Abstract
The persistence of drug taking despite its adverse consequences plays a central role in the presentation, diagnosis, and impacts of addiction. Eventual recognition and appraisal of these adverse consequences is central to decisions to reduce or cease use. However, the most appropriate ways of conceptualizing persistence in the face of adverse consequences remain unclear. Here we review evidence that there are at least three pathways to persistent use despite the negative consequences of that use. A cognitive pathway for recognition of adverse consequences, a motivational pathway for valuation of these consequences, and a behavioral pathway for responding to these adverse consequences. These pathways are dynamic, not linear, with multiple possible trajectories between them, and each is sufficient to produce persistence. We describe these pathways, their characteristics, brain cellular and circuit substrates, and we highlight their relevance to different pathways to self- and treatment-guided behavior change.
Similar content being viewed by others
Introduction
In 2016, Pickard and Ahmed posed the ‘puzzle of choice’ [1]. They began by considering evidence that people with problematic drug use can frequently control their behavior and can choose to abstain under many circumstances. Given this evidence for controlled drug use, Pickard and Ahmed asked why do these individuals choose to use despite the portent of negative consequences from that use?
The apparent insensitivity of drug taking to its adverse consequences is among the most pernicious features of addiction. It is responsible for a large part of the human toll of addiction, contributing directly to the detriments in health and well-being suffered by individuals, and imposing substantial burdens upon families and communities. Insensitivity to adverse consequences is not limited to drug use. It is shared with other problematic behaviors such as problem gambling that impose real and significant costs on individuals and the community.
Given the key role that insensitivity to adverse consequences plays in the presentation, diagnosis, and impacts of persistent drug use, as well as evidence that the eventual recognition and appraisal of these adverse consequences contributes to decisions to reduce or cease use [2,3,4], it is not surprising that it has been of intense interest. However, the most appropriate ways of conceptualizing this insensitivity remains unclear [5] and sometimes controversial [6, 7]. The diverse conditions under which insensitivity is observed and heterogeneity in its presentation imply that it is multifactorial. Yet, often only single mechanism solutions are presented for this problem [7], and these are typically presented as linear transitions or trajectories.
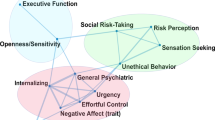
Here we argue for three pathways to insensitivity that may contribute to persistent drug use despite its negative consequences (Fig. 1)Footnote 1. A cognitive pathway for recognition of adverse consequences, a motivational pathway for valuation of these consequences, and a behavioral pathway for responding to these consequences. These pathways can operate in the same individual at different times, they can be independent with multiple possible trajectories between them, and each is sufficient to produce insensitivity. These pathways are embedded in complex backgrounds of intoxication, history of dependence, acute or protracted withdrawal, and stress. We describe how these pathways differ from each other and we consider their relevance for self- and treatment-guided behavior change.
At least three pathways, representing distinct psychological factors, may each be sufficient to produce insensitivity to punishment and cause persistent, detrimental behavior. Insensitivity can arise from poor instrumental contingency knowledge (cognitive pathway), distortions in positive and/or negative valuation of consequences (motivational pathway), and/or alterations in behavioral autonomy (behavioral pathway). These pathways occur against complex backgrounds of intoxication, history of dependence, acute or protracted withdrawal, and acute as well as chronic stressors that can influence capacity to detect, appropriately learn about, weight, and respond to negative consequences. These pathways can operate independently but may also interact. They are underpinned by still poorly understood distinct (as shown in colored) but partially overlapping (as shown in gray) neural circuitries. These pathways are likely dynamic and non-linear. Each may operate within the same individual at different times. Resolution of problematic behaviors will depend on which of these factors is contributing at specific times to cause persistence of behavior. dlPFC—dorsolateral prefrontal cortex, mPFC—medial prefrontal cortex, IC—insular cortex, Thal—thalamus, Str—striatum, DM—dorsomedial striatum, DL—dorsolateral striatum, V—ventral striatum, Ce—central amygdala, BL—basolateral amygdala complex.
The adverse consequences of drug use
Although not all drug use, even when prolonged, has negative consequences for an individual, prolonged drug use can have profound deleterious impacts on the health and well-being of individual users, ranging from acute toxicity to chronic health conditions [8,9,10]. Some adverse consequences may be directly, causally linked to drug use (e.g., overdose, hepatitis, HIV), whereas others are multifactorial and drug use adds to their risk (e.g., psychiatric disorders, cancers). Regardless, the burden of illicit drug use is estimated at 0.8% of global all-cause disability adjusted life years [9, 11]. The impact of licit substance use is greater still with alcohol use alone accounting for 5.1% of the global burden of disease and injury [12]. Adverse effects are not restricted to impacts on health. Persistent substance use creates and exacerbates relationship and interpersonal problems and can lead to detrimental neglect of familial and occupational responsibilities as well as direct harm to others. Persistence of use in the face of adverse impacts is held to distinguish problematic from recreational drug use. It also forms a key part of formal diagnosis [13, 14].
Non-human animal models of drug use serve an important role in studying adverse consequences because they allow precise control over drug history, assessment of individual differences, and titration of adverse consequences. Indeed, there has been progress in understanding whether, when, and why laboratory animals persist in drug self-administration despite adverse consequences [15]. In a typical experiment, rats or mice are first trained to self-administer a substance, under simple (e.g., fixed ratio) or more sophisticated (e.g., ‘seeking-taking’) schedules. Then, adverse consequences are introduced to punish this behavior, such as arranging that responding for the substance also leads to footshock [16,17,18,19,20], conditioned fear [21, 22], air puffs [23], or adulteration of the substance [24, 25]. The precise parametric relationship between drug seeking or taking and punishment varies across studies and these parameters are important to consider because they constrain and confound interpretation [19, 26]. In general, though, under these conditions, some laboratory animals reduce or cease drug self-administration, showing that drug seeking and taking are sensitive to adverse consequences. However, despite being subjected to negative consequences, some laboratory animals persist in seeking and taking. Such persistence has been observed in laboratory animals self-administering cocaine [19, 27,28,29,30,31], heroin [32], methamphetamine, and alcohol [24, 33].
This work has identified at least five features of insensitivity to adverse consequences. First, when low to moderate intensity punishers are used, only some mice [24] and rats [20, 33] are insensitive, speaking to individual variability in humans. Second, factors relating to initial drug use, including preference, intake, and rate of self-administration, are unrelated to insensitivity [18, 19, 21, 29, 34, 35]. This shows that insensitivity is separate to mechanisms governing initial use [36,37,38]. Third, extended self-administration and longer access per self-administration session favor insensitivity [19, 27, 38]. Fourth, propensity to drug seek under progressive ratio schedules [16, 18,19,20, 28, 30, 33, 39, 40], increased responding during extinction [18, 21, 28, 39, 40] or increased economic demand [41, 42] can predict insensitivity (but see [29, 35, 43,44,45]). Fifth, response impulsivity, such as reduced ability to wait before performing an appropriate response [29, 35] can predict insensitivity. These features are robust and replicable. They are important because they speak to, and constrain, mechanisms for insensitivity. We draw on these features when considering properties of the three putative pathways to insensitity to adverse consequences.
Cognitive pathways: recognizing adverse consequences
The cognitive pathway to persisting in drug taking despite negative consequences refers to the knowledge that an individual has about the consequences of their drug use (Fig. 1). Recognizing and identifying the negative consequences of drug use are necessary conditions for those consequences to change behavior. Yet for many individuals, choices to use a drug often do not incorporate possible adverse consequences from that use [3, 4, 46]. To be sure, severe adverse consequences such as financial, familial, medical, employment, or legal problems can predict treatment seeking in some people [47, 48]. However, recognition of the severity of these consequences and their relationship to drug use is rarely immediate [1]. Recognition that one’s drug use is responsible for negative consequences often occurs gradually, with individuals engaging in cognitive appraisals that can help drive self- or treatment-guided behavior change [2,3,4, 49, 50].
Engaging in these reappraisals may be difficult. Counselling approaches, such as motivational interviewing, capitalize on and enhance motivation to change [51]. These approaches can be highly effective for some people [52] but they can be less effective at creating the initial motivation to change [51, 53]. Reappraisals start gradually and behavior changes irregularly, often in highly personalized ways [3, 49]. This individuality has been argued to be beyond the reach of neuroscience [3], but recent work is beginning to show why correctly recognizing the negative consequences of our actions can be difficult.
Experience does not always deliver veridical causal knowledge about our actions. Humans [54,55,56] and other animals [57, 58] differ profoundly in what they learn about the consequences of their actions. These differences in learning can drive pronounced differences in choice. Some people form correct causal beliefs about how their actions cause adverse consequences. They can use this knowledge to choose other behaviors. In contrast, other people form incorrect beliefs about the causes of adverse consequences. Their lack of correct awareness leads them to choose actions with adverse consequences.
For example, Jean-Richard-dit-Bressel et al. [54] used a conditioned punishment task in young adults that allowed them to choose between two responses, one earning probabilistic rewards and one earning probabilistic reward and punishment. Participants were provided with no information about the specific punishment contingencies. They had to learn these from experience. Some readily learned to reallocate behavior away from the punished behavior, others did not. These differences were not due to differences in engagement with the task or in valuation of reward or punishment. Instead, sensitive and insensitive individuals differed profoundly in what they learned. Punishment sensitive individuals acquired correct causal beliefs about their behavior. They learned the correct Action–Punisher contingencies that they used to avoid further punishment. Punishment insensitive individuals also learned Action–Punisher contingencies. However, what they had learned was incorrect. Insensitive individuals formed incorrect beliefs about the causes of negative consequences so they could not withhold the specific action that caused punishment. This same bimodal punishment sensitivity driven by deficits in accurate instrumental contingency knowledge is observed in non-human animals [57], suggesting that it is a core property of learning and amenable to mechanistic deconstruction.
Lacking awareness or possessing erroneous causal beliefs about the adverse consequence of a behavior is not always problematic. In many individuals, lack of awareness or incorrect causal beliefs can be corrected to change behavior [59]. For example, explicit information about Action–Punisher contingencies changes the behavior and beliefs of some insensitive people, causing them to cease that behavior and avoid further punishment. However, lack of awareness or incorrect beliefs can sometimes be problematic. In some insensitive people, behavior resists counterevidence about why they are being punished, trapping them in a cycle of repeating negative consequences [59]. This is likely under at least one condition: when adverse consequences are infrequent [59]. Under this condition, some insensitive individuals discount veridical counterevidence about the causes of punishment and detrimental behavior persists [59].
So, insensitivity to adverse consequences can emerge from the different things that we learn about the negative consequences of our actions. Three features make the negative consequences of drug use especially prone to this insensitivity. First, the negative consequences of drug use are probabilistic, and any experienced contingencies are typically weak. The probability that any individual act of drug use will have detectable negative consequences for the individual is low. This makes learning about adverse consequences from experience difficult. We underweight rare, adverse events when making experience-based choices [55, 60]. Indeed, when individuals do experience adverse consequences from initial drug use (e.g., nausea in response to nicotine; flushing in response to ethanol), further use can be slowed [61,62,63,64]. Second, the trajectory of drug-related harms often involves escalation from minor to more severe, typically over many years. This trajectory undermines the ability of those consequences to change behavior. Severe negative consequences are less effective at changing behavior if they have been preceded by less severe negative consequences than if they had been experienced from the outset [65,66,67]. Third, the negative consequences of drug use are often temporally removed from the act of use. This delay between cause and effect further undermines learning [68, 69] and the capacity of negative outcomes to shape choices and behavior.
The brain mechanisms underlying this cognitive pathway are poorly understood. Core features are that valuation and action control can be intact but individuals differ in correct awareness of the consequences of their behavior as well as in their willingness to update beliefs in response to counterevidence. Progress in understanding may benefit from considering theoretical and computational advances in the mechanisms of belief updating [70,71,72,73] and their application to neuropsychiatric conditions [74,75,76]. This has identified key roles for dopamine [77] and a network of cortical regions involving dorsolateral prefrontal cortex and their interactions with medial prefrontal cortex [78, 79]. Interestingly, these mechanisms for belief updating depend on more than just the prediction error often studied in addiction neuroscience. For example, they depend on the meaningfulness of the new information being considered to the belief rather than on just how surprising or different from expectation that information is [78]. There is some evidence from laboratory animal studies that exposure to addictive drugs may alter these updating processes [76].
Given these pronounced individual differences in what we learn about the adverse consequences of behavior and in our willingness to change behavior in response to counterevidence, we argue that a cognitive pathway to persistent drug use despite potential negative consequences is more common than appreciated in the addiction neuroscience literature. Correctly recognizing the adverse consequences of one’s actions is more complex than simply experiencing or being educated about those consequences. Sustaining correct recognition may be equally difficult [75, 76]. These cognitive barriers must be overcome if negative consequences are to shape future choice and action.
Motivational pathways: valuing adverse consequences
If the negative consequences of drug use have been recognized and attributed, then a second pathway to persisting in drug taking despite adverse consequences can be linked to distortions in value-based choice [6, 80, 81] (Fig. 1). This has emerged from literature studying drug choice and economic demand [6, 41, 80, 82, 83] (see [6, 84, 85] for review). It shows that drug seeking and taking can be strongly linked to the relative value of the drug which, in turn, is determined by its relevance to the users’ current desires and needs. Drugs can be chosen when their expected benefits exceed those of other behaviors, and they exceed any expected costs. When controlled by expected value, drug use can be highly flexible, with individuals choosing to use despite negative consequences and choosing to abstain should there be sufficient incentive [1, 86, 87]. The evidence for this is compelling [6, 82, 88, 89]. It aligns with laboratory findings from smokers [90], opioid users [85, 91] and polydrug users [92] as well as with self-reports that cognitive appraisals and cost-benefit evaluations about use precede self- and treatment-guided behavior change [2,3,4, 49, 50]. It also aligns well with the evidence that cognitive re-evaluations of the ‘pros and cons’ of drug use are central to behavior change [93].
Pharmacotherapies designed to manage craving and withdrawal as well as treatments such as contingency management capitalize directly on this role of value to provide approaches effective for some people [94]. For example, in voucher-based reinforcement therapy, individuals earn vouchers and other incentives if they reach an agreed therapeutic goal. Success of these treatments is influenced by variables known to influence value computations, including voucher value and immediacy of voucher receipt [94].
Value is pleiotropic. So, distortions of value not only explain why an individual persists in drug-seeking despite adverse consequences but also why this persistence is expressed in other behaviors such as increased break points [16, 18,19,20, 28, 30, 33, 39, 40], increased responding during extinction [18, 21, 28, 39, 40] and increased economic demand [41, 42] in animal models, highlighting the need for such assessments when attempting to isolate causes of punishment insensitivity. Moreover, this pathway predicts that sensitivity or insensitivity to punishment depends on the experiences of the individual [66, 67, 95].
The importance of value in dictating choices to abstain or use underscores the need for deeper understanding of how negative and positive value are computed and used. One possibility is that excessive valuation is due to increased dopaminergic neurotransmission [96, 97]. To study this, Lüscher and colleagues developed an optical model of midbrain dopamine neuron self-stimulation. Here mice respond under simple [35] or seeking-taking [23] schedules for dopamine neuron excitation that also yield footshock punishment. Under these conditions some mice are insensitive to punishment. This insensitivity is due to increased excitability of orbitofrontal cortex neurons [35] and potentiation of orbitofrontal synapses in dorsal striatum [23, 98]. Remarkably, artificially sculpting plasticity in this orbitofrontal projection induced persistent seeking in punishment sensitive mice and reversed persistent seeking in punishment resistant mice [98]. Whether plasticity in this circuit adjusts response and/or outcome values remains unclear. Furthermore, the mechanisms for valuation are likely to be more complex still. Dopamine serves different roles in learning depending on its specific local and long-range circuit features [99,100,101]. This role is often value free [102, 103] and increasing dopamine neurotransmission has also been shown to increase, not decrease, punishment learning [104].
A second possibility is linked to the repeated cycles of instrumental incentive learning [105, 106] embedded in drug use. Here, individuals learn from experience that drug taking augments positive emotional states and/or ameliorates negative ones (boredom, social exclusion, depressed mood, drug withdrawal) [107,108,109,110]. This learning causes a revaluation of the drug, inflating its value and transforming it into a goal to be sought in future such states. For example, experiencing the alleviation of drug withdrawal by drug intake increases the incentive value of the drug in, and propensity to seek and take the drug during, future withdrawal states. This learning is outcome (i.e., drug) and state specific, so it can account for context-specific drug preferences and their reversal in different settings [111,112,113,114]. Incentive learning is well established for non-drug reinforcers [105, 115, 116]. However, evidence from drug reinforcers is sparse [117]. Understanding whether this incentive learning guides drug choices in the face of adverse consequences remains important, as does understanding how pharmacotherapies for withdrawal management affect this transformation and use of drug values.
The neurobiological mechanisms for these choices to seek and consume drugs despite negative consequences have attracted considerable attention. In addition to the mechanisms described above, insula cortex, basolateral amygdala and their interactions are essential to encoding internal states [118] and dynamic changes in reward and punishment value in humans, non-human primates, and rodents [106, 119,120,121,122,123,124,125]. Meta [126] and mega [127] analyses show alterations in human insula volume and/or gray matter thickness across dependence to several drugs [128], that could suggest potential alterations in punishment or reward encoding. This is supported by alterations in resting state functional connectivity of frontal and insular cortical regions in cocaine users [129].
Laboratory animal studies extend these findings. Propensity to seek alcohol [130, 131] or nicotine [132] after punishment or seek methamphetamine after voluntary (i.e., choice-induced) abstinence [133] is associated with increased activity in the anterior insula whereas choice-induced prevention of incubated craving for methamphetamine is linked to reduced anterior insula cortex activity [134]. Studies with non-drug rewards implicate insula projections to ventral striatum, particularly accumbens core, in retrieving and using outcome values in action selection [135, 136]. This pathway also mediates punishment resistant alcohol drinking [25]. However, other insula projections are relevant, including projections to the central amygdala. This projection mediates propensity to choose methamphetamine when alternative non-drug choices are removed [133]. Activity of amygdaloid PKCδ + neurons predicts punishment resistant alcohol drinking [33]. Reducing activity of these neurons reduces punished alcohol choice [33] and mediates the protective effect of non-drug choices on incubation of methamphetamine craving [134]. However, this circuitry is more complex still, with important roles for orbitofrontal cortex [137, 138]. Both lateral [139] and medial [140] orbitofrontal cortex are essential for learning about the adverse consequences of behavior. Studies with non-drug rewards show that distinct orbitofrontal cortical-amygdala projections in encoding (lateral orbitofrontal → basolateral amygdala) and retrieving (medial orbitofrontal → basolateral amygdala) reward value [138]. The role of these orbitofrontal cortical-amygdala interactions in choices to seek and take drugs despite negative consequences are important issues for the field to address.
Medial prefrontal cortex and its projections are also relevant. Medial prefrontal cortex is essential to value-based choice [141, 142] including cost-benefit decisions [143]. Medial prefrontal cortex shows structural alterations across dependence to several drugs [126, 127] and animal studies show that drug self-administration and exposure remodels [144] and reduces excitability [24, 145] as well as plasticity [16, 28] of prefrontal neurons. These circuits, especially those in the rodent prelimbic cortex and its projections to striatum and midbrain, are directly implicated in the choice of reward (sucrose, alcohol, cocaine) under punishment [16, 24, 28, 146,147,148]. Moreover, punishment resistant seeking has been linked to reductions in excitability of prelimbic neurons, while increasing activity in these prelimbic circuits can reduce choice of punished cocaine [148] and alcohol [24].
Choice is more than behavioral allocation. Process models such as sequential sampling models (e.g., drift-diffusion [149] and linear ballistic accumulator [150]) provide computationally tractable decomposition of choice into its latent cognitive processes [37, 151,152,153]. These models identify computational similarities [154] between human [151], non-human primate [151], and rodent [155] choice. They have parallels to circuit function [156,157,158,159,160], holding promise for achieving a formal understanding of how value is used when making drug choices [81, 161], complementing reinforcement learning models for learning this value [149, 162]. They may help identify how medications and interventions facilitate cognitive appraisal of the negative consequences of use that drive abstinence. Field et al. [80] have shown that these process models provide coherent explanations of drug choices as well as their remediation across recovery (see also [81]). This aligns with demonstrations that deliberative choice, including when evaluating the risk versus benefits of seeking rewards under punishment, is linked to medial prefrontal cortex [155, 163, 164] and its projections to thalamus [155, 165]. These findings are relevant to evidence that training deliberative choice of non-alcohol rewards over alcohol reduces rates of relapse to alcohol drinking in the high-risk period following inpatient discharge [166]. Process models also hold promise for understanding intra-individual variation in choice. Even with correct understanding of consequences, choices are not always optimal and preference is not always stable. Process models provide one way of understanding stochastic and probabilistic variation in choice including those based on fluctuations in value and cognitive control.
Behavioral pathways: responding to adverse consequences
If the negative consequences of drug use have been recognized, attributed, and valued, then a third pathway to persisting in drug taking despite adverse consequences is behavioral (Fig. 1) [37, 38, 167, 168]. Proposed and elaborated by Everitt, Robbins et al. (see [167, 169, 170] for review), this pathway is based on dichotomy of control by goal-directed versus habitual instrumental learning [171, 172] and their distinct neural circuit bases [173,174,175,176,177,178,179,180]. Across prolonged drug self-administration, there may be a transition from intentional control of value-based choice to Stimulus–Response control that is separate to any value of the drug to the users’ needs or desires. Such seeking is a relatively automatic response to antecedent environmental and behavioral stimuli [181].
Drug seeking as a habit may be autonomous but not necessarily insensitive to adverse consequences. Stimulus–Response associations are not immutable and they may be especially fragile [182]. For example in the laboratory, detection of behavioral autonomy depends on context [183] and number of behavioral choices [184], among other variables [185]. Thus, it is additionally assumed that a feature of drug seeking Stimulus–Response habits, and a characteristic that makes them resistant to their adverse consequences, is that they are divorced from the reinforcement mechanisms that would otherwise update them [167]. Under these conditions, drug seeking can be insensitive to any consequences, adverse or otherwise [167, 169].
The relevance of this pathway to the experiences and behavior of drug users has been questioned [6, 86, 87, 186]. This pathway may be the most difficult to study because it requires exclusion of the cognitive and motivational pathways [19, 29, 34, 43,44,45, 187]. Nonetheless, this pathway captures a core feature of human and other animal behavior [188]. Choices, including among cocaine [189] or alcohol [190] dependent individuals, can sometimes be independent of the current value of what is being chosen [171, 191, 192]. The behavioral pathway offers parsimonious explanation of examples of drug seeking in humans (e.g., absentminded relapse) [7, 193] that are reminiscent of the ‘slips of action’ observed in human laboratory choice tasks [190, 194, 195].
The brain mechanisms of this behavioral pathway are based on findings in humans and rodents identifying a change in control from ventral to dorsal and then from dorsomedial to dorsolateral striatum/putamen, as well as a reduction in “deliberative” medial prefrontal control, as behavior becomes more stimulus-bound [36,37,38, 167, 169, 194, 195]. They include, but are not limited to, demonstrations from laboratory animals that prolonged self-administration promotes dorsolateral striatal control of cocaine [196], alcohol [197,198,199,200], and heroin [201] seeking. Importantly, the control of choice by Stimulus–Response mechanisms in alcohol-dependent individuals is associated with increased putamen choice-related activity [190]. The cortical morphological and volumetric changes seen in drug dependence [127, 128] are obvious candidates for alterations in top-down control. Indeed, choice in alcohol-dependent individuals is associated with reductions in ventromedial prefrontal cortex activity [190].
Punishment-resistant drug seeking can depend on these striatal circuits. For example, Jonkman [202] showed that cocaine seeking under punishment, but not in the absence of punishment, was reduced by reversible inactivation of dorsolateral striatum. Giuliano et al. [187] extended this to show that persistent alcohol seeking despite punishment was predicted by the extent to which alcohol seeking depended on dopamine receptors in the dorsolateral striatum. Crucially, after rats had been identified as sensitive or insensitive to punishment, dorsolateral striatal dopamine receptor antagonism only reduced seeking in laboratory animals insensitive to punishment. Giuliano et al. could exclude differences in propensity to drink alcohol, differences in alcohol preference, and differences in alcohol self-administration as causal to this insensitivity. Persistence of alcohol-seeking in the face of punishment may be due to this failure to disengage dopamine-dependent signalling in the dorsolateral striatum. The mechanisms for this are poorly understood but these are important targets for pharmacotherapies due to their potential to facilitate value-based choice essential for cognitive appraisals of drug use. It is worth noting that a common role for dorsolateral striatal circuitry in punishment-resistant drug seeking and a role for this circuitry in autonomous Stimulus–Response associations does not show that such associations drive punishment resistance, but it does add some evidence for this behavioral pathway.
Alterations in endocannabinoid [203] and serotonin signalling (5-HT) may also be relevant. 5-HT has complex roles in behavioral control [204] that may contribute to insensitivity. Pelloux et al. [31] showed that rats insensitive to punishment of cocaine seeking under a seeking-taking schedule had reduced 5-HT turnover in prefrontal cortex and striatum. Insensitivity was alleviated by the selective serotonin-reuptake inhibitor citalopram [31]. This was linked to 5-HT actions at 5-HT2C receptors because 5-HT2C agonist mCPP counteracted insensitivity while 5-HT2C antagonist increased punished cocaine-seeking. Other 5-HT receptors have also been implicated. Lüscher and colleagues showed that 5-HT1B receptors on orbitofrontal cortical projections to dorsal striatum promote presynaptic depression of this projection and maintain sensitivity of cocaine taking to punishment in mice [205]. Projection-specific knock-out of these 5-HT1B receptors reduced the sensitivity of cocaine taking to punishment [205]. These findings suggest that upregulating 5-HT may assist in pharmacotherapy for drug use disorder, but evidence remains unclear [206].
Conclusions
The persistence of drug use despite negative consequences is complex. We have argued that this is not a unitary construct but rather that there are at least three pathways to this persistence—cognitive, motivational, and behavioral. These pathways are dissociable but they are neither mutually exclusive nor exhaustive. They may operate dynamically within the same individual at different times. They can also interact. For example, valuation (motivational pathway) depends on correctly recognizing actions and their consequences (cognitive pathway) but valuation also governs salience and detection of these consequences [207, 208]. Likewise, transient fluctuations in attention to action can influence relative contributions of the cognitive or behavioral pathways [183]. Crucially, these pathways occur against complex backgrounds of intoxication, individual histories of drug use, acute or protracted withdrawal, and acute as well as chronic stressors that can influence capacity to detect, appropriately learn about, weight, and ultimately respond to negative consequences.
Different pathways for persistent drug use despite adverse consequences align well with and may help reconcile findings that there are only partially overlapping brain circuitries for this persistence. We argue that understanding how insensitivity to adverse consequences arises has important implications not only for understanding the underlying brain mechanisms of this persistence but also for understanding how different pharmacotherapies and treatment strategies may act, possibly in complementary ways, to reduce this persistence and enhance sensitivity to adverse consequences.
Finally, different pathways for persistent drug use despite its adverse consequences align well with the fact that recovery from drug addiction is highly personalized. Choices to use or abstain from use of a drug are not immalleable. Individuals follow different pathways to self- or treatment-guided recovery—where the necessary appraisals of costs versus benefits of use are predicated upon being able to recognize those costs, evaluate their importance, and adjust behavior in response to them. Progress is neither linear nor always predictable. We argue that resolution of problematic behaviors will depend on which of these pathways is contributing at specific times to cause persistence of behavior. A better understanding of why behaviors persist despite adverse consequences, and a more thorough examination of these underlying pathways to insensitivity may help us understand these recoveries, improve understanding of the variation in efficacy of existing treatment strategies, as well as promote development of more effective individualized treatments.
Notes
We use the terms ‘punishment insensitivity’ and ‘persistence despite negative consequences’ in preference to the term ‘compulsivity’. The studies we review operationalize insensitivity to adverse consequences via punishment procedures and our focus is on how people and other animals may fail to detect, learn, and respond to these adverse consequences. The reader is referred to George et al. [5] for evaluation of use of the term ‘compulsivity’ in addiction neuroscience.
References
Pickard H, Ahmed SH. How do you know you have a drug problem? The role of knowledge of negative consequences in explaining drug choice in humans and rats. In: Heather N, Segal G, editors. Addiction and Choice. Oxford: Oxford University Press; 2016. p. 29–48.
Klingemann H, Sobell MB, Sobell LC. Continuities and changes in self-change research. Addiction. 2010;105:1510–8.
Klingemann H, Sobell LC. Promoting self-change from addictive behaviours: practical implications for policy, prevention, and treatment. New York: Springer; 2007.
Sobell LC, Sobell MB, Toneatto T, Leo GI. What Triggers the Resolution of Alcohol Problems Without Treatment. Alcohol: Clin Exp Res. 1993;17:217–34.
George O, Ahmed SH, Gilpin NW. Are we compulsively chasing rainbows? Neuropsychopharmacology. 2022;47:2013–5.
Hogarth L. Addiction is driven by excessive goal-directed drug choice under negative affect: translational critique of habit and compulsion theory. Neuropsychopharmacology. 2020;45:720–35.
Epstein DH. Let’s agree to agree: a comment on Hogarth (2020), with a plea for not-so-competing theories of addiction. Neuropsychopharmacology. 2020;45:715–6.
Babor TF, Caulkins J, Edwards G, Fischer B, Foxcroft DR, Humphreys K, et al. Drug policy and the public good. Oxford: Oxford Univerity Press; 2010.
Degenhardt L, Whiteford HA, Ferrari AJ, Baxter AJ, Charlson FJ, Hall WD, et al. Global burden of disease attributable to illicit drug use and dependence: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1564–74.
Degenhardt L, Hall W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet. 2012;379:55–70.
Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1575–86.
Global status report on alcohol and health 2018. In: Poznyak V, Rekve D, editors. Geneva: World Health Organisation; 2018.
Hasin DS, O’Brien CP, Auriacombe M, Borges G, Budney A, Compton WM, et al. DSM-5 criteria for substance use disorders: Recommendations and rationale. Am J Psychiatry. 2013;170:834–51.
Organization WH. International Classification of Diseases Eleventh Revision (ICD-11). Geneva: World Heath Organization; 2022.
Vanderschuren LJMJ, Minnaard AM, Smeets JA, Lesscher HM. Punishment models of addictive behavior. Curr Opin Behav Sci. 2017;13:77–84.
Kasanetz F, Lafourcade M, Deroche-Gamonet V, Revest J-M, Berson N, Balado E, et al. Prefrontal synaptic markers of cocaine addiction-like behavior in rats. Mol Psychiatry. 2013;18:729–37.
Belin D, Balado E, Piazza PV, Deroche-Gamonet V. Pattern of intake and drug craving predict the development of cocaine addiction-like behavior in rats. Biol Psychiatry. 2009;65:863–8.
Deroche-Gamonet V, Belin D, Piazza P-V. Evidence for addiction-like behavior in the rat. Science. 2004;305:1014–7.
Pelloux Y, Everitt BJ, Dickinson A. Compulsive drug seeking by rats under punishment: effects of drug taking history. Psychopharmacol (Berl). 2007;194:127–37.
Augier E, Barbier E, Dulman RS, Licheri V, Augier G, Domi E, et al. A molecular mechanism for choosing alcohol over an alternative reward. Science. 2018;360:1321–6.
Vanderschuren LJMJ, Everitt BJ. Drug Seeking Becomes Compulsive After Prolonged Cocaine Self-Administration. Science. 2004;305:1017–9.
Limpens JH, Schut EH, Voorn P, Vanderschuren LJ. Using conditioned suppression to investigate compulsive drug seeking in rats. Drug Alcohol Depend. 2014;142:314–24.
Harada M, Pascoli V, Hiver A, Flakowski J, Lüscher C. Cortico-striatal activity driving compulsive reward-seeking. Biol Psychiatry. 2021;90:808–18.
Siciliano CA, Naomany H, Chang C-J, Brown AR, Chen X, Leible D, et al. A cortical-brainstem circuit predicts and governs compulsive alcohol drinking. Science. 2019;366:1008–12.
Seif T, Chang S-J, Simms JA, Gibb SL, Dadgar J, Chen BT, et al. Cortical activation of accumbens hyperpolarization-active NMDARs mediates aversion-resistant alcohol intake. Nat Neurosci. 2013;16:1094–1100.
Jean-Richard-Dit-Bressel P, Killcross S, McNally GP. Behavioral and neurobiological mechanisms of punishment: implications for psychiatric disorders. Neuropsychopharmacology. 2018;43:1639–50.
Ahmed SH. The science of making drug-addicted animals. Neuroscience. 2012;211:107–25.
Kasanetz F, Deroche-Gamonet V, Berson N, Balado E, Lafourcade M, Manzoni O, et al. Transition to addiction is associated with a persistent impairment in synaptic plasticity. Sci (N. Y, NY). 2010;328:1709–12.
Belin D, Mar AC, Dalley JW, Robbins TW, Everitt BJ. High Impulsivity Predicts the Switch to Compulsive Cocaine-Taking. Science. 2008;320:1352–5.
Pelloux Y, Murray JE, Everitt BJ. Differential vulnerability to the punishment of cocaine related behaviours: effects of locus of punishment, cocaine taking history and alternative reinforcer availability. Psychopharmacol (Berl). 2015;232:125–34.
Pelloux Y, Dilleen R, Economidou D, Theobald D, Everitt BJ. Reduced Forebrain Serotonin Transmission is Causally Involved in the Development of Compulsive Cocaine Seeking in Rats. Neuropsychopharmacology. 2012;37:2505–14.
Blackwood CA, McCoy MT, Ladenheim B, Cadet JL. Escalated Oxycodone Self-Administration and Punishment: Differential Expression of Opioid Receptors and Immediate Early Genes in the Rat Dorsal Striatum and Prefrontal Cortex. Front Neurosci. 2019;13:1392.
Domi E, Xu L, Toivainen S, Nordeman A, Gobbo F, Venniro M, et al. A neural substrate of compulsive alcohol use. Sci Adv. 2021;7:eabg9045.
Giuliano C, Pena-Oliver Y, Goodlett CR, Cardinal RN, Robbins TW, Bullmore ET, et al. Evidence for a Long-Lasting Compulsive Alcohol Seeking Phenotype in Rats. Neuropsychopharmacology. 2018;43:728–38.
Pascoli V, Terrier J, Hiver A, Luscher C. Sufficiency of Mesolimbic Dopamine. Neuron Stimul Prog Addict Neuron. 2015;88:1054–66.
Everitt BJ, Robbins TW. From the ventral to the dorsal striatum: devolving views of their roles in drug addiction. Neurosci Biobehav Rev. 2013;9:1946–54.
Dalley JW, Everitt BJ, Robbins TW. Impulsivity, compulsivity, and top-down cognitive control. Neuron. 2011;69:680–94.
Everitt BJ, Belin D, Economidou D, Pelloux Y, Dalley JW, Robbins TW. Review. Neural mechanisms underlying the vulnerability to develop compulsive drug-seeking habits and addiction. Philos Trans R Soc Lond: Ser B, Biol Sci. 2008;363:3125–35.
Belin D, Berson N, Balado E, Piazza PV, Deroche-Gamonet V. High-novelty-preference rats are predisposed to compulsive cocaine self-administration. Neuropsychopharmacology. 2011;36:569–79.
Singer BF, Fadanelli M, Kawa AB, Robinson TE. Are Cocaine-Seeking “Habits” Necessary for the Development of Addiction-Like Behavior in Rats? J Neurosci. 2018;38:60–73.
Bentzley BS, Jhou TC, Aston-Jones G. Economic demand predicts addiction-like behavior and therapeutic efficacy of oxytocin in the rat. Proc Natl Acad Sci USA. 2014;111:11822–7.
James MH, Bowrey HE, Stopper CM, Aston-Jones G. Demand elasticity predicts addiction endophenotypes and the therapeutic efficacy of an orexin/hypocretin-1 receptor antagonist in rats. Eur J Neurosci. 2019;50:2602–12.
Datta U, Martini M, Sun W. Different functional domains measured by cocaine self-administration under the progressive-ratio and punishment schedules in male Wistar rats. Psychopharmacol (Berl). 2018;235:897–907.
Datta U, Martini M, Fan M, Sun W. Compulsive sucrose- and cocaine-seeking behaviors in male and female Wistar rats. Psychopharmacol (Berl). 2018;235:2395–405.
Jonkman S, Pelloux Y, Everitt BJ. Drug Intake is Sufficient, but Conditioning is not Necessary for the Emergence of Compulsive Cocaine Seeking After Extended Self-Administration. Neuropsychopharmacology. 2012;37:1612–9.
Smith KE. Disease and decision. J Subst Abuse Treat. 2022;142:108874.
DiClemente CC, Bellino LE, Neavins TM. Motivation for change and alcoholism treatment. Alcohol Res Health. 1999;23:86–92.
Ryan RM, Plant RW, O’Malley S. Initial motivations for alcohol treatment: Relations with patient characteristics, treatment involvement, and dropout. Addict Behav. 1995;20:279–97.
Ebaugh HRF. Becoming an Ex. Chicago: University of Chicago Press;1988.
Heyman GM, Mims V. What addicts can teach us about addiction: a natural history approach. In: Heather N, Segal G, editors. Addiction and choice: Rethinking the relationship. Oxford, UK: Oxford University Press; 2017. p. 385–408.
Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. J Consult Clin Psychol. 2003;71:843–61.
Lubman DI, Grigg J, Reynolds J, Hall K, Baker AL, Staiger PK, et al. Effectiveness of a Stand-alone Telephone-Delivered Intervention for Reducing Problem Alcohol Use: A Randomized Clinical Trial. JAMA Psychiatry. 2022;79:1055–64.
Hettema J, Steele J, Engleman EA, Miller WR. Motivational Interviewing. Annu Rev Clin Psychol. 2005;1:91–111.
Jean-Richard-Dit-Bressel P, Lee JC, Liew SX, Weidemann G, Lovibond PF, McNally GP. Punishment insensitivity in humans is due to failures in instrumental contingency learning. Elife. 2021;10:e69594.
Hertwig R, Erev I. The description-experience gap in risky choice. Trends Cogn Sci. 2009;13:517–23.
Carver CS, White TL. Behavioral inhibition, behavioral activation, and the affective responses to impending reward and punishment: The BIS/BAS scales. J Personal Soc Psychol. 1994;67:319–33.
Jean-Richard-Dit-Bressel P, Ma C, Bradfield LA, Killcross S, McNally GP. Punishment insensitivity emerges from impaired contingency detection, not aversion insensitivity or reward dominance. Elife. 2019;8:e52765.
Marchant NJ, Campbell EJ, Kaganovsky K. Punishment of alcohol-reinforced responding in alcohol preferring P rats reveals a bimodal population: Implications for models of compulsive drug seeking. Prog Neuro-Psychopharmacol Biol Psychiatry. 2017;87:68–77.
Jean Richard Dit Bressel P, Lee JC, Liew SX, Weidemann G, Lovibond PF, McNally GP. A cognitive pathway to punishment insensitivity. PsyArXiv; 2023. https://doi.org/10.31234/osf.io/qw534.
Newell BR, Shanks DR, Lagnado L. Straight Choices: The Psychology of Decision Making. Oxfordshire: Psychology Press; 2007.
Richardson CG, Okoli CT, Ratner PA, Johnson JL. Empirical support for a multi-dimensional model of sensations experienced by youth during their initial smoking episodes. Addiction. 2010;105:1827–34.
Acosta MC, Eissenberg T, Nichter M, Nichter M, Balster RL. Characterizing early cigarette use episodes in novice smokers. Addict Behav. 2008;33:106–21.
Perkins KA, Lerman C, Coddington S, Jetton C, Karelitz JL, Wilson A, et al. Gene and gene by sex associations with initial sensitivity to nicotine in nonsmokers. Behav Pharmacol. 2008;19:630–40.
de Wit H, Phillips TJ. Do initial responses to drugs predict future use or abuse? Neurosci Biobehav Rev. 2012;36:1565–76.
Jean Richard Dit Bressel P, McNally GP. Punishment and compulsion: more than meets the eye. Neuropsychopharmacology. 2021;47:425–6.
Miller NE. Learning resistance to pain and fear: Effects of overlearning, exposure, and rewarded exposure in context. J Exp Psychol. 1960;60:137–45.
Church RM. Repsonse suppression. In: Campbell BA, Church RM, editors. Punishment and aversive behavior. New York, NY: Appleton-Century-Crofts;1969.
Kamin LJ. The delay of punishment gradient. J Comp Physiol Psychol. 1959;52:434–7.
Liley AE, Gabriel DBK, Sable HJ, Simon NW. Sex Differences and Effects of Predictive Cues on Delayed Punishment Discounting. eNeuro. 2019;6:ENEURO.0225-19.2019
Scheffer M, Borsboom D, Nieuwenhuis S, Westley F. Belief traps: Tackling the inertia of harmful beliefs. Proc Natl Acad Sci USA. 2022;119:e2203149119.
Galesic M, Olsson H, Dalege J, van der Does T, Stein DL. Integrating social and cognitive aspects of belief dynamics: towards a unifying framework. J R Soc: Interfac. 2021;18:20200857.
Garrett N, Daw ND. Biased belief updating and suboptimal choice in foraging decisions. Nat Commun. 2020;11:3417.
Harris C, Fiedler K, Marien H, Custers R. Biased preferences through exploitation: How initial biases are consolidated in reward-rich environments. J Exp Psychol: Gen. 2020;149:1855–77.
Sheffield JM, Suthaharan P, Leptourgos P, Corlett PR. Belief Updating and Paranoia in Individuals With Schizophrenia. Biol Psychiatry Cogn Neurosci Neuroimaging. 2022;7:1149–57.
Corlett PR, Fletcher P. Modelling delusions as temporally-evolving beliefs. Cogn Neuropsychiatry. 2021;26:231–41.
Reed EJ, Uddenberg S, Suthaharan P, Mathys CD, Taylor JR, Groman SM, et al. Paranoia as a deficit in non-social belief updating. Elife. 2020;9:e56345.
Nour MM, Dahoun T, Schwartenbeck P, Adams RA, FitzGerald THB, Coello C, et al. Dopaminergic basis for signaling belief updates, but not surprise, and the link to paranoia. Proc Natl Acad Sci USA. 2018;115:E10167–E10176.
Kobayashi K, Hsu M. Neural Mechanisms of Updating under Reducible and Irreducible Uncertainty. J Neurosci. 2017;37:6972–82.
Tomov MS, Dorfman HM, Gershman SJ. Neural Computations Underlying Causal Structure Learning. J Neurosci. 2018;38:7143–57.
Field M, Heather N, Murphy JG, Stafford T, Tucker JA, Witkiewitz K. Recovery from addiction: Behavioral economics and value-based decision making. Psychol Addict Behav. 2020;34:182–93.
Redish AD, Jensen S, Johnson A. A unified framework for addiction: vulnerabilities in the decision process. Behav Brain Sci. 2008;31:415–37.
Hogarth L, Field M. Relative expected value of drugs versus competing rewards underpins vulnerability to and recovery from addiction. Behav Brain Res. 2020;394:112815.
Bentzley BS, Fender KM, Aston-Jones G. The behavioral economics of drug self-administration: a review and new analytical approach for within-session procedures. Psychopharmacol (Berl). 2013;226:113–25.
Bickel WK, Mellis AM, Snider SE, Athamneh LN, Stein JS, Pope DA. 21st century neurobehavioral theories of decision making in addiction: Review and evaluation. Pharm Biochem Behav. 2018;164:4–21.
Bickel WK, Marsch LA. Toward a behavioral economic understanding of drug dependence: delay discounting processes. Addiction. 2001;96:73–86.
Heather N. Is the concept of compulsion useful in the explanation or description of addictive behaviour and experience? Addict Behav Rep. 2017;6:15–38.
Heather N, Segal G. Addiction and Choice. Oxford: Oxford University Press; 2016.
Hogarth L, Hardy L. Depressive statements prime goal-directed alcohol-seeking in individuals who report drinking to cope with negative affect. Psychopharmacol (Berl). 2018;235:269–79.
Hogarth L, He Z, Chase HW, Wills AJ, Troisi J 2nd, Leventhal AM, et al. Negative mood reverses devaluation of goal-directed drug-seeking favouring an incentive learning account of drug dependence. Psychopharmacol (Berl). 2015;232:3235–47.
Field M, Santarcangelo M, Sumnall H, Goudie A, Cole J. Delay discounting and the behavioural economics of cigarette purchases in smokers: the effects of nicotine deprivation. Psychopharmacol (Berl). 2006;186:255–63.
Jacobs EA, Bickel WK. Modeling drug consumption in the clinic using simulation procedures: Demand for heroin and cigarettes in opioid-dependent outpatients. Exp Clin Psychopharmacol. 1999;7:412–26.
Sumnall HR, Tyler E, Wagstaff GF, Cole JC. A behavioural economic analysis of alcohol, amphetamine, cocaine and ecstasy purchases by polysubstance misusers. Drug Alcohol Depend. 2004;76:93–9.
Sobell LC, Ellingstad TP, Sobell MB. Natural recovery from alcohol and drug problems: methodological review of the research with suggestions for future directions. Addiction. 2000;95:749–64.
Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2006;101:192–203.
Durand A, Girardeau P, Freese L, Ahmed SH. Increased responsiveness to punishment of cocaine self-administration after experience with high punishment. Neuropsychopharmacology. 2021;47:444–53.
Robinson TE, Berridge KC. Addiction. Annu Rev Psychol. 2003;54:25–53.
Robinson TE, Berridge KC. The neural basis of drug addiction: an incentive-sensitization theory of addiction. Brain Res Rev. 1993;18:247–91.
Pascoli V, Hiver A, Van Zessen R, Loureiro M, Achargui R, Harada M, et al. Stochastic synaptic plasticity underlying compulsion in a model of addiction. Nature. 2018;564:366–71.
de Jong JW, Afjei SA, Pollak Dorocic I, Peck JR, Liu C, Kim CK, et al. A Neural Circuit Mechanism for Encoding Aversive Stimuli in the Mesolimbic Dopamine System. Neuron. 2019;101:133–51.e137.
Lammel S, Lim BK, Ran C, Huang KW, Betley MJ, Tye KM, et al. Input-specific control of reward and aversion in the ventral tegmental area. Nature. 2012;491:212–7.
Lammel S, Ion DI, Roeper J, Malenka RC. Projection-specific modulation of dopamine neuron synapses by aversive and rewarding stimuli. Neuron. 2011;70:855–62.
Sharpe MJ, Schoenbaum G. Evaluation of the hypothesis that phasic dopamine constitutes a cached-value signal. Neurobiol Learn Mem. 2018;153:131–6.
Langdon AJ, Sharpe MJ, Schoenbaum G, Niv Y. Model-based predictions for dopamine. Curr Opin Neurobiol. 2017;49:1–7.
Killcross AS, Everitt BJ, Robbins TW. Symmetrical effects of amphetamine and alpha-flupenthixol on conditioned punishment and conditioned reinforcement: contrasts with midazolam. Psychopharmacology. 1997;129:141–52.
Dickinson A, Balleine BW. The role of learning in the operation of motivational systems. In: Pashler H, Gallistel CR, editors. vol. 34B. Hoboken, NJ, USA: Wiley Online Library; 2002. p. 497–533.
Balleine BW, Dickinson A. Goal-directed instrumental action: contingency and incentive learning and their cortical substrates. Neuropharmacology. 1998;37:407–19.
Koob GF, Mason BJ. Existing and Future Drugs for the Treatment of the Dark Side of Addiction. Annu Rev Pharmacol Toxicol. 2016;56:299–322.
Koob GF. The dark side of emotion: the addiction perspective. Eur J Pharmacol. 2015;753:73–87.
Koob GF. Negative reinforcement in drug addiction: the darkness within. Curr Opin Neurobiol. 2013;23:559–63.
Koob GF, Powelll P, White A. Addiction as a coping response: Hyperkatifeia, deaths of despair, and COVID-19. Am J Psychiatry. 2020;177:1031–7.
Ahmed SH, Badiani A, Miczek KA, Muller CP. Non-pharmacological factors that determine drug use and addiction. Neurosci Biobehav Rev. 2020;110:3–27.
Badiani A, Belin D, Epstein DH, Calu DJ, Shaham Y. Opiate versus psychostimulant addiction: the differences do matter. Nat Rev Neurosci. 2011;12:685–700.
De Luca MT, Montanari C, Meringolo M, Contu L, Celentano M, Badiani A. Heroin versus cocaine: opposite choice as a function of context but not of drug history in the rat. Psychopharmacol (Berl). 2019;236:787–98.
De Pirro S, Galati G, Pizzamiglio L, Badiani A. The Affective and Neural Correlates of Heroin versus Cocaine Use in Addiction Are Influenced by Environmental Setting But in Opposite Directions. J Neurosci. 2018;38:5182–95.
Dickinson A, Balleine B. Motivational control of goal-directed action. Anim Learn Behav. 1994;22:1–18.
Balleine B. Instrumental Performance Following a Shift in Primary Motivation Depends on Incentive Learning. J Exp Psychol. 1992;18:236–50.
Hutcheson DM, Everitt BJ, Robbins TW, Dickinson A. The role of withdrawal in heroin addiction: enhances reward or promotes avoidance? Nat Neurosci. 2001;4:943–7.
Craig AD. How do you feel? Interoception: the sense of the physiological condition of the body. Nat Rev Neurosci. 2002;3:665–6.
Parkes SL, Balleine BW. Incentive Memory: Evidence the Basolateral Amygdala Encodes and the Insular Cortex Retrieves Outcome Values to Guide Choice between Goal-Directed Actions. J Neurosci. 2013;33:8753–63.
Balleine BW. Killcross aS, Dickinson A. The effect of lesions of the basolateral amygdala on instrumental conditioning. J Neurosci: Off J Soc Neurosci. 2003;23:666–75.
Yang YP, Li X, Stuphorn V. Primate anterior insular cortex represents economic decision variables proposed by prospect theory. Nat Commun. 2022;13:717.
Jean-Richard-dit-Bressel P, Tran J, Didachos A, McNally GP. Instrumental aversion coding in the basolateral amygdala and its reversion by a benzodiazepine. Neuropsychopharmacology. 2021;47:1199–209.
Liu X, Hairston J, Schrier M, Fan J. Common and distinct networks underlying reward valence and processing stages: a meta-analysis of functional neuroimaging studies. Neurosci Biobehav Rev. 2011;35:1219–36.
Von Siebenthal Z, Boucher O, Lazzouni L, Taylor V, Martinu K, Roy M, et al. Expected value and sensitivity to punishment modulate insular cortex activity during risky decision making. Sci Rep. 2020;10:11920.
Piantadosi PT, Yeates DCM, Wilkins M, Floresco SB. Contributions of basolateral amygdala and nucleus accumbens subregions to mediating motivational conflict during punished reward-seeking. Neurobiol Learn Mem. 2017;140:92–105.
Ersche KD, Williams GB, Robbins TW, Bullmore ET. Meta-analysis of structural brain abnormalities associated with stimulant drug dependence and neuroimaging of addiction vulnerability and resilience. Curr Opin Neurobiol. 2013;23:615–24.
Mackey S, Allgaier N, Chaarani B, Spechler P, Orr C, Bunn J, et al. Mega-analysis of gray matter volume in substance dependence: General and substance-specific regional effects. Am J Psychiatry. 2018;176:119–28.
Campbell EJ, Lawrence AJ. It’s more than just interoception: The insular cortex involvement in alcohol use disorder. J Neurochem. 2021;157:1644–51.
Hu Y, Salmeron BJ, Gu H, Stein EA, Yang Y. Impaired functional connectivity within and between frontostriatal circuits and its association with compulsive drug use and trait impulsivity in cocaine addiction. JAMA Psychiatry. 2015;72:584–92.
Campbell EJ, Flanagan JPM, Walker LC, Hill M, Marchant NJ, Lawrence AJ. Anterior Insular Cortex is Critical for the Propensity to Relapse Following Punishment-Imposed Abstinence of Alcohol Seeking. J Neurosci. 2019;39:1077–87.
Chen H, Lasek AW. Perineuronal nets in the insula regulate aversion-resistant alcohol drinking. Addict Biol. 2020;25:e12821.
Ghareh H, Alonso-Lozares I, Schetters D, Herman RJ, Heistek TS, Van Mourik Y, et al. Role of anterior insula cortex in context-induced relapse of nicotine-seeking. Elife. 2022;11:e75609.
Venniro M, Caprioli D, Zhang M, Whitaker LR, Zhang S, Warren BL, et al. The Anterior Insular Cortex->Central Amygdala Glutamatergic Pathway Is Critical to Relapse after Contingency Management. Neuron. 2017;96:414–27.e418.
Venniro M, Zhang M, Caprioli D, Hoots JK, Golden SA, Heins C, et al. Volitional social interaction prevents drug addiction in rat models. Nat Neurosci. 2018;21:1520–9.
Parkes SL, Bradfield LA, Balleine BW. Interaction of insular cortex and ventral striatum mediates the effect of incentive memory on choice between goal-directed actions. J Neurosci. 2015;35:6464–71.
Tang H, Costa VD, Bartolo R, Averbeck BB. Differential coding of goals and actions in ventral and dorsal corticostriatal circuits during goal-directed behavior. Cell Rep. 2022;38:110198.
Baltz ET, Yalcinbas EA, Renteria R, Gremel CM. Orbital frontal cortex updates state-induced value change for decision-making. Elife. 2018;7:e35988.
Malvaez M, Shieh C, Murphy MD, Greenfield VY, Wassum KM. Distinct cortical–amygdala projections drive reward value encoding and retrieval. Nat Neurosci. 2019;22:762–9.
Jean-Richard Dit Bressel P, McNally GP. Lateral, not medial, prefrontal cortex contributes to punishment and aversive instrumental learning. Learn Mem. 2016;23:607–17.
Ma C, Jean-Richard-Dit-Bressel P, Roughley S, Vissel B, Balleine BW, Killcross S, et al. Medial Orbitofrontal Cortex Regulates Instrumental Conditioned Punishment, but not Pavlovian Conditioned Fear. Cereb Cortex Commun. 2020;1:tgaa039.
Glimcher PW. Value-Based Decision Making. In: Glimcher PW, Fehr E, editors. Neuroeconomics. Amsterdam: Elsevier; 2014. p. 373–91.
Levy DJ, Glimcher PW. The root of all value: a neural common currency for choice. Curr Opin Neurobiol. 2012;22:1027–38.
Wallis JD, Rushworth MFS. Integrating Benefits and Costs in Decision Making. In: Glimcher PW, Fehr E, editors. Neuroeconomics. Amsterdam: Elsevier; 2014. p. 411–33.
Holmes A, Fitzgerald PJ, MacPherson KP, DeBrouse L, Colacicco G, Flynn SM, et al. Chronic alcohol remodels prefrontal neurons and disrupts NMDAR-mediated fear extinction encoding. Nat Neurosci. 2012;15:1359–61.
Pleil KE, Lowery-Gionta EG, Crowley NA, Li C, Marcinkiewcz CA, Rose JH, et al. Effects of chronic ethanol exposure on neuronal function in the prefrontal cortex and extended amygdala. Neuropharmacology. 2015;99:735–49.
Verharen JPH, den Ouden HEM, Adan RAH, Vanderschuren L. Modulation of value-based decision making behavior by subregions of the rat prefrontal cortex. Psychopharmacol (Berl). 2020;237:1267–80.
Verharen JPH, van den Heuvel MW, Luijendijk M, Vanderschuren L, Adan RAH. Corticolimbic Mechanisms of Behavioral Inhibition under Threat of Punishment. J Neurosci. 2019;39:4353–64.
Chen BT, Yau H-J, Hatch C, Kusumoto-Yoshida I, Cho SL, Hopf FW, et al. Rescuing cocaine-induced prefrontal cortex hypoactivity prevents compulsive cocaine seeking. Nature. 2013;496:359–62.
Pedersen ML, Frank MJ, Biele G. The drift diffusion model as the choice rule in reinforcement learning. Psychonomic Bull Rev. 2017;24:1234–51.
Brown SD, Heathcote A. The simplest complete model of choice response time: linear ballistic accumulation. Cogn Psychol. 2008;57:153–78.
Forstmann BU, Ratcliff R, Wagenmakers EJ. Sequential Sampling Models in Cognitive Neuroscience: Advantages, Applications, and Extensions. Annu Rev Psychol. 2016;67:641–66.
Johnson EJ, Ratcliff R. Computational and process models of decision making in psychology and behavioral economics. In: Glimcher PW, Fehr E, editors. Neuroeconomics: Decision making and the brain. Amsterdam: Elseovier; 2018. p. 35–47.
Ratcliff R, Smith PL, Brown SD, McKoon G. Diffusion Decision Model: Current Issues and History. Trends Cogn Sci. 2016;20:260–81.
Redish AD, Kepecs A, Anderson LM, Calvin OL, Grissom NM, Haynos AF, et al. Computational validity: using computation to translate behaviours across species. Philos Trans R Soc Lond: B: Biol Sci. 2022;377:20200525.
Choi EA, Husic M, Millan EZ, Gilchrist S, Power JM, Jean Richard Dit Bressel P, et al. A corticothalamic circuit trades off speed for safety during decision-making under motivational conflict. J Neurosci. 2022;42:3473–83.
Gold JI, Shadlen MN. Banburismus and the brain: Decoding the relationships between sensory stimuli, decisions, and reward. Neuron. 2002;36:299–308.
Hanks T, Kiani R, Shadlen MN. A neural mechanism of speed-accuracy tradeoff in macaque area LIP. eLife. 2014;3:e02260.
Gold JI, Shadlen MN. The neural basis of decision making. Annu Rev Neurosci. 2007;30:535–74.
Shadlen MN, Newsome RN. Neural basis of a perceptual decision in the parietal cortex (Area LIP) of the Rhesus monkey. J Neurophsyiol. 2001;86:1916–36.
Shadlen MN, Newsome RT. Motion perception: Seeing and deciding. Proc Natl Acad Sci USA. 1996;93:628–33.
Sebold M, Nebe S, Garbusow M, Guggenmos M, Schad DJ, Beck A, et al. When Habits Are Dangerous: Alcohol Expectancies and Habitual Decision Making Predict Relapse in Alcohol Dependence. Biol Psychiatry. 2017;82:847–56.
Ratcliff R, Frank MJ. Reinforcement-based decision making in corticostriatal circuits: Mututal constraints by neurocomputational and diffusion models. Neural Comput. 2012;24:1186–229.
Botvinick M, Braver T. Motivation and cognitive control: from behavior to neural mechanism. Annu Rev Psychol. 2015;66:83–113.
Botvinick M, Braver T, Barch DM, Carter CS, Cohen JD. Conflict monitoring and cognitive control. Psychol Rev. 2001;108:624–52.
Campus P, Covelo IR, Kim Y, Parsegian A, Kuhn BN, Lopez SA, et al. The paraventricular thalamus is a critical mediator of top-down control of cue-motivated behavior in rats. eLife. 2019;8:e49041.
Manning V, Garfield JBB, Staiger PK, Lubman DI, Lum JAG, Reynolds J, et al. Effect of cognitive bias modification on early relapse among adults undergoing inpatient alcohol withdrawal treatment: A randomized clinical trial. JAMA Psychiatry. 2021;78:133–40.
Everitt BJ, Robbins TW. Drug Addiction: Updating Actions to Habits to Compulsions Ten Years On. Annu Rev Psychol. 2016;67:23–50.
Belin D, Belin-Rauscent A, Murray JE, Everitt BJ. Addiction: failure of control over maladaptive incentive habits. Curr Opin Neurobiol. 2013;23:564–72.
Luscher C, Robbins TW, Everitt BJ. The transition to compulsion in addiction. Nat Rev Neurosci. 2020;21:247–63.
Everitt BJ. Neural and psychological mechanisms underlying compulsive drug seeking habits and drug memories - indications for novel treatments of addiction. Eur J Neurosci. 2014;40:2163–82.
Adams C, Dickinson A. Actions and Habits: Variations in Associative Representations During Instrumental Learning. Inf Process Anim. 1982;Chapter 5:143–65.
Dickinson A. Actions and habits: the development of behavioural autonomy. Philos Trans R Soc Lond B: Biol Sci. 1985;308:67–78.
Balleine BW. The meaning of behavior: Discriminating reflex and volition in the brain. Neuron. 2019;104:47–62.
Hart G, Bradfield LA, Fok SY, Chieng B, Balleine BW. The Bilateral Prefronto-striatal Pathway Is Necessary for Learning New Goal-Directed Actions. Curr Biol. 2018;28:2218–29.e2217.
Bradfield LA, Balleine BW. Thalamic Control of Dorsomedial Striatum Regulates Internal State to Guide Goal-Directed Action Selection. J Neurosci. 2017;37:3721–33.
Corbit LH, Balleine BW. Learning and motivational processes contributing to Pavlovian-instrumental transfer and their neural bases: Dopamine and beyond. Curr Top Behav Neurosci. 2016;27:259–89.
Balleine BW, Morris RW, Leung BK. Thalamocortical integration of instrumental learning and performance and their disintegration in addiction. Brain Res. 2015;1628:104–16.
Hart G, Leung BK, Balleine BW. Dorsal and ventral streams: The distinct role of striatal subregions in the acquisition and performance of goal-directed actions. Neurobiol Learn Mem. 2014;108:104–18.
Balleine BW, O’Doherty JP. Human and rodent homologies in action control: corticostriatal determinants of goal-directed and habitual action. Neuropsychopharmacology. 2010;35:48–69.
Balleine BW, Liljeholm M, Ostlund SB. The integrative function of the basal ganglia in instrumental conditioning. Behav Brain Res. 2009;199:43–52.
Dickinson A, Wood N, Janice W. Alcohol seeking by rats: Action or habit? Q J Exp Psychol. 2002;55B:331–48.
de Wit S, Kindt M, Knot SL, Verhoeven AAC, Robbins TW, Gasull-Camos J, et al. Shifting the balance between goals and habits: Five failures in experimental habit induction. J Exp Psychol: Gen. 2018;147:1043–65.
Bouton ME. Context, attention, and the switch between habit and goal-direction in behavior. Learn Behav. 2021;49:349–62.
Kosaki Y, Dickinson A. Choice and contingency in the development of behavioral autonomy during instrumental conditioning. J Exp Psychol: Anim Behav Proc. 2010;36:334–42.
Perez OD, Dickinson A. A theory of actions and habits: The interaction of rate correlation and contiguity systems in free-operant behavior. Psychol Rev. 2020;127:945–71.
Hogarth L, Lam-Cassettari C, Pacitti H, Currah T, Mahlberg J, Hartley L, et al. Intact goal-directed control in treatment-seeking drug users indexed by outcome-devaluation and Pavlovian to instrumental transfer: critique of habit theory. Eur J Neurosci. 2019;50:2513–25.
Giuliano C, Belin D, Everitt BJ. Compulsive Alcohol Seeking Results from a Failure to Disengage Dorsolateral Striatal Control over Behavior. J Neurosci. 2019;39:1744–54.
Robbins TW, Costa RM. Habits. Curr Biol. 2017;27:R1200–R1206.
Ersche KD, Gillan CM, Jones S, Williams GB, Ward LHE, Luitjen M, et al. Carrots and sticks fail to change behavior in cocaine addiction. Science. 2016;352:1468–71.
Sjoerds Z, de Wit S, van den Brink W, Robbins TW, Beekman AT, Penninx BW, et al. Behavioral and neuroimaging evidence for overreliance on habit learning in alcohol-dependent patients. Transl Psychiatry. 2013;3:e337.
Colwill RM, Rescorla RA. Postconditioning devaluation of a reinforcer affects instrumental responding. J Exp Psychol: Anim Behav Proc. 1985;11:120–32.
de Wit S, Niry D, Wariyar R, Aitken MR, Dickinson A. Stimulus-outcome interactions during instrumental discrimination learning by rats and humans. J Exp Psychol: Anim Behav Proc. 2007;33:1–11.
Catley D, O’Connell KA, Shiffman S. Absentminded lapses during smoking cessation. Psychol Addict Behav. 2000;14:73–6.
Watson P, van Wingen G, de Wit S. Conflicted between Goal-Directed and Habitual Control, an fMRI Investigation. eNeuro. 2018;5:ENEURO.0240-18.2018.
de Wit S, Watson P, Harsay HA, Cohen MX, van de Vijver I, Ridderinkhof KR. Corticostriatal connectivity underlies individual differences in the balance between habitual and goal-directed action control. J Neurosci. 2012;32:12066–75.
Belin D, Everitt BJ. Cocaine seeking habits depend upon dopamine-dependent serial connectivity linking the ventral with the dorsal striatum. Neuron. 2008;57:432–41.
Corbit LH, Nie H, Janak PH. Habitual Alcohol Seeking: Time Course and the Contribution of Subregions of the Dorsal Striatum. Biol Psychiatry. 2012;72:389–95.
Spoelder M, Hesseling P, Styles M, Baars AM. Lozeman-van ‘t Klooster JG, Lesscher HM et al. Dopaminergic neurotransmission in ventral and dorsal striatum differentially modulates alcohol reinforcement. Eur J Neurosci. 2017;45:147–58.
Walker LC, Berizzi AE, Chen NA, Rueda P, Perreau VM, Huckstep K, et al. Acetylcholine Muscarinic M4 Receptors as a Therapeutic Target for Alcohol Use Disorder: Converging Evidence From Humans and Rodents. Biol Psychiatry. 2020;88:898–909.
Berizzi AE, Perry CJ, Shackleford DM, Lindsley CW, Jones CK, Chen NA, et al. Muscarinic M5 receptors modulate ethanol seeking in rats. Neuropsychopharmacology. 2018;43:1510–7.
Hodebourg R, Murray JE, Fouyssac M, Puaud M, Everitt BJ, Belin D. Heroin seeking becomes dependent on dorsal striatal dopaminergic mechanisms and can be decreased by N-acetylcysteine. Eur J Neurosci. 2019;50:2036–44.
Jonkman S, Pelloux Y, Everitt BJ. Differential roles of the dorsolateral and midlateral striatum in punished cocaine seeking. J Neurosci. 2012;32:4645–50.
Gremel CM, Chancey JH, Atwood BK, Luo G, Neve R, Ramakrishnan C, et al. Endocannabinoid Modulation of Orbitostriatal Circuits Gates Habit Formation. Neuron. 2016;90:1312–24.
Dayan P, Huys Q. Serotonin’s many meanings elude simple theories. eLife. 2015;4:463–463.
Li Y, Simmler LD, Van Zessen R, Flakowski J, Wan J-X, Deng F, et al. Synaptic mechanism underlying serotonin modulation of transition to cocaine addiction. Science. 2021;373:1252–6.
Higgins GA, Fletcher PJ. Therapeutic Potential of 5-HT2C Receptor Agonists for Addictive Disorders. ACS Chem Neurosci. 2015;6:1071–88.
Pearson D, Watson P, Albertella L, Le Pelley ME. Attentional economics links value-modulated attentional capture and decision-making. Nat Rev Psychol. 2022;1:320–33.
Le Pelley ME, Pearson D, Griffiths O, Beesley T. When goals conflict with values: counterproductive attentional and oculomotor capture by reward-related stimuli. J Exp Psychol: Gen. 2015;144:158–71.
Acknowledgements
We thank Gabrielle Weidemann for discussion and comments on this paper.
Funding
Preparation of this manuscript was supported by a Synergy grant from the National Health and Medical Research Council (GNT2009851) [GPM, EZM AJL], Discovery Project funding from the Australian Research Council (DP220100040 [GPM]; DP200102576 [GPM]; DP190100482 [GPM]; DP220102317 [PJRDB]). AJL acknowledges the Victorian State Government Operational Infrastructure Program. Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
GPM and PJRDB conceived the paper with input from EZM and AJL. GPM wrote the first draft and all authors contributed to editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
McNally, G.P., Jean-Richard-dit-Bressel, P., Millan, E.Z. et al. Pathways to the persistence of drug use despite its adverse consequences. Mol Psychiatry 28, 2228–2237 (2023). https://doi.org/10.1038/s41380-023-02040-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-023-02040-z
This article is cited by
-
Incubation of methamphetamine craving in punishment-resistant individuals is associated with activation of specific gene networks in the rat dorsal striatum
Molecular Psychiatry (2024)
-
Delay of punishment highlights differential vulnerability to developing addiction-like behavior toward sweet food
Translational Psychiatry (2024)
-
The selective D3Receptor antagonist VK4-116 reverses loss of insight caused by self-administration of cocaine in rats
Neuropsychopharmacology (2024)