennedy PJ, Martins S, Sarmento B. Delivery of siRNA silencing P-gp in peptide-functionalized nanoparticles causes efflux modulation at the blood-brain barrier. Nanomed (Lond). 2017;12:1385–99.
Aryal M, Vykhodtseva N, Zhang Y-Z, McDannold N. Multiple sessions of liposomal doxorubicin delivery via focused ultrasound mediated blood-brain barrier disruption: a safety study. J Control Release. 2015;204:60–69.
Nance E, Timbie K, Miller GW, Song J, Louttit C, Klibanov AL, et al. Non-invasive delivery of stealth, brain-penetrating nanoparticles across the blood-brain barrier using MRI-guided focused ultrasound. J Control Release. 2014;189:123–32.
Zhang F, Lin Y-A, Kannan S, Kannan RM. Targeting specific cells in the brain with nanomedicines for CNS therapies. J Control Release. 2016;240:212–26.
Chu DSH, Schellinger JG, Bocek MJ, Johnson RN, Pun SH. Optimization of Tet1 ligand density in HPMA-co-oligolysine copolymers for targeted neuronal gene delivery. Biomaterials. 2013;34:9632–7.
Alvarez-Erviti L, Seow Y, Yin H, Betts C, Lakhal S, Wood MJA. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat Biotechnol. 2011;29:341–5.
Minami SS, Sun B, Popat K, Kauppinen T, Pleiss M, Zhou Y, et al. Selective targeting of microglia by quantum dots. J Neuroinflammation. 2012;9:22.
Pimentel E, Sivalingam K, Doke M, Samikkannu T. Effects of Drugs of Abuse on the Blood-Brain Barrier: A Brief Overview. Front Neurosci. 2020;14:513.
Zhao Z, Hu Y, Harmon T, Pentel PR, Ehrich M, Zhang C. Hybrid nanoparticle-based nicotine nanovaccines: Boosting the immunological efficacy by conjugation of potent carrier proteins. Nanomedicine. 2018;14:1655–65.
Funding
This work was supported by the National Institute on Drug Abuse (U18DA052394) and The American Foundation for Pharmaceutical Education Gateway to Research Award.
Author information
Authors and Affiliations
Contributions
VK, RJM, RB, and GCS wrote and revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kasina, V., Mownn, R.J., Bahal, R. et al. Nanoparticle delivery systems for substance use disorder. Neuropsychopharmacol. 47, 1431–1439 (2022). https://doi.org/10.1038/s41386-022-01311-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-022-01311-7