Abstract
Malignant peritoneal mesothelioma historically carried a grim prognosis, but outcomes have improved substantially in recent decades. The prognostic significance of clinical, morphologic, and immunophenotypic features remains ill-defined. This multi-institutional cohort comprises 225 malignant peritoneal mesotheliomas, which were assessed for 21 clinical, morphologic, and immunohistochemical parameters. For epithelioid mesotheliomas, combining nuclear pleomorphism and mitotic index yielded a composite nuclear grade, using a previously standardized grading system. Correlation of clinical, morphologic, and immunohistochemical parameters with overall and disease-free survival was examined by univariate and multivariate analyses. On univariate analysis, longer overall survival was significantly associated with diagnosis after 2000 (P = 0.0001), age <60 years (P = 0.0001), ECOG performance status 0 or 1 (P = 0.01), absence of radiographic lymph-node metastasis (P = 0.04), cytoreduction surgery (P < 0.0001), hyperthermic intraperitoneal chemotherapy (P = 0.0001), peritoneal carcinomatosis index <27 (P = 0.01), absence of necrosis (P = 0.007), and epithelioid histotype (P < 0.0001). Among epithelioid malignant mesotheliomas only, longer overall survival was further associated with female sex (P = 0.03), tubulopapillary architecture (P = 0.005), low nuclear pleomorphism (P < 0.0001), low mitotic index (P = 0.0007), and low composite nuclear grade (P < 0.0001). On multivariate analyses, the low composite nuclear grade was independently associated with longer overall and disease-free survival (P < 0.0001). Our data further clarify the interactions of clinical and pathologic features in peritoneal mesothelioma prognosis and validate the prognostic significance of a standardized nuclear-grading system in epithelioid malignant mesothelioma of the peritoneum.
Similar content being viewed by others
Introduction
Malignant mesothelioma is a rare neoplasm arising in the serosal lining of body cavities, with around 3000 new cases diagnosed annually in the United States. Although the pleura is the most common primary site, ~10% of mesotheliomas arise in the peritoneum [1, 2]. Pericardial and paratesticular mesothelioma each account for <1% of cases [3]. The incidence of peritoneal mesothelioma in the United States, Western Europe, and Australia has remained relatively stable for 40 years, at ~0.04–0.11 new diagnoses per 100,000 person-years among women, and 0.07–0.16 per 100,000 person-years among men [2, 4].
Mesotheliomas arising at different sites have distinct morphologic, molecular, and clinical profiles. Compared to pleural mesothelioma, peritoneal tumors occur more often in younger patients and women, are less often linked to asbestos exposure, and more often show epithelioid histotype [2, 5,6,7,8,9]. However, given its relative rarity, peritoneal mesothelioma has not been as well characterized as pleural mesothelioma.
Historically, options for management of peritoneal mesothelioma were limited, and clinical outcomes were correspondingly dismal, with median survival generally around 12 months after diagnosis [10,11,12,13]. However, increased use of cytoreductive surgery combined with intraoperative infusion of hyperthermic intraperitoneal chemotherapy has dramatically improved peritoneal mesothelioma outcomes over the past 30 years, with a median survival of 31–92 months among patients receiving this modern therapeutic approach [8, 10, 14,15,16,17,18]. Population-based studies provide compelling evidence that this improvement in survival is directly linked to more thorough cytoreduction and hyperthermic intraperitoneal chemotherapy [4, 8, 19], and prognosis remains poor in recent cohorts where these treatments have not been used [20, 21].
Despite recent improvements in survival, peritoneal mesothelioma remains an inexorable and incurable disease, with a societal burden magnified by the young median age at diagnosis. Furthermore, the disease shows a variable clinical course, as some patients succumb rapidly, while others experience a years-long relapsing course. Previous work has quite convincingly shown that longer survival in peritoneal mesothelioma is associated with female sex, younger age at diagnosis, and epithelioid histotype [4, 5, 10, 14,15,16,17,18, 20, 22, 23]. Although previous studies have examined the prognostic significance of nuclear features and mitotic rate in peritoneal mesothelioma, grading criteria and mitotic cutoffs have varied widely, and in some studies were left unspecified [11, 13,14,15,16,17, 22, 24,25,26,27,28,29,30,31,32].
In a recent study of 776 pleural mesotheliomas, our group reported that survival in pleural mesothelioma was strongly correlated with a standardized nuclear-grading system that combines nuclear pleomorphism and mitotic rate [33], as originally proposed by the Memorial Sloan Kettering Cancer Center (MSKCC) group in 2012 [34]. Given its multiple attestations in the literature and robust performance in the pleura, we hypothesized that this composite nuclear-grading system could also provide a reliable standard for morphologic prognosis in peritoneal mesothelioma. In this study, we assembled a large cohort of malignant peritoneal mesotheliomas from 11 institutions in 6 countries, undertook central pathology review and immunohistochemistry, and performed univariate and multivariate survival analyses to more robustly and comprehensively characterize prognostically relevant clinical, morphological, and immunohistochemical parameters in peritoneal malignant mesothelioma.
Materials and methods
Collaborating pathologists submitted cases of peritoneal malignant mesothelioma for this retrospective cohort study. Diagnoses of well-differentiated papillary mesothelioma and benign multicystic mesothelioma were excluded. Appropriate approvals were obtained from institutional review boards at participating institutions.
Clinical, surgical, and radiographic parameters
Clinical, surgical, and radiographic parameters are shown in Table 1. Data were retrieved from patient medical records by the submitting pathologist. Patients with pleural involvement were permitted only if recognition of pleural involvement followed the diagnosis of peritoneal mesothelioma, or if the peritoneal and pleural disease were identified simultaneously, but clinical and radiographic disease distribution favored peritoneal origin. Data on preoperative platelet count, preoperative serum CA-125, intraoperative assessment of ascites, completeness of first cytoreduction, and asbestos exposure (including fiber type and dose) were solicited, but were available in too few cases for analysis.
Some clinical parameters were further specified for statistical analyses:
-
1.
ECOG performance status at diagnosis was stratified as good (0 or 1) versus poor (2 or 3).
-
2.
Age was stratified by the cohort median into patients younger than 60 versus 60 years and older.
-
3.
Peritoneal carcinoma index (a continuous score ranging from 0 to 39, assigned at surgery based on presence and size of tumor deposits in 13 intraperitoneal zones) was divided into three groups: 0–13, 14–26, and 27–39.
Morphologic parameters
Morphologic parameters are shown in Table 1. Contributing pathologists submitted three hematoxylin and eosin-stained slides from each case for central pathology review by two pathologists (DBC, ANH). The diagnosis of malignant peritoneal mesothelioma was confirmed by morphology. To reduce sampling bias, reviewed slides were selected from different intraperitoneal sites and from cytoreduction specimens, when possible. Reviewed tissues were obtained prior to the administration of systemic or intraperitoneal chemotherapy.
Some morphologic parameters were further specified, as follows:
-
1.
Nuclear grading of epithelioid mesothelioma was performed, as previously described [33]. Briefly, nuclear pleomorphism was graded as mild (1 point), moderate (2 points), or marked (3 points). The number of mitoses per 10 high-power fields was divided into three groups: 0–1 (low mitotic index; 1 point), 2–4 (intermediate; 2 points), and >4 (high; 3 points). The sum of pleomorphism and mitotic index scores yielded a total score from 2 to 6, which was used to assign composite nuclear grade: score 2 or 3 = grade I; score 4 or 5 = grade II; score 6 = grade III.
-
2.
Architectural patterns recognized in epithelioid mesothelioma included tubulopapillary, papillary, micropapillary, trabecular, acinar, and solid. Percent contribution of each pattern was documented. Based on previous reports of prognostically significant architectural patterns [14, 17, 24, 28, 30, 31], the following architectural parameters were considered for statistical analysis: predominantly (>50%) solid growth, predominantly tubulopapillary growth, and any micropapillary growth.
Immunohistochemical parameters
Immunohistochemistry for BAP1 (Santa Cruz (sc-28383), C-4, 1:80) and Ki67 (DAKO (M7240), MIB1, 1:100) was performed centrally on unstained slides submitted by contributing pathologists. BAP1 was considered lost if tumor cells showed a complete absence of nuclear staining in the presence of positive internal control. Ki67 index refers to the percentage of tumor cells with positive nuclear staining. Based on previously published cutoffs [35], tumors were divided into three groups for analysis: 0–9%, 10–17%, and >17% tumor nuclei staining for Ki67. Immunostains were not performed on tumors diagnosed before 2000, due to inconsistent tissue antigenicity.
Cases from one institution were not available for central review, and morphologic and immunohistochemical parameters were provided by the submitting pathologists (YPH, MM-K).
Outcomes
Overall survival was defined as the interval between the date of pathologic diagnosis and date of death or last follow-up. Disease-free survival was defined as the interval between the date of first cytoreduction and date of first clinical, surgical, or radiographic recurrence (or date of death or last follow-up for patients documented to have no recurrence). Patients not undergoing cytoreduction were not included in analyses of disease-free survival.
Subcohort construction
Cases were divided into two subcohorts for analysis, based on anticipated differences in pathobiology and clinical behavior:
-
1.
Malignant mesotheliomas diagnosed after 2000 (n = 186)
-
2.
Malignant mesotheliomas diagnosed before 2000 (n = 39; diagnosed 1970–1996).
Data on performance status, pleural involvement, radiographic lymph node involvement, cytoreduction, peritoneal carcinomatosis index, and systemic chemotherapy were not available for the subcohort diagnosed before 2000.
Statistical analysis
All statistical analyses were performed in SAS 9.4 (SAS Institute, Cary, NC), with P < 0.05 considered significant. Statistical associations between individual parameters were compared by Chi-squared test and Student’s t test, as appropriate. Univariate survival analyses were performed by log-rank test, with hazard ratios generated by univariate Cox proportional hazard regression. Multiple comparisons were corrected by Holm’s method. Parameters significantly associated with survival on univariate analysis were entered into a multivariate Cox proportional hazards regression model using stepwise inclusion. To maintain statistical power, peritoneal carcinomatosis index and performance status were not included in multivariate analyses. Although overall survival by histotype was determined for all patients, only patients diagnosed with mesothelioma after 2000 were included in more detailed survival analyses, due to significant differences in demographic, clinical, and pathologic features seen in patients diagnosed before 2000 (see Table 2).
Results
Clinical characteristics
Clinical comparisons of malignant mesotheliomas diagnosed before and after 2000 are shown in Table 2. Compared to those diagnosed before 2000, patients diagnosed after 2000 were significantly younger at diagnosis and were more often female. No patients diagnosed before 2000 received hyperthermic intraperitoneal chemotherapy, compared to 53% of patients diagnosed after 2000.
Morphologic characteristics
Morphologic comparisons of malignant mesotheliomas diagnosed before and after 2000 are shown in Table 2. Among malignant mesotheliomas diagnosed after 2000, 94% showed epithelioid histotype, of which 53%, 39%, and 8% were grade I, grade II, and grade III, respectively (Fig. 1).
Compared to malignant mesotheliomas diagnosed before 2000, those diagnosed after 2000 had a lower proportion of biphasic and sarcomatoid tumors and lower prevalence of tumor necrosis. Epithelioid tumors diagnosed after 2000 had a lower prevalence of high nuclear pleomorphism, but no significant difference in mitotic index, composite nuclear grade, or architecture.
Immunohistochemical characteristics
Immunohistochemical data for malignant mesotheliomas diagnosed after 2000 are shown in Table 3. BAP1 loss was significantly more common in epithelioid compared to biphasic tumors, and BAP1 was retained in the sole sarcomatoid tumor. There was a trend toward higher Ki67 index in biphasic compared to epithelioid tumors, but power was limited by the low number of biphasic tumors.
Overall survival by year of diagnosis
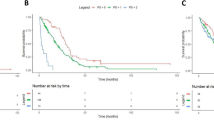
Comparisons of overall survival by tumor histotype and year of diagnosis are shown in Table 4. Overall survival was significantly longer in epithelioid malignant mesothelioma than in biphasic and sarcomatoid tumors (irrespective of diagnosis before or after 2000), and significantly longer for patients diagnosed after 2000 than for those diagnosed before 2000 (irrespective of histotype) (Fig. 2a; P < 0.001 for all pairwise comparisons). When comparing only those patients who did not undergo cytoreduction or hyperthermic intraperitoneal chemotherapy (i.e., correcting for the anticipated effect of this therapeutic regimen in more recently diagnosed cases), overall survival was still significantly longer in patients diagnosed after 2000 versus before 2000 (21 versus 7 months, respectively; P = 0.0006).
a Overall survival was significantly longer for epithelioid versus biphasic or sarcomatoid tumors, and significantly longer for diagnosis after versus before 2000 (P < 0.001 for all pairwise comparisons) (a). Among all malignant mesotheliomas diagnosed after 2000, longer overall survival was significantly associated with younger age at diagnosis (b), good performance status, absence of radiographic evidence of lymph node metastasis (c), cytoreduction surgery (d), hyperthermic intraperitoneal chemotherapy (e), low peritoneal carcinomatosis index, and absence of tumor necrosis. Among epithelioid mesotheliomas only, longer overall survival was further associated with female sex, tubulopapillary architecture (f), lower nuclear pleomorphism, lower mitotic index, lower composite nuclear grade (g; P < 0.0001 for all pairwise comparisons), and lower Ki67 index. On multivariate analysis, histotype and composite nuclear grade are independently associated with overall survival (P < 0.0001 for both parameters). Note the near-total overlap of the survival curves for grade III epithelioid malignant mesothelioma and biphasic mesothelioma (h). BMM biphasic malignant mesothelioma, EMM epithelioid malignant mesothelioma, G1 composite nuclear grade I, G2 composite nuclear grade II, G3 composite nuclear grade III, HIPEC hyperthermic intraperitoneal chemotherapy, SMM sarcomatoid malignant mesothelioma.
Overall survival: univariate and multivariate analyses
All malignant mesotheliomas
On univariate analyses of overall survival among malignant mesotheliomas diagnosed after 2000 (n = 186), longer overall survival was significantly associated with younger age (Fig. 2b), better performance status, absence of lymph node metastasis by radiology (Fig. 2c), cytoreduction surgery (Fig. 2d), hyperthermic intraperitoneal chemotherapy (Fig. 2e), peritoneal carcinomatosis index <27, absence of necrosis, and epithelioid histotype. The results are shown in Table 5.
In a multivariate model correcting for age, longer overall survival was independently associated with cytoreduction surgery, non-sarcomatoid histotype, and absence of necrosis. The results are shown in Table 6.
Epithelioid malignant mesotheliomas only
On univariate analyses of only epithelioid malignant mesotheliomas diagnosed after 2000 (n = 168), longer overall survival was significantly associated with all parameters significant in the total cohort (see preceding section), as well as female sex, tubulopapillary architecture (Fig. 2f), lower nuclear pleomorphism, low mitotic index, lower composite nuclear grade (Fig. 2g), and low Ki67 index. The results are shown in Table 5.
In a multivariate model correcting for sex, age, necrosis, nuclear pleomorphism, mitotic index, and solid architecture, longer overall survival was independently associated with cytoreduction surgery, lower composite nuclear grade, and tubulopapillary architecture. Necrosis was not independently associated with overall survival among epithelioid mesotheliomas only. The results are shown in Table 6.
Strikingly, when histotype was added and this multivariate model was plotted for histotype and composite nuclear grade (for epithelioid tumors), the survival curves for grade III epithelioid malignant mesothelioma and biphasic malignant mesothelioma essentially overlapped (Fig. 2h).
Cytoreduced and hyperthermic intraperitoneal chemotherapy-treated malignant mesotheliomas only
Among only those patients undergoing cytoreduction and hyperthermic intraperitoneal chemotherapy (n = 104; 99 epithelioid and 5 biphasic tumors), associations between overall survival and clinical, morphologic, and immunohistochemical parameters closely mirrored the associations seen for all epithelioid malignant mesotheliomas. The results are shown in Supplementary Table 1.
Although not statistically significant, the 5 biphasic mesotheliomas that underwent both cytoreduction and hyperthermic intraperitoneal chemotherapy had longer median overall survival than the 12 biphasic tumors treated more conservatively (63 versus 12 months, respectively). This is consistent with reports that select biphasic tumors show substantial clinical benefit from these therapies [36].
Disease-free survival: univariate and multivariate analyses
All malignant mesotheliomas
On univariate analyses of all cytoreduced malignant mesotheliomas with recurrence data (n = 115), longer disease-free survival was significantly associated with low peritoneal carcinomatosis index, epithelioid histotype, absence of necrosis, and low Ki67 index. The results are shown in Table 7.
In a multivariate model correcting for histotype and necrosis, only low Ki67 index was independently associated with longer disease-free survival. The results are shown in Table 8.
Epithelioid malignant peritoneal mesotheliomas only
On univariate analyses of cytoreduced epithelioid malignant mesotheliomas with recurrence data (n = 107), longer disease-free survival was significantly associated with the absence of lymph node metastasis by radiology, low peritoneal carcinomatosis index, absence of necrosis, low nuclear pleomorphism, low mitotic index, lower composite nuclear grade, and low Ki67 index. The results are shown in Table 7.
In a multivariate model correcting for necrosis, nuclear pleomorphism, and mitotic index, longer disease-free survival was independently associated with low composite nuclear grade (grade I) and low Ki67 index. The results are shown in Table 8.
Discussion
Peritoneal mesothelioma is an exceptionally rare tumor. As a result, although many studies on the topic have been published in the last 30 years, only a few fundamental clinicopathologic properties of peritoneal mesothelioma are well established in the literature. This large multi-institutional peritoneal mesothelioma cohort builds on earlier work regarding improved prognosis in recent decades. More importantly, our data provide adequate statistical power to address questions regarding prognostically relevant morphologic and immunohistochemical parameters.
Our comparisons of patients diagnosed before and after the year 2000 emphasize the markedly improved outlook for peritoneal mesothelioma patients diagnosed in the past 20 years. This improvement is in large part directly linked to increased use of cytoreduction and hyperthermic intraperitoneal chemotherapy [8]. In large population-based studies in the Netherlands and United States, cytoreduction with hyperthermic intraperitoneal chemotherapy was associated with significantly longer survival than cytoreduction alone, systemic chemotherapy alone, or cytoreduction with systemic chemotherapy, and increased use of cytoreduction with hyperthermic intraperitoneal chemotherapy over time correlated with a significant improvement in overall survival among all peritoneal mesothelioma patients [19, 37]. A recent analysis of 16 French cancer registries likewise showed significantly better overall survival among peritoneal mesothelioma patients diagnosed after 2000, although correlation with therapies was not attempted [4]. Notwithstanding, these population-based data indicate that a majority of peritoneal mesothelioma patients in countries with highly developed medical capabilities still do not receive cancer-directed therapy [19, 37], highlighting substantial room for improvement in patient outcomes.
Our data further indicate that improved prognosis in recent decades is not solely due to cytoreduction and hyperthermic intraperitoneal chemotherapy. Among patients not receiving these interventions, median survival was still three times longer among patients diagnosed after 2000, compared to those diagnosed before. This residual improvement in prognosis, independent of treatment modality, appears linked in the literature to a gradual decrease in the proportion of [1] non-epithelioid tumors, [2] asbestos-related tumors, [3] diagnoses in men, and [4] diagnoses in older patients—all of which have been associated with poorer prognosis in earlier studies [1, 5, 7, 13, 14, 16, 17, 20, 23, 38].
Our data indicate that a composite nuclear-grading system based on nuclear pleomorphism and the mitotic rate has prognostic value in epithelioid malignant mesothelioma of the peritoneum. Among 21 clinical and pathologic parameters evaluated, the composite nuclear grade was the only variable independently associated with both overall and disease-free survival on multivariate analysis. Furthermore, the almost complete overlap of survival curves for biphasic mesothelioma and grade III epithelioid mesothelioma emphasizes the prognostic relevance of nuclear grading to identify the latter.
Although some previous studies of peritoneal mesothelioma have reported a prognostic role for nuclear pleomorphism or mitotic rate, each of these earlier studies used a different grading system [14,15,16,17, 22, 24,25,26,27,28,29,30]. The composite grading system employed in this study was first proposed for epithelioid pleural mesothelioma by the MSKCC group in 2012 [34], and aims to standardize nuclear grading among pathologists. One study of 51 peritoneal mesotheliomas showed that a modified two-tier variant of the MSKCC grading system was correlated with overall and progression-free survival on univariate analysis [32], but was underpowered to assess a three-tier grading system and for multivariate analysis. Accordingly, this study is the first to demonstrate that the prognostic significance of composite nuclear grade is independent of numerous other clinical and pathologic parameters, and to show that each of the three nuclear grades in the MSKCC system is statistically distinct [34].
Our working group also recently validated the MSKCC composite nuclear-grading system in a large multi-institutional cohort of epithelioid pleural mesothelioma [33], which could permit the application of a single nuclear-grading system to both pleural and peritoneal epithelioid mesotheliomas. However, in contrast to our recent large study of pleural mesothelioma [33], necrosis does not appear to have an independent prognostic role in epithelioid mesothelioma of the peritoneum, and a recent consensus recommendation to incorporate necrosis into pleural mesothelioma risk stratification is not presently applicable to peritoneal tumors [39].
Although BAP1 loss appears to be a positive prognostic finding in pleural mesothelioma, this remains unsubstantiated in peritoneal mesothelioma [40, 41]. Our data provide additional evidence that immunohistochemical loss of BAP1 is not associated with improved prognosis in peritoneal mesothelioma, as patients with and without BAP1 loss had virtually identical overall survival—34 and 36 months, respectively. The reason for this apparent difference between pleural and peritoneal mesothelioma is unclear and may reflect an underlying biological difference, masking of a positive prognostic effect by improved treatment options for peritoneal tumors, or a combination of factors. Of note, BAP1 germline mutation is associated with improved prognosis in both pleural and peritoneal mesothelioma [42], but immunohistochemistry does not distinguish germline from somatic loss, and germline sequencing was not available for this study. One recent study showed that peritoneal mesothelioma with BAP1 haploinsufficiency constitutes a uniquely immunogenic tumor subset that may be more susceptible to immune checkpoint inhibition, suggesting that BAP1 immunohistochemistry may ultimately have a predictive role [43].
Routine application of Ki67 immunohistochemistry for prognostic stratification of peritoneal mesothelioma remains an area of uncertainty, and standardized prognostic cutoffs for the Ki67 index are undefined. Nonetheless, all studies of the Ki67 index in peritoneal mesothelioma have found a significant association between a higher Ki67 index and poorer prognosis [18, 35, 44, 45]. The most statistically robust study reported three prognostically significant Ki67 strata, with cutoffs at 9% and 17% [35]. Three additional studies found that a higher Ki67 index was independently associated with shorter survival on multivariate analysis, but the three studies used different cutoffs—5% in one, 10% in a second, 25% in a third [18, 44, 45]. We could obtain Ki67 index in only a subset of cases, and our findings are somewhat mixed, but on multivariate analyses higher Ki67 was associated only with shorter disease-free survival. Overall, our data generally suggest that a two-tier Ki67 prognostic stratification is likely as informative as a three-tier system, but further study is necessary for standardization.
Our data also contain some pertinent negatives. As discussed above, we did not find necrosis to be independently associated with overall survival in epithelioid malignant mesothelioma, in contrast to recent work on pleural mesothelioma [33]. We also found no adverse impact of pleural involvement on survival. This finding is in keeping with a recent study of bicavitary mesothelioma [46], and may reflect the increased incidence of bicavitary disease in patients with a prognostically favorable BAP1 germline mutation.
This study has some caveats and limitations:
-
1.
To promote uptake and reproducibility, we elected to validate an existing pleural mesothelioma grading system in peritoneal mesothelioma. The independent prognostic value of this system in peritoneal mesothelioma appears to support our choice. However, given clinical and biological differences between pleural and peritoneal tumors, it is conceivable that certain morphologic parameters in a peritoneal-specific grading system might differ from those in the original pleural model. The development of a novel peritoneal-specific grading system and head-to-head comparison with the system used here should be examined in additional studies.
-
2.
Because clinical data were retrospectively collected from electronic medical records at multiple institutions, two variables significantly associated with survival on univariate analysis (peritoneal carcinomatosis index and ECOG performance status) could not be included in multivariate models.
-
3.
Our morphologic analyses were limited to pre-treatment surgical specimens, and are not validated for post-treatment material.
-
4.
Although central pathology review increases internal validity, available data suggest that interobserver agreement for architectural pattern, nuclear pleomorphism, and mitotic index in peritoneal mesothelioma is fair, at best [47], which may limit the implementation of nuclear grading.
-
5.
Certain rare histotypes are not well represented in this cohort. Of 186 tumors diagnosed after 2000, only one had pure sarcomatoid morphology, limiting analyses of the sarcomatoid histotype [1]. We also identified no cases with heterologous elements—an exceptionally rare finding, generally limited to the tumor with a sarcomatoid element and associated with poor outcome [48]. And although the tunica vaginalis is an anatomic extension of the peritoneum, paratesticular mesotheliomas were excluded from this cohort, as available data indicate that they are clinicopathologically distinct from mesothelioma of the peritoneum proper [3].
-
6.
Numerous prognostic immunomarkers have been reported in single studies (including GLUT1, MUC1, BCL2, IMP3, EGFR, and PTEN) [49,50,51,52,53]. These were not included in our analysis, but may warrant further investigation.
In summary, this study substantiates published reports of treatment- and histotype-specific survival in peritoneal mesothelioma; validates an increasingly codified composite nuclear-grading system for use in peritoneal mesothelioma; and provides further insights into the prognostic relevance of BAP1 and Ki67 immunostaining. More broadly, our data emphasize that pathologic parameters have independent prognostic value, and that clinical and pathologic features cannot be assessed in isolation when caring for peritoneal mesothelioma patients. Given the complex interplay of clinical and pathologic factors, communication may be best facilitated by a dedicated multidisciplinary tumor board to bring together the unique combination of specialized surgeons, oncologists, radiologists, and pathologists involved in diagnosis and management of peritoneal mesothelioma patients.
References
Pavlisko EN, Roggli VL. Sarcomatoid peritoneal mesothelioma: clinicopathologic correlation of 13 cases. Am J Surg Pathol. 2015;39:1568–75.
Soeberg MJ, Creighton N, Currow DC, Young JM, van Zandwijk N. Patterns in the incidence, mortality and survival of malignant pleural and peritoneal mesothelioma, New South Wales, 1972–2009. Aust N. Z J Public Health. 2016;40:255–62.
Butnor KJ, Pavlisko EN, Sporn TA, Roggli VL. Mesothelioma of the tunica vaginalis testis. Hum Pathol. 2019;92:48–58.
Le Stang N, Bouvier V, Glehen O, Villeneuve L, Galateau-Salle F, Clin B. Incidence and survival of peritoneal malignant mesothelioma between 1989 and 2015: a population-based study. Cancer Epidemiol. 2019;60:106–11.
Antman K, Shemin R, Ryan L, Klegar K, Osteen R, Herman T, et al. Malignant mesothelioma: prognostic variables in a registry of 180 patients, the Dana-Farber Cancer Institute and Brigham and Women’s Hospital experience over two decades, 1965–1985. J Clin Oncol. 1988;6:147–53.
Thomas A, Chen Y, Yu T, Gill A, Prasad V. Distinctive clinical characteristics of malignant mesothelioma in young patients. Oncotarget. 2015;6:16766–73.
Goldblum J, Hart WR. Localized and diffuse mesotheliomas of the genital tract and peritoneum in women. A clinicopathologic study of nineteen true mesothelial neoplasms, other than adenomatoid tumors, multicystic mesotheliomas, and localized fibrous tumors. Am J Surg Pathol. 1995;19:1124–37.
Helm JH, Miura JT, Glenn JA, Marcus RK, Larrieux G, Jayakrishnan TT, et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for malignant peritoneal mesothelioma: a systematic review and meta-analysis. Ann Surg Oncol. 2015;22:1686–93.
Pavlisko EN, Liu B, Green C, Sporn TA, Roggli VL. Malignant diffuse mesothelioma in women: a study of 354 cases. Am J Surg Pathol. 2020;44:293–304.
Sebbag G, Yan H, Shmookler BM, Chang D, Sugarbaker PH. Results of treatment of 33 patients with peritoneal mesothelioma. Br J Surg. 2000;87:1587–93.
Sebbag G, Sugarbaker PH. Peritoneal mesothelioma proposal for a staging system. Eur J Surg Oncol. 2001;27:223–4.
Jones DE, Silver D. Peritoneal mesotheliomas. Surgery. 1979;86:556–60.
Clement PB, Young RH, Scully RE. Malignant mesotheliomas presenting as ovarian masses. A report of nine cases, including two primary ovarian mesotheliomas. Am J Surg Pathol. 1996;20:1067–80.
Feldman AL, Libutti SK, Pingpank JF, Bartlett DL, Beresnev TH, Mavroukakis SM, et al. Analysis of factors associated with outcome in patients with malignant peritoneal mesothelioma undergoing surgical debulking and intraperitoneal chemotherapy. J Clin Oncol. 2003;21:4560–7.
Yan TD, Brun EA, Cerruto CA, Haveric N, Chang D, Sugarbaker PH. Prognostic indicators for patients undergoing cytoreductive surgery and perioperative intraperitoneal chemotherapy for diffuse malignant peritoneal mesothelioma. Ann Surg Oncol. 2007;14:41–9.
Magge D, Zenati MS, Austin F, Mavanur A, Sathaiah M, Ramalingam L, et al. Malignant peritoneal mesothelioma: prognostic factors and oncologic outcome analysis. Ann Surg Oncol. 2014;21:1159–65.
Alexander HR Jr., Bartlett DL, Pingpank JF, Libutti SK, Royal R, Hughes MS, et al. Treatment factors associated with long-term survival after cytoreductive surgery and regional chemotherapy for patients with malignant peritoneal mesothelioma. Surgery. 2013;153:779–86.
Baratti D, Kusamura S, Cabras AD, Bertulli R, Hutanu I, Deraco M. Diffuse malignant peritoneal mesothelioma: long-term survival with complete cytoreductive surgery followed by hyperthermic intraperitoneal chemotherapy (HIPEC). Eur J Cancer. 2013;49:3140–8.
de Boer NL, van Kooten JP, Damhuis RAM, Aerts JGJV, Verhoef C, Madsen EVE. Malignant peritoneal mesothelioma: patterns of care and survival in the Netherlands: a population-based study. Ann Surg Oncol. 2019;26:4222–8.
Mirabelli D, Roberti S, Gangemi M, Rosato R, Ricceri F, Merler E, et al. Survival of peritoneal malignant mesothelioma in Italy: a population-based study. Int J Cancer. 2009;124:194–200.
de Pangher Manzini V. Malignant peritoneal mesothelioma. Tumori J. 2005;91:1–5.
Borczuk AC, Taub RN, Hesdorffer M, Hibshoosh H, Chabot JA, Keohan ML, et al. P16 loss and mitotic activity predict poor survival in patients with peritoneal malignant mesothelioma. Clin Cancer Res. 2005;11:3303–8.
Cao C, Yan TD, Deraco M, Elias D, Glehen O, Levine EA, et al. Importance of gender in diffuse malignant peritoneal mesothelioma. Ann Oncol. 2012;23:1494–8.
Cerruto CA, Brun EA, Chang D, Sugarbaker PH. Prognostic significance of histomorphologic parameters in diffuse malignant peritoneal mesothelioma. Arch Pathol Lab Med. 2006;130:1654–61.
Kerrigan SA, Turnnir RT, Clement PB, Young RH, Churg A. Diffuse malignant epithelial mesotheliomas of the peritoneum in women: a clinicopathologic study of 25 patients. Cancer. 2002;94:378–85.
Nonaka D, Kusamura S, Baratti D, Casali P, Cabras AD, Younan R, et al. Diffuse malignant mesothelioma of the peritoneum: a clinicopathological study of 35 patients treated locoregionally at a single institution. Cancer. 2005;104:2181–8.
Deraco M, Nonaka D, Baratti D, Casali P, Rosai J, Younan R, et al. Prognostic analysis of clinicopathologic factors in 49 patients with diffuse malignant peritoneal mesothelioma treated with cytoreductive surgery and intraperitoneal hyperthermic perfusion. Ann Surg Oncol. 2006;13:229–37.
Scattone A, Serio G, Marzullo A, Nazzaro P, Corsi F, Cocca MP, et al. High Wilms’ tumour gene (WT1) expression and low mitotic count are independent predictors of survival in diffuse peritoneal mesothelioma. Histopathology. 2012;60:472–81.
Ordóñez NG. Deciduoid mesothelioma: report of 21 cases with review of the literature. Mod Pathol. 2012;25:1481–95.
Liu S, Staats P, Lee M, Alexander HR, Burke AP. Diffuse mesothelioma of the peritoneum: correlation between histological and clinical parameters and survival in 73 patients. Pathology. 2014;46:604–9.
Krasinskas AM, Borczuk AC, Hartman DJ, Chabot JA, Taub RN, Mogal A, et al. Prognostic significance of morphological growth patterns and mitotic index of epithelioid malignant peritoneal mesothelioma. Histopathology. 2016;68:729–37.
Valente K, Blackham AU, Levine E, Russell G, Votanopoulos KI, Stewart JH, et al. A histomorphologic grading system that predicts overall survival in diffuse malignant peritoneal mesothelioma with epithelioid subtype. Am J Surg Pathol. 2016;40:1243–8.
Rosen LE, Karrison T, Ananthanarayanan V, Gallan AJ, Adusumilli PS, Alchami FS, et al. Nuclear grade and necrosis predict prognosis in malignant epithelioid pleural mesothelioma: a multi-institutional study. Mod Pathol. 2018;31:598–606.
Kadota K, Suzuki K, Colovos C, Sima CS, Rusch VW, Travis WD, et al. A nuclear grading system is a strong predictor of survival in epithelioid diffuse malignant pleural mesothelioma. Mod Pathol. 2012;25:260–71.
Kusamura S, Torres Mesa PA, Cabras A, Baratti D, Deraco M. The role of Ki-67 and pre-cytoreduction parameters in selecting diffuse malignant peritoneal mesothelioma (DMPM) patients for cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC). Ann Surg Oncol. 2016;23:1468–73.
Votanopoulos KI, Sugarbaker P, Deraco M, Morris D, Glehen O, Elias D, et al. Is cytoreductive surgery with hyperthermic intraperitoneal chemotherapy justified for biphasic variants of peritoneal mesothelioma? Outcomes from the peritoneal surface oncology group international registry. Ann Surg Oncol. 2018;25:667–73.
Verma V, Sleightholm RL, Rusthoven CG, Koshy M, Sher DJ, Grover S, et al. Malignant peritoneal mesothelioma: national practice patterns, outcomes, and predictors of survival. Ann Surg Oncol. 2018;25:2018–26.
Ihemelandu C, Bijelic L, Sugarbaker PH. Iterative cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for recurrent or progressive diffuse malignant peritoneal mesothelioma: clinicopathologic characteristics and survival outcome. Ann Surg Oncol. 2015;22:1680–5.
Nicholson AG, Sauter JL, Nowak AK, Kindler HL, Gill RR, Remy-Jardin M, et al. EURACAN/IASLC proposals for updating the histologic classification of pleural mesothelioma: towards a more multidisciplinary approach. J Thorac Oncol. 2020;15:29–49.
Leblay N, Lepretre F, Le Stang N, Gautier-Stein A, Villeneuve L, Isaac S, et al. BAP1 is altered by copy number loss, mutation, and/or loss of protein expression in more than 70% of malignant peritoneal mesotheliomas. J Thorac Oncol. 2017;12:724–33.
Singhi AD, Krasinskas AM, Choudry HA, Bartlett DL, Pingpank JF, Zeh HJ, et al. The prognostic significance of BAP1, NF2, and CDKN2A in malignant peritoneal mesothelioma. Mod Pathol. 2016;29:14–24.
Baumann F, Flores E, Napolitano A, Kanodia S, Taioli E, Pass H, et al. Mesothelioma patients with germline BAP1 mutations have 7-fold improved long-term survival. Carcinogenesis. 2015;36:76–81.
Shrestha R, Nabavi N, Lin YY, Mo F, Anderson S, Volik S, et al. BAP1 haploinsufficiency predicts a distinct immunogenic class of malignant peritoneal mesothelioma. Genome Med. 2019;11:8.
Deraco M, Cabras A, Baratti D, Kusamura S. Immunohistochemical evaluation of minichromosome maintenance protein 7 (MCM7), topoisomerase IIα, and Ki-67 in diffuse malignant peritoneal mesothelioma patients using tissue microarray. Ann Surg Oncol. 2015;22:4344–51.
Pillai K, Pourgholami MH, Chua TC, Morris DL. Prognostic significance of Ki67 expression in malignant peritoneal mesothelioma. Am J Clin Oncol. 2015;38:388–94.
Letica-Kriegel AS, Leinwand JC, Sonett JR, Gorenstein LA, Taub RN, Chabot JA, et al. 50 Patients with malignant mesothelioma of both the pleura and peritoneum: a single-institution experience. Ann Surg Oncol. 2020;27:205–13.
Hartman DJ, Borczuk A, Dacic S, Krasinskas A. Reproducibility for histologic parameters in peritoneal mesothelioma. Hum Pathol. 2017;67:54–9.
Klebe S, Mahar A, Henderson DW, Roggli VL. Malignant mesothelioma with heterologous elements: clinicopathological correlation of 27 cases and literature review. Mod Pathol. 2008;21:1084–94.
Hommell-Fontaine J, Isaac S, Passot G, Decullier E, Traverse-Glehen A, Cotte E, et al. Malignant peritoneal mesothelioma treated by cytoreductive surgery and hyperthermic intraperitoneal chemotherapy: is GLUT1 expression a major prognostic factor? A preliminary study. Ann Surg Oncol. 2013;20:3892–8.
Pillai K, Pourgholami MH, Chua TC, Morris DL. Ki67-BCL2 index in prognosis of malignant peritoneal mesothelioma. Am J Cancer Res. 2013;3:411–23.
Pillai K, Pourgholami MH, Chua TC, Morris DL. MUC1 has prognostic significance in malignant peritoneal mesothelioma. Int J Biol Markers. 2013;28:303–12.
Song H, Zheng GQ, Guo XZ, Liu CR, Liang YF, Yang DL. IMP3 as a prognostic biomarker in patients with malignant peritoneal mesothelioma. Hum Pathol. 2018;81:138–47.
Liang Y, Zheng G, Yin W, Song H, Li C, Tian L, et al. Significance of EGFR and PTEN expression and PLR and NLR for predicting the prognosis of epithelioid malignant peritoneal mesothelioma. Gastroenterol Res Pr. 2019;2019:7103915.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Kindler has received consulting fees from Aldeyra Therapeutics, Astellas, Boehringer-Ingelheim, Bristol-Myers Squibb, Erytech, Five Prime Therapeutics, Ipsen Pharmaceuticals, Kyowa, Paredox Therapeutics, Merck, and MedImmune. None of the other authors has relevant financial disclosures or conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Chapel, D.B., Schulte, J.J., Absenger, G. et al. Malignant peritoneal mesothelioma: prognostic significance of clinical and pathologic parameters and validation of a nuclear-grading system in a multi-institutional series of 225 cases. Mod Pathol 34, 380–395 (2021). https://doi.org/10.1038/s41379-020-00688-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-020-00688-4
This article is cited by
-
Organoids derived from patients provide a new opportunity for research and individualized treatment of malignant peritoneal mesothelioma
Molecular Cancer (2024)
-
Peritoneal Mesothelioma: Systematic Review of Hyperthermic Intraperitoneal Chemotherapy (HIPEC) Protocol Outcomes
Indian Journal of Surgical Oncology (2023)
-
Advances in the management of peritoneal malignancies
Nature Reviews Clinical Oncology (2022)
-
Evaluation of prognostic histological parameters proposed for pleural mesothelioma in diffuse malignant peritoneal mesothelioma. A short report
Diagnostic Pathology (2021)
-
Combined grade and nuclear grade are prognosis predictors of epithelioid malignant peritoneal mesothelioma: a multi-institutional retrospective study
Virchows Archiv (2021)