Abstract
Early interventions to improve resilience require the identification of objective risk biomarkers for PTSD symptom development. Although altered hippocampal and amygdala volumes are consistently observed in PTSD, it remains currently unknown whether they represent a predisposing vulnerability factor for PTSD symptom development or an acquired consequence of trauma exposure and/or the disorder. We conducted a longitudinal, prospective study in 210 police recruits at high risk for trauma exposure (56 females(26.7%); mean[SD] age = 24.02[5.19]). Structural MRI scans and trauma-related symptom severity were assessed at pre-trauma baseline and at 16-month follow-up. Between assessments, police recruits were exposed to various potentially traumatic events during their police training. Police recruits reported a significant increase in police-related trauma exposure and stress-related symptoms between assessments. Smaller hippocampal left dentate gyrus (DG) volumes at baseline predicted increase in self-reported PTSD symptoms (B[SE] = −0.21[0.08], p = 0.011), stress symptoms (B[SE] = −0.16[0.07], p = 0.024) and negative affect (B[SE] = −0.21[0.07], p = 0.005) upon trauma exposure. Amount of police-related trauma exposure between assessments was positively associated with an increase in left basal amygdala nucleus volume (B[SE] = 0.11[0.05], p = 0.026). Taken together, smaller DG-volumes pre-trauma may represent a predisposing neurobiological vulnerability factor for development of trauma-related symptoms. On the other hand, amount of trauma exposure between assessments was positively associated with increased amygdala basal nucleus volume, suggesting acquired neural effects. These findings suggest that preventive interventions for PTSD aimed at improving resilience could be targeted at increasing DG-volume and potentially its functioning.
Similar content being viewed by others
Introduction
Posttraumatic stress disorder (PTSD) is associated with large individual and societal burden, including high mortality, decreased well-being, and psychiatric and somatic comorbidity [1]. As preventive interventions should be specifically targeted at individuals at increased PTSD risk, there is a great need to identify neurobiological vulnerability factors for PTSD. This may not only improve screening for at risk individuals with objective biomarkers, but may also provide new neurobiological and psychological targets for (preventive) interventions [2]. Given the unpredictable occurrence of traumatic events, identifying predisposing PTSD risk factors is challenging and requires large-scale longitudinal prospective studies in high-risk professions, such as police officers [3].
Core symptoms of PTSD include excessive fear of trauma reminders, memory intrusions, and reexperiencing the traumatic event, even in safe contexts [4]. Neurobiological models of PTSD have focused on the amygdala and hippocampus, given their respective roles in the fear response and its contextual modulation [2, 5]. Previous studies have consistently observed smaller hippocampal [6,7,8], and amygdala volumes [7, 9], although this latter finding is less consistent (e.g., see Bromis et al. [6]). However, a major outstanding question is whether these volumetric alterations pose a vulnerability or are a consequence of PTSD [2], or a combination of both. On the one hand, evidence exists that smaller hippocampal [10,11,12,13] and amygdala [9] volumes may represent a vulnerability factor for stress-related disorders. For example, reduced hippocampal volumes were observed in monozygotic twin-pairs, of which one had PTSD but the other was non-trauma-exposed [10]. On the other hand, both structures are susceptible to chronic stress effects [14, 15], suggesting acquired neurobiological alterations [7, 16]. Whereas hippocampal volume is reduced by elevated levels of glucocorticoids [15], severe stress induces amygdala sensitivity and initial hypertrophy [14], which may result in volume reductions in the long-term [7, 17]. However, these previous studies were conducted in relatively small military and civilian samples, thwarting the settlement of the vulnerability versus consequence debate. Moreover, mainly due to methodological limitations, these studies focused on the whole hippocampus and amygdala, while acknowledging that these regions consist of functionally and cytoarchitecturally distinct substructures, which may be differentially involved in PTSD pathophysiology.
Distressing memory intrusions of the original trauma are believed to be the driving factor in the etiology and maintenance of PTSD [18]. The dentate gyrus (DG) subfield of the hippocampus is essential for successful encoding and retrieval of distinct memory traces of similar experiences, disambiguating overlapping, perceptually similar sensory inputs (i.e., pattern separation). DG-dysfunction may therefore be at the root of dysfunctional memory processes in PTSD [19, 20]. Indeed, smaller DG-volumes were observed in PTSD patients compared to trauma-exposed [21, 22] and non-trauma-exposed controls [23]. Yet, other hippocampal subfields, such as the cornu ammonis (CA) 1 and 3 subfields, are also compromised in PTSD [23, 24]. The CA1 subfield is responsive to global contextual regularities across experiences [25], enabling for instance context-specific extinction memory retrieval [26] and the CA3 subfield is thought to aid in pattern completion given noisy inputs [20].
Regarding the amygdala, its basolateral (BLA) nucleus is involved in fear learning, whereas the centromedial nucleus is involved in fear expression, via efferent projections to the brainstem and hypothalamus [27]. In rodents, smaller BLA volumes were associated with greater fear conditioning and glucocorticoid stress reactivity [28]. In PTSD patients, smaller BLA and central amygdala subnuclei volumes were observed [17, 29], and related to increased re-experiencing symptoms [29]. In a recent large-scale study, PTSD patients exhibited greater cortical, central and medial subnuclei volumes, but smaller lateral and paralaminar amygdala subnuclei compared to trauma-exposed controls [30].
Disentangling which hippocampal and amygdala substructures form predisposing or acquired factors in PTSD development could enhance mechanistic insights in PTSD pathophysiology, as these substructures show clear functional heterogeneity. For example, the DG and CA3 are involved in pattern separation and completion, respectively. Further, linking substructure alterations with development of specific symptom clusters, as well as with different symptom trajectories [31], could provide new targets for interventions and primary preventions.
To disentangle predisposing from acquired alterations in hippocampal and amygdala substructure volumes, we conducted a large-scale longitudinal prospective study in 210 police recruits. We acquired structural MRI scans and symptom measures before and after recruits were exposed to various traumatic events during their services at the emergency aids. We expected to find smaller baseline DG-volume as vulnerability factor for development of trauma-related symptoms, especially intrusions. We further investigated whether other hippocampal (CA1 and CA3) and amygdala (lateral, medial, basal and central) substructure volumes at baseline are predictive of increased symptoms following trauma. We also hypothesized that higher levels of trauma exposure would be related to increased basolateral and central amygdala volumes post-trauma.
Materials and methods
Study design
We conducted a longitudinal, prospective study in Dutch police recruits, consisting of two assessments (see Fig. 1A for the study design). The baseline assessment took place while recruits were in the safe school environment at the police academy. The follow-up assessment took place on average 16 months later (mean [SD] = 484.69 [56.28] days, range: 349–679), after recruits were trained in the emergency aid services, during which they were exposed to potentially traumatic events. Both assessments consisted of clinical, behavioral, physiological and neuroimaging data collection (see [32] for details). This study was approved by the Independent Review Board Nijmegen, registered in the Netherlands Trial Registry (NTR6355), and conducted in accordance with the principles of the Declaration of Helsinki. An independent monitor assured study quality. Participants provided written informed consent before participation.
A Design of the police-in-action study. Trauma-related symptoms and a structural T1-weighted scan were acquired in police recruits at baseline and follow-up. Between assessments, participants served at emergency aids during 2 periods of 4 months. B Self-reported PTSD symptoms (PCL-5) at baseline and follow-up for each participant, showing high individual variability in symptom change (ΔPCL). Black horizontal lines represent the mean of each assessment. C Exposure to different police-related traumatic events (PLES total score) between baseline and follow-up. Self-reported perceived stress (PSS) and negative affect (VAS) increased significantly between baseline and follow-up. D Based on delta-PCL, three symptom trajectories were identified: symptom increase (n = 35), symptom decrease (n = 46) and no symptom change (n = 140). Shaded areas indicate standard error of the mean (SEM). PCL-5 PTSD checklist for DSM-5, VAS visual analog scale, PLES Police-life events scale, PSS perceived stress scale, Quest. intermediate questionnaire, n.s. not significant; *p < 0.05; **p < 0.001 (compared to the previous assessment).
Participants
In total, 713 police recruits were assessed for eligibility, of which 57 (7.99%) were excluded, 314 (44.04%) declined to participate, and 342 (47.97%) provided informed consent (Supplementary Fig. 1 for flowchart). Included participants (n = 342) did not differ significantly from non-participants (n = 371) on year of birth (U = 59813.00, p = 0.341), educational level (Χ2(2) = 1.26, p = 0.533) and gender (Χ2(1) = 3.00, p = 0.084). All participants were between 18 and 45 years of age and eligible for MRI. Exclusion criteria were any current psychiatric or neurological disorder; history of, or current, neurological or endocrinological treatment; current use of psychotropic medication; and current drug-or alcohol abuse. 340 participants completed the baseline assessment, of which 271 (79.71%) completed follow-up, 21 (6.18%) completed follow-up symptom assessments only, and 48 (14.12%) were lost to follow-up. Study attrition was not related to demographics, trauma history or baseline clinical characteristics (see Supplementary Table 1). Since we investigated PTSD onset, we selected police recruits who experienced their core traumatic event between assessments (n = 222), and excluded one recruit who scored above the clinical cut-off of PTSD at baseline (PCL sum > 33) [33]. Analyses of symptom change were conducted in these 221 participants. As structural MRI-scans were not acquired in four participants at both assessments, and seven participants were excluded after quality control (see Supplementary Methods for quality control procedure), we tested our main hypotheses regarding hippocampal and amygdala substructures in 210 recruits (56 females (26.7%); mean [SD] age = 24.02 [5.19]).
Study procedures
We acquired a structural T1-weighted MRI-scan and assessed symptom severity at both assessments. As pre-registered [32], change in self-reported PTSD symptom severity was our main outcome measure (PTSD Checklist for DSM-5; PCL-5 [33]). A change of ≥ 10 points on the PCL-5 is considered to be clinically significant [33]. Secondary outcome measures included perceived stress (perceive stress scale; PSS [34]) and negative affect (sum of three negative Visual Analog Scales; VAS), which were assessed at four time-points: at baseline, after the first emergency aid period, before the second emergency aid period, and at follow-up. At follow-up, we assessed clinician-rated PTSD symptom severity with the Clinician-Administered PTSD Scale (CAPS-5) [35], administered by telephone within one week after follow-up (mean [SD] = 1.51 [2.74] days, range: 0–27), which has shown high agreement (82%) with face-to-face interviews [36]. Additionally, we recorded the types of police-related traumatic events experienced before baseline and between assessments (Police Life Events Scale; PLES [37]) (see Supplementary Methods for more details on these questionnaires).
MRI acquisition
Structural MRI images were obtained with a 3T Magnetom Prisma scanner (Siemens Medical Systems, Erlangen, Germany), using a 32-channel head coil. We used a combined MPRAGE and GRAPPA sequence to acquire structural T1-weighted images (192 slices; repetition time (TR) = 2300 ms; echo time (TE) = 3.03 ms; field of view (FOV) = 256 mm; voxel size = 1.0 mm3; flip angle = 8°).
Hippocampal and amygdala segmentations
Hippocampal and amygdala substructure segmentations were performed on structural T1-weighted images (voxel size: 1.0 mm3) with the longitudinal processing pipeline [38] (default options in FreeSurfer developer v6.0) (see Supplementary Methods). This analysis provides volumes of 12 bilateral hippocampal subfields, subdivided in body and head when applicable (default options [39]), and volumes of 9 bilateral amygdala subnuclei (see Fig. 2 and Supplementary Fig. 2). We extracted volumes of the CA1, CA3 and DG, given previous observations of volume alterations in these regions in PTSD [21, 22, 24]. Volumes of the bilateral basal, lateral, medial and central amygdala were extracted, based on previous findings of baso-lateral and centro-medial volume alterations in PTSD [17, 29]. Output was visually inspected and checked according to standardized quality control procedures [24] (see Supplementary Methods and Supplementary Fig. 3). Reliability of (sub)structure segmentations was assessed by computing intraclass correlations, showing excellent concordance between volumes acquired at baseline and follow-up (see Supplementary Methods and Supplementary Fig. 4).
Automatic substructure segmentations generated with FreeSurfer 6.0 (developer version) for one representative subject. A Hippocampal subfields are displayed in the sagittal plane and B Amygdala subnuclei are displayed in the coronal plane. Substructures in bold text were included in the analyses. See Supplementary Fig. 2 for all generated substructures.
Statistical analysis
All statistical analyses were done in SPSS25. Differences in demographics, trauma exposure and clinical characteristics between drop-outs and study completers were tested with ANOVA’s for normally distributed continuous variables and Χ2-tests for categorical variables. We checked for outliers |Z | > 3.29 [40] and normality of continuous variables. To assess longitudinal changes in trauma exposure and trauma-related symptoms, we used repeated-measures ANOVA’s with between-subject factor Sex (male/female) and within-subjects factor Time (baseline/follow-up).
Prospective analysis
To investigate whether baseline hippocampal (DG/CA/CA3) and amygdala (basal/lateral/medial/central) substructure volumes predict an increase in trauma-related symptoms, we conducted three different analyses. First, we conducted multiple linear regression analyses on continuous symptom change. Next, to ascertain robustness of our findings, these analyses on continuous symptom change were complemented by exploratory logistic regression analyses on symptom development trajectories and on binary clinical cutoff.
Linear regression analyses were conducted on change in PTSD symptoms (ΔPCL; follow-up minus baseline), perceived stress (ΔPSS) and negative affect (ΔVAS) as dependent variables. Covariates included sex, age and baseline symptom severity. Following previous studies [21, 24], we corrected for whole hippocampal/amygdala volume, as substructures are highly correlated with whole structure volumes (in our sample: range r = [0.305 0.955]). To prevent multicollinearity issues, we calculated proportions of each substructure relative to its ipsilateral whole structure volume (i.e., proportion = substructure/ipsilateral whole structure volume). Using substructure proportions resulted in low collinearity statistics in all linear regression models (all Variance Intolerance Factors, VIFs < 2). Importantly, all substructure proportions were normally distributed, as indicated with skewness and kurtosis measures (all substructure proportions: skewness = [−0.262 0.911], kurtosis = [−0.556 0.833], rule of thumb skewness and kurtosis <2 [41]). In the linear regression models on prediction of symptom change, continuous variables were standardized to compare their predictive values. Heteroscedasticity-consistent standard errors (HC4) were used to reduce potential effects of heteroscedasticity on statistical inference [42]. For each structure (hippocampus/amygdala) and each hemisphere (left/right), all substructures were included as predictors in multiple linear regression models. We adjusted the alpha-level for multiple comparisons with Bonferroni correction, for our main outcome measure (ΔPCL: 4 models: 2 structures x 2 hemispheres) and our secondary outcome measures (ΔPSS-ΔVAS: 8 models: 2 structures × 2 hemispheres × 2 outcomes).
In exploratory follow-up analyses, we investigated whether hippocampal subfield volumes at baseline predicted specific DSM-5 PTSD symptom clusters (Cluster B: Intrusions; Cluster C: Avoidance; Cluster D: Negative alterations in cognitions and mood; Cluster E: Alterations in arousal and reactivity). As cluster subscores were zero-inflated, which could not be corrected for with data-transformations, we coded the development of at least one clinical symptom (severity ≥ 2) between assessments [43]. Binary logistic regression analyses were conducted on development of symptoms at each cluster (yes/no). The alpha-level was corrected for multiple comparisons (8 models: one model for each of the four symptom clusters, for left and right hippocampal subnuclei separately). Further, we conducted a logistic regression analysis on clinician-administered subthreshold PTSD at follow-up (yes/no).
Recent computational approaches have consistently identified different PTSD symptom trajectories, which may provide important implications for risk identification and interventions [31]. Therefore, in an exploratory analysis, we automatically identified PTSD symptom trajectories based on Δ-PCL, using the two-step cluster method [44]. In the first step (pre-clustering), cases are pre-clustered based on the log-likelihood distance measure. In the second step (clustering), the identified pre-clusters are merged into the desired number of clusters, which are automatically determined using the Akaike Information Criterion (AIC) as measure of fit. This two-step cluster method bares the advantage that the number of clusters is not based on arbitrary decisions. This clustering approach resulted in three symptom clusters: increase, decrease and no change (see results). Next, multinomial logistic regression analyses were conducted to investigate whether substructure volumes predicted symptom trajectories. The alpha-level was corrected for multiple comparisons (2 models: no change and decrease vs increase; increase and no change vs decrease). Covariates included age and sex in all logistic regression models.
To ascertain that predictive effects were not affected by pre-baseline trauma history, we repeated all linear and logistic regression analyses with childhood trauma (Childhood Trauma Questionnaire [CTQ] total sum), previous military experience (yes/no) and baseline police-related trauma history (PLES-baseline) as covariates. Additionally, we reran all regression analyses controlling for amount of police-related trauma exposure between assessments (ΔPLES as covariate).
Acquired changes
To investigate effects of trauma exposure and symptom change on alterations in substructure volumes, we conducted linear mixed models, allowing us to use all available datapoints (i.e., also when follow-up data were missing). Models included Time (baseline/follow-up), Sex (male/female), PTSD symptoms (ΔPCL), age and ipsilateral hippocampal/amygdala volume as fixed factors and a random intercept (maximum likelihood, AR1 covariance structure). Main effects of all fixed factors were investigated, as well as the interaction between Time and ΔPCL. These analyses were repeated with number of different police-related traumatic events experienced between waves (ΔPLES) as factor to test effects of trauma exposure on subfield/subnuclei volume changes.
Results
Trauma exposure and symptom development
See Table 1 for demographics, trauma history and clinical characteristics. Recruits reported a significant overall increase in police-related traumatic events between assessments (PLES: F(1,211) = 1018.00, p < 0.001, ωp2 = 0.827) (see Fig. 1C and Supplementary Fig. 5 for most frequently experienced events). Between assessments, we observed increased self-reported perceived stress (PSS: F(1,210) = 4.02, p = 0.046, ωp2 = 0.014) and negative affect (VAS: F(1,211) = 12.60, p < 0.001, ωp2 = 0.052) in all recruits, and increased PTSD symptoms in males (PCL: main effect Time: F(1,160) = 4.58, p = 0.034, ωp2 = 0.022), but not in females (Time x Sex interaction: F(1,219) = 4.06, p = 0.045, ωp2 = 0.014). Moreover, according to the diagnostic interview (CAPS), 29 participants fulfilled criteria for at least subthreshold PTSD at follow-up [45] (See Supplementary Results). Self-reported PTSD symptoms at follow-up (PCL) were positively associated with number of different experienced police-related traumatic events between assessments (PLES) (ρ(221) = 0.293, p < 0.001). See Supplementary Results for all results regarding trauma exposure and symptom change.
Smaller left DG-volume predicts PTSD symptom increase
Linear regression analyses
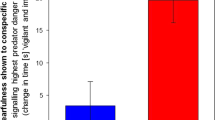
Smaller left DG-volumes at baseline predicted development of PTSD symptoms (ΔPCL: B(SE) = −0.21 (0.08), p = 0.011, 95% CI = −0.38–0.05) (αadjusted = 0.0125). Additionally, smaller left DG-volume was associated with development of negative affect (ΔVAS: B(SE) = −0.21 (0.07), p = 0.005, 95% CI = −0.36–0.06) and perceived stress (ΔPSS: B(SE) = −0.16 (0.07), p = 0.024, 95% CI = 0.29–0.02), although the latter did not survive multiple comparison correction (αadjusted = 0.0062) (see Fig. 3). These effects became slightly stronger when correcting for amount of trauma exposure between assessments (ΔPCL B(SE) = −0.22 (0.08), p = 0.007; ΔVAS B(SE) = −0.30 (−0.03), p = 0.003; ΔPSS B(SE) = −0.16 (0.07), p = 0.018), and when correcting for pre-baseline trauma history (ΔPCL B(SE) = −0.22 (0.08), p = 0.006; ΔVAS B(SE) = −0.21 (−0.08), p = 0.006; ΔPSS B(SE) = −0.16 (0.07), p = 0.018) (see Supplementary Table 2). The magnitude of correlation coefficients were comparable for males and females (ΔPCL Fisher’s z = −0.23, p = 0.82; ΔVAS z = −1.01, p = 0.31; ΔPSS z = −0.68, p = 0.50). Interestingly, an exploratory analysis showed that the negative association between left DG-volumes at baseline and increase in PTSD symptoms was stronger for participants who experienced relatively more childhood trauma (CTQ x left DG interaction: B(SE) = −0.23 (0.08), p = 0.006, 95% CI = −0.40–0.07). This interaction effect did not reach statistical significance for negative affect and perceived stress as outcome measures (Bs [−0.14 0.00], all p > 0.14).
Negative associations between pre-trauma left DG-volume and increase in A PTSD symptoms (ΔPCL: wave 2–1), B perceived stress symptoms (ΔPSS) and C negative affect (ΔVAS). Shaded areas indicate 95% confidence interval. PCL PTSD checklist, PSS perceived stress scale, VAS visual analog scales. ZResidual standardized residual, corrected for age, sex, baseline symptoms, CA1 and CA3 volumes.
Other hippocampal subfields did not predict change in trauma-related symptoms (Bs [−0.12 0.16], all p > 0.09) (see Supplementary Table 2). Critically, baseline PTSD symptoms, perceived stress and negative affect were not significantly associated with left DG-volume, nor with other subfield volumes (Bs [−0.08 0.13], all p > 0.167). Whole left and right hippocampal volumes and amygdala (sub)volumes were not associated with symptom change (Bs [−0.18 0.09], all p > 0.04) (see Supplementary Table 3). Furthermore, pre-baseline trauma exposure (childhood trauma history, previous military experience and baseline police-related traumatic events) was not significantly associated with hippocampal subfield volumes at baseline (Bs [−0.16 0.29], all p > 0.065) (see Supplementary Table 5). Taken together, pre-trauma left DG-volume predicted an increase of stress-related symptoms upon trauma exposure.
Symptom trajectories and clusters
We identified three symptom-change groups based on ΔPCL: 1) PTSD symptom increase (N = 35, 15.84%, ΔPCL [SD] = 16.00 [7.26]); 2) PTSD symptom decrease (N = 46, 20.5%, ΔPCL [SD] = −8.61 [4.28]); and 3) no symptom change (N = 140, 62.5%, ΔPCL [SD] = 0.76 [2.23]) (see Fig. 1D). These groups did not differ in age, sex distribution, number of drop-outs, educational level, baseline and follow-up and childhood trauma history (all p > 0.064). Increases in PTSD symptoms (ΔPCL), perceived stress (ΔPSS) and negative affect (ΔVAS) were significantly greater in the symptom increase group, compared to the no change group (all p < 0.005) and were higher at follow-up compared to the symptom decrease group (all p < 0.008) (see Supplementary Results for all comparisons and Supplementary Fig. 6). Critically, smaller left DG-volume at baseline was associated with higher risk for the symptom increase group, compared to the no symptom change group (W = 5.35, p = 0.021) and nominally compared to the symptom decrease group (W = 4.42, p = 0.036) (αadjusted = 0.025) (see Fig. 4). These group analyses also revealed no associations with any other subfield volumes (all p > 0.155), and left DG-volume was not predictive of the PTSD symptom decrease group vs the no change group (p = 0.843). Furthermore, when we divide participants into those that show a clinically significant increase of ≥10 points on the PCL-5 (n = 28), a clinically significant decrease of ≥10 points (n = 18) and those who did not show a clinically significant change in PCL-5 score (n = 164) [33], multinomial regression analyses again showed that smaller left DG volumes at baseline predicted symptom increase vs no change (W = 5.12, p = 0.024).
Left dentate gyrus (DG) volume significantly predicting symptom increase, development of cluster B and cluster D symptoms and subthreshold PTSD. OR odds ratio; *p < 0.05 Bonferroni corrected; #p < 0.10 Bonferroni corrected. CAPS Clinician administered PTSD scale. Cluster B: Intrusions; Cluster C: Avoidance; Cluster D: Negative alterations in cognitions and mood; Cluster E: Alterations in arousal and reactivity.
Regarding PTSD symptom clusters, smaller left DG-volumes at baseline predicted increase in intrusions (Cluster-B: W = 9.98, p = 0.002) and negative alterations in cognitions and mood (Cluster-D: W = 8.82, p = 0.003), but not avoidance (Cluster-C) or hyperarousal (Cluster-E) symptoms (see Fig. 4) (αadjusted = 0.0062). Finally, smaller left DG-volume (but no other subfield volume) was nominally associated with higher risk of developing clinician-rated subthreshold PTSD at follow-up (W = 3.59, p = 0.058). Findings remained significant after controlling for trauma exposure between assessments and after controlling for pre-baseline trauma history (see Supplementary Table 4).
Subfield partialization
To explore more specific localization of DG-volume effects on stress vulnerability, the abovementioned analyses were repeated for DG-subfield body and head volumes separately (see Supplementary Fig. 2). The predictive effects were driven by both left DG body and head volumes (see Supplementary Results and Supplementary Fig. 7). No significant effects were found for other subfields’ body and head volumes (all p > 0.056), except for larger CA3-head volume predicting development of cluster-D symptoms (W = 6.76, p = 0.018).
Acquired changes
Hippocampal and amygdala (sub)structure volumes did not change between assessments (Main effect Time: all p > 0.215), which was not moderated by symptom change (Time × ΔPCL interaction: all p > 0.110). Experiencing more police-related traumatic events between assessments was associated with an increase in left basal nucleus volume (Time × ΔPLES interaction: B(SE) = 0.11 (0.05), p = 0.026), but not with other (sub)structure volume changes (all p > 0.070). Follow-up analyses showed that the trauma-related increase in left basal nucleus volume was not associated with amount of childhood trauma exposure (Time × ΔPLES × CTQ interaction: p = 0.225) or development of PTSD symptoms (Time × ΔPLES × ΔPCL interaction: p = 0.440). See Supplementary Results for all results.
Discussion
The aim of this study was to investigate whether alterations in hippocampal and amygdala volume, previously observed in PTSD-patients, may represent predisposing vulnerability factors or are acquired after trauma exposure. In a prospective longitudinal investigation among healthy police recruits at high risk for trauma exposure, we showed that left dentate gyrus (DG) volumes at baseline predicted development of trauma-related symptoms at follow-up. This pattern emerged not only when using trauma-related symptoms as continuous measures, but also in confirmatory follow-up analyses classifying participants into symptom-trajectory and diagnostic classification groups. Regarding acquired effects, increased volume of the left basal nucleus of the amygdala post-trauma was positively related to amount of trauma exposure between both baseline and follow-up.
Our findings indicate that, specifically, smaller pre-trauma DG-volumes represent a vulnerability factor for development of trauma-related symptoms, even when corrected for amount of trauma exposure. Recent insights from animal work suggest that this vulnerability may be mediated by decreased adult DG-neurogenesis: suppression of adult DG-neurogenesis increases vulnerability to chronic stress, while increasing neurogenesis confers resilience [46]. Of note, we cannot ascertain that smaller DG volumes in humans resulted from decreased neurogenesis specifically. Nevertheless, human work with electroconvulsive therapy was positively associated with clinical improvement of depressive symptoms [47]. Theories linking DG-functioning to PTSD typically build on the fact that the DG plays an important role in pattern separation, or the ability to store similar events as separate memories [19, 20]. DG-dysfunction has been associated with failure to disambiguate a new experience from stored fearful memories, possibly underlying excessive fear and intrusive thoughts in PTSD in response to stimuli that bear resemblance to features of the traumatic event [5, 19, 48]. Indeed, we observed that smaller DG-volume predicted development of intrusion symptoms specifically.
These observations tentatively suggest that interventions targeting DG-dependent memory function may be of critical preventive and therapeutic value. One promising way to stimulate DG-dependent pattern separation could be physical activity: exercise was found to stimulate DG-neurogenesis and to improve memory function in rodents [49]. In humans, aerobic exercise (40-min walking for three times a week over the course of one year) resulted in a 2% increase of anterior hippocampal volumes (including the DG) as well as improved memory function [50]. Furthermore, antidepressants are effective in increasing DG-dependent pattern separation [19]. These findings suggest promising directions for future research, since exactly how smaller DG-volumes are associated with cognitive and affective functioning remains elusive, as well as whether stimulating DG-functioning may indeed protect against the development of PTSD-symptomatology.
Regarding amygdala subnuclei, amount of police-related trauma exposure between assessments was positively associated with left basal nucleus volume increases. This nucleus is part of BLA [27], which is implicated in fear acquisition, by receiving inputs from sensory cortices, thalamus and dorsal anterior cingulate cortex. In rodents, chronic stress [51] and elevated corticosterone levels [52] increased BLA spine density and dendritic hypertrophy, as well as anxiogenic behavior, which both persisted up until 3 weeks of stress-free recovery [51]. Possibly, trauma-induced amygdala sensitivity, including increased basal nucleus volume, mediates cumulative effects of multiple trauma’s on PTSD symptom severity [53]. Notably, our findings suggest that amygdala alterations in PTSD may result from trauma exposure, rather than PTSD [7, 54]. Investigating the effects of timing, duration and severity of trauma exposure on amygdala subfield volumes remains an important research avenue.
Notably, whole hippocampal and amygdala volumes were not associated with symptom development or trauma exposure. This seems to contradict previous large-scale meta-analytic findings, showing smaller hippocampal and amygdala volumes PTSD patients compared to controls [7]. We hypothesize that changes in whole hippocampal and amygdala volumes may become apparent after more prolonged exposure to chronic stress and/or PTSD. Possibly, hippocampal and amygdala (sub)volume changes in PTSD reflect a complex interaction between predisposing vulnerability effects and effects of subsequent chronic stress exposure or disease duration, with different substructures being differentially affected at these distinct stages.
Our findings should be interpreted in light of several strengths and limitations. We investigated a large sample of resilient police recruits, with the majority of participants reporting no clinical symptoms at follow-up and 14% reporting a clinically significant increase in PTSD symptoms between assessments. Our large resilient sample bears the advantage we can pick up subtle individual differences in PTSD vulnerability, without potentially confounding effects of common comorbidities, such as major depressive disorder and substance abuse. However, our resilient and predominantly male sample (73.3% males) may have limited the generalizability of our findings to the broader PTSD population, which is characterized by a higher prevalence in females [55, 56] and co-morbid psychiatric disorders [1]. Further, it remains to be shown whether our findings generalize to consequences of more prolonged or different types of trauma exposure [53]. In addition, while we controlled for various types of trauma history, including childhood trauma, military experience, and police-related trauma, these measures were taken retrospectively and may not have captured all trauma exposure before study participation. Therefore we cannot rule out that pre-baseline traumatic experiences influenced hippocampal and amygdala substructure volumes at baseline. Additionally, DG volume reductions are not a unique neural signature of PTSD, but also apparent in other psychiatric disorders, including depression [57] and schizophrenia [58]. Given the high comorbidity of PTSD and depression, it is relevant to investigate whether smaller DG-volumes represent a predisposing vulnerability for development of depressive symptoms. Finally, we found significant predictive effects of left (but not right) DG-volumes, although directionality of the effects was similar for right DG-volumes, and strength of the effects was not significantly different between left and right DG-volumes (all p > 0.056). On the one hand, this could indicate a lack of power to pick up right DG-volume effects. On the other, a recent meta-analysis on structural imaging studies in PTSD also showed that left hippocampal volume reductions were associated with higher PTSD symptoms, and suggested that left hippocampal volumes may be more severely affected in PTSD [8]. In line with this suggestion, left hippocampal volume reductions were predictive of persistence of PTSD symptoms after treatment [11], and were associated with higher PTSD symptom severity [59, 60], including intrusion symptoms in a civilian [61] and Dutch police sample [62]. Similarly, we observed acquired effects of amount of trauma exposure in the left, but not right, basal amygdala nucleus. Notably, a recent study also found that amount of trauma exposure was positively associated with left, but not right amygdala volumes in children and adolescents [63]. Our findings are thus consistent with recent literature suggesting that both acquired and predictive effects in amygdala-hippocampal circuitry may be relatively more apparent in the left hemisphere.
Identifying neurobiological vulnerability factors for PTSD development could improve screening of at risk individuals and result in new neurobiological targets for early interventions. Our longitudinal, prospective study allowed us to disentangle predisposing hippocampal and amygdala substructure abnormalities predictive of PTSD symptom development, from the acquired effects of trauma exposure on these regions. We showed that smaller pre-trauma DG-volumes predicted increase in trauma-related symptoms, suggesting that smaller DG-volumes may be a biomarker for PTSD vulnerability. Targeting this vulnerability factor with interventions, such as antidepressants, ECT, or exercise, to improve resilience, should be the focus of future research.
Funding and disclosures
This study was funded by the Netherlands Organization for Scientific Research (NWO VICI-grant 453-12-0010) and a starting grant from the European Research Council (StG2012 313749), both awarded to Karin Roelofs. The authors declare no conflicts of interest.
References
Goldstein R, Smith S, Chou S, Saha T, Jung J, Zhang H, et al. The epidemiology of DSM-5 posttraumatic stress disorder in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Soc Psychiatry Psychiatr Epidemiol. 2016;51:1137–48.
Pitman RK, Rasmusson AM, Koenen KC, Shin LM, Orr SP, Gilbertson MW, et al. Biological studies of post-traumatic stress disorder. Nat Rev Neurosci. 2012;13:769–87.
Koch SBJ, Morey RA, Roelofs K. The role of the dentate gyrus in stress-related disorders. Mol Psychiatry. 2019;25:1361–63.
American Psychiatric Association. DSM-5, diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA, US: American Psychiatric Publishing Inc.; 2013.
Liberzon I, Abelson JL. Context processing and the neurobiology of post-traumatic stress disorder. Neuron. 2016;92:14–30.
Bromis K, Calem M, Reinders AATS, Williams SCR, Kempton MJ. Meta-analysis of 89 structural MRI studies in posttraumatic stress disorder and comparison with major depressive disorder. Am J Psychiatry. 2018;175:989–98.
Logue MW, van Rooij SJH, Dennis EL, Davis SL, Hayes JP, Stevens JS, et al. Smaller hippocampal volume in posttraumatic stress disorder: a multisite ENIGMA-PGC study: subcortical volumetry results from posttraumatic stress disorder consortia. Biol Psychiatry. 2018;83:244–53.
Nelson MD, Tumpap AM. Posttraumatic stress disorder symptom severity is associated with left hippocampal volume reduction: a meta-analytic study. CNS Spectr. 2017;22:363–72.
Morey RA, Gold AL, LaBar KS, Beall SK, Brown VM, Haswell CC, et al. Amygdala volume changes in posttraumatic stress disorder in a large case-controlled veterans group. Arch Gen Psychiatry. 2012;69:1169–78.
Gilbertson M, Shenton M, Ciszewski A. Smaller hippocampal volume predicts pathologic vulnerability to psychological trauma. Nat Neurosci. 2002;i:1242–7.
van Rooij SJH, Kennis M, Sjouwerman R, van den Heuvel MP, Kahn RS, Geuze E. Smaller hippocampal volume as a vulnerability factor for the persistence of post-traumatic stress disorder. Psychol Med. 2015;45:2737–46.
Lindgren L, Bergdahl J, Nyberg L. Longitudinal evidence for smaller hippocampus volume as a vulnerability factor for perceived stress. 2016. https://doi.org/10.1093/cercor/bhw154.
Quidé Y, Andersson F, Dufour-Rainfray D, Descriaud C, Brizard B, Gissot V, et al. Smaller hippocampal volume following sexual assault in women is associated with post-traumatic stress disorder. Acta Psychiatr Scand. 2018;138:312–24.
Roozendaal B, McEwen BS, Chattarji S. Stress, memory and the amygdala. Nat Rev Neurosci. 2009;10:423–33.
Sapolsky RM. Why stress is bad for your brain. Science. 1996;273:749–50.
Admon R, Milad MR, Hendler T. A causal model of post-traumatic stress disorder: disentangling predisposed from acquired neural abnormalities. Trends Cogn Sci. 2013;17:337–47.
Veer IM, Oei NYL, van Buchem MA, Spinhoven P, Elzinga BM, Rombouts SARB. Evidence for smaller right amygdala volumes in posttraumatic stress disorder following childhood trauma. Psychiatry Res Neuroimaging. 2015;233:436–42.
Kleim B, Ehlers A, Glucksman E. Early predictors of chronic post-traumatic stress disorder in assault survivors. Psychol Med. 2007;37:1457–67.
Kheirbek MA, Klemenhagen KC, Sahay A, Hen R. Neurogenesis and generalization: a new approach to stratify and treat anxiety disorders. Nat Neurosci. 2012;15:1613–20.
Leal SL, Yassa MA. Integrating new findings and examining clinical applications of pattern separation. Nat Neurosci. 2018;21:163–73.
Hayes JP, Hayes S, Miller DR, Lafleche G, Logue MW, Verfaellie M. Automated measurement of hippocampal subfields in PTSD: Evidence for smaller dentate gyrus volume. J Psychiatr Res. 2017;95:247–52.
Wang Z, Neylan TC, Mueller SG, Lenoci M, Truran D, Marmar CR, et al. Magnetic resonance imaging of hippocampal subfields in posttraumatic stress disorder. Arch Gen Psychiatry. 2010;67:296–303.
Luo Y, Liu Y, Qin Y, Zhang X, Ma T, Wu W, et al. The atrophy and laterality of the hippocampal subfields in parents with or without posttraumatic stress disorder who lost their only child in China. Neurol Sci. 2017;38:1241–7.
Chen LW, Sun D, Davis SL, Haswell CC, Dennis EL, Swanson CA, et al. Smaller hippocampal CA1 subfield volume in posttraumatic stress disorder. Depress Anxiety. 2018;35:1018–29.
Dimsdale-Zucker HR, Ritchey M, Ekstrom AD, Yonelinas AP, Ranganath C. CA1 and CA3 differentially support spontaneous retrieval of episodic contexts within human hippocampal subfields. Nat Commun. 2018;9:1–8.
Ji J, Maren S. Differential roles for hippocampal areas CA1 and CA3 in the contextual encoding and retrieval of extinguished fear. Learn Mem. 2008;15:244–51.
Tovote P, Fadok JP, Lüthi A. Neuronal circuits for fear and anxiety. Nat Rev Neurosci. 2015;16:317–31.
Yang RJ, Mozhui K, Karlsson RM, Cameron HA, Williams RW, Holmes A. Variation in mouse basolateral amygdala volume is associated with differences in stress reactivity and fear learning. Neuropsychopharmacology. 2008;33:2595–604.
Yang RJ, Mozhui K, Karlsson RM, Cameron HA, Williams RW, Holmes A. The association of PTSD symptom severity with localized hippocampus and amygdala abnormalities. Chronic Stress. 2017;1:2470547017724069.
Morey RA, Clarke EK, Haswell CC, Phillips RD, Clausen AN, Mufford MS, et al. Amygdala nuclei volume and shape in military veterans with posttraumatic stress disorder. Biol Psychiatry Cogn Neurosci Neuroimaging 2020;5:281–90.
Galatzer-Levy IR, Huang SH, Bonanno GA. Trajectories of resilience and dysfunction following potential trauma: a review and statistical evaluation. Clin Psychol Rev. 2018;63:41–55.
Koch SBJ, Klumpers F, Zhang W, Hashemi MM, Kaldewaij R, van Ast VA, et al. The role of automatic defensive responses in the development of posttraumatic stress symptoms in police recruits: protocol of a prospective study. Eur J Psychotraumatol. 2017;8:1412226.
Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov. 2013.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385.
Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a Clinician-Administered PTSD Scale. J Trauma Stress. 1995;8:75–90.
Aziz MA, Kenford S. Comparability of telephone and face-to-face interviews in assessing patients with posttraumatic stress disorder. J Psychiatr Pract. 2004;10:307–13.
Carlier I, Gersons B. Development of a scale for traumatic incidents in police work. Psychiatr Fenn. 1992;23:59–70.
Reuter M, Schmansky NJ, Rosas HD, Fischl B. Within-subject template estimation for unbiased longitudinal image analysis. Neuroimage. 2012;61:1402–18.
Iglesias JE, Augustinack JC, Nguyen K, Player CM, Player A, Wright M, et al. A computational atlas of the hippocampal formation using ex vivo, ultra-high resolution MRI: Application to adaptive segmentation of in vivo MRI. Neuroimage. 2015;115:117–37.
Tabachnick BG, Fidell LS. Using Multivariate Statistics. 4th Edn. Boston: Allyn and Bacon; 2001.
George D, Mallery M. SPSS for windows step by step: a simple guide and reference, 17.0 update. 10a ed. Boston: Pearson; 2010.
Hayes AF, Cai L. Using heteroskedasticity-consistent standard error estimators in OLS regression: an introduction and software implementation. Behav Res Methods. 2007;39:709–22.
Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, Keane TM. The clinician-administered PTSD scale for DSM-5 (CAPS-5). Interview available from the National Center for PTSD at www.ptsd.va.gov. 2013.
Peter-Hagene LC, Ullman SE. Sexual assault-characteristics effects on PTSD and psychosocial mediators: a cluster-analysis approach to sexual assault types. Psychol Trauma. 2015;7:162–70.
Brancu M, Mann-Wrobel M, Beckham JC, Wagner HR, Elliott A, Robbins AT, et al. Subthreshold posttraumatic stress disorder: a meta-analytic review of DSM–IV prevalence and a proposed DSM–5 approach to measurement. Psychol Trauma Theory, Res Pr Policy. 2016;8:222–32.
Anacker C, Luna VM, Stevens GS, Millette A, Shores R, Jimenez JC, et al. Hippocampal neurogenesis confers stress resilience by inhibiting the ventral dentate gyrus. Nature. 2018;559:98–102.
Nuninga JO, Mandl RCW, Boks MP, Bakker S, Somers M, Heringa SM, et al. Volume increase in the dentate gyrus after electroconvulsive therapy in depressed patients as measured with 7T. Molecular Psychiatry. 2020;25;1559–68.
Morey RA, Dunsmoor JE, Haswell CC, Brown VM, Vora A, Weiner J, et al. Fear learning circuitry is biased toward generalization of fear associations in posttraumatic stress disorder. Transl Psychiatry. 2015;5:e700.
Creer DJ, Romberg C, Saksida LM, van Praag H, Bussey TJ. Running enhances spatial pattern separation in mice. Proc Natl Acad Sci USA. 2010;107:2367–72.
Erickson KI, Voss MW, Prakash RS, Basak C, Szabo A, Chaddock L, et al. Exercise training increases size of hippocampus and improves memory. Proc Natl Acad Sci USA. 2011;108:3017–22.
Vyas A, Pillai AG, Chattarji S. Recovery after chronic stress fails to reverse amygdaloid neuronal hypertrophy and enhanced anxiety-like behavior. Neuroscience. 2004;128:667–73.
Mitra R, Sapolsky RM. Acute corticosterone treatment is sufficient to induce anxiety and amygdaloid dendritic hypertrophy. Proc Natl Acad Sci USA. 2008;105:5573–8.
Liu H, Petukhova MV, Sampson NA, Aguilar-Gaxiola S, Alonso J, Andrade LH, et al. Association of DSM-IV posttraumatic stress disorder with traumatic experience type and history in the World Health Organization World Mental Health Surveys. JAMA Psychiatry. 2017;74:270.
van Wingen GA, Geuze E, Vermetten E, Fernández G. Perceived threat predicts the neural sequelae of combat stress. Mol Psychiatry. 2011;16:664–71.
Olff M, Langeland W, Draijer N, Gersons BPR. Gender differences in posttraumatic stress disorder. Psychol Bull. 2007;133:183–204.
Olff M. Sex and gender differences in post-traumatic stress disorder: an update. Eur J Psychotraumatol. 2017;8;1351204. https://doi.org/10.1080/20008198.2017.1351204.
Boldrini M, Santiago AN, Hen R, Dwork AJ, Rosoklija GB, Tamir H, et al. Hippocampal granule neuron number and dentate gyrus volume in antidepressant-treated and untreated major depression. Neuropsychopharmacology. 2013;38:1068–77.
Haukvik UK, Westlye LT, Mørch-Johnsen L, Jørgensen KN, Lange EH, Dale AM, et al. In vivo hippocampal subfield volumes in schizophrenia and bipolar disorder. Biol Psychiatry. 2015;77:581–8.
Shu X-JJ, Xue L, Liu W, Chen F-YY, Zhu C, Sun X-HH, et al. More vulnerability of left than right hippocampal damage in right-handed patients with post-traumatic stress disorder. Psychiatry Res. 2013;212:237–44.
Villarreal G, Hamilton DA, Petropoulos H, Driscoll I, Rowland LM, Griego JA, et al. Reduced hippocampal volume and total white matter volume in posttraumatic stress disorder. Biol Psychiatry. 2002;52:119–25.
Villarreal G, Petropoulos H, Hamilton DA, Rowland LM, Horan WP, Griego JA, et al. Proton magnetic resonance spectroscopy of the hippocampus and occipital white matter in PTSD: preliminary results. Can J PsychiatryRevue Can Psychiatr. 2002;47:666–70.
Lindauer RJL, Vlieger EJ, Jalink M, Olff M, Carlier IVE, Majoie CBLM, et al. Smaller hippocampal volume in Dutch police officers with posttraumatic stress disorder. Biol Psychiatry. 2004;56:356–63.
van Rooij SJH, Smith RD, Stenson AF, Ely TD, Yang X, Tottenham N, et al. Increased activation of the fear neurocircuitry in children exposed to violence. Depress Anxiety. 2020. https://doi.org/10.1002/da.22994.
Acknowledgements
We thank all participants for their willingness to participate in this study. The authors thank Annika Smit and other personnel of the Dutch Police Academy for their valuable help with recruiting participants and facilitating our study. We gratefully acknowledge contributions of the Ingrid Kerstens, Tiele Döpp, Naomi de Valk, Leonore Bovy and Lisanne Nuijen in participant recruitment and data acquisition.
Author information
Authors and Affiliations
Contributions
All authors contributed to designing the study. RK, WZ & MMH acquired the data and SBJK analyzed the data. All authors contributed to interpreting the results and writing the manuscript. All authors approved the final version of the manuscript before submission.
Corresponding author
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Koch, S.B.J., van Ast, V.A., Kaldewaij, R. et al. Larger dentate gyrus volume as predisposing resilience factor for the development of trauma-related symptoms. Neuropsychopharmacol. 46, 1283–1292 (2021). https://doi.org/10.1038/s41386-020-00947-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-020-00947-7
This article is cited by
-
Neuroimaging of posttraumatic stress disorder in adults and youth: progress over the last decade on three leading questions of the field
Molecular Psychiatry (2024)
-
Longitudinal volumetric evaluation of hippocampus and amygdala subregions in recent trauma survivors
Molecular Psychiatry (2023)
-
Sex-dependent risk factors for PTSD: a prospective structural MRI study
Neuropsychopharmacology (2022)
-
Structural covariance of the ventral visual stream predicts posttraumatic intrusion and nightmare symptoms: a multivariate data fusion analysis
Translational Psychiatry (2022)
-
Neural contributors to trauma resilience: a review of longitudinal neuroimaging studies
Translational Psychiatry (2021)