Abstract
Objective
Describe care surrounding the end of life (EOL) in the neonatal intensive care unit (NICU).
Study design
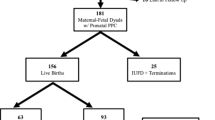
Retrospective chart review of 208 infants who died in a level IV referral-only NICU over 5 years.
Results
A goals of care (GOC) conversation was documented before the day of death for 63% of infants. 73% died following withdrawal of life-sustaining treatment (WD); 13% died in a code. The median age at death was 17.5 days. 72% were held by a parent at EOL. 94% of families desired formal memory-making. We identified associations with mode of death and parental holding at death, including: WD was associated with palliative care consultation, early GOC conversations, and increased unit-specific length of stay. Holding was associated with chaplain visits, memory-making, and increased home-to-hospital distance.
Conclusion
We present a detailed description of EOL care in an outborn NICU, including novel data on parental holding and memory-making.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Datasets generated during the current study are available upon reasonable request.
References
Ely DM, Driscoll AK. Infant Mortality in the United States, 2019:Data From the Period Linked Birth/Infant Death File. Natl Vital Stat Rep. 2021;70:1–18.
Chow S, Chow R, Popovic M, Lam M, Popovic M, Merrick J, et al. A Selected Review of the Mortality Rates of Neonatal Intensive Care Units. Front Public Health. 2015;3:225.
Matoba N, Kwon S, Collins JW, Davis MM. Risk factors for death during newborn and post-newborn hospitalizations among preterm infants. J Perinatol. 2022;42:1288–93.
Juul SE, Wood TR, Comstock BA, Perez K, Gogcu S, Puia-Dumitrescu M, et al. Deaths in a Modern Cohort of Extremely Preterm Infants From the Preterm Erythropoietin Neuroprotection Trial. JAMA Netw Open. 2022;5:e2146404.
Duff RS, Campbell AG. Moral and ethical dilemmas in the special-care nursery. N Engl J Med. 1973;289:890–4.
Weiner J, Sharma J, Lantos J, Kilbride H. How infants die in the neonatal intensive care unit: trends from 1999 through 2008. Arch Pediatr Adolesc Med. 2011;165:630–4.
Fry JT, Matoba N, Datta A, DiGeronimo R, Coghill CH, Natarajan G, et al. Center, Gestational Age, and Race Impact End-of-Life Care Practices at Regional Neonatal Intensive Care Units. J Pediatr. 2020;217:86–91.e1.
Michel MC, Colaizy TT, Klein JM, Segar JL, Bell EF. Causes and circumstances of death in a neonatal unit over 20 years. Pediatr Res. 2018;83:829–33.
Lin M, Deming R, Wolfe J, Cummings C. Infant mode of death in the neonatal intensive care unit: A systematic scoping review. J Perinatol. 2022;42:551–68.
Guttmann KF, Puoplo N, Richter F, Weintraub AS. Trends in length of stay for Neonatal Intensive Care Unit patients who die before hospital discharge. Am J Perinatol. 2021 https://doi.org/10.1055/a-1712-5313.
Kenner C, Press J, Ryan D. Recommendations for palliative and bereavement care in the NICU: a family-centered integrative approach. J Perinatol. 2015;35:S19–23.
Brooten D, Youngblut JM, Caicedo C, Del Moral T, Cantwell GP, Totapally B. Parents’ Acute Illnesses, Hospitalizations, and Medication Changes During the Difficult First Year After Infant or Child NICU/PICU Death. Am J Hosp Palliat Care. 2018;35:75–82.
Snaman J, Morris SE, Rosenberg AR, Holder R, Baker J, Wolfe J. Reconsidering early parental grief following the death of a child from cancer: a new framework for future research and bereavement support. Support Care Cancer. 2020;28:4131–9.
Hendrickson KC. Morbidity, mortality, and parental grief: a review of the literature on the relationship between the death of a child and the subsequent health of parents. Palliat Support Care. 2009;7:109–19.
Youngblut JM, Brooten D, Cantwell GP, del Moral T, Totapally B. Parent health and functioning 13 months after infant or child NICU/PICU death. Pediatrics. 2013;132:e1295–301.
Currie ER, Christian BJ, Hinds PS, Perna SJ, Robinson C, Day S, et al. Life after loss: Parent bereavement and coping experiences after infant death in the neonatal intensive care unit. Death Stud. 2019;43:333–42.
Tan JS, Docherty SL, Barfield R, Brandon DH. Addressing parental bereavement support needs at the end of life for infants with complex chronic conditions. J Palliat Med. 2012;15:579–84.
Lin M, Williams D, Vitcov G, Sayeed S, DeCourcey DD, Wolfe J, et al. Advance Care Planning and Parent-Reported End-of-Life Outcomes in the Neonatal Intensive Care Unit. Am J Perinatol. 2023 https://doi.org/10.1055/s-0043-1768488.
Samalik JM, Goldberg CS, Modi ZJ, Fredericks EM, Gadepalli SK, Eder SJ, et al. Discrepancies in Race and Ethnicity in the Electronic Health Record Compared to Self-report. J Racial Ethn Health Disparities. 2023;10:2670–5.
Weikel BW, Klawetter S, Bourque SL, Hannan KE, Roybal K, Soondarotok M, et al. Defining an Infant’s Race and Ethnicity: A Systematic Review. Pediatrics. 2023;151:e2022058756.
Wang YX, Minguez-Alarcon L, Gaskins AJ, Wang L, Ding M, Missmer SA, et al. Pregnancy loss and risk of cardiovascular disease: the Nurses’ Health Study II. Eur Heart J. 2022;43:190–9.
Delabaere A, Huchon C, Deffieux X, Beucher G, Gallot V, Nedellec S, et al. [Epidemiology of loss pregnancy]. J Gynecol Obstet Biol Reprod. 2014;43:764–75.
Cohain JS, Buxbaum RE, Mankuta D. Spontaneous first trimester miscarriage rates per woman among parous women with 1 or more pregnancies of 24 weeks or more. BMC Pregnancy Childbirth. 2017;17:437.
Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int J Epidemiol. 2014;43:476–93.
Hellmann J, Knighton R, Lee SK, Shah PS, Canadian Neonatal Network End of Life Study G. Neonatal deaths: prospective exploration of the causes and process of end-of-life decisions. Arch Dis Child Fetal Neonatal Ed. 2016;101:F102–7.
Lam V, Kain N, Joynt C, van Manen MA. A descriptive report of end-of-life care practices occurring in two neonatal intensive care units. Palliat Med. 2016;30:971–8.
Koper JF, Bos AF, Janvier A, Verhagen AA. Dutch neonatologists have adopted a more interventionist approach to neonatal care. Acta Paediatr. 2015;104:888–93.
Patel RM, Kandefer S, Walsh MC, Bell EF, Carlo WA, Laptook AR, et al. Causes and timing of death in extremely premature infants from 2000 through 2011. N Engl J Med. 2015;372:331–40.
Simpson CD, Ye XY, Hellmann J, Tomlinson C. Trends in cause-specific mortality at a Canadian outborn NICU. Pediatrics. 2010;126:e1538–44.
Roy R, Aladangady N, Costeloe K, Larcher V. Decision making and modes of death in a tertiary neonatal unit. Arch Dis Child Fetal Neonatal Ed. 2004;89:F527–30.
Younge N, Smith PB, Goldberg RN, Brandon DH, Simmons C, Cotten CM, et al. Impact of a palliative care program on end-of-life care in a neonatal intensive care unit. J Perinatol. 2015;35:218–22.
Barton L, Hodgman JE. The contribution of withholding or withdrawing care to newborn mortality. Pediatrics. 2005;116:1487–91.
Cortezzo DE, Sanders MR, Brownell EA, Moss K. End-of-life care in the neonatal intensive care unit: experiences of staff and parents. Am J Perinatol. 2015;32:713–24.
Clark OE, Fortney CA, Dunnells ZDO, Gerhardt CA, Baughcum AE. Parent Perceptions of Infant Symptoms and Suffering and Associations With Distress Among Bereaved Parents in the NICU. J Pain Symptom Manag. 2021;62:e20–e7.
Berger TM, Hofer A. Causes and circumstances of neonatal deaths in 108 consecutive cases over a 10-year period at the Children’s Hospital of Lucerne, Switzerland. Neonatology. 2009;95:157–63.
Hagen CM, Hansen TW. Deaths in a neonatal intensive care unit: a 10-year perspective. Pediatr Crit Care Med. 2004;5:463–8.
Arlettaz R, Mieth D, Bucher HU, Duc G, Fauchere JC. End-of-life decisions in delivery room and neonatal intensive care unit. Acta Paediatr. 2005;94:1626–31.
Cambonie G, Desage C, Thaller P, Lemaitre A, de Balanda KB, Combes C, et al. Context of a neonatal death affects parental perception of end-of-life care, anxiety and depression in the first year of bereavement. BMC Palliat Care. 2023;22:58.
Yui Y, October TW. Parental Perspectives on the Postpartum Bonding Experience after Neonatal Intensive Care Unit Transfer to a Referral Hospital. Am J Perinatol. 2021;38:1358–65.
Gibson J, Finney S, Boilanger M. Developing a bereavement program in the newborn intensive care unit. J Perinat Neonatal Nurs. 2011;25:331–41.
Harvey S, Snowdon C, Elbourne D. Effectiveness of bereavement interventions in neonatal intensive care: a review of the evidence. Semin Fetal Neonatal Med. 2008;13:341–56.
Jennings V, Nicholl H. Bereavement support used by mothers in Ireland following the death of their child from a life-limiting condition. Int J Palliat Nurs. 2014;20:173–8.
Capitulo KL. Evidence for healing interventions with perinatal bereavement. MCN Am J Matern Child Nurs. 2005;30:389–96.
Singh J, Lantos J, Meadow W. End-of-life after birth: death and dying in a neonatal intensive care unit. Pediatrics. 2004;114:1620–6.
Boileau P, Letouzey M, Morgan AS, Lorthe E, Kaminski M, Coquelin A, et al. Circumstances, causes and timing of death in extremely preterm infants admitted to NICU: The EPIPAGE-2 study. Acta Paediatr. 2023;112:2066–74.
Fontana MS, Farrell C, Gauvin F, Lacroix J, Janvier A. Modes of death in pediatrics: differences in the ethical approach in neonatal and pediatric patients. J Pediatr. 2013;162:1107–11.
Pierucci RL, Kirby RS, Leuthner SR. End-of-life care for neonates and infants: the experience and effects of a palliative care consultation service. Pediatrics. 2001;108:653–60.
Marcola L, Barbosa SMM, Zoboli I, Polastrini RTV, Ceccon MEJ. Analysis of Death and Palliative Care in a Neonatal Intensive Care Unit. Rev Paul Pediatr. 2017;35:125–9.
Finn D, Collins A, Murphy BP, Dempsey EM. Mode of neonatal death in an Irish maternity centre. Eur J Pediatr. 2014;173:1505–9.
Verhagen AA, Janvier A, Leuthner SR, Andrews B, Lagatta J, Bos AF, et al. Categorizing neonatal deaths: a cross-cultural study in the United States, Canada, and The Netherlands. J Pediatr. 2010;156:33–7.
Acknowledgements
Thank you to Leah Engelstad and Elizabeth Boring.
Author information
Authors and Affiliations
Contributions
CMG conceived the study, performed the chart review, and drafted the manuscript. MR and PH contributed to study design, data analysis and interpretation, and critical review of the manuscript. JDA conceived the study and contributed to data analysis and interpretation and critical review of the manuscript.
Corresponding author
Ethics declarations
Competing interests
CMG previously owned stock in Merck. This does not conflict with this study. All other authors report no competing interests.
Ethics approval
This study was deemed exempt by the Institutional Review Board at Indiana University.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Groden, C.M., Raed, M., Helft, P. et al. End of life care in a level IV outborn neonatal intensive care unit. J Perinatol (2024). https://doi.org/10.1038/s41372-024-01930-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41372-024-01930-6