Abstract
Nodular fasciitis is a benign, self-limited, pseudosarcomatous neoplasm that can mimic malignancy due to its rapid growth, cellularity, and mitotic activity. Involvement of the breast is rare and diagnosis on biopsy can be challenging. In this largest series to date, we examined the clinicopathologic and molecular characteristics of 12 cases of nodular fasciitis involving the breast/axilla. All patients were female, with a median age of 32 years (range 15–61). The lesions were 0.4 to 5.8 cm in size (median 0.8). All cases presented as palpable masses, and two patients had overlying skin retraction. Microscopically, lesions were relatively well-circumscribed nodular masses of bland myofibroblastic spindle cells within a variably myxoid stroma. Infiltrative growth into adipose tissue or breast epithelium was frequent. Mitotic figures were present in all cases, ranging from 1 to 12 per 10 high-power fields (median 3). Immunohistochemically, all cases expressed smooth muscle actin and were negative for pan-cytokeratin, p63, desmin, CD34, and nuclear beta-catenin. Targeted RNA sequencing performed on 11 cases identified USP6 gene fusions in eight; one additional case was positive by break-apart fluorescence in situ hybridization. The common MYH9-USP6 rearrangement was detected in four cases; another case had a rare alternative fusion with CTNNB1. Three cases harbored novel USP6 gene fusions involving NACA, SLFN11, or LDHA. All fusions juxtaposed the promoter region of the 5′ partner gene with the full-length coding sequence of USP6. Outcome data were available for eight patients; none developed recurrence or metastasis. Five patients elected for observation without immediate excision, and self-resolution of the lesions was reported in three cases. Albeit uncommon, nodular fasciitis should be considered in the differential diagnosis of breast spindle cell lesions. A broad immunohistochemical panel to exclude histologic mimics, including metaplastic carcinoma, is important. Confirmatory detection of USP6 rearrangements can aid in classification, with potential therapeutic implications.
Similar content being viewed by others
Introduction
Nodular fasciitis is a benign, self-limited mesenchymal neoplasm of unknown etiology that most commonly occurs in younger to middle-aged individuals [1]. It typically presents as a small (<2 cm), rapidly growing mass within the subcutaneous tissue. Nodular fasciitis can occur at virtually any anatomic site, although it most frequently involves the extremities, head and neck, and trunk. Histopathologically, nodular fasciitis is characterized by a cellular proliferation of mitotically active myofibroblastic/fibroblastic spindle cells that express smooth muscle actin [2]. Molecularly, the majority of cases harbor a gene rearrangement involving USP6 (ubiquitin specific peptidase 6), which encodes a deubiquitination enzyme [3]. Typically, USP6 is fused with MYH9 (myosin heavy chain 9), although rare alternative non-MYH9 fusion partners have been recently reported [3,4,5]. Given the recurrent nature of USP6 fusions in nodular fasciitis, molecular testing can be diagnostically helpful [6]. In contrast to other spindle cell lesions, nodular fasciitis often spontaneously regresses without treatment, and recurrences are extremely rare [7, 8].
Despite increased awareness since its initial description in 1955 [9], nodular fasciitis remains prone to misdiagnosis. Studies estimate that up to 60% of cases are misclassified and 20–30% are overdiagnosed as malignancy [2, 10]. The high rate of misclassification may be due in part to its rapid clinical growth and pseudosarcomatous microscopic appearance. Accurate diagnosis of nodular fasciitis may be particularly challenging when cases arise at unusual anatomic sites, such as the breast, or when tissue sampling is limited. Involvement of the breast by nodular fasciitis is extremely rare with only a limited number of cases reported in the literature [2, 3, 7, 10,11,12,13,14,15,16,17,18,19]. Diagnostic distinction of nodular fasciitis from other spindle cell lesions of the breast, such as metaplastic carcinoma, may have critical implications for guiding appropriate clinical management. Recognition of nodular fasciitis on biopsy requires awareness of the spectrum of morphologic features, thoughtful application of immunohistochemistry, and, occasionally, confirmatory molecular testing. To date, a systematic and comprehensive clinicopathologic and molecular analysis of nodular fasciitis involving the breast has not been reported.
In this study, as the largest series to date, we present the clinical, morphologic, and immunohistochemical features of 12 cases of nodular fasciitis involving the breast and axilla. In addition, we performed RNA-based next-generation sequencing and identified novel USP6 gene fusions, expanding the genetic spectrum of USP6-rearranged neoplasms.
Materials and methods
Study population
With institutional review board approval, the pathology archives of Stanford University and Kaiser Permanente (San Francisco, CA) were searched for cases of nodular fasciitis or likely nodular fasciitis of the breast. Representative H&E slides were then independently reviewed by two soft tissue pathologists with agreement, resulting in a study cohort of 12 cases. Five cases were core biopsies and seven were excision specimens. Each tumor was assessed for common microscopic features of nodular fasciitis, including mitotic activity, extravasated red blood cells, microcystic change, and an infiltrative border. Prior to the study, one case had already undergone confirmatory USP6 break-apart fluorescence in situ hybridization (FISH) testing. Clinicopathologic and outcome data were obtained from electronic medical records when available.
Hybrid capture next-generation DNA and RNA sequencing
RNA from 11 cases was extracted from sectioned scrolls of formalin-fixed paraffin-embedded (FFPE) tissue using a Qiagen RNeasy FFPE Kit (Qiagen, Germantown, MD, USA). A reference purified RNA sample (Seraseq Fusion RNA Mix; SeraCare, Cat. No. 0710-0431, Milford, MA, USA) was used as a positive control. cDNA was synthesized from total RNA and sequencing libraries were constructed using a KAPA Stranded RNA-Seq Library Preparation Kit (Roche Sequencing, Pleasanton, CA, USA). Samples were multiplexed and underwent enrichment for a 43-gene targeted RNA fusion panel (Fusion-STAMP, Supplemental Table S1) using Roche SeqCap RNA Choice target enrichment probes spanning the entirety of the gene transcripts of interest (Roche Sequencing). Sequencing was performed on an Illumina MiSeq (Illumina, San Diego, CA). Sequencing reads were mapped to the human reference genome (GRCh37, hg19) using the STAR-Fusion algorithm (v 1.1.0). STAR-Fusion uses the STAR aligner to map reads and identify candidate fusion transcripts, which are then processed by the STAR-Fusion algorithm to map junction reads and spanning reads to a reference annotation set and to produce a final fusion transcript list [20]. Two cases were additionally subjected to DNA extraction and underwent sequencing using a 130-gene targeted panel (STAMP, Supplemental Table S2), as previously described [21]. Results were visualized and verified using Integrated Genome Viewer (Broad Institute, Cambridge, MA).
Immunohistochemistry
For immunohistochemistry, the following antibodies were used: SMA (smooth muscle actin, 1A4, 1:200, Cell Marque, Rocklin, CA, USA), cytokeratin cocktail (AE1/AE3 + Cam5.2, 1:75 + 1:25, Dako, Santa Clara, CA, USA, and BD Biosciences, Franklin Lakes, NJ, USA), CK5/6 (D5/16B4, 1:50, Cell Marque), p63 (BC4A4, 1:50, Biocare Medical, Pacheco, CA, USA), CD34 (MY10, 1:160, BD Biosciences), desmin (DE-R-11, undiluted, Ventana, Tucson, AZ, USA), beta-catenin (14, undiluted, Ventana), S100 protein (polyclonal, 1:1000, Dako), and ER (estrogen receptor, SP1, undiluted, Ventana). CK5/6, p63, CD34, ER (all with ER2 retrieval), and S100 protein (enzyme retrieval) were performed on Leica BOND III (Buffalo Grove, IL, USA) instruments. SMA (no retrieval), cytokeratin cocktail (protease2 retrieval), desmin (protease1 retrieval), and beta-catenin (CC1 retrieval) were performed on Roche Ventana Benchmark Ultra instruments. For consultation cases, a minority of immunohistochemical stains were performed at the original institution.
USP6 fluorescence in situ hybridization
USP6 break-apart FISH testing was performed at the Mayo Clinic Sequencing Core on four cases. 5′ USP6 DNA (clones RP11-198F11, RP11-115H24, and RP11-124C16) labeled with SpectrumOrange dUTP (Abbott Molecular/Vysis Products, Abbott Park, IL, USA) and 3′ USP6 DNA (clones CTD-2367F23, RP11-457I18, RP11-1140D18, and RP11-373N8) labeled in SpectrumGreen dUTP (Abbott Molecular/Vysis Products) were combined as one probe set. The break-apart probe set was applied to individual slides, hybridized, and washed according to the PAT reduced pepsin FISH protocol [22]. At least 50 non-overlapping nuclei were analyzed per case.
Results
Clinicopathologic features of mammary nodular fasciitis
We identified 12 cases histopathologically and immunohistochemically compatible with nodular fasciitis and located in the breast (n = 10) or axilla (n = 2). Five cases were core biopsies and seven were excision specimens. In all cases, the patients were evaluated and managed by dedicated breast imaging and surgery teams, and subsequent specimens were directed to a breast pathology service or pathologist with breast subspecialty experience. The clinicopathologic characteristics of these tumors are summarized in Table 1.
All patients were women with an age range from 15 to 61 years (median 32). For 10 cases with detailed clinical information, all presented as self-detected, palpable masses. Overlying skin retraction was noted in two patients. Three patients described the lesions as tender or painful, while three other patients denied pain. One case occurred in the setting of recent local trauma, one arose during pregnancy, and another developed seven months postpartum. Patient 10 underwent an excision of a hamartoma involving the ipsilateral breast three years prior. Patient 6 underwent partial mastectomy and sentinel lymphadenectomy for ipsilateral invasive lobular carcinoma five years prior, followed by margin re-excision, radiation, and endocrine therapy.
The lesions ranged from 0.4 to 5.8 cm in size (median 0.8 cm). Ultrasound performed in six cases (patients 1, 3, 5–7, and 11) demonstrated ovoid hypoechoic masses with irregular (n = 5) or spiculated (n = 1) margins, and surrounding or internal vascularity in two cases. An additional magnetic resonance imaging (MRI) study on patient 3 noted enhancement with apparent tethering of adjacent skin. Patient 4 underwent mammography which revealed an indistinct, oval, solid mass with surrounding echogenic reaction extending to the skin and marked internal vascularity with power Doppler. Four masses (cases 1, 4, 9, and 10) were described as superficial or subcutaneous by the radiologist. Case 2 was in the pediatric setting and imaging was omitted.
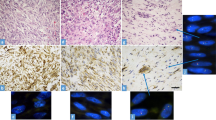
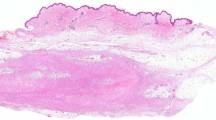
By microscopic assessment, 4 of 12 specimens (33%) included breast ducts and/or lobules, while eight lesions (67%) were surrounded by fibroadipose tissue without mammary epithelium. Two of the seven excisions contained skin. Where evaluable, the lesions formed well-circumscribed nodular masses with varying degrees of fibrous encapsulation (partial in three, complete in one) (Fig. 1). Despite their circumscription, the majority of cases had at least a focally infiltrative peripheral tumor border into surrounding adipose tissue (10/12), breast epithelium (2/12), and/or fibroconnective tissue (1/12). The lesions showed a range of cellularity and myxoid stromal change. Relatively hypocellular lesions often displayed the most prominent myxoid change, while lesions with higher cellularity featured a more collagenous stroma.
A Lesions were typically well-circumscribed with a nodular architecture and variable degrees of encapsulation. B While most lesions arose in the subcutaneous tissue, a subset was located deeper within the parenchyma, as evidenced by adjacent breast epithelium (lactational change at right). This case was relatively hypocellular and showed a prominent myxoid stroma. C Some lesions were comparatively less myxoid and more cellular. In this case, there was focal entrapment of breast epithelial elements (arrows). D The majority of cases showed at least a focally infiltrative tumor border. E The lesions were comprised of relatively uniform plump spindled cells admixed with foci of extravasated erythrocytes. Occasionally, deposits of hemosiderin were seen. F Other classical features of nodular fasciitis were present, including stromal microcystic change and scattered multinucleated giant cells (arrows). G Typical mitotic figures (arrow) were present in all cases. H All cases were positive for smooth muscle actin by immunohistochemistry.
The lesions were composed of relatively uniform, plump myofibroblastic spindle cells with normochromatic nuclei, discernible nucleoli, and wispy cytoplasm, predominantly arranged in short storiform fascicles. Foci of stromal microcystic change were seen in most cases, imparting the classic “tissue culture” appearance. Significant cytologic atypia or pleomorphism was not observed. Mitotic figures were present in all cases, ranging from 1 to 12 per 10 high-power fields (400×) (median 3 per 10 HPF); atypical forms were not identified. Admixed extravasated erythrocytes (11/12, 92%) and lymphoid cells (8/12, 67%) were commonly identified in the background. A subset of cases had foci of hemosiderin-laden macrophages (3/12, 25%) or multinucleated giant cells (4/12, 33%).
Immunohistochemically, all cases expressed smooth muscle actin. Expression of SMA was generally diffuse, although rare cases showed more patchy expression (Fig. 1). The tumor cells were negative for pan-cytokeratin (0/12), CK5/6 (0/7), p63 (0/10), CD34 (0/12), desmin (0/11), and nuclear beta-catenin (0/9). Weak focal S100 protein staining was seen in two of eleven cases. Estrogen receptor (ER) was negative in all three evaluated cases.
Seven patients underwent surgical excision and five patients elected for observation only after a diagnosis was rendered on core biopsy. Of the excisions, surgical margins were negative in three cases (cases 4, 9, and 11) and positive in four cases (cases 2, 5, 7, and 12). Cases 2, 7, and 12 did not undergo further surgery, but case 5 proceeded with re-excision for negative margins (with no residual lesion present) despite a definitive diagnosis of “nodular fasciitis.” Clinical follow-up beyond surgery was available for eight patients (67%) (Table 1). The median duration of follow-up was 4 years (range 5–114 months). No recurrences or metastases occurred. Within the observation-only group, three lesions self-resolved without treatment (by 4 weeks in case 3, 3 weeks in case 8, and 14 weeks in case 10). Patient 3 subsequently underwent an excision at this same site one year later for fibroadenomas, with no residual nodular fasciitis identified. Case 1 showed no interval growth during the limited follow-up period of 5 months, and case 6 was too recent for significant evaluation.
Genomic features
To interrogate for USP6 rearrangements, all cases were subjected to molecular analysis by a targeted RNA sequencing fusion panel (11 cases) and/or USP6 FISH (4 cases). Molecular results are summarized in Table 1 and Fig. 2. USP6 rearrangements were identified in nine cases (75%); eight were detected by RNA sequencing and one was identified by FISH.
A Schematic illustrating the canonical MYH9-USP6 gene fusion that juxtaposes exon 1 of MYH9 to mid-exon 1 of USP6 (NM_004505.4, red lines, and box) or exon 2 of USP6 (blue lines and box). Adapted from Patel et al. [4]. B Schematic depicting the alternative USP6 gene fusions identified in this study. Exon 1 of the 5′ partner gene (CTNNB1, NACA, LDHA, and SLFN11) is fused with exon 1 of USP6. (C) Integrative Genome Viewer (IGV) visualization of a representative MYH9-USP6 fusion breakpoint identified by RNA sequencing (case 9). Top panel shows read spanning MYH9 exon 1. Reads to the right of the dotted vertical line correctly map to the MYH9 coding sequence, while select reads to the left (unmapped, colored) align to USP6. The bottom panel shows the corresponding breakpoint in mid-exon 1 of the USP6 locus. (D) Break-apart fluorescence in situ hybridization (FISH) showing rearrangement of the USP6 locus (separation of green and orange signals) (case 12).
Of the eight cases detected by RNA sequencing, four (50%) harbored the common MYH9-USP6 fusion transcript. The remaining four cases harbored USP6 gene fusions with alternative partners. In case 4, USP6 was fused with CTNNB1 (catenin beta-1; 3p22.1). Cases 7, 8, and 10 harbored novel USP6 fusion partners, involving NACA (nascent-polypeptide-associated complex alpha polypeptide; 12q13.3), LDHA (lactate dehydrogenase; 11p15.1), and SLFN11 (schlafen family member 11; 17q.12), respectively. In all cases, a noncoding exon 1 of the 5’ partner gene was fused with the full-length coding sequence of USP6 (Fig. 2). The USP6 breakpoints were located within exon 1 (6/8, 75%) or at the start of exon 2 (2/8, 25%) (Supplemental Table S3). Two cases were additionally interrogated by a targeted DNA sequencing panel: one fusion-positive and one fusion-negative (cases 12 and 5, respectively). No pathogenic alterations were detected in either lesion.
Discussion
In this study, we describe the spectrum of clinicopathologic and molecular features of 12 cases of nodular fasciitis occurring in the breast or axilla, representing the largest series of its kind to date. Most cases presented in the third and fourth decades, although rare cases occurred in younger (age 15) and significantly older patients (age 61). Nodular fasciitis of the breast has been reported in patients as old as 88 years, indicating a wide possible age range [15]. The majority of lesions are <2 cm in size; rare cases can be quite large, as exemplified by case 12 of our series (5.8 cm). All patients in our cohort presented with self-detected, palpable masses, and some described pain or tenderness; skin retraction was additionally present in two cases. Most lesions were located in the outer quadrants of the breast and appeared to be situated within the subcutaneous tissue. Associated breast epithelium was present in a minority of cases. Whether these cases originated within the breast parenchyma itself or secondarily involved breast parenchyma by subcutaneous extension is unclear, in part due to the absence of a well-defined tissue plane between subcutis and breast parenchyma. While nodular fasciitis has a tendency to arise in the subcutis, it can occur primarily in deeper tissues, such as skeletal muscle.
Generally, lesions form well-circumscribed, nodular masses with varying degrees of encapsulation. Almost all cases in our series showed at least focal infiltration into adjacent tissue. This finding should not be misinterpreted to suggest an invasive malignancy. Other key features that can facilitate a diagnosis of nodular fasciitis of the breast include recognition of the myxoid stroma, foci of microcystic change, uniform myofibroblastic spindle cells, and admixed erythrocytes and lymphoid cells. While mitotic figures are frequently encountered and can occasionally be numerous, atypical forms would not be expected. No specific features differed between cases with or without mammary epithelium in our series, although two cases illustrated that nodular fasciitis can variably infiltrate and envelop breast ducts and lobules.
The differential diagnosis of spindle cell lesions of the breast is broad and includes benign and malignant neoplasms and reactive conditions. Distinguishing spindle cell lesions on biopsy is often diagnostically challenging because many entities display significant histopathologic overlap; an immunohistochemical panel is often prudent. Nodular fasciitis is consistently negative for most commonly used markers, yet invariably expresses SMA. While this can aid in the diagnosis, SMA is non-specific and warrants care in interpretation. Multiple keratins and p63 are important to rule out metaplastic carcinoma, which may manifest with only low-grade morphologic features, thus potentially mimicking nodular fasciitis. Additional markers including CD34, desmin, S100 protein, and beta-catenin can be helpful to exclude other neoplasms, including phyllodes tumor, myofibroblastoma, dermatofibrosarcoma protuberans, smooth muscle tumors, neural lesions, and desmoid fibromatosis, among others. While focal weak expression of S100 protein was seen in two cases in our cohort, strong diffuse expression was never observed, and all other examined markers were negative.
Nodular fasciitis is prone to misdiagnosis as malignancy, as described in numerous studies and case reports [2, 12, 13, 15, 18]. Its pseudosarcomatous appearance with high cellularity, increased mitotic activity, and infiltrative borders can result in misinterpretation as a more aggressive lesion. Moreover, these lesions often present with rapid clinical growth and are associated with vague or potentially concerning imaging characteristics, such as irregular or spiculated margins and internal vascularity. Involvement of the breast by nodular fasciitis is extremely uncommon [23, 24]. In a recent comprehensive review of the literature, Paliogiannis et al. [19] identified only 22 reported cases of nodular fasciitis involving the breast over a period from 1990 to 2016. Given its rarity at this anatomic site, nodular fasciitis is infrequently encountered by breast pathologists. As such, it may be overlooked as a diagnostic consideration in the workup of a mammary spindle cell lesion. Recognition that nodular fasciitis can occur in the breast and appreciation of the distinctive histopathologic features is critical to avoid misdiagnosis and unnecessary overtreatment. Nodular fasciitis does not require radical surgical intervention given its benign clinical course and limited capacity for recurrence [25]. In addition, nodular fasciitis may spontaneously resolve without treatment, typically within a period of 2–4 weeks after diagnosis [8, 26]. Therefore, in contrast to most spindle cell lesions of the breast for which surgical excision is standard, a period of non-operative watchful waiting may be appropriate when nodular fasciitis is definitively diagnosed on core biopsy.
In practice, arriving at a diagnosis of nodular fasciitis on biopsy requires careful exclusion of other entities in the differential diagnosis. In a specimen with well-sampled lesional tissue, if (1) there are multiple histologic features of nodular fasciitis, including a characteristic microcystic change imparting a tissue culture-like appearance, extravasated erythrocytes, and non-atypical cytomorphology, (2) smooth muscle actin stains in a myofibroblastic (“tram-track”) pattern, and (3) additional immunohistochemical workup is negative, then it would be reasonable to sign out a core biopsy as consistent with nodular fasciitis in our view. Of note, nodular fasciitis has been purely a morphologic diagnosis only until recently. In the last 10 years, the identification of recurrent USP6 rearrangements in nodular fasciitis and the increased utilization of genetic testing has allowed USP6 molecular analysis to play a role in the diagnostic process. In difficult cases and/or cases with limited sampling, detection of a USP6 fusion can provide additional confidence for a diagnosis of nodular fasciitis.
The reported frequency of USP6 gene rearrangements in nodular fasciitis occurring at any anatomic site has ranged from 74 to 100% [3, 4, 10, 27]. Since the discovery of USP6 fusions in nodular fasciitis in 2011, there have been 16 cases reported that have involved the breast or axilla [3, 4, 13, 15,16,17, 28,29,30,31,32,33,34,35,36] (see Table 2). Of these cases, USP6 status was interrogated in only five cases by FISH, and only 2/5 were positive for a USP6 rearrangement; in one case, the fusion partner was identified as MYH9 by RT-PCR [4]. In our study, we detected a USP6 rearrangement in 75% of cases using a combination of break-apart FISH and targeted RNA sequencing. We retrospectively re-examined the three cases where a USP6 rearrangement was not detected (cases 3, 5, and 6). These lesions generally displayed a more fibrous stroma but were otherwise indistinguishable morphologically and immunohistochemically from the USP6 fusion-positive cases. Targeted DNA sequencing of one fusion-negative case detected no pathologic alterations; further evaluation of the two remaining fusion-negative cases was no longer possible following exhaustion of lesional tissue. The differential diagnosis for these three cases primarily includes scar. Indeed, all of these patients had prior injuries to the site that could have resulted in scar formation (prior excisions in cases 3 and 6 and local trauma in case 5). Of course, this history does not exclude nodular fasciitis, as preceding trauma is also believed to be a precipitating factor for nodular fasciitis. While the distinction between scar and nodular fasciitis may be difficult, if not impossible, in many cases, both represent benign lesions for which clinical management is similar. In our opinion, if molecular studies fail to identify a USP6 rearrangement but morphologic and immunohistochemical findings are most suggestive of nodular fasciitis, one may still favor a diagnosis of nodular fasciitis. However, if a case lacks a USP6 rearrangement and has any atypical morphologic or immunohistochemical findings, it would be prudent to offer a narrowed differential diagnosis and defer final classification to the excision specimen.
A variety of methods have been utilized for the detection of USP6 gene rearrangements, including FISH [3, 4, 6], RT-PCR [3, 4], and RNA sequencing [4]. Of these methodologies, FISH is particularly useful in the setting of limited tissue, as only 1–2 tissue sections are needed. RNA sequencing may offer several advantages over FISH, including the ability to identify “cryptic” rearrangements, the potential to identify a multitude of other possible gene fusions, and the ability to characterize both constituent genes of the fusion. In approximately two-thirds of reported cases, USP6 is fused with MYH9 on chromosome 22q12.3 [3]. In our study, an MYH9-USP6 fusion was detected in half of the cases in which the partner gene was characterized by RNA sequencing. Consistent with prior reports [3, 4], these fusions result in juxtaposition of the noncoding exon 1 of MYH9, adjacent to the gene’s promoter region, to the full-length coding sequence of USP6. This “promoter swap” positions USP6 under the transcriptional control of the strong ectopic promoter of MYH9 ([3, 4]). The resulting overexpression of USP6 is thought to be one possible mechanism that drives cell proliferation in nodular fasciitis [3].
Our study also identified several non-canonical USP6 gene fusions in nodular fasciitis. In case 4, USP6 was fused to CTNNB1, the gene encoding beta-catenin. This fusion was recently reported in one case of nodular fasciitis arising in the neck of a 21-year-old woman [4]. The remaining three fusion partners identified in our series were NACA, LDHA, and SLFN11. To our knowledge, fusions involving these genes and USP6 have not been previously reported. NACA encodes a chaperone protein that binds to nascent polypeptide chains [37]. The product of LDHA, lactate dehydrogenase A, plays a critical role in glycolysis by catalyzing the conversion of lactate to pyruvate [38]. SLFN11 encodes a DNA/RNA helicase that has been linked to the sensitization of cancer cells to DNA damaging agents [39]. A similar promoter swap event occurred in these four cases, in which the noncoding first exons of CTNNB1, NACA, LDHA, or SLFN11 were fused upstream of the full-length USP6 coding region. Given that these genes encode proteins with important cellular housekeeping functions, they are expected to have active promoters to induce USP6 overexpression and subsequent neoplasia. Our novel findings add to the growing body of literature that emphasizes the impressive genetic plasticity of USP6-rearranged neoplasms, which includes nodular fasciitis [4, 5], fibroma of tendon sheath [40], and aneurysmal bone cyst [41,42,43].
All of the cases in our study, including those with non-canonical USP6 fusions, followed benign clinical courses with no recurrences. Moreover, two lesions with novel fusion partners (LDHA and SLFN11) self-resolved without surgical excision. Another lesion that was negative for USP6 rearrangement also reportedly self-resolved. This is consistent with other reports of self-resolving cases of mammary nodular fasciitis (see Table 2). The mechanism underlying spontaneous resolution is not well understood. Among nodular fasciitis cases, there has been a single report of a histologically typical tumor associated with a more aggressive clinical course, including multiple recurrences and eventual metastases over a period of 10 years [5]. This case arose in the thigh and harbored an unusual amplified USP6 gene fusion involving PPP6R3. This striking report demonstrates that in exceptional cases nodular fasciitis may follow a more aggressive clinical course. More studies are necessary to determine if this distinctive behavior is due to a specific 5′ gene partner, secondary amplification of the USP6 fusion, or other alteration.
Accurate classification of spindle cell lesions of the breast is critical for guiding surgical and oncologic decision-making. This study highlights the importance of considering nodular fasciitis in the differential diagnosis of mammary spindle cell lesions. Arriving at the correct diagnosis and avoiding misclassification as malignancy relies on recognition of the spectrum of histopathologic features of nodular fasciitis with appreciation that lesions can be mitotically active and infiltrative appearing. Judicious use of immunohistochemistry is suggested to exclude more aggressive histologic mimics, especially metaplastic carcinoma. In difficult cases, molecular tools such as USP6 FISH or RNA sequencing can be particularly helpful to establish the diagnosis and prevent potentially unnecessary surgical intervention.
Data availability
Data generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Oliveira A, Wang J, Wang W. Nodular fasciitis. In: Antonescu CR, Bridge JA, Cunha IW, Dei Tos AP, Fletcher CDM, Folpe AL, et al, (eds). WHO Classification of Tumours: Soft Tissue and Bone Tumours. 5th edn. Lyon (France): International Agency for Research of Cancer; 2020. p. 49–50.
Montgomery EA, Meis JM. Nodular fasciitis: its morphologic spectrum and immunohistochemical profile. J Surg Pathol. 1991;15:942–8.
Erickson-Johnson MR, Chou MM, Evers BR, Roth CW, Seys AR, Jin L, et al. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011;91:1427–33.
Patel NR, Chrisinger JSA, Demicco EG, Sarabia SF, Reuther J, Kumar E, et al. USP6 activation in nodular fasciitis by promoter-swapping gene fusions. Mod Pathol. 2017;30:1577–88.
Guo R, Wang X, Chou MM, Asmann Y, Wenger DE, Al‐Ibraheemi A, et al. PPP6R3-USP6 amplification: novel oncogenic mechanism in malignant nodular fasciitis. Genes Chromosomes Cancer. 2016;55:640–9.
Amary MF, Ye H, Berisha F, Tirabosco R, Presneau N, Flanagan AM. Detection of USP6 gene rearrangement in nodular fasciitis: an important diagnostic tool. Virchows Arch. 2013;463:97–98.
Lu L, Lao IW, Liu X, Yu L, Wang J. Nodular fasciitis: a retrospective study of 272 cases from China with clinicopathologic and radiologic correlation. Ann Diagn Pathol. 2015;19:180–5.
Wong NL, Di F. Pseudosarcomatous fasciitis and myositis: diagnosis by fine-needle aspiration cytology. Am J Clin Pathol. 2009;132:857–65.
Konwaler BE, Keasbey L, Kaplan L. Subcutaneous pseudosarcomatous fibromatosis (fasciitis). Am J Clin Pathol. 1955;25:241–52.
Erber R, Agaimy A. Misses and near misses in diagnosing nodular fasciitis and morphologically related reactive myofibroblastic proliferations: experience of a referral center with emphasis on frequency of USP6 gene rearrangements. Virchows Arch. 2018;473:351–60.
Brown V, Carty NJ. A case of nodular fascitis of the breast and review of the literature. Breast. 2005;14:384–7.
Dahlstrom J, Buckingham J, Bell S, Jain S. Nodular fasciitis of the breast simulating breast cancer on imaging. Australas Radio. 2001;45:67–70.
Erinanc H, Türk E. The rare benign lesion that mimics a malignant tumor in breast parenchyma: nodular fasciitis of the breast. Case Rep Pathol. 2018;1612587.
Green JS, Crozier AEC, Walker RA. Case report: nodular fasciitis of the breast. Clin Radio. 1997;52:961–2.
Hayashi S, Yasuda S, Takahashi N, Okazaki S, Ishibashi K, Kitada M, et al. Nodular fasciitis of the breast clinically resembling breast cancer in an elderly woman: a case report. J Med Case Rep. 2017;11:57.
Kang A, Kumar JB, Thomas A, Bourke AG. A spontaneously resolving breast lesion: imaging and cytological findings of nodular fasciitis of the breast with FISH showing USP6 gene rearrangement. BMJ Case Rep. 2015;2015.
Naso JR, Chiu CG, Goecke ME, Chang D, Shiau CJ. Benign spindle cell lesions of the breast: a diagnostic approach to solitary fibrous tumour, nodular pseudoangiomatous stromal hyperplasia and nodular fasciitis. J Clin Pathol. 2019;72:438–42.
Ozben V, Aydogan F, Karaca FC, Ilvan S, Uras C. Nodular fasciitis of the breast previously misdiagnosed as breast carcinoma. Breast Care. 2009;4:401–2.
Paliogiannis P, Cossu A, Palmieri G, Scognamillo F, Pala C, Nonnis R, et al. Breast nodular fasciitis: a comprehensive review. Breast Care. 2016;11:270–4.
Dobin A, Davis CA, Schlesinger F, Drenkow J, Zaleski C, Jha S, et al. STAR: ultrafast universal RNA-seq aligner. Bioinforma Oxf Engl. 2013;29:15–21.
Yang S-R, Lin C-Y, Stehr H, Long SR, Kong CS, Berry GJ, et al. Comprehensive genomic profiling of malignant effusions in patients with metastatic lung adenocarcinoma. J Mol Diagn. 2018;20:184–94.
Salib C, Edelman M, Lilly J, Fantasia JE, Yancoskie AE. USP6 gene rearrangement by FISH analysis in cranial fasciitis: a report of three cases. Head Neck Pathol. 2020;14:257–61.
Karim RZ, Brogi E, Liegl-Atzwanger B, Shin SJ. Nodular fasciitis. In: Goldblum JR, Lazar AJ, Schnitt SJ, Tan PH, (eds). WHO Classification of Tumours: Breast Tumours. 5th edn. Lyon (France): International Agency for Research of Cancer; 2019. p. 202–3.
Krings G, McIntire P, Shin SJ. Myofibroblastic, fibroblastic and myoid lesions of the breast. Semin Diagn Pathol. 2017;34:427–37.
Allen PW. Nodular fasciitis. Pathology. 1972;4:9–26.
Stanley MW, Skoog L, Tani EM, Horwitz CA. Nodular fasciitis: spontaneous resolution following diagnosis by fine-needle aspiration. Diagn Cytopathol. 1993;9:322–4.
Chen J, Ye X, Li Y, Wei C, Zheng Q, Zhong P, et al. Chromosomal translocation involving USP6 gene in nodular fasciitis. Zhonghua Bing Li Xue Za Zhi. 2014;43:533–6.
Paker I, Kokenek TD, Kacar A, Ceyhan K, Alper M. Fine needle aspiration cytology of nodular fasciitis presenting as a mass in the male breast: report of an unusual case. Cytopathology. 2013;24:201–3.
Son YM, Nahm JH, Moon HJ, Kim MJ, Kim E-K. Imaging findings for malignancy-mimicking nodular fasciitis of the breast and a review of previous imaging studies. Acta Radio Short Rep. 2013;2:2047981613512830.
Rhee SJ, Ryu JK, Kim JH, Lim S-J. Nodular fasciitis of the breast: two cases with a review of imaging findings. Clin Imaging. 2014;38:730–3.
Yamamoto S, Chishima T, Adachi S. Nodular fasciitis of the breast mimicking breast cancer. Case Rep. Surg. 2014;2014:747951.
Samardzic D, Chetlen A, Malysz J. Nodular fasciitis in the axillary tail of the breast. J Radio Case Rep. 2014;8:16–26.
Sakuma T, Matsuo K, Koike S, Tagami K. Fine needle aspiration cytology of nodular fasciitis of the breast. Diagn Cytopathol. 2015;43:222–9.
Shin C, Low I, Ng D, Oei P, Miles C, Symmans P. USP6 gene rearrangement in nodular fasciitis and histological mimics. Histopathology. 2016;69:784–91.
Moghimi M, Yazdian Anari P, Vaghefi M, Meidany A, Salehi H. Nodular fasciitis of the breast. Iran J Radio Q J Publ Iran Radio Soc. 2016;13:e18774.
Knight JA, Hunt KN, Carter J. Nodular fasciitis of the breast in an elderly woman. Radio Case Rep. 2017;12:642–4.
Wiedmann B, Sakai H, Davis TA, Wiedmann M. A protein complex required for signal-sequence-specific sorting and translocation. Nature. 1994;370:434–40.
Chung FZ, Tsujibo H, Bhattacharyya U, Sharief FS, Li SS. Genomic organization of human lactate dehydrogenase-A gene. Biochem J. 1985;231:537–41.
Zoppoli G, Regairaz M, Leo E, Reinhold WC, Varma S, Ballestrero A, et al. Putative DNA/RNA helicase Schlafen-11 (SLFN11) sensitizes cancer cells to DNA-damaging agents. Proc Natl Acad Sci USA. 2012;109:15030–5.
Mantilla JG, Gross JM, Liu YJ, Hoch BL, Ricciotti RW. Characterization of novel USP6 gene rearrangements in a subset of so-called cellular fibroma of tendon sheath. Mod Pathol. 2021;34:13–19.
Oliveira AM, Perez-Atayde AR, Inwards CY, Medeiros F, Derr V, Hsi B-L, et al. USP6 and CDH11 oncogenes identify the neoplastic cell in primary aneurysmal bone cysts and are absent in so-called secondary aneurysmal bone cysts. Am J Pathol. 2004;165:1773–80.
Oliveira AM, Perez-Atayde AR, Dal Cin P, Gebhardt MC, Chen C-J, Neff JR, et al. Aneurysmal bone cyst variant translocations upregulate USP6 transcription by promoter swapping with the ZNF9, COL1A1, TRAP150, and OMD genes. Oncogene. 2005;24:3419–26.
Panagopoulos I, Gorunova L, Andersen K, Lobmaier I, Lund-Iversen M, Micci F, et al. Fusion of the lumican (LUM) gene with the ubiquitin specific peptidase 6 (USP6) gene in an aneurysmal bone cyst carrying a t(12;17)(q21;p13) chromosome translocation. Cancer Genomics Proteom. 2020;17:555–61.
Acknowledgements
The authors would like to thank Grace Allard and Shirley Kwok for histology work; Ivy Mangonon and Ellen Gomulia for assistance with immunohistochemistry; Sara Hartinger and the Stanford Molecular Pathology Laboratory for assistance with RNA sequencing; the Mayo Cytogenetics Core, Director Patricia T. Greipp, Sara Kloft-Nelson, and Ryan Knudson for technical assistance with USP6 FISH; Drs. Richard Sibley, Robert West, and Shine Yun for case contribution; and Norm Cyr for help with figures.
Funding
GRB is supported in part by departmental startup funds, which covered the costs of this work.
Author information
Authors and Affiliations
Contributions
JMC and GRB designed the study and wrote the manuscript; JMC, CAK, GWC, EMH, JJG, RAB, MLT, KHA, and GRB acquired and analyzed the data; all authors read and approved the final paper.
Corresponding author
Ethics declarations
Ethics approval/consent to participate
This study was performed in accordance with research policies approved by the Institutional Review Boards of Stanford University and Kaiser Permanente San Francisco.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Cloutier, J.M., Kunder, C.A., Charville, G.W. et al. Nodular fasciitis of the breast: clinicopathologic and molecular characterization with identification of novel USP6 fusion partners. Mod Pathol 34, 1865–1875 (2021). https://doi.org/10.1038/s41379-021-00844-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-021-00844-4
This article is cited by
-
Nodular fasciitis of the breast: the report of three cases
BMC Women's Health (2022)