Abstract
The role of programmed cell death-ligand 1 (PD-L1) in cervical cancer has been widely investigated; however, the influences of other inhibitory B7 family members are poorly understood. We investigated the expression of PD-L1, B7 homolog 3 (B7-H3), B7-H4, and V-domain Ig suppressor of T-cell activation (VISTA) and their association with the clinicopathological features and outcomes of a large cohort of 673 patients with squamous cell carcinoma or adenocarcinoma of the uterine cervix. The positivity rates for PD-L1 (combined positive score ≥1), B7-H3 in tumor cells (TCs), B7-H4 (exclusively in TCs), VISTA in immune cells (ICs), and VISTA in TCs were 57.9%, 62.8%, 44.8%, 92.6%, and 4.8%, respectively, in 606 primary cervical cancer samples. Co-expression of PD-L1 with B7-H3 in TCs and with B7-H4 and VISTA in ICs was observed in 38.8%, 25.4%, and 57.9% of samples, respectively. B7-H3 in TCs and B7-H4 and VISTA in ICs were observed in 58.1%, 46.6%, and 83.1% of PD-L1-negative samples, respectively. These proteins were observed more frequently in squamous cell carcinomas and in moderately to poorly differentiated carcinomas. VISTA (in ICs) and B7-H4 were more frequent in primary tumors than in recurrent counterparts and correlated with improved survival; in contrast, B7-H3 positivity in TCs was less frequent in primary tumors and correlated with short disease-specific survival. Co-expression of B7-H4 and VISTA in ICs was an independent predictor of favorable outcomes overall and among patients with PD-L1-negative tumors. These data indicate that B7 family proteins exhibit differing expression patterns, distributions, and prognostic implications in cervical cancer. Furthermore, the co-expression of PD-L1 with other checkpoint proteins suggests that PD-1/PD-L1 blockade combined with modulating other immune checkpoints may present a novel therapeutic approach for cervical cancer. Future studies are needed to validate prognostic values of B7 family proteins and explore their biological roles in this malignancy.
Similar content being viewed by others
Introduction
Cervical cancer is diagnosed in about 500,000 women and causes over 265,000 deaths annually worldwide1. Despite the availability of screening programs, 5–15% of patients are diagnosed at advanced stages and have metastatic disease. Even among women with earlier disease stages, 15–61% will experience metastasis or recurrence2. The prognoses of patients with advanced or recurrent cervical cancer are poor, with response rates ranging from 13% to 36% using currently available therapeutic options3. Inhibiting immune checkpoint proteins such as programmed cell death 1 (PD-1) or its ligand PD-L1 improves the outcomes of patients with several types of malignancies4,5. The PD-1 inhibitor pembrolizumab has been approved by the United States Food and Drug Administration for patients with advanced PD-L1-positive (defined as a combined positive score [CPS] ≥ 1) cervical cancer that progresses during or after chemotherapy. However, the objective response rate is relatively low (12% and 17% in the KEYNOTE-028 and KEYNOTE-158 studies, respectively)6,7. Therefore, there is an unmet need for novel therapeutic strategies that increase durable response rates, utilize more effective agents, and improve lives and outcomes of patients with this disease.
The B7 family includes 10 immune checkpoint proteins: B7-1 (CD80), B7-2 (CD86), B7 homolog 1 (B7-H1, PD-L1), B7-DC (PD-L2), B7-H2, B7-H3, B7-H4, B7-H5 (V-domain Ig suppressor of T-cell activation, VISTA), B7-H6, and B7-H78,9. These proteins function as important secondary signals that either stimulate and support T-cell action or suppress T-cell responses by selectively binding to CD28 family members such as PD-1. They also play an important role in maintaining self-tolerance and antitumor immunity. Like their well-studied family member PD-L1, other B7 proteins exhibit immunomodulatory behaviors and are correlated with survival in patients with cancer9. Such previously published data prompted us to investigate whether B7 family proteins can serve as prognostic biomarkers and/or potential therapeutic targets in patients with cervical cancer.
The expression of PD-L1, B7-H3, and B7-H4 in cervical cancer has been previously described;10,11,12,13,14,15,16 however, VISTA expression status and the interactions among these immune checkpoint proteins remain unknown. Additionally, the sample sizes in previous studies were small, rendering their conclusions not very persuasive. We previously investigated the expression of B7 family proteins in clear cell carcinoma of the uterine cervix17. In the present study, we investigated the expression profiles of the inhibitory B7 family checkpoint proteins PD-L1, B7-H3, B7-H4, and VISTA, examined their potential associations, and searched for any correlations with clinicopathological features and outcomes in a large cohort of 673 patients with cervical cancer.
Materials and methods
Study cohort and tissue microarray (TMA) construction
This retrospective study included 606 patients with primary cervical cancer who underwent cervical conization (N = 16) or hysterectomy (including radical hysterectomy) (N = 590), as well as 67 patients with recurrent cervical cancer who underwent pelvic exenteration or metastasectomy. All patients were treated between January 2004 and December 2018 at the Peking Union Medical College Hospital in Beijing, China. Only patients diagnosed with squamous cell carcinoma (SCC) and usual-type adenocarcinoma were included in this study; we excluded those with adenosquamous carcinoma, those with non-usual types of endocervical adenocarcinoma (i.e., mucinous gastric/intestinal, adenoma malignum, serous, clear cell, or endometrioid carcinoma), those with neuroendocrine carcinoma, or those with inadequate formalin-fixed and paraffin-embedded tissue blocks for TMAs. To determine the depth of stromal invasion, lymphovascular space invasion (LVSI), lymph node metastasis, histological type, tumor differentiation, hematoxylin and eosin-stained slides were reviewed by 2 gynecologic subspecialty pathologists (L. Zong and S. Yu) who were blinded to the original pathology reports and to each other’s interpretations. In case of disagreement, a third expert pathologist (J. Chen) was consulted to arrive at a final decision. Representative tumor tissue areas exhibiting epithelial tumor tissue mixed with tumor-related stroma were marked on hematoxylin and eosin-stained slides and sampled for TMA blocks. TMAs with single 2-mm core per case were constructed using a tissue arrayer (MiniCore, Mitogen, Hertford, UK). Clinical data such as age at diagnosis, tumor size, neoadjuvant chemotherapy, postoperative adjuvant treatment (chemotherapy and/or radiotherapy), date of recurrence or last follow-up, and patient status at the last follow-up were collected from medical records. All patients were staged using the 2009 International Federation of Gynecology and Obstetrics (FIGO) staging system for carcinoma of the cervix. This study conformed to the ethical standards set forth in the Declaration of Helsinki and in national and international guidelines and was approved by the Institutional Review Board of Peking Union Medical College Hospital (SK-995). All patients signed consent forms upon admission to the hospital allowing the review of their medical records, use of their tissue samples, and possible publication of associated reports. None of the patients can be identified based on their clinical information or images in this study, and informed consent to determine B7 family proteins was not required owing to the retrospective nature of the analysis.
Immunohistochemistry
Immunohistochemistry was performed using our laboratory protocol as described previously17,18,19,20,21. Briefly, 4 μm TMA serial sections were deparaffinized and subjected to heat-induced epitope retrieval with 10 mM sodium citrate (pH 6.0) at 95°C for 20 min. The endogenous peroxidase activity was quenched using a 0.3% hydrogen peroxide solution. TMA sections were incubated with primary antibodies against PD-L1 (dilution 1:200, clone E1L3N, Cell Signaling Technology [CST], Danvers, USA), B7-H3 (dilution 1:200, clone D9M2L, CST), B7-H4 (dilution 1:200, clone D1M8I, CST), and VISTA (dilution 1:200, clone D1L2G, CST). Human tonsil tissues treated with primary antibodies were used as positive controls, while the same tissues treated with isotype-matched antibodies comprised the negative controls. All slides were stained using an automatic immunohistochemistry staining instrument (BOND-III; Leica Biosystems, Wetzlar, Germany) according to the manufacturer’s instructions.
Assessment of PD-L1, B7-H3, B7-H4, and VISTA
PD-L1 was evaluated based on the CPS, which was calculated as the sum of the number of PD-L1-stained cells (tumor cells [TCs], lymphocytes, and macrophages) divided by the total number of viable TCs, with the quotient multiplied by 100. A CPS ≥ 1 denoted positive PD-L1 expression. Samples were considered positive for B7-H3/B7-H4 when ≥5% of TCs expressed these proteins at any intensity, as described in a previous study22. Per previously published guidance, B7-H3 was considered positive when observed in stromal cells (predominately in fibroblasts)23,24. VISTA expression was evaluated in TCs and immune cells (ICs) separately. TCs were considered VISTA positive if at least 1% of cells per TMA core had membranous and/or cytoplasmic staining. The proportions of VISTA-expressing tumor-infiltrated and stromal (i.e., tumor-adjacent) ICs to the total tumor-infiltrated and stromal ICs per TMA core, respectively, were determined; these values were considered continuous variables. ICs or TCs with ≥1% VISTA staining were defined as VISTA-positive, as described in our studies in ovarian cancer, invasive ductal carcinoma of the breast, colorectal cancer, and endometrial cancer18,19,21,25.
Statistical analysis
The χ² test was used to determine associations among categorical variables, and Spearman’s rank correlation coefficients were used to determine correlations among continuous variables. Relapse-free survival (RFS) was defined as the interval between the date of surgery and that of the detection of the first relapse. Disease-specific survival (DSS) was defined as the interval between the date of surgery and that of death owing to cervical cancer. Survival curves were plotted using the Kaplan-Meier method and compared using the log-rank test. To identify prognostic predictors, univariate and multivariate survival analyses were performed using the Cox proportional hazards regression model, and hazard ratios with 95% confidence intervals for recurrence and death were calculated. All statistical analyses were conducted using the Statistical Package for the Social Sciences (version 20.0; IBM Corp., Armonk, NY, USA). A 2-sided P-value < 0.05 was considered statistically significant.
Results
Expression of B7 family proteins in primary and recurrent cervical cancer
The median age of patients with primary cervical cancer was 44 years (range, 23–74 years). Among the 606 samples, 491 (81.0%) and 115 (19.0%) were diagnosed as SCC and adenocarcinoma, respectively; the clinicopathological characteristics of the patients are summarized in Supplementary Table S1. One hundred and twenty-eight patients (21.1%) received neoadjuvant chemotherapy before undergoing surgery. Adjuvant treatment, when required, included radiotherapy (pelvic external beam radiotherapy and/or vaginal brachytherapy) with or without platinum-based chemotherapy. None of the patients were administered immune checkpoint inhibitors or other immunotherapeutic agents.
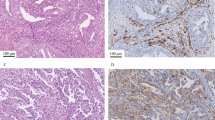
PD-L1 and VISTA were detected in both TCs and ICs, while B7-H3 was detected in both TCs and stromal cells (predominately in fibroblasts). In contrast, B7-H4 was expressed exclusively in TCs and exhibited a cytoplasmic/membranous staining pattern (Fig. 1). Positive PD-L1 (i.e., a CPS ≥ 1) was observed in 57.9% of the samples, and B7-H4 was observed in the TCs of 44.8%. VISTA was detected in the ICs of 92.6% of samples, while only 4.8% expressed VISTA in TCs. B7-H3 was detected in TCs of 62.8% of the samples, while its expression in stromal compartments was observed in 94.0% (Table 1).
The median age of the 67 patients with recurrent cervical cancer was 45 years; most received initial treatment at other hospitals and were admitted to Peking Union Medical College Hospital to receive salvage treatment upon experiencing recurrence. Thus, the samples from these 67 recurrent patients were not matched with the abovementioned primary cervical cancers; their clinicopathological features are summarized in Supplementary Table S2. PD-L1, B7-H4, and VISTA positivity in ICs was more frequent in primary tumors than in recurrent counterparts, while tumoral B7-H3 expression was observed more frequently in recurrent cervical cancer (Table 1).
Association between B7 family proteins and clinicopathological features
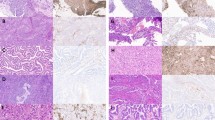
The associations between the expression of B7 family checkpoint proteins and patients’ clinicopathological features are presented in Supplementary Table S3. PD-L1, VISTA in ICs and B7-H3, B7-H4, and VISTA in TCs were observed significantly more frequently in SCCs than in adenocarcinomas (Fig. 2A). PD-L1, B7-H3 (in stromal cells and TCs), B7-H4, and VISTA (in ICs) were more frequently positive in moderately and poorly differentiated carcinomas (Fig. 2B). B7-H3 expression in stromal cells was associated with unfavorable pathological features (i.e., the presence of LVSI and lymph node metastasis). B7-H4 positivity correlated with small tumor size (<4 cm) and the presence of LVSI. None of the 4 investigated B7 family proteins were associated with FIGO stage or stromal invasion. Additionally, there was no difference in B7 family protein expression between patients who received neoadjuvant chemotherapy and those who did not.
PD-L1, B7-H3 in tumor cells (TCs) and in stroma, B7-H4 in TCs, VISTA in TCs, and VISTA in ICs across A histological types: squamous cell carcinoma (SCC) and adenocarcinoma and B tumors with well, moderate, and poor differentiation. PD-L1 programmed cell death-ligand 1, B7-H3 B7 homolog 3, B7-H4 B7 homolog 4, VISTA V-domain Ig suppressor of T-cell activation, TCs tumor cells, ICs immune cells.
Association between PD-L1, B7-H3, B7-H4, and VISTA
As shown in Table 2, VISTA expression in ICs correlated positively with PD-L1, B7-H4, and B7-H3 in TCs; VISTA in TCs was associated with PD-L1 but not with B7-H3 or B7-H4; both PD-L1 and B7-H4 positively correlated with B7-H3 in TCs; and no association was observed between PD-L1 and B7-H4. When evaluated as a continuous variable, the extent of VISTA positivity in ICs was significantly and directly correlated with the CPS of PD-L1 (Spearman’s ρ = 0.382, P < 0.001). Co-expression of PD-L1 with B7-H3 (in TCs), B7-H4, and VISTA (in ICs) was observed in 38.8%, 25.4%, and 57.9% of the samples, respectively. Notably, 83.1% of the PD-L1-negative samples expressed VISTA in ICs, 58.1% expressed B7-H3 in TCs, 46.6% expressed B7-H4, and 92.7% expressed at least 1 of these checkpoint proteins (B7-H3, B7-H4, and/or VISTA). Of the 605 patient samples for which data regarding both B7-H4 and VISTA in ICs were available, 261 (43.1%) were double positive for B7-H4 and VISTA in ICs, 35 (5.8%) were double negative, and 309 (51.1%) had only one or the other (single positive).
Association between B7 family protein expression and prognosis in patients with cervical cancer
After excluding patients who only had conization specimens available and those whose follow-up times were under 3 months, 531 patients with primary cervical cancer who underwent radical surgeries with complete adjuvant systemic therapy (when necessary) were subjected to survival analysis. There were no significant differences between the entire cohort of 606 patients and this survival analysis-only subgroup in terms of clinicopathological parameters (data not shown). After a median follow-up of 36 months (range, 9–195 months), 64 patients (12.1%) had relapsed and 49 (9.2%) had died owing to cervical cancer as of July 2020.
Univariate analysis showed that FIGO stage, lymph node metastasis, and VISTA in ICs were significantly associated with survival across the entire cohort (Fig. 3, Supplementary Fig. S1, and Table S4). Positive B7-H4, negative B7-H3 in TCs, and small tumor size (<4 cm) tended to be associated with improved DSS, although the relationship was not significant. Although VISTA in TCs was not associated with RFS (P = 0.083), none of the 24 patients with VISTA-positive TCs relapsed (Fig. 3). Moreover, 230 patients were double positive for B7-H4 and VISTA in ICs, 31 were double negative, and 270 were single positive. Kaplan-Meier analysis showed that patients with B7-H4 and VISTA double-positive tumors had excellent outcomes, those with double-negative tumors had poor RFS, and those with single-positive status had intermediate outcomes (Fig. 3 and Supplementary Table S4). On multivariate analysis adjusted for FIGO stage and lymph node metastasis, B7-H4 combined with VISTA in ICs remained significantly associated with RFS and DSS (Table 3). Additionally, B7-H3 positivity in TCs was a predictor of poor DSS independent of B7-H4 and VISTA in ICs or of FIGO stage.
Subgroup survival analyses were performed according to PD-L1 status. VISTA expression in ICs was significantly associated with improved RFS and DSS in 216 patients with PD-L1-negative cervical cancer, while B7-H4 positivity was associated with improved RFS (Fig. 4). Consistent with results observed in the entire cohort, patients with B7-H4 and VISTA double-positive tumors had favorable outcomes, while those with double-negative tumors had poor outcomes (Fig. 4). On univariate and multivariate analyses, double-negative B7-H4 and VISTA in ICs was the only predictor of poor RFS and DSS in patients with PD-L1-negative tumors (Table 4). B7-H4 expression or B7-H4 combined with VISTA in ICs was not associated with survival in patients with PD-L1-positive cervical cancer (data not shown). The association between VISTA in ICs and survival was not analyzed in patients with PD-L1-positive tumors considering all had VISTA-positive ICs.
Discussion
To our knowledge, this is the first study of the expression profiles of the inhibitory B7 family checkpoint proteins PD-L1, B7-H3, B7-H4, and VISTA in a large cohort of patients with cervical cancer. Despite their varying expression patterns and distributions, these proteins positively correlated with each other (the only lack of association was between PD-L1 and B7-H4). These proteins were expressed more frequently in SCC than in adenocarcinoma and were also more prevalent in moderately and poorly differentiated carcinomas. VISTA in ICs and B7-H4 were observed more frequently in primary tumors than in recurrent counterparts and were correlated with improved RFS and DSS; in contrast, B7-H3 positivity in TCs was less frequent in primary tumors than in recurrent lesions and was correlated with poor DSS. Double positivity for B7-H4 and VISTA (in ICs) predicted excellent outcomes overall as well as in the subgroup of patients with PD-L1-negative cervical cancer. These data suggest that, although B7 family proteins are closely related, their expression status and clinical significance thereof have distinct implications in patients with cervical cancer.
PD-1 inhibitors have been approved for treating PD-L1-positive cervical cancer, and many studies have investigated the expression of PD-L1 in this disease10,11,12,26,27,28,29,30. However, the sample sizes in most of these studies were small, and the data they produced were conflicting. In 3 previous studies, PD-L1 expression was associated with unfavorable prognosis;10,12,28 in contrast, Kawachi et al.’s study of 127 patients with invasive adenocarcinoma found that those with PD-L1-positive tumors tended to experience longer survival26. In our present large-sample study, PD-L1 was not associated with patient survival, which is consistent with data from 3 older studies11,27,29. PD-L1 positivity was observed more frequently in SCC than in adenocarcinoma, which is consistent with the observations of Heeren et al. and Zhang et al.12,16. Additionally, we found that PD-L1 expression was more frequent in moderately and poorly differentiated carcinomas than in well-differentiated counterparts, which is consistent with data reported by Saglam et al.27 and Zhang et al.16. These findings indicate that PD-L1 is not necessarily a predictor of survival, and that only half of the patients with SCC and with moderately and poorly differentiated tumors are candidates for anti-PD-1 immunotherapy.
The B7-H3 and B7-H4 checkpoints inhibit the activation and function of T cells9. Their expression profiles have been investigated in various cancers, including cervical cancer, and they were found to be associated with poor survival9,13,14,15,16,31,32,33,34. B7-H3 positivity was observed more frequently in SCC and in tumors with unfavorable pathological features (such as LVSI and lymph node metastasis) in both Zhang et al.’s study16 and ours. We found that B7-H3 in TCs correlated with unfavorable prognosis and was an independent predictor of short DSS, which is consistent with previously published data14,15,16,31. Previous investigations suggested that B7-H4 expression impairs antitumor immune responses and correlates with poor survival outcomes in cervical cancer13,31,32,34. In contrast, our analysis showed that B7-H4 expression correlated with improved survival in the entire cohort and in the subgroup of patients with PD-L1-negative tumors. B7-H4 has been identified as an immune coinhibitory molecule; however, recent evidence suggests that it limits tumor growth in animal models35. Rahbar et al. found that high B7-H4 expression correlated with improved RFS in 2681 patients with breast cancer35, which is consistent with our findings in endometrial cancer (data not published) and cervical cancer (the present study). These data suggest that B7-H3 expression is a predictor of poor outcomes and a potential immunotherapeutic target; in contrast, anti-B7-H4 therapy may be detrimental considering this protein’s correlation with favorable prognosis, especially in patients with PD-L1-negative tumors.
Discovered in 2011, VISTA is a coinhibitory molecule that suppresses T-cell activation, proliferation, and cytokine release36,37. VISTA expression was found to be a poor prognostic factor in patients with oral squamous cell carcinoma38 and in those with melanoma39. However, increasing evidence suggests that VISTA correlates with improved survival in patients with many other cancer types40. Consistent with our findings in endometrial cancer25, breast and colorectal cancers18,21, VISTA expression in ICs was associated with favorable survival outcomes in patients with cervical cancer. Interestingly, patients with B7-H4 and VISTA double-positive tumors had the most favorable outcomes, those with double-negative tumors had short survival, and those with single-positive tumors had intermediate survival durations. Importantly, co-expression of B7-H4 and VISTA in ICs was a prognostic indicator independent of FIGO stage or lymph node metastasis status. To our knowledge, our study is the first to investigate the co-expression of both B7-H4 and VISTA in terms of identifying patients with a distinct risk of relapse and cancer-specific death. T-cell-based immunoscoring has been validated and is recommended as a new component of a TNM immune classification for colon cancer41. As such, an immunoscore based on B7-H4 and VISTA could be considered for cervical cancer risk classification once these markers’ prognostic values are validated. Additionally, the association between VISTA/B7-H4 expression and favorable prognosis should be considered in future clinical trials of immunotherapy for cervical cancer.
The association between PD-L1 and each of B7-H3, B7-H4, and VISTA has been investigated previously in various cancers16,42,43,44,45,46,47,48,49,50,51,52. Zhang et al. found that B7-H3 positively correlated with PD-L1 and that they were co-expressed in 21.0% of 552 cervical cancer samples16. Consistent with their study, our results showed that B7-H3 was associated with PD-L1, with 38.8% of our samples positive for both. These data support the combined blockade of B7-H3 and PD-1/PD-L1 as a therapeutic strategy. B7-H4 is positively correlated with PD-L1 in oral squamous cell carcinoma53 but is inversely correlated with PD-L1 in breast and lung cancers43,47. In our present study, no association between B7-H4 and PD-L1 was observed, which corresponds to previous findings in ovarian cancer54. Interestingly, B7-H4 positivity was observed in 46.6% of PD-L1-negative samples and was associated with a favorable prognosis; such individuals had low response rates to PD-1 inhibitors and therefore lacked effective immunotherapeutic options. VISTA in ICs was positively associated with PD-L1; this is consistent with previous findings in lung cancer51,52, lymphoma44, and craniopharyngioma50 as well as those of our studies of patients with breast cancer18, colorectal cancer21, and endometrial cancer25. Additionally, VISTA in ICs was associated with B7-H3 and B7-H4 in TCs of cervical cancer. In a study of 132 patients with craniopharyngioma, Wang et al. found that VISTA correlated with PD-L1 but not with B7-H3 or B7-H450. The expression of one or more B7 family checkpoint proteins suggest that they play synergic and/or complementary roles in the immune evasion of cervical cancer. Although the regulatory mechanism of B7 family proteins in cervical cancer remains unknown, the expression profiles of B7 family proteins as elucidated in our present study ought to contribute to the better understanding of the tumor immune environment and the mechanisms by which cervical cancers evade immune surveillance. Future studies are warranted to validate the prognostic values of B7 family members in cervical cancer and identify their regulatory mechanisms as this may assist in the development of new immunotherapeutic agents.
The strengths of our study were its exclusivity to SCC and usual-type adenocarcinoma, its comprehensive analysis of B7 family proteins, and its large sample size derived from a single tertiary hospital. This study also had some limitations. First, it was a retrospective investigation that produced inherent unavoidable biases. Second, the use of TMAs may not have accurately represented the entirety of each sample considering the intratumoral heterogeneity and variable sampling of the tumor-stroma interface across patients. PD-L1 was observed in 57.9% of the primary tumors in our study as assessed using TMAs; this proportion was approximately 80% in both the KEYNOTE-028 and KEYNOTE-158 clinical trials, which assessed PD-L1 in whole sections6,7. As such, the relatively low proportion of PD-L1-positive tumors may be attributed to our use of TMAs and/or to the relatively high proportion of adenocarcinomas in our study, as these tumor types express PD-L1 less frequently than do SCCs. Finally, our study was limited by its single-center nature and the lack of an independent validation cohort. Further studies from independent cohorts are needed to validate our findings.
In conclusion, we found that the inhibitory B7 family members PD-L1, B7-H3, B7-H4, and VISTA are expressed frequently in cervical cancer, particularly in SCC and moderately to poorly differentiated carcinomas. Although these 4 proteins are closely related, their expression patterns, distributions, and prognostic implications differ. B7-H3 positivity in TCs correlates with poor prognosis, while double positivity for B7-H4 and VISTA in ICs is an independent predictor of favorable outcomes. The co-expression of PD-L1 and other checkpoint proteins suggest that PD-1/PD-L1 blockade combined with the modulation (including the upregulation) of other immune checkpoints may represent a novel therapeutic approach for patients with cervical cancer. Future studies are needed to explore the underlying regulatory mechanisms of B7 family proteins and their biological roles in cervical cancer, especially in PD-L1-negative tumors.
Data availability
The raw data used in this study are available from the corresponding author upon reasonable request.
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2015. CA Cancer J. Clin. 65, 5–29 (2015).
Waggoner, S. E. Cervical cancer. Lancet 361, 2217–2225 (2003).
Boussios, S. et al. Management of patients with recurrent/advanced cervical cancer beyond first line platinum regimens: where do we stand? A literature review. Crit. Rev. Oncol. Hematol. 108, 164–174 (2016).
Schellens, J. H. M. et al. Pembrolizumab for previously treated advanced cervical squamous cell cancer: preliminary results from the phase 2 KEYNOTE-158 study. J. Clin. Oncol. 35, 5514 (2017). suppl.
Atkins, M. B., Clark, J. I. & Quinn, D. I. Immune checkpoint inhibitors in advanced renal cell carcinoma: experience to date and future directions. Ann. Oncol. 28, 1484–1494 (2017).
Chung, H. C. et al. Efficacy and safety of pembrolizumab in previously treated advanced cervical cancer: results from the phase II KEYNOTE-158 study. J. Clin. Oncol. 37, 1470–1478 (2019).
Frenel, J. S. et al. Safety and efficacy of pembrolizumab in advanced, programmed death ligand 1-positive cervical cancer: results from the phase Ib KEYNOTE-028 trial. J. Clin. Oncol. 35, 4035–4041 (2017).
Janakiram, M. et al. The third group of the B7-CD28 immune checkpoint family: HHLA2, TMIGD2, B7x, and B7-H3. Immunol. Rev. 276, 26–39 (2017).
Andrews, L. P., Yano, H. & Vignali, D. A. A. Inhibitory receptors and ligands beyond PD-1, PD-L1 and CTLA-4: breakthroughs or backups. Nat. Immunol. 20, 1425–1434 (2019).
Rivera-Colon, G. et al. PD-L1 expression in endocervical adenocarcinoma: correlation with patterns of tumor invasion, CD8+ tumor-infiltrating lymphocytes, and clinical outcomes. Am. J. Surg. Pathol. 45, 742–752 (2021).
Enwere, E. K. et al. Expression of PD-L1 and presence of CD8-positive T cells in pre-treatment specimens of locally advanced cervical cancer. Mod. Pathol. 30, 577–586 (2017).
Heeren, A. M. et al. Prognostic effect of different PD-L1 expression patterns in squamous cell carcinoma and adenocarcinoma of the cervix. Mod. Pathol. 29, 753–763 (2016).
Han, S. et al. Negative roles of B7-H3 and B7-H4 in the microenvironment of cervical cancer. Exp. Cell Res. 371, 222–230 (2018).
Han, S. et al. Roles of B7-H3 in cervical cancer and its prognostic value. J. Cancer 9, 2612–2624 (2018).
Li, Y. et al. B7-H3 promotes the proliferation, migration and invasiveness of cervical cancer cells and is an indicator of poor prognosis. Oncol. Rep. 38, 1043–1050 (2017).
Zhang, Q. et al. Expression of B7-H3 correlates with PD-L1 and poor prognosis in patients with cervical cancer. OncoTargets Ther. 14, 4275–4283 (2021).
Zong, L. et al. Expression and significance of immune checkpoints in clear cell carcinoma of the uterine cervix. J. Immunol. Res. 2020, 1283632 (2020).
Zong, L. et al. Expression of the immune checkpoint VISTA in breast cancer. Cancer Immunol. Immunother. 69, 1437–1446 (2020).
Zong, L. et al. VISTA expression is associated with a favorable prognosis in patients with high-grade serous ovarian cancer. Cancer Immunol. Immunother. 69, 33–42 (2020).
Zong, L. et al. PD-L1, B7-H3 and VISTA are highly expressed in gestational trophoblastic neoplasia. Histopathology 75, 421–430 (2019).
Zong, L. et al. High VISTA expression correlates with a favorable prognosis in patients with colorectal cancer. J. Immunother. 44, 22–28 (2021).
Zang, X. et al. B7-H3 and B7x are highly expressed in human prostate cancer and associated with disease spread and poor outcome. Proc. Natl Acad. Sci. USA 104, 19458–19463 (2007).
Zhang, Q. et al. Expression of B7-H3 correlates with PD-L1 and poor prognosis in patients with cervical cancer. OncoTargets Ther. 14, 4275–4283 (2021).
Zang, X. et al. Tumor associated endothelial expression of B7-H3 predicts survival in ovarian carcinomas. Mod. Pathol. 23, 1104–1112 (2010).
Zong L., et al. Analysis of the immune checkpoint V-domain Ig-containing suppressor of T-cell activation (VISTA) in endometrial cancer. Mod. Pathol. (2021), https://doi.org/10.1038/s41379-021-00901-y
Kawachi, A. et al. Tumor-associated CD204(+) M2 macrophages are unfavorable prognostic indicators in uterine cervical adenocarcinoma. Cancer Sci. 109, 863–870 (2018).
Saglam, O. et al. PD-L1 expression correlates with young age and CD8+ TIL density in poorly differentiated cervical squamous cell carcinoma. Int. J. Gynecol. Pathol. 39, 428–435 (2020).
Wang, S. et al. Programmed death ligand 1 promotes lymph node metastasis and glucose metabolism in cervical cancer by activating integrin beta4/SNAI1/SIRT3 signaling pathway. Oncogene 37, 4164–4180 (2018).
Karim, R. et al. Tumor-expressed B7-H1 and B7-DC in relation to PD-1+ T-cell infiltration and survival of patients with cervical carcinoma. Clin. Cancer Res. 15, 6341–6347 (2009).
Mezache, L. et al. Enhanced expression of PD L1 in cervical intraepithelial neoplasia and cervical cancers. Mod. Pathol. 28, 1594–1602 (2015).
Huang, C. et al. B7-H3, B7-H4, Foxp3 and IL-2 expression in cervical cancer: associations with patient outcome and clinical significance. Oncol Rep. 35, 2183–2190 (2016).
Wang, X. et al. B7-H4 overexpression impairs the immune response of T cells in human cervical carcinomas. Hum. Immunol. 75, 1203–1209 (2014).
Brustmann, H. et al. Epithelial and tumor-associated endothelial expression of B7-H3 in cervical carcinoma: relation with CD8+ intraepithelial lymphocytes, FIGO stage, and phosphohistone H3 (PHH3) reactivity. Int. J. Gynecol. Pathol. 34, 187–195 (2015).
Liu, W. et al. B7-H4 overexpression correlates with a poor prognosis for cervical cancer patients. Mol. Clin. Oncol. 2, 219–225 (2014).
Rahbar, R. et al. B7-H4 expression by nonhematopoietic cells in the tumor microenvironment promotes antitumor immunity. Cancer Immunol. Res. 3, 184–195 (2015).
Flies, D. B. et al. Coinhibitory receptor PD-1H preferentially suppresses CD4(+) T cell-mediated immunity. J. Clin. Invest. 124, 1966–1975 (2014).
Wang, L. et al. VISTA, a novel mouse Ig superfamily ligand that negatively regulates T cell responses. J. Exp. Med. 208, 577–592 (2011).
Wu, L. et al. Expression of VISTA correlated with immunosuppression and synergized with CD8 to predict survival in human oral squamous cell carcinoma. Cancer Immunol. Immunother. 66, 627–636 (2017).
Kuklinski, L. F. et al. VISTA expression on tumor-infiltrating inflammatory cells in primary cutaneous melanoma correlates with poor disease-specific survival. Cancer Immunol. Immunother. 67, 1113–1121 (2018).
Yum, J. I. & Hong, Y. K. Terminating cancer by blocking VISTA as a novel immunotherapy: Hasta la vista, baby. Front. Oncol. 11, 658488 (2021).
Pagès, F. et al. International validation of the consensus Immunoscore for the classification of colon cancer: a prognostic and accuracy study. Lancet 391, 2128–2139 (2018).
Altan, M. et al. B7-H3 expression in NSCLC and its association with B7-H4, PD-L1 and tumor-infiltrating lymphocytes. Clin. Cancer Res. 23, 5202–5209 (2017).
Altan, M. et al. Association of B7-H4, PD-L1, and tumor infiltrating lymphocytes with outcomes in breast cancer. NPJ Breast Cancer 4, 40 (2018).
He, H. X. et al. VISTA and PD-L1 synergistically predict poor prognosis in patients with extranodal natural killer/T-cell lymphoma. Oncoimmunology 10, 1907059 (2021).
Chen, D. et al. Enhanced B7-H4 expression in gliomas with low PD-L1 expression identifies super-cold tumors. J. Immunother. Cancer 8, e000154 (2020).
Lu, Z. et al. B7-H3 immune checkpoint expression is a poor prognostic factor in colorectal carcinoma. Mod. Pathol. 33, 2330–2340 (2020).
Schalper, K. A. et al. Differential expression and significance of PD-L1, IDO-1, and B7-H4 in human lung cancer. Clin. Cancer Res. 23, 370–378 (2017).
Gruosso, T. et al. Spatially distinct tumor immune microenvironments stratify triple-negative breast cancers. J. Clin. Invest. 129, 1785–1800 (2019).
Cheng, H. et al. Wide expression and significance of alternative immune checkpoint molecules, B7x and HHLA2, in PD-L1-negative human lung cancers. Clin. Cancer Res. 24, 1954–1964 (2018).
Wang, Y. et al. Expression and clinical significance of PD-L1, B7-H3, B7-H4 and VISTA in craniopharyngioma. J. Immunother. Cancer 8, e000406 (2020).
Parra, E. R. et al. Immunohistochemical and image analysis-based study shows that several immune checkpoints are co-expressed in non-small cell lung carcinoma tumors. J. Thorac. Oncol. 13, 779–791 (2018).
Villarroel-Espindola, F. et al. Spatially resolved and quantitative analysis of VISTA/PD-1H as a novel immunotherapy target in human non-small cell lung cancer. Clin. Cancer Res. 24, 1562–1573 (2018).
Wu, L. et al. B7-H4 expression indicates poor prognosis of oral squamous cell carcinoma. Cancer Immunol. Immunother. 65, 1035–1045 (2016).
MacGregor, H. L. et al. Tumor cell expression of B7-H4 correlates with higher frequencies of tumor-infiltrating APCs and higher CXCL17 expression in human epithelial ovarian cancer. Oncoimmunology 8, e1665460 (2019).
Acknowledgements
We thank the medical record room staff for their assistance in retrieving the patients’ medical records. This work was supported by grants from the National Natural Science Foundation of China (Nos. 81772783, 81971475, and 82001664), National Scientific Data Sharing Platform for Population and Health (NCMI-YF01N-201906), and Chinese Academy of Medical Sciences Initiative for Innovative Medicine (Nos. CAMS-2017-I2M-1-002 and CAMS-2016-I2M-1-001). The funders of the study had no role in the design of the study; collection, analysis, and interpretation of the data; or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
Y.X. and J.C. made substantial contributions to the conception and design, acquisition of data, and critical revision of the manuscript. Y.Z., Y.K. and Y.G. made substantial contributions to patient selection and clinical data. L.Z., S.M. and S.Y. made substantial contributions to reviewing pathological parameters, assessing the results of immunohistochemistry, interpreting the data, and drafting the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
The study was approved by the Institutional Review Board of Peking Union Medical College Hospital (approval number: S-K995).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Zong, L., Gu, Y., Zhou, Y. et al. Expression of B7 family checkpoint proteins in cervical cancer. Mod Pathol 35, 786–793 (2022). https://doi.org/10.1038/s41379-021-00979-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-021-00979-4