Abstract
In the urinary tract, there is an uncertain relationship between intestinal metaplasia (IM), primary adenocarcinoma, and urothelial carcinoma. Although IM is usually found adjacent to concurrent urothelial carcinoma or adenocarcinoma, small retrospective series have shown that most bladder biopsies with only IM do not subsequently develop cancer. However, IM with dysplasia does seem to be associated with a higher risk of concurrent malignancy or progressing to cancer. Since the molecular landscape of these lesions has remained largely unexplored, there are significant uncertainties about the oncogenic potential of IM in the bladder and urethra. This study investigated the presence of potentially oncogenic genetic variants in cases of IM with and without dysplasia. Twenty-three (23) cases of IM (3 urethra, 20 bladder) were sequenced using a solid tumor next-generation sequencing panel. Of these, five contained IM with high-grade dysplasia (including a case with paired IM-adenocarcinoma and another with paired IM-urothelial carcinoma) and 18 lacked dysplasia. Oncogenic genetic variants were found in all cases of IM with high-grade dysplasia and in five non-dysplastic IM cases, including mutations and copy number variants commonly seen in primary adenocarcinoma of the bladder and urothelial carcinoma. This study demonstrates that IM can harbor potentially oncogenic genetic variants, suggesting that it might represent a cancer precursor or a marker of increased cancer risk in a subset of cases.
Similar content being viewed by others
Introduction
Intestinal metaplasia (IM) is relatively uncommon in endoscopic bladder and urethral biopsies, and can be considered a subtype of cystitis/urethritis glandularis [1, 2]. The most common form of cystitis glandularis shows glandular spaces with an inner lining of cuboidal or columnar cells surrounded by benign urothelium [2]. The so called “intestinal type” of cystitis glandularis, which is much less frequent than the usual type, can be regarded as equivalent to IM [2]. In the esophagus and stomach, IM is considered a risk factor for intestinal-type adenocarcinoma as part of a metaplasia-dysplasia-carcinoma sequence [3,4,5]. However, the association between IM and cancer risk in the urinary tract is still unclear and somewhat debated. In the bladder, IM can be found adjacent to urothelial carcinoma, adenocarcinoma, and squamous cell carcinoma [1, 6]. Nonetheless, seemingly few patients with only IM on biopsy show progression to carcinoma [1, 7, 8]. In contrast, IM with dysplasia seems to have a higher association with concurrent or subsequent carcinoma and likely represents a stronger risk factor for progression when it is the only finding in bladder biopsies [6].
Because the molecular landscape of IM of the bladder and urethra remains largely unexplored, it is uncertain whether urinary tract IM has oncogenic potential from a genetic perspective. Therefore, the objective of this study was to investigate the presence of potentially oncogenic genetic variants in IM of the bladder and urethra.
Materials and methods
This research was performed with the approval of the Institutional Review Board of Brigham and Women’s Hospital.
Cases
A total of 23 cases from 23 different patients were included; 20 from the bladder and 3 from the urethra. The series comprised cases of IM without dysplasia (n = 18) and with dysplasia (n = 5); the latter group included dysplasia only (n = 1), dysplasia adjacent to adenocarcinoma (n = 1), dysplasia with concurrent urothelial carcinoma present in a separate sample (n = 1), and dysplasia vs superficial fragments of adenocarcinoma (no evidence of invasion, n = 2). IM with dysplasia was present in all three urethral cases.
Collection of tissue
The study workflow and a breakdown of the cases is illustrated in Fig. 1. Formalin-fixed paraffin-embedded (FFPE) tissue was collected by coring specific areas from histology tissue blocks (n = 16) or manual dissection from 5 µm tissue sections on glass slides (n = 7), depending on the abundance and distribution of the lesions of interest. In cases where IM was focal or intermingled with normal urothelium or inflammation, the areas of interest were cored to ensure adequate cellularity and to minimize contamination from other tissues/cells. When there was abundant lesional tissue present, and the different lesions of interest were clearly separated and amenable to manual dissection, FFPE tissue was scraped off glass slides. Depending on the size of the lesion, coring was performed using disposable 750 µm or 1 mm punches with plungers (Robbins Instruments, Chatham, NJ). H&E stained sections were performed before and after coring to map the areas of interest on the block and to confirm adequate sampling, respectively. Manual dissection of FFPE sections was performed using H&E slides marked by a pathologist for reference.
IM without dysplasia (n = 18), IM with dysplasia (n = 1), IM with dysplasia with concurrent adenocarcinoma or urothelial carcinoma (n = 2) and IM with dysplasia vs. adenocarcinoma in-situ (no evidence of invasion, n = 2). The two cases in the fourth column showed superficial fragments of atypical intestinal epithelium without evidence of invasion. Because both patients had a history of intestinal-type adenocarcinoma status post treatment, the distinction between IM with high-grade dysplasia and superficial fragments of adenocarcinoma or adenocarcinoma in-situ was difficult. AdenoCa adenocarcinoma, IM intestinal metaplasia, UC urothelial carcinoma.
Normal urothelium was obtained in 11 cases to compare with the corresponding (paired) IM samples. In all of these cases, both the IM and normal urothelium were cored from tissue blocks (Fig. 1). One case showed both IM with dysplasia and adenocarcinoma present on separate tissue fragments, which were manually dissected and differentially sequenced for comparison. Another case showed IM with dysplasia and concurrent high-grade urothelial carcinoma in different samples; both lesions were manually dissected and independently sequenced. For the remaining cases, only IM was collected.
Nucleic acid extraction, sequencing and informatics analysis (oncopanel)
DNA extraction and sequencing were performed as previously described by Garcia et al. and Sholl et al. [9, 10]. Briefly, cellularity was estimated on H&E-stained sections by a pathologist using a threshold of 20% for sample acceptance. DNA was extracted from FFPE scrapings and cores using standard commercial kits (Qiagen, Valencia, CA) according to the manufacturer’s recommendations. Sequencing libraries were prepared using TruSeq LT library preparation kit (Illumina, San Diego, California) with a DNA input of 200 ng (threshold of 100 ng). Sequences of interest were selected by hybridization to a set of custom-designed capture probes (Agilent SureSelect; Agilent Technologies, Santa Clara, CA). Sequencing was performed on an Illumina HiSeq 2500 System (Illumina, San Diego, CA). Deconvolution of pooled samples, read alignment, variant calling (single nucleotide variants, insertion-deletions, copy number variants (CNVs) and structural variants) and annotation was carried out using an institutional bioinformatic pipeline [9,10,11]. To remove contaminating germline variants in this tumor-only sequencing assay, variants present at a population frequency of >0.1% in the gnomAD database (Broad Institute) were filtered out. Additionally, the informatics analysis of Oncopanel includes in-house developed algorithms for detection of mismatch repair deficiency and several mutational signatures (smoking, UV, and APOBEC) [12]. All variants were reviewed and approved by a molecular genetic pathologist (LMS) and evaluated for pathogenicity.
Immunohistochemistry
Immunohistochemistry for MTAP and IDH2 R172 mutant proteins was performed using primary anti-MTAP (Cat# sc-100782, clone 42-T, Santa Cruz Biotechnology, TX) and mutation-specific anti-IDH1 R132/IDH2 R172 (Cat# MABC1103, clone R132/172, Millipore Sigma, Burlington, MA) mouse monoclonal antibodies. Paraffin‐embedded sections were incubated in hydrogen peroxide and absolute alcohol for 30 min to block endogenous peroxidase activity. Heat-induced antigen retrieval was performed in a pressure cooker with sodium citrate buffer (10 mM, pH6). After blocking of non-specific binding sites, tissue sections were incubated with anti-MTAP (dilution 1:75, overnight incubation) and anti-IDH1 R132/IDH R172 (dilution 1:350) primary antibodies. A Novolink Polymer Detection System (Leica Biosystems, Buffalo Groove, IL) was used for detection. Staining was performed in a Link48 automated platform (Agilent, Santa Clara, CA, USA).
Cohort of primary bladder adenocarcinomas for comparison
An institutional cohort of 30 primary bladder adenocarcinomas previously sequenced with Oncopanel was analyzed. These patients were part of consented institutional protocols (DFCI protocols 11-104/17-000). This cohort was evaluated as a comparator; relevant genes affected in >20% of cases were extracted, and their frequencies were plotted as presented in the results section.
Clinical and pathologic follow-up data
Electronic medical records, laboratory information systems and available scanned outside pathology reports were reviewed to obtain follow-up information.
Results
General histopathologic and clinical characteristics of the cases
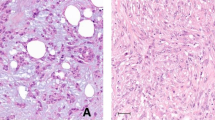
All cases of IM without dysplasia (n = 18) arose in the bladder, with the extent of IM ranging from focal (up to three discrete foci and <50% of the tissue) to diffuse (>3 discrete foci or >50% of the tissue) (Fig. 2a). Most cases demonstrated tall columnar epithelium with interspersed goblet cells, but a subset showed predominantly columnar mucinous cells. Nuclei were elongated, containing delicately dispersed chromatin and variably sized basophilic nucleoli. A mixed inflammatory infiltrate including plasma cells, lymphocytes, eosinophils, and neutrophils was almost invariably present. Mitoses and morphologic features suggestive of malignancy (e.g., enlarged hyperchromatic nuclei or atypical mitotic figures) were uniformly absent in IM without dysplasia. A single focus of IM with scattered Paneth cells was seen in only one sample. One case had a somewhat polypoid appearance on cystoscopy and was diagnosed as polypoid cystitis glandularis with IM.
a Prototypical case of bladder IM without dysplasia showing abundant goblet cells adjacent to normal urothelium. b IM with dysplasia below the urothelial surface. Unlike non-dysplastic IM, these cases show marked mucin depletion, nuclear enlargement and hyperchromasia. c IM with dysplasia in urethra of a patient with a history of primary urethral adenocarcinoma. Foci of non-dysplastic IM were also present adjacent to the dysplastic foci (inset). d Urethral lesion showing highly atypical intestinal epithelium without evidence of invasion. However, this patient also had a history of a primary adenocarcinoma of the bladder, suggesting that the lesion might represent superficial fragments of adenocarcinoma. Paired IM with dysplasia (e) and primary adenocarcinoma of the urethra (f) were present in separate tissue fragments in the biopsy of case 20.
Dysplastic IM (n = 5) was found in the bladder (n = 2) and urethra (n = 3), and showed mucin depletion, pseudostratification, nuclear enlargement and hyperchromasia (Fig. 2b–f). Prominent basophilic nucleoli and numerous mitotic figures were readily identified. A single gland with focal architectural complexity somewhat suspicious for, but not diagnostic of adenocarcinoma was present in one case. This sample was considered dysplastic IM for the purposes of the study. One case of dysplastic IM (case 20) contained IM with high-grade dysplasia and invasive adenocarcinoma present in separate tissue fragments, which were differentially dissected and sequenced for comparison (Fig. 2e, f). Another case (case 21) also showed concurrent high-grade papillary urothelial carcinoma in separate biopsies, which was sequenced in parallel for comparison. Two additional cases, one in the bladder and one in the urethra, showed superficial fragments of atypical intestinal epithelium, without clear evidence of invasion. Both patients had a history of intestinal-type adenocarcinoma status post treatment, making the distinction between IM with high-grade dysplasia and superficial fragments of adenocarcinoma or adenocarcinoma in-situ very difficult.
Next-generation sequencing (NGS) results
A total of 36 samples from 23 individual patients were sequenced. The breakdown of the cases and samples is as follows: 11 patients with paired non-dysplastic IM-normal urothelium (22 samples), 10 patients with only IM (7 non-dysplastic and 3 dysplastic, 10 samples), 1 case with paired dysplastic IM-adenocarcinoma (2 samples) and 1 case with paired dysplastic IM-high-grade urothelial carcinoma (2 samples). Potentially oncogenic genetic variants were detected in a subset of 10/23 IM cases (43%), comprising 5 cases of non-dysplastic IM and all 5 cases of IM with dysplasia (including the cases with paired adenocarcinoma and high-grade urothelial carcinoma) (Fig. 3). All 23 cases were mismatch-repair proficient. Overall, the mutational burden and number of CNVs was higher in IM with dysplasia and adenocarcinoma than in IM without dysplasia and normal urothelium (Table 1 and Fig. 3). No oncogenic genetic variants were seen in normal urothelium. Of note, our assay only considers variants present at allele frequencies higher than 3% to reduce the risk of false positives, which might increase the rate of false negatives for real low-level variants corresponding to small clones within the histologically normal urothelium. A summary of the specific single nucleotide variants (SNVs) and indels present in each case is presented in Table 2.
IM without dysplasia
Of the 18 cases of IM without dysplasia, 5 showed potentially oncogenic somatic variants (Fig. 3, cases 1–5). Of note, there were no significant morphologic differences between non-dysplastic IM cases with and without potentially oncogenic variants. Two of the five cases (cases 1 and 2) had paired morphologically normal urothelium for comparison, whereas cases 3, 4, and 5 did not. IM from cases 1 and 2 showed Lysine Methyltransferase 2D (KMT2D) and Stromal Antigen 2 (STAG2) mutations, respectively. These variants were not seen in the paired histologically normal urothelium. Case 3 had multiple KMT2D mutations, suggesting biallelic loss of the gene. Additionally, this case harbored an Adenomatous Polyposis Coli (APC) p.I1307K variant that was most likely germline (VAF ~50%). Germline APC p.I1307K is a known genetic risk factor for development of colorectal adenocarcinoma in Ashkenazi Jewish populations [13]. This patient had a remote history of low-grade papillary urothelial carcinoma (pTa) status-post treatment, but there was no morphologic evidence of residual urothelial carcinoma in the current specimen and IM was collected by coring, minimizing the chance of contamination. Case 4 had a well-characterized hotspot Isocitrate Dehydrogenase 2 (IDH2) variant. Mutation-specific antibodies for IDH1 R132X/IDH2 R172X variants demonstrated expression of mutant IDH2 protein in IM, consistent with the NGS findings (Fig. 4a, b). Expression of the mutant IDH2 protein was not seen in adjacent stromal or inflammatory cells. In case 5, there was a deep (double copy) 9p21.3 deletion encompassing Cyclin-Dependent Kinase Inhibitor 2A (CDKN2A), Cyclin-Dependent Kinase Inhibitor 2B (CDKN2B) and Methylthioadenosine Phosphorylase (MTAP), in addition to chromosomal-level gains of chromosome 20 and a Tumor Protein P53 Binding Protein 1 (TP53BP1) mutation. Immunohistochemistry showed loss of MTAP protein expression in IM, which contrasted with the positivity seen in adjacent stromal and inflammatory cells (Fig. 4c, d). Interestingly, per clinical notes, this patient had a history of Peutz–Jeghers syndrome, consistent with the double copy loss of Serine/Threonine Kinase 11 (STK11) exon 3 detected by NGS (Fig. 5).
a In case 4, IM showed a predominance of mucinous cells and absence of architectural and/or cytologic atypia. b IDH1 R132X/IDH2 R172X mutation-specific immunohistochemistry demonstrates cytoplasmic expression of mutant IDH2 protein in the cytoplasm of IM cells, consistent with the IDH2 R172S mutation identified by NGS (Oncopanel). c Lesion from the posterior bladder wall of case 5 showing non-dysplastic IM. d MTAP expression is lost in the intestinal-type epithelium but retained in the stromal and inflammatory cells. e The copy number plot corresponding to chromosome 9 shows deep (double copy) loss of a region within 9p21.3 encompassing the sequences of CDKN2A, CDKN2B and MTAP. Copy number changes are presented as log2 ratios.
Dysplastic IM
Case 19 harbored a well-known hotspot Human Homologue of Harvey Rat Sarcoma Viral Oncogene (HRAS) mutation. No additional genetic variants were identified.
Paired dysplastic IM-adenocarcinoma and dysplastic IM-papillary urothelial carcinoma
The one case (Fig. 3, case 20) with paired dysplastic IM-adenocarcinoma showed multiple somatic variants and numerous CNVs in both samples, including chromosomal-level loss of chromosomes 4 and 17, chromosomal-level gain of chromosome 20 and multiple arm-level and regional events (Fig. 3). Of note, both the IM and adenocarcinoma showed biallelic loss of Tumor Protein P53 (TP53), whereas Structural Maintenance Of Chromosomes 3 (SMC3) and Protein Phosphatase 2 Scaffold Subunit Alpha (PPP2R1A) mutations were exclusive to the dysplastic IM and adenocarcinoma, respectively. The IM also showed amplification of a region of chromosome 12 encompassing Human Homologue of Mouse Double Minute 2 (MDM2).
Case 21 was more complex in that it harbored multiple somatic SNVs, including both cancer-relevant mutations (see Table 2) and numerous variants of uncertain significance. Case 20 showed an APOBEC mutational signature, which is associated with upregulation of APOBEC enzymes and might predict somewhat favorable clinical outcomes in urothelial carcinoma [14, 15]. Regional amplifications of 6p and 12q were also identified, the latter involving the MDM2 locus. Paired urothelial carcinoma also showed an APOBEC signature and a very similar mutational profile, with identical disease-relevant mutations and a few different variants of uncertain significance (not shown), as well as a slightly higher mutational burden. Akin to dysplastic IM, the CNV profile of the urothelial carcinoma also showed 6p and 12q amplifications, with additional gains of 10q and 16q.
Dysplastic IM versus adenocarcinoma
The two cases (Fig. 3, cases 22 and 23) with a differential diagnosis of IM with dysplasia vs. adenocarcinoma showed multiple somatic genetic variants. Case 1 demonstrated biallelic loss of APC with multiple concurrent cancer-relevant mutations (Fig. 3 and Table 1). Chromosomal-level gains of chromosomes 6, 12, and 20, arm-level gain of 13q and 19q13.11 amplification (locus encompassing CCAAT Enhancer Binding Protein Alpha, CEBPA) were also present. Case 2 had Ataxia Telangiectasia Mutated (ATM) and BRCA1 Interacting Protein C-Terminal Helicase 1 (BRIP1) variants, and multiple CNVs including a focal 3q amplification (Fig. 3).
Frequency of genetic variants in a cohort of primary bladder adenocarcinomas
In general, the genes with the highest frequency of variants were TP53, AT-Rich Interaction Domain 1A (ARID1A), KMT2D, Lysine Demethylase 6A (KDM6A) and Fibroblast Growth Factor Receptor 3 (FGFR3). All these genes showed variants in 20% or more of the cases (Fig. 6).
Clinical follow-up
Demographic and relevant clinical follow-up data for the cases with positive genetic findings are summarized in Table 3.
Discussion
In the stomach and esophagus, it has been shown that IM may harbor oncogenic genetic variants that make it prone to malignant transformation as further genetic changes accumulate in susceptible IM subclones [16, 17]. Conversely, in the urinary tract, the relationship between IM and cancer is unclear and somewhat debated. Although IM can recur locally, most series have shown that only a small number of patients develop adenocarcinoma during follow-up [6, 7]. However, IM with and without dysplasia is often found in association with both gland-forming and non-gland-forming malignancies of the urinary tract [1, 6]. In fact, one of the largest available series of cystitis glandularis, which includes 19 cases of IM, shows that this lesion is more commonly associated with concurrent urothelial carcinoma than with primary adenocarcinoma of the bladder [1]. However, because of the retrospective design and relatively small size of most studies, the true significance of urinary tract IM as a cancer risk factor is not well-established.
Given the difficulties inherent to collecting data prospectively and gathering a large number of cases of a relatively rare entity, alternative strategies are required to explore the oncogenic potential of IM and the relationship between IM and urinary tract malignancies. A reasonable approach is to perform comparative immunophenotypic and molecular studies at the tissue level. Immunohistochemistry has shown that, unlike usual cystitis cystica/glandularis and normal urothelium, IM expresses keratin 20 and CDX2, and loses expression of keratin 7 [18]. However, very little is known about the molecular characteristics of IM of the urinary tract. Prior studies of single cases have shown evidence of loss of heterozygosity of the D2S123 microsatellite sequence, as well as Telomerase Reverse Transcriptase (TERT) promoter and F-Box And WD Repeat Domain Containing 7 (FBXW7) mutations [19, 20]. Additionally, loss of heterozygosity of TP53 can be seen in dysplastic glandular foci within IM [19]. IM of the bladder has also been associated with telomere shortening and chromosomal gains [21]. More recently, Amin et al. performed mutation analysis on a limited number of colon cancer-related genes to compare IM of the bladder, tubular adenomas, and papillary urothelial carcinomas [22]. Their study found APC and Neuroblastoma RAS Viral (V-Ras) Oncogene Homolog (NRAS) mutations in 2 of 9 IM cases.
In the present study, 2 of 23 patients had a suspected or known germline event (~10%) which is roughly in keeping with the rates of significant germline events detected by routine profiling in cancer cohorts [23]. Interestingly, case 3 (from a patient who had no history of colon carcinoma) demonstrated a likely germline APC p.I1307K variant, which constitutes a well-recognized genetic risk factor for colorectal cancer [13]. This raises the possibility that APC p.I1307K might also have an association with glandular lesions of the bladder, although this is speculative. The second patient (case 5) had a history of Peutz-Jeghers Syndrome, which is consistent with the identification of biallelic deletion of exon 3 of STK11. Deletion of exon 3 of STK11 has been previously reported in patients with Peutz-Jeghers and had been identified in a germline sample of case 5 according to clinical notes [24, 25].
In the present study, 5/18 cases (28%) with non-dysplastic IM harbored potentially oncogenic somatic genetic variants in the metaplastic epithelium (Fig. 3). Of these five cases, only one had a remote history of low-grade papillary urothelial carcinoma (pTa). Some of the variants identified in IM without dysplasia, such as KMT2D (cases 1 and 3), STAG2 (case 2) and RNA Binding Motif Protein 10 (RBM10, case 4) mutations, have been described both in non-nvasive and invasive urothelial carcinoma [26, 27].
Cases 4 and 5 show additional interesting results and merit individual discussion. Case 4 harbored an activating hotspot IDH2 p.R172S mutation confirmed by mutation-specific immunohistochemistry (Fig. 5). This particular variant, IDH2 p.R172S, has been described as a driver event in primary bladder adenocarcinoma [28]. Case 5 is the only non-dysplastic IM case with CNVs, which included biallelic loss of tumor suppressors CDKN2A (p16) and CDKN2B. In urothelial carcinoma, CDKN2A (p16) inactivation/deletion characterizes a specific subset of tumors and is mutually exclusive with loss of Retinoblastoma-Associated Protein (RB1) [26]. Homozygous deletion of CDKN2A was also observed in a small number of cases (2/30) in our series of primary bladder adenocarcinomas. The MTAP gene, which encodes an enzyme that plays a major role in the salvage of methionine and adenine and is therefore considered a ubiquitously expressed housekeeping gene, is located in close proximity to CDKN2A. Consequently, these genes are usually co-deleted and loss of MTAP expression by immunohistochemistry is therefore a a useful surrogate marker of homozygous CDKN2A/P16 loss in multiple lesions, including non-dysplastic IM [29]. Homozygous deletion of this chromosomal region (9p21.3) in case 5 was confirmed by MTAP immunohistochemistry (Fig. 4).
The data presented herein shows that IM with high-grade dysplasia always harbored at least one, but usually multiple, genetic variants (Fig. 3), including several mutations that have been described in primary adenocarcinomas of the bladder [20, 28]. These included, but were not restricted to, APC (case 22), Phosphatidylinositol-4,5-Bisphosphate 3-Kinase Catalytic Subunit Alpha (PIK3CA, case 22), FBXW7 (cases 21 and 22) and Kirsten Rat Sarcoma Viral Oncogene Homolog (KRAS, case 22) mutations. Interestingly, some cases of IM with dysplasia showed variants that are also commonly seen in urothelial carcinoma of the bladder, such as ARID1A (case 21), HRAS (case 19) and Lysine Demethylase 5A (KDM5A, case 21) mutations [26]. Moreover, IM of case 21 showed an APOBEC mutational signature, which can be seen in multiple tumors including urothelial carcinoma [14, 15], and the mutational and CNV profile of this lesion was markedly similar to that seen in separate foci of concurrent urothelial carcinoma. In case 20, paired dysplastic IM-primary bladder adenocarcinoma samples showed very similar mutational profiles with biallelic inactivation of TP53. Despite the absence of overtly invasive tumor in cases 22 and 23, both patients had a history of adenocarcinoma. Therefore, it is possible that the lesion represented in the samples was recurrent adenocarcinoma without evidence of invasion. Four of 5 (80%) IMs with dysplasia harbored multiple CNVs, which were particularly complex in the case with paired dysplastic IM-adenocarcinoma. TERT promoter mutations were not detected in any case.
This study has limitations that need to be discussed. First, there was no normal urothelium for comparison in a subset of samples, which is an almost unavoidable problem in studies of archival FFPE tissue. Therefore, the interpretation of variants as germline and/or somatic in cases without paired normal tissue is somewhat speculative. However, the variant allele frequency/fraction (VAF) is a particularly valuable metric that can be used to interpret variants as somatic or potentially germline [30]. In this study, the VAF of the APC p.I1307K variant was supportive of a germline origin, in keeping with previously published data [13]. The other potentially germline variant detected in this series (homozygous deletion of STK11) had been previously identified as the cause of Peutz-Jeghers syndrome in a germline sample of case 5 according to available clinical notes. All the other variants identified in the study showed sequencing metrics consistent with a somatic origin. Moreover, mutation-specific IDH1 and MTAP immunohistochemistry demonstrated that IDH1 p.R172S mutation and MTAP loss were only present in the lesional tissue (IM) of cases 4 and 5, respectively. Despite the lack of paired normal tissue in a subset of cases, this is the first molecular study of urinary tract IM to include non-lesional tissue control for a significant proportion of the samples (11/23 cases). Also, paired dysplastic IM-adenocarcinoma and dysplastic IM-high-grade urothelial carcinoma were analyzed in parallel in two cases. Another potential weakness of our approach is the use of coring and manual dissection instead of laser microdissection. However, multiple measures were taken to avoid contamination and ensure correct sampling, as described above. Finally, our cases have limited clinical follow-up data.
Despite the aforementioned limitations, this series presents the largest and most comprehensive molecular characterization of IM with and without dysplasia to date. Given the short follow-up of most cases, the absence of progression to malignancy in patients with non-dysplastic IM harboring potentially oncogenic mutations should be interpreted cautiously; especially considering that the interval between diagnosis of IM and development of high-grade dysplasia or adenocarcinoma in other organs is 5–10 years, but not uncommonly much longer [31, 32]. In this regard, data from studies of upper gastrointestinal lesions show that while IM significantly increases the risk of adenocarcinoma, only a small fraction of cases eventually develop an overt malignancy [33]. Unlike upper gastrointestinal tract IM, whose prevalence is known thanks to endoscopic screening programs [33] of high-risk populations, the true incidence of urinary tract IM is unknown. This series demonstrated potentially oncogenic genetic variants in 5/18 (28%) cases of non-dysplastic IM, suggesting that biologic progression to dyplasia and carcinoma is theoretically possible in a subset of cases.
Of note, highly recurrent genetic variants were not identified. This suggests that, if genitourinary IM is indeed a precursor, it might progress via diverse oncogenic pathways and give rise to different types of cancer. This contrasts with the somewhat linear molecular evolution of esophageal IM, where progression to dysplasia and adenocarcinoma consistently correlates with sequential biallelic loss of CDKN2A and TP53 [16]. Similarly, urothelial carcinoma in situ, a known precursor of muscle-invasive bladder cancer, usually shows consistent genetic alterations of TERT, TP53, and CDKN2A [34, 35].
The results presented herein show that IM with high-grade dysplasia invariably harbors oncogenic genetic variants associated with both urothelial carcinoma and primary adenocarcinoma of the bladder. Therefore, the presence of IM with dysplasia in the absence of concurrent cancer in bladder and urethral biopsies likely warrants close follow-up. Unfortunately, there were no significant morphologic differences between the subsets of non-dysplastic IM cases with and without potentially oncogenic genetic variants. Two of the non-dysplastic IM cases (cases 4 and 5) with oncogenic genetic variants showed florid IM, but so did multiple cases without molecular findings. Identification of biallelic CDKN2A loss in case 5 suggests that the presence of IM – even without dysplasia – might warrant clinical follow-up in the context of Peutz-Jeghers syndrome. Interestingly, some of the variants detected in IM have been also identified in urothelial carcinoma, suggesting that IM might have a relationship to urothelial cancer. In this regard, it is uncertain if IM that harbors genetic variants frequently seen in urothelial carcinoma is a direct cancer precursor or part of a field change. Further studies are required to answer these questions.
References
Smith AK, Hansel DE, Jones JS. Role of cystitis cystica et glandularis and intestinal metaplasia in development of bladder carcinoma. Urology. 2008;71:915–8.
Young RH. Tumor-like lesions of the urinary bladder. Mod Pathol. 2009;22:S37–52.
Haggitt RC, Tryzelaar J, Ellis FH, Colcher H. Adenocarcinoma complicating columnar epithelium-lined (Barrett’s) esophagus. Am J Clin Pathol. 1978;70:1–5.
DeMeester SR, DeMeester TR. Columnar mucosa and intestinal metaplasia of the esophagus: fifty years of controversy. Ann Surg. 2000;231:303–21.
Correa P. Human gastric carcinogenesis: a multistep and multifactorial process-First American Cancer Society Award Lecture on Cancer Epidemiology and Prevention. Cancer Res. 1992;52:6735–40.
Gordetsky J, Epstein JI. Intestinal metaplasia of the bladder with dysplasia: a risk factor for carcinoma? Histopathology. 2015;67:325–30.
Xin Z, Zhao C, Huang T, Zhang Z, Chu C, Lu C, et al. Intestinal metaplasia of the bladder in 89 patients: a study with emphasis on long-term outcome. BMC Urol. 2016;16:24.
Corica FA, Husmann DA, Churchill BM, Young RH, Pacelli A, Lopez-Beltran A, et al. Intestinal metaplasia is not a strong risk factor for bladder cancer: study of 53 cases with long-term follow-up. Urology. 1997;50:427–31.
Garcia EP, Minkovsky A, Jia Y, Ducar MD, Shivdasani P, Gong X, et al. Validation of OncoPanel: a targeted next-generation sequencing assay for the detection of somatic variants in cancer. Arch Pathol Lab Med. 2017;141:751–8.
Sholl LM, Do K, Shivdasani P, Cerami E, Dubuc AM, Kuo FC, et al. Institutional implementation of clinical tumor profiling on an unselected cancer population. JCI Insight. 2016;1:e87062.
Abo RP, Ducar M, Garcia EP, Thorner AR, Rojas-Rudilla V, Lin L, et al. BreaKmer: detection of structural variation in targeted massively parallel sequencing data using kmers. Nucleic Acids Res. 2015;43:e19.
Papke DJ, Nowak JA, Yurgelun MB, Frieden A, Srivastava A, Lindeman NI, et al. Validation of a targeted next-generation sequencing approach to detect mismatch repair deficiency in colorectal adenocarcinoma. Mod Pathol. 2018;31:1882–90.
Boursi B, Sella T, Liberman E, Shapira S, David M, Kazanov D, et al. The APC p.I1307K polymorphism is a significant risk factor for CRC in average risk Ashkenazi Jews. Eur J Cancer. 2013;49:3680–5.
Glaser AP, Fantini D, Wang Y, Yu Y, Rimar KJ, Podojil JR, et al. APOBEC-mediated mutagenesis in urothelial carcinoma is associated with improved survival, mutations in DNA damage response genes, and immune response. Oncotarget. 2018;9:4537–48.
Jaguva Vasudevan AA, Kreimer U, Schulz WA, Krikoni A, Schumann GG, Häussinger D, et al. APOBEC3B activity is prevalent in urothelial carcinoma cells and only slightly affected by LINE-1 expression. Front Microbiol. 2018;9:2088.
Grady WM, Yu M. Molecular evolution of metaplasia to adenocarcinoma in the esophagus. Dig Dis Sci. 2018;63:2059–69.
Huang KK, Ramnarayanan K, Zhu F, Srivastava S, Xu C, Keng Tan AL, et al. Genomic and epigenomic profiling of high-risk intestinal metaplasia reveals molecular determinants of progression to gastric cancer. Cancer Cell. 2018;33:137–.e5.
Sung M-T, Lopez-Beltran A, Eble JN, MacLennan GT, Tan PH, Montironi R, et al. Divergent pathway of intestinal metaplasia and cystitis glandularis of the urinary bladder. Mod Pathol. 2006;19:1395–401.
Srivastava S, Yan B, Chin SY, Muliana T, Salto-Tellez M, Teh M. Nuclear p53 expression is associated with allelic imbalance (TP53) in glandular dysplasia and typical cystitis glandularis: a LCM-based molecular analysis. Clin Genitourin Cancer. 2012;10:57–59.
Maurer A, Ortiz-Bruechle N, Guricova K, Rose M, Morsch R, Garczyk S, et al. Comparative genomic profiling of glandular bladder tumours. Virchows Arch. 2020. https://doi.org/10.1007/s00428-020-02787-8.
Morton MJ, Zhang S, Lopez-Beltran A, MacLennan GT, Eble JN, Montironi R, et al. Telomere shortening and chromosomal abnormalities in intestinal metaplasia of the urinary bladder. Clin Cancer Res. 2007;13:6232–6.
Amin A, Murati-Amador B, Lombardo KA, Jackson CL, Grada Z, Palsgrove DN, et al. Analysis of intestinal metaplasia without dysplasia in the urinary bladder reveal only rare mutations associated with colorectal adenocarcinoma. Appl Immunohistochem Mol Morphol. 2019. https://doi.org/10.1097/PAI.0000000000000812.
Mandelker D, Zhang L, Kemel Y, Stadler ZK, Joseph V, Zehir A, et al. Mutation detection in patients with advanced cancer by universal sequencing of cancer-related genes in tumor and normal DNA vs guideline-based germline testing. JAMA. 2017;318:825–35.
Askree SH, Chin ELH, Bean LH, Coffee B, Tanner A, Hegde M. Detection limit of intragenic deletions with targeted array comparative genomic hybridization. BMC Genet. 2013;14:116.
Aretz S, Stienen D, Uhlhaas S, Loff S, Back W, Pagenstecher C, et al. High proportion of large genomic STK11 deletions in Peutz-Jeghers syndrome. Hum Mutat. 2005;26:513–9.
Weinstein JN, Akbani R, Broom BM, Wang W, Verhaak RGW, McConkey D, et al. Comprehensive molecular characterization of urothelial bladder carcinoma. Nature. 2014;507:315–22.
Hurst CD, Alder O, Platt FM, Droop A, Stead LF, Burns JE, et al. Genomic subtypes of non-invasive bladder cancer with distinct metabolic profile and female gender bias in KDM6A mutation frequency. Cancer Cell. 2017;32:701–15.e7.
Roy S, Pradhan D, Ernst WL, Mercurio S, Najjar Y, Parikh R, et al. Next-generation sequencing-based molecular characterization of primary urinary bladder adenocarcinoma. Mod Pathol. 2017;30:1133–43.
Powell EL, Leoni LM, Canto MI, Forastiere AA, Iocobuzio-Donahue CA, Wang JS, et al. Concordant loss of MTAP and p16/CDKN2A expression in gastroesophageal carcinogenesis: evidence of homozygous deletion in esophageal noninvasive precursor lesions and therapeutic implications. Am J Surg Pathol. 2005;29:1497–504.
Li MM, Datto M, Duncavage EJ, Kulkarni S, Lindeman NI, Roy S, et al. Standards and guidelines for the interpretation and reporting of sequence variants in cancer: a joint consensus recommendation of the Association for Molecular Pathology, American Society of Clinical Oncology, and College of American Pathologists. J Mol Diagn. 2017;19:4–23.
den Hoed CM, van Blankenstein M, Dees J, et al. The minimal incubation period from the onset of Barrett’s oesophagus to symptomatic adenocarcinoma. Br J Cancer. 2011;105:200–5.
Reddy KM, Chang JI, Shi JM, Kuipers EJ. Risk of gastric cancer among patients with intestinal metaplasia of the stomach in a US integrated health care system. Clin Gastroenterol Hepatol. 2016;14:1420–5.
You WC, Li JY, Blot WJ, Chang YS, Jin ML, Gail MH, et al. Evolution of precancerous lesions in a rural Chinese population at high risk of gastric cancer. Int J Cancer. 1999;83:615–9.
Garczyk S, Ortiz-Brüchle N, Schneider U, Lurje I, Guricova K, Gaisa NT, et al. Next-generation sequencing reveals potential predictive biomarkers and targets of therapy for urothelial carcinoma in situ of the urinary bladder. Am J Pathol. 2020;190:323–32.
Hartmann A, Schlake G, Zaak D, Hungerhuber E, Hofstetter A, Hofstaedter F, et al. Occurrence of chromosome 9 and p53 alterations in multifocal dysplasia and carcinoma in situ of human urinary bladder. Cancer Res. 2002;62:809–18.
Funding
This study was supported by intradepartmental research funds (BWH).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Acosta, A.M., Sholl, L.M., Fanelli, G.N. et al. Intestinal metaplasia of the urinary tract harbors potentially oncogenic genetic variants. Mod Pathol 34, 457–468 (2021). https://doi.org/10.1038/s41379-020-00655-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-020-00655-z
This article is cited by
-
Seltenere Tumoren und Tumortypen des ableitenden Harnsystems in der 5. Aufl. der WHO-Klassifikation 2022
Die Pathologie (2024)
-
Telomerase reverse transcriptase (TERT) promoter mutations in primary adenocarcinoma of bladder and urothelial carcinoma with glandular differentiation: pathogenesis and diagnostic implications
Modern Pathology (2021)