Abstract
Neoplastic cartilage is a common component of teratomas in type II germ cell tumors. Although IDH1/2 mutations have been well-described in somatic cartilaginous tumors, ranging from benign enchondromas to highly aggressive dedifferentiated chondrosarcomas, the presence of IDH1/2 mutations in cartilaginous neoplasms arising from germ cell tumors has not been previously investigated. To better understand the relationship between these tumors and their bone/soft tissue counterpart, we studied the IDH1/2 mutational status of 20 cases of primary mediastinal mixed germ cell tumors with areas of readily identifiable cartilaginous differentiation. Our study found that cartilaginous lesions arising in germ cell tumors have a different frequency and distribution of IDH1/2 mutations compared to those at somatic sites. We identified IDH1/2 mutations in only 15% (3/20) of cases, compared to a frequency in the literature among differentiated chondroid tumors of bone and soft tissue of 54%, a highly significant decreased frequency (p = 0.0011; chi-square test). Furthermore, they were exclusively IDH2 R172 mutations that occurred at a non-significant, increased frequency in the germ cell tumor group compared to conventional chondrosarcoma (15% vs. 5%, respectively, p > 0.05, chi-square test). The unexpected finding, therefore, was entirely attributable to the absence of IDH1 R132 mutation in chondroid neoplasia of germ cell origin (p < 0.00001, Fisher exact test). Our results suggest that a subset of cartilaginous lesions arising within type II germ cell tumors have a similar oncogenic mechanism to their bone/soft tissue counterpart but that the majority form using different oncogenic mechanisms compared to their somatic counterparts.
Similar content being viewed by others
Introduction
Type II germ cell tumors1,2 develop in the testis, ovary, dysgenetic gonad, anterior mediastinum and pineal gland. They, except for the relatively uncommon cases in dysgenetic gonads and the pineal, are almost exclusively seen in young, sexually mature individuals, mostly males. They are characterized by amplification of a segment of 1750—3000 kilobases on the short arm of chromosome 12 corresponding to region 12p11.1-p12.13 and are prone to develop a variety of “somatic-type” malignancies4,5,6,7, which represent one of the most common causes of treatment failure in these young patients. This unfortunate complication is especially frequent in the mediastinal cases. The pathogenesis of such somatic-type malignancies is not well understood. Recently, Matoso et al. found that neuroglial neoplasms arising from type II testicular germ cell tumors lacked immunohistochemical evidence of a variety of underlying pathogenic mutations that are found in the central nervous system counterparts8. Among their findings was the absence of mutant isocitrate dehydrogenase 1 (IDH1) protein expression that would be expected in over 50% of central nervous system gliomas, where it correlates closely with IDH1 pathogenic mutation. This finding, as well as retained expression of ATRX and absence of BRAF V600E expression or BRAF mutation, suggest that neuroglial neoplasms derived from type II germ cell tumors originate by a fundamentally different mechanism from those of the central nervous system.
Neoplastic cartilage is a common component of teratomas in type II germ cell tumors. Even when not showing pronounced overgrowth, the cartilaginous teratoma component frequently shows chondroid atypia similar to that seen in conventional chondrosarcoma. Although IDH1/2 mutations have been well-described in somatic cartilaginous tumors, ranging from benign enchondromas to highly aggressive dedifferentiated chondrosarcomas, the presence of IDH1/2 mutations in cartilaginous neoplasms arising in germ cell tumors has not been previously investigated. Given the findings of Matoso et al., it would be of interest to know if such chondroid lesions from type II teratomas showed the IDH1/IDH2 mutations of their bone/soft tissue counterparts. We therefore undertook an investigation of IDH alterations in cartilaginous neoplasms arising in mediastinal germ cell tumors to see if there was support for a similar or different oncogenic mechanism compared to somatic chondroid tumors.
Materials and methods
With approval from the Internal Review Board of Indiana University, we retrospectively searched the pathology files and identified 20 cases of primary mediastinal mixed germ cell tumors from 1993 to 2018 with readily identifiable foci of cartilaginous differentiation within the teratoma component. Most of these cases had previously been reviewed for a study that examined vascular lesions in post-chemotherapy resections of primary mediastinal germ cell tumors9. Hematoxylin and eosin (H&E)-stained slides were collected and reviewed by two surgical pathologists (L.M.W. and T.M.U.).
For each case, a representative hematoxylin and eosin (H&E)-stained slide containing a focus of prominent cartilaginous differentiation was selected, and the corresponding formalin-fixed, paraffin-embedded tissue block was retrieved. Ten unstained sections (10 µm in thickness per section) were cut from each tissue block and mounted on uncharged slides (1 section per slide). Areas with prominent cartilaginous differentiation were circled by comparison with the corresponding selected H&E-stained slide and removed for DNA extraction. IDH1/2 mutational analysis was performed by polymerase chain reaction in the Indiana University Molecular Diagnostic Laboratory according to a previously published protocol10,11. None of the selected blocks had undergone any decalcification procedure.
IDH1/2 immunohistochemistry was performed on formalin-fixed paraffin-embedded whole sections from each case following pressure cooker antigen retrieval (DAKO PT Module; low pH Target Retrieval; Carpinteria, CA, USA) using a mouse monoclonal antibody for IDH1/2 mutant R132/172 (Millipore-Sigma, clone MsMab-1; 1:50 dilution; Darmstadt, Germany) with DAKO EnVision FLEX Detection System (Carpinteria, CA, USA). Appropriate positive and negative controls were included in each staining run.
Clinical information was collected from the electronic medical records, and all available follow-up information was reviewed.
Results
Clinical findings
This series consists of 20 primary mediastinal surgical resection specimens of mixed germ cell tumors containing a readily identifiable teratomatous cartilaginous component. Clinical and pathological details are summarized in Table 1. The majority of the resection specimens (19/20, 95%) were post chemotherapy; only one patient (case 20) did not receive neoadjuvant treatment with chemotherapy. One case (case 5) included the additional review of a focus of metastatic teratoma involving the lung, which was synchronously excised with the mediastinal primary. All patients were male with an average age of 29 years (range: 19–48 years). The majority presented with a mediastinal mass with associated elevated serum alpha-fetoprotein (AFP) (up to 24,610 ng/mL), and a few patients also had increased serum β-subunit of human chorionic gonadotropin β-hCG (up to 53,074 IU/L). Common presenting symptoms included shortness of breath (n = 10), chest pain/tightness (n = 7) and cough (n = 5). One patient presented with superior vena cava syndrome (case 3), and another had significant gynecomastia (case 4). Two years prior to definitive histologic diagnosis, one patient (case 9) was found to have elevated β-hCG with negative testicular work-up. The average overall tumor size for the primary mediastinal tumors was 15.3 cm (range: 3.5–27.0 cm in greatest dimension); the size of the lung metastasis (case 5) was 1.1 cm in greatest dimension. The largest continuous size of the cartilaginous component within the primary tumors was 1.6 cm and 0.2 cm in the lung metastasis (case 5). According to the Moran and Suster proposed clinical staging system for primary germ cell tumors of the mediastinum12, most cases were Stage I (n = 9), while the others were Stage II (n = 1), Stage IIIA (n = 8) and Stage IIIB (n = 2). Among the cases with metastases to intrathoracic organs (Stage IIIA), the involved metastatic sites were pleura (n = 3), lung (n = 4) and pectoral subcutaneous tissue (n = 1). The two cases with extrathoracic metastases (Stage IIIB) had involvement of the brain and liver. Clinical follow-up information was available in patients with an average duration of 29 months post primary resection (range: <1 to 216 months). One patient died at 2 months secondary to bleomycin-related pulmonary toxicity. Seven additional patients died of tumor progression at 2 to 216 months (mean, 48 months), including one from germ cell tumor-derived acute megakaryoblastic leukemia at 39 months13,14. Nine patients had no evidence of disease at an average of 27 months (range: <1 to 71 months).
Morphologic findings
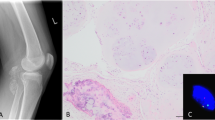
The morphologic findings were reviewed blindly without knowledge of the molecular or immunohistochemical results. Each case had readily identifiable teratoma elements with a component of well-circumscribed, discrete nodules of hyaline cartilage arising from a background of cellular stroma (Fig. 1A). The average number of cartilaginous nodules was 14 (range: 1–89), and most were small, averaging 5 mm in greatest dimension (range: 1–16 mm), with frequent slight increase in cellularity around the periphery. After careful searching, most cases (18/20, 90%) had at least one chondrocyte with multiple nuclei within one lacunar space (Fig. 2A). Two cases (cases 11 and 16) had areas of myxoid change, where the lacunae became poorly formed and the nodules less discrete, merging with the background stromal component (Fig. 1E). Histologic grading, as previously described by Evans15, showed that the majority of cases (15/20, 75%) were predominantly grade 1 (Fig. 1B), composed of cells with small, darkly staining nuclei without much nuclear detail. Five cases (cases 5, 7, 9, 10 and 16) had notable areas consistent with grade 2 (Fig. 1C), showing an increase in nuclear size with visible intranuclear detail. While some of the cases had occasional bizarre cells (Fig. 1F), none of the cases showed a predominance of areas resembling grade 3. Of the five cases with grade 2 features: one had myxoid change, three had mitotic figures, two had poorly formed nodules (Fig. 1D), and one case had known lung metastasis. Three cases had nucleoli visible at 10x (cases 5, 10 and 16), while the other cases had only inconspicuous nucleoli with several small pin-point nucleoli visible at high power (×40). Focal necrosis post chemotherapy was only visible in the cartilage component in one case (case 10). The remainder of cases showed no identifiable treatment effect within the cartilage component. Mitotic figures (Fig. 2B), which were in the adjacent spindle cell component as well as the chondrocytes, were present in three cases [case 7 (2 mitotic figures per 10 high power fields [hpf]), case 9 (3 mitotic figures per 10 hpf) and case 16 (4 mitotic figures per 10 hpf)]. In addition, three cases (cases 12, 17 and 20) had associated bone formation (Fig. 2C), resembling endochondral ossification. Lastly, the one case (case 5) with simultaneous evaluation of both the primary mediastinal lesion and lung metastasis showed similar histologic features in both lesions corresponding to grade 2.
The neoplastic cartilage in the teratoma component often formed well-circumscribed, discrete nodules of hyaline cartilage (1A, case 13, ×20) with a peripheral increase in cellularity. Most cases had a predominance of small, dark staining nuclei with features compatible with grade 1 (1B, case 20, ×40). A few cases had a moderate increase in nuclear size with intranuclear detail and several pinpoint nucleoli visible at high power (1C, case 7, ×40). Case 16 was notable for irregular, poorly defined nodules of cartilage that intermixed with adjacent cells (1D, case 16, ×20) and showed areas of myxoid change with poorly formed lacunae (1E, case 16, ×40). Occasional bizarre nuclei were present (1F, case 5, ×40); however, no cases showed features consistent with grade 3.
Most cases had at least one cell with multiple nuclei involving one lacunar space (2A, case 5, ×40) and rare cells had numerous nuclei (2A inset, case 2, ×40). Three cases had easily identifiable mitotic figures (2B, case 9, ×40), and three cases had associated bone formation, suggestive of endochondral ossification (2C, case 8, ×20).
Molecular findings
A subset of cases (3/20, 15%; cases 13, 16, and 17) had IDH2 R172 mutations, while the remainder were wild-type. No mutations in IDH1 were detected. The three cases with IDH2 R172 mutations did not share any identifiable pattern in either clinicopathologic or morphologic findings.
Immunohistochemical findings
Immunohistochemical staining with an anti-IDH1/2 mutant (R132/172) antibody was performed to assess the presence of mutated protein expression in correlation with the known molecular findings. Moderate to strong granular cytoplasmic staining was considered to be positive. Most cases without a detectable IDH1/2 mutation (13/17, 76%) demonstrated a complete lack of staining with the IDH1/2 mutant antibody (Fig. 3A, B), while a few cases (4/17, 24%) showed focal aberrant staining. Similarly, two of the three cases with a molecularly confirmed IDH2 R172 mutation demonstrated positive staining with the IDH1/2 mutant antibody (Fig. 3C, D), while the remaining case showed no significant cytoplasmic staining.
The majority of cases without an IDH1/2 mutation (IDH wild-type) demonstrated a lack of staining with an IDH1/2 immunohistochemical stain (3A–3B, case 8, ×40), while a few cases showed focal aberrant staining. Two of the three cases with a molecularly confirmed IDH2 mutation demonstrated strong positive staining with an IDH1/2 immunohistochemical stain (3C–3D, case 17, ×40), while one was negative.
Discussion
Isocitrate dehydrogenase (IDH) is a metabolic enzyme that plays an important role in the citric acid cycle, catalyzing the oxidative decarboxylation of isocitrate to produce alpha-ketoglutarate and carbon dioxide. In humans, the enzyme exists in three isoforms: IDH1, IDH2 and IDH3. IDH3, located in the mitochondrial matrix16, catalyzes the third step of the citric acid cycle using NAD+ as a cofactor. Likewise, IDH1, located in the cytoplasm and peroxisomes, and IDH2, also located in the mitochondrial matrix, catalyze the same reaction outside of the citric acid cycle using NADP+ as a cofactor. Heterozygous point mutations in IDH1/2 cause specific amino acid changes near the active site of the enzyme and occur almost exclusively at arginine residues, R132 in IDH1 and either R140 or R172 in IDH2. These mutations alter the function of the enzyme, resulting in the reduction of alpha-ketoglutarate to an oncometabolite, 2-hydroxyglutarate17,18. The resulting accumulation of 2-hydroxyglutarate leads to the inhibition of alpha-ketoglutarate-dependent oxygenases, such as the TET family of 5-methylcytosine hydroxylases, and prevents DNA demethylation19. These metabolic and epigenetic changes lead to global hypermethylation, thereby altering gene expression and playing an important role in oncogenesis.
While IDH3 mutations have not been reported in cancer to date, IDH1/2 mutations have been described in multiple, diverse tumor types, including: gliomas (80–90% of cases)20, acute myeloid leukemia (AML) (20% of cases)21,22, sinonasal undifferentiated carcinoma23, colorectal carcinoma24, cholangiocarcinoma25, prostate cancer26 and paraganglioma27, among others. In terms of connective tissue neoplasms, IDH1/2 mutations appear to be restricted to conventional central and periosteal cartilaginous tumors, as these mutations were not detected in ~1000 other bone and soft tissue neoplasms28. The presence of IDH1/2 mutations in multiple tumor types, including cartilaginous neoplasms, emphasizes the importance of altered metabolic pathways in cancer and suggests a possible shared oncogenic mechanism.
While IDH alterations have been described in numerous neoplasms, different tumors have been shown to have different IDH mutations. IDH1/2 mutations are present in >80% of diffuse gliomas (grade II–III), as well as most secondary glioblastomas29, and most of these mutations occur in IDH1 R132H, making the use of an immunohistochemical stain directed against the mutated IDH1 R132H protein an acceptable screening approach in neuroglial tumors30,31. In contrast to gliomas, IDH2 mutations are the most common in AML, frequently involving R14032, while sinonasal undifferentiated carcinomas have been found to have IDH2 R172X mutations (6/11, 55%), including R172S (n = 4), R172T (n = 1) and R172M (n = 1)23.
Conventional chondrosarcomas, in the combined experience of 3 studies10,28,33, harbored IDH1 R132 mutations in 93 of 148 (63%) informative cases, with IDH2 R172 mutations in 8 of 148 (5%); the remaining tumors (47/148, 32%) were wild-type for IDH1/IDH2. The distribution of IDH1 mutations in chondrosarcoma is quite different from gliomas, with the most frequent one being R132C followed by R132G and R132L. IDH2 mutations in chondrosarcomas occur in R172, with R172S being the most frequent34. The prevalence of IDH mutations has further been observed to increase with increasing histologic grade among chondrosarcomas. IDH1/2 mutations were detected in 87% (20/23) of dedifferentiated chondrosarcomas, with 1 R132H, 5 R132C, and 5 R132 mutations in the IDH1 gene and 9 R172 mutations in the IDH2 gene10. Among cases where both components were analyzed, the same mutation occurred in both the well-differentiated and dedifferentiated components. In addition, 88% of patients with Ollier disease and Maffucci syndrome have been shown to have identical IDH mutations across multiple tumors35. Unlike central chondrosarcoma and periosteal cartilaginous tumors, osteochondroma and secondary/peripheral chondrosarcoma are characterized by mutations in EXT1 and EXT2 rather than IDH1/2 mutations36.
Our study found that cartilaginous lesions arising in germ cell tumors of the mediastinum have a different frequency and distribution of IDH1/2 mutations compared to differentiated chondroid neoplasms at somatic sites. We identified an IDH1/2 mutation in only 15% (3/20) of cases, compared to a 54% (86/160) frequency in the combined experience of three series (Kerr DA and Nielsen GP, personal communication, 2022)10,28,33. This is a highly significant decreased frequency (p = 0.0011; chi-square test). Furthermore, these were exclusively IDH2 R172 mutations that occurred at a non-significant, increased frequency in the germ cell tumor group compared to conventional chondrosarcoma (15% [3/20] versus 5% [8/160], respectively, p = 0.078, chi-square test). The unexpected finding, therefore, was entirely attributable to the absence of any IDH1 R132 mutation in the chondroid neoplasia of germ cell origin (p < 0.00001, Fisher exact test). Our results suggest that a subset of cartilaginous lesions arising within type II germ cell tumors of the mediastinum have a similar oncogenic mechanism to their bone/soft tissue counterpart but that the majority form using different oncogenic mechanisms compared to their somatic counterparts. Furthermore, the predominance of IDH2 mutations underscores that screening with an immunohistochemical stain specific to IDH1 R132H, as commonly done in neuroglial neoplasms, is inadequate to capture the IDH alterations in the setting of germ cell tumors. Instead, an IDH1/2 specific antibody may be used, although based on our experience with one such antibody, the specificity and sensitivity were suboptimal compared to the gold standard of molecular mutational analysis.
In our series, similar to prior studies, no specific histologic or morphologic findings correlated with the presence or absence of IDH1/2 mutations. One interesting observation was that several cases had prominent areas of associated bone formation, which may relate to the presence of IDH mutations in these tumors and may mirror a similar proposed finding in conventional chondrosarcomas. Among chondrosarcomas arising in the head and neck, 60% of skull base tumors were found to have IDH mutations, while none of the tumors arising from the craniofacial bones had any detectable mutations. The difference was hypothesized to arise from the distinct modes of ossification where the skull base bones develop by endochondral ossification, and facial bones originate from intramembranous ossification34,37. The presence of IDH mutations in a subset of our group, which included one of the cases with associated bone formation reminiscent of endochondral ossification (case 17), suggests a similarity to the skull base lesions.
In our study, we did not have the opportunity to compare the IDH1/2 mutational status of any pre-treatment cartilaginous components with those found in the post-treatment specimens because either the initial biopsies were performed at outside facilities, or the patients were treated based solely on the clinical finding of an anterior mediastinal mass in conjunction with elevated serum tumor markers. It is, therefore, not possible for us to determine if chemotherapy had any effect on the IDH1/2 mutational status of our cases. Furthermore, based on the experience with type II germ cell tumors of the testis, many post-treatment metastatic teratomas (including those with cartilaginous components) do not have a corresponding teratomatous component in the primary tumor. Based on molecular studies, this phenomenon is felt to be due to the teratoma subsequently evolving from clones of cancer stem cells of the non-teratomatous components of the testicular tumor38. It seems likely that a similar process would apply to type II germ cell tumors of the mediastinum.
The prognostic significance of IDH1/2 mutations in the cartilaginous component of germ cell tumors remains to be determined, similar to conventional chondrosarcomas39. While IDH1/2 mutations are associated with a favorable outcome in gliomas40 and glioblastomas41, most studies have failed to demonstrate a significant prognostic impact of IDH mutations in conventional chondrosarcoma with somewhat conflicting results. For example, Lugowska et al. indicated an association of IDH mutations and shorter overall survival in chondrosarcoma42, while other studies failed to establish this relationship, showing instead that IDH mutations were found to be associated with longer relapse-free survival in grade 2–3 chondrosarcomas43. In addition, among skull base chondrosarcomas, Kanamori et al. did not find any significant correlation between IDH1 mutations and tumor relapse44.
While the mainstay of treatment for primary mediastinal germ cell tumors with a readily identifiable cartilaginous teratoma component remains surgical resection, the presence of IDH1/2 mutations may offer a future therapeutic target for patients with refractory disease associated with progression of chondroid neoplasms. One of us (T.M.U.) has seen a case of dedifferentiated chondrosarcoma arising from a germ cell tumor and metastasizing to the brain. (No material was available for investigation of the mutational status of this case). Mutant IDH inhibitors continue to be investigated and may represent an alternative therapeutic strategy in similar cases. In IDH1-mutant chondrosarcoma cell lines, the mutant IDH1 inhibitor AGI-5198 was shown to decrease (D)-2-hydroxyglutarate levels, resulting in diminished viability45; however, inhibition alone was likely not enough to suppress tumor growth46. Likewise, in patients with relapsed/refractory acute myeloid leukemia with detectable IDH2 mutations, an oral mutant IDH2-inhibitor (enasidenib) has been approved by the FDA for treatment47. Therefore, the presence of IDH2 mutations in a subset of our cases, offers the possibility for further investigation into the potential use of these inhibitors in patients with refractory disease.
In summary, our study suggests that most neoplastic chondroid lesions arising in type II germ cell tumors of the mediastinum, as exemplified by their lack of IDH1 R132 mutations, form differently from conventional chondrosarcoma of bone or soft tissue. Our results add to the evidence that somatic-type malignancies arising from type II germ cell tumors usually develop from different oncogenic mechanisms compared to the histologically similar neoplasms of somatic sites.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Oosterhuis JW, Looijenga LH. Testicular germ-cell tumours in a broader perspective. Nat Rev Cancer 5, 210–222 (2005)
Oosterhuis JW, Looijenga LH. Human germ cell tumours from a developmental perspective. Nat Rev Cancer 19, 522–537 (2019)
Mostert MC, Verkerk AJ, van de Pol M, J Heighway, P Marynen, C Rosenberg et al. Identification of the critical region of 12p over-representation in testicular germ cell tumors of adolescents and adults. Oncogene 16, 2617–2627 (1998)
Colecchia M, Necchi A, Paolina B, Nicolai N, Salvioni R. Teratoma with somatic-type malignant components in germ cell tumors of the testis: a clinicopathologic analysis of 40 cases with outcome correlation. Int J Surg Pathol 19, 321–327 (2011)
Magers MJ, Kao CD, Cole CD, Rice KR, Foster RS, Einhorn LH. “Somatic-type” malignancies arising from testicular germ cell tumors: a clinicopathologic study of 124 cases with emphasis on glandular tumors supporting frequent yolk sac tumor origin. Am J Surg Pathol 38, 1396–1409 (2014)
Guo CC., Punar M, Contreras AL, Tu SM, Pisters L, Tamboli, P. Testicular germ cell tumors with sarcomatous components: an analysis of 33 cases. Am J Surg Pathol 33 (8), 1173–1178 (2009).
Motzer RJ, Amsterdam A, Prieto V, Sheinfeld J, Murty VV, Mazumdar M. Teratoma with malignant transformation: diverse malignant histologies arising in men with germ cell tumors. J Urol 159, 133–138 (1998)
Matoso A, Idrees MT, Rodriguez FJ, Ibrahim J, Perrino CM, Ulbright TM, et al. Neuroglial differentiation and neoplasms in testicular germ cell tumors lack immunohistochemical evidence of alterations characteristic of their CNS counterparts: a study of 13 cases. Am J Surg Pathol 43, 422–431 (2019)
Levy DR, Agaram NP, Kao CS, Franks SE, Kesler KA, Stram AR, et al. Vasculogenic mesenchymal tumor: a clinicopathologic and molecular study of 55 cases of a distinctive neoplasm originating from mediastinal yolk sac tumor and an occasional precursor to angiosarcoma. Am J Surg Pathol 45, 463–476 (2021)
Chen S, Fritchie K, Wei S, Ali N, Curless K, Shen T et al. Diagnostic utility of IDH1/2 mutations to distinguish dedifferentiated chondrosarcoma from undifferentiated pleomorphic sarcoma of bone. Hum Pathol 65, 239–246 (2017)
Gondim DD, Gener MA, Curless KL, Cohen-Gadol AA, Hattab EM, Cheng L. Determining IDH-Mutational Status in Gliomas Using IDH1-R132H Antibody and Polymerase Chain Reaction. Appl Immunohistochem Mol Morphol 27, 722–725 (2019)
Moran CA, Suster S. Primary germ cell tumors of the mediastinum: I. Analysis of 322 cases with special emphasis on teratomatous lesions and a proposal for histopathologic classification and clinical staging. Cancer 80, 681–690 (1997)
Nichols CR, Hoffman R, Einhorn LH, Williams SD, Wheeler LA, Garnick MB. Hematologic malignancies associated with primary mediastinal germ-cell tumors. Ann Intern Med 102, 603–609 (1985)
Ladanyi M, Samaniego F, Reuter VE, Motzer RJ, Jhanwar SC, Bosl GJ et al. Cytogenetic and immunohistochemical evidence for germ cell origin of a subset of acute leukemias associated with mediastinal germ cell tumors. J Natl Cancer Inst 82, 221–227 (1990)
Evans HL, Ayala AG, Romsdahl MM. Prognostic factors in chondrosarcoma of bone: a clinicopathologic analysis with emphasis on histologic grading. Cancer 40, 818–831 (1977)
Losman JA, Kaelin WG Jr What a difference a hydroxyl makes: mutant IDH, (R)-2-hydroxyglutarate, and cancer. Genes Dev 27, 836–52 (2013)
Dang L, White DW, Gross S, Bennett BD, Bittinger MA, Driggers EM et al. Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature 462, 739–744 (2009)
Yen KE, Schenkein DP. Cancer-associated isocitrate dehydrogenase mutations. Oncologist 17, 5–8 (2012)
Schaefer IM, Hornick JL, Bovee JVMG. The role of metabolic enzymes in mesenchymal tumors and tumor syndromes: genetics, pathology and molecular mechanisms. Laboratory Investigation 98, 414–426 (2018)
Yan H, Parsons DW, Jin G, McLendon R, Rasheed BA, Yuan W et al. IDH1 and IDH2 mutations in gliomas. N Engl J Med 360, 765–773 (2009)
Abbas S, Lugthart S, Kavelaars FG, Schelen A, Koenders JE, Zeilemaker A et al. Acquired mutations in the genes encoding IDH1 and IDH2 both are recurrent aberrations in acute myeloid leukemia (AML): prevalence and prognostic value. Blood 116, 2122–2126 (2010)
Paschka P, Schlenk RF, Gaidzik VI, Habdank M, Kronke J, Bullinger L, et al. IDH1 and IDH2 mutations are frequent genetic alterations in acute myeloid leukemia and confer adverse prognosis in cytogenetically normal acute myeloid leukemia with NPM1 mutation without FLT3 internal tandem duplication. J Clin Oncol 28, 3636–3643 (2010)
Jo VY, Chau NG, Hornick JL, Krane JF, Sholl LM. Recurrent IDH2 R172X mutations in sinonasal undifferentiated carcinoma. Mod Pathol 30, 650–659 (2017)
Yen KE, Bittinger MA, Su SM, Fantin VR. Cancer-associated IDH mutations: biomarker and therapeutic opportunities. Oncogene 29, 6409–6417 (2010)
Borger DR, Tanabe KK, Fan KC, Lopez HU, Fantin VR, Straley KS, et al. Frequent mutation of isocitrate dehydrogenase (IDH)1 and IDH2 in cholangiocarcinoma identified through broad-based tumor genotyping. Oncologist 17, 72–79 (2012)
Kang MR, Kim MS, Oh JE, Kim YR, Song SY, Seo SI, et al. Mutational analysis of IDH1 codon 132 in glioblastomas and other common cancers. Int J Cancer 125, 353–355 (2009)
Gaal J, Burnichon N, Korpershoek E, Roncelin I, Bertherat J, Plouin PF, et al. Isocitrate dehydrogenase mutations are rare in pheochromocytomas and paragangliomas. J Clin Endocrinol Metab 95, 1274–1278 (2010)
Amary MF, Bacsi K, Maggiani F, Damato S, Halai D, Berisha F, et al. IDH1 and IDH2 mutations are frequent events in central chondrosarcoma and central and periosteal chondromas but not in other mesenchymal tumours. J Pathol 224, 334–343 (2011)
Cancer Genome Atlas Research Network, Brat DJ, Verhaak RG, Aldape KP, Yung WK, Salama SR, Cooper LA, et al. Comprehensive, integrative genomic analysis of diffuse lower-grade gliomas. N Engl J Med 372, 2481–2498 (2015)
Capper D, Zentgraf H, Balss J, Hartmann C, von Deimling A. Monoclonal antibody specific for IDH1 R132H mutation. Acta Neuropathol 118, 599–601 (2009)
Hartmann C, Meyer J, Balss J, Capper D, Mueller W, Christians A, et al. Type and frequency of IDH1 and IDH2 mutations are related to astrocytic and olidgogendroglial differentiation and age: a study of 1,010 diffuse gliomas. Acta Neuropathol 118, 469–474 (2009)
Thol F, Damm F, Wagner K, Gohring G, Schlegelberger B, Hoelzer D, et al. Prognostic impact of IDH2 mutations in cytogenetically normal acute myeloid leukemia. Blood 116, 614–616 (2010)
Kerr DA, Lopez HU, Deshpande V, Hornicek FJ, Duan Z, Zhang Y, et al. Molecular distinction of chondrosarcoma from chondroblastic osteosarcoma through IDH1/2 mutations. Am J Surg Pathol 37, 787–795 (2013)
Vuong HG, Ngo TNM, Dunn IF. Prognostic importance of IDH mutations in chondrosarcoma: An individual patient data meta-analysis. Cancer Medicine 10, 4415–4423 (2021)
Pansuriya TC, van Eijk R, d’Adamo P, van Ruler MAJH, Kuijjer ML, Oosting J, et al. Somatic mosaic IDH1 and IDH2 mutations are associated with enchondroma and spindle cell hemangioma in Ollier disease and Maffucci syndrome. Nat Genet 43, 1256–1261 (2011)
Szuhai K, Jennes I, de Jong D, Bovee JVMG, Wiweger M, Wuyts W, et al. Tiling resolution array-CGH shows that somatic mosaic deletion of the EXT gene is causative in EXT gene mutation-negative multiple osteochondroma patients. Hum Mutat 32, E2036–2049 (2011)
Tallegas M, Miquelestorena-Standley E, Labit-Bouvier C, Badoual C, Francois A, Gomez-Brouchet A, et al. IDH mutation status in a series of 88 head and neck chondrosarcomas: different profile between tumors of the skull base and tumors involving the facial skeleton and the laryngotracheal tract. Hum Pathol 84, 183–191 (2019)
Dorssers LCJ, Gillis AJM, Stoop H, van Marion R, Nieboer MM, van Riet J, et al. Molecular heterogeneity and early metastatic clone selection in testicular germ cell cancer development. Br J Cancer 120, 444–452 (2019)
Cleven AHG, Suijker J, Agrogiannis G, Briaire-de Bruijn IH, Frizzell N, Hoekstra AS, et al. IDH1 or -2 mutations do not predict outcome and do not cause loss of 5-hydroxymethylcytosine or altered histone modifications in central chondrosarcomas. Clin Sarcoma Res 7, 8 (2017)
Houillier C, Wang X, Kaloshi G, Mokhtari K, Guillevin R, Laffaire J, et al. IDH1 or IDH2 mutations predict longer survival and response to temozolomide in low-grade gliomas. Neurology 75, 1560–1566 (2010)
Sanson M, Marie Y, Paris S, Idbaih A, Laffaire J, Ducray F, et al. Isocitrate dehydrogenase 1 codon 132 mutation is an important prognostic biomarker in gliomas. J Clin Oncol 27, 4150–4154 (2009)
Lugowska I, Teterycz P, Mikula M, Kulecka M, Kluska A, Balabas A, et al. IDH1/2 mutations predict shorter survival in chondrosarcoma. J Cancer 9, 998–1005 (2018)
Zhu GG, Nafa K, Agaram N, Zehir A, Benayed R, Sadowska J, et al. Genomic profiling identifies association of IDH1/IDH2 mutation with longer relapse-free and metastasis-free survival in high-grade chondrosarcoma. Clin Cancer Res 26, 419–427 (2020)
Kanamori H, Kitamura Y, Kimura T, Yoshida K, Sasaki H. Genetic characterization of skull base chondrosarcomas. J Neurosurg 123, 1036–1041 (2015)
Li L, Paz AC, Wilky BA, Johnson B, Galoian K, Rosenberg EA, et al. Treatment with a small molecule mutant IDH1 inhibitor suppresses tumorigenic activity and decreases production of the oncometabolite 2-hydroxyglutarate in human chondrosarcoma cells. PLoS ONE 10, e0133813 (2015)
Suijker J, Oosting J, Koornneef A, Struys EA, Salomons GS, Schaap FG, et al. Inhibition of mutant IDH1 decreases D-2-HG levels without affecting tumorigenic properties of chondrosarcoma cell lines. Oncotarget 6, 12505–12519 (2015)
Kim ES. Enasidenib: first global approval. Drugs 77, 1705–1711 (2017)
Author information
Authors and Affiliations
Contributions
LMW performed study concept and design, performed development of methodology and writing, and reviewed and revised the paper. MS and JDS provided acquisition, analysis and interpretation of data. LC provided acquisition, analysis and interpretation of data and reviewed and revised the paper. TMU performed study concept and design, reviewed and revised the paper and performed statistical analysis. All authors read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was performed in accordance with the Declaration of Helsinki. No identifying data is included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Warmke, L.M., Cheng, L., Sperling, R.M. et al. Atypical cartilage in type II germ cell tumors of the mediastinum show significantly different patterns of IDH1/2 mutations from conventional chondrosarcoma. Mod Pathol 35, 1636–1643 (2022). https://doi.org/10.1038/s41379-022-01106-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-022-01106-7