Abstract
Objective
To inform clinical practice by describing a model of perinatal palliative care delivery within a fully staffed fetal health center (FHC) inside a freestanding children’s hospital.
Study design
The team conducted a retrospective chart review of the palliative care team (PaCT) database from FHC’s inception in 2010 to 31 December, 2018, and surveyed the FHC neonatologists.
Results
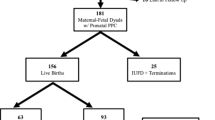
PaCT consults in the FHC increased from 1 in 2010 to 102 in 2018. PaCT met 430 mothers for prenatal consultation. Of the 390 live-born infants, 172 died; 48 received comfort care only from birth; and 19 survived to discharge home with hospice. At the time of review, PaCT still follows 109 children met prenatally. PaCT discharged 96 patients that no longer required PaCT services.
Conclusions
PaCT provides an integral service within the FHC as evidenced by the increasing volume of consultations, variety of care provided and perceived value by FHC neonatologists.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Xu J, Murphy SL, Kochanek KD, Bastian BB, Arias E. Deaths: final data for 2016. Natl Vital Stat Rep. 2018;67:1–76.
Wool C, Repke JT, Woods AB. Parent reported outcomes of quality care and satisfaction in the context of a life-limiting fetal diagnosis. J Matern Fetal Neonatal Med. 2017;30:894–9.
Hasegawa SL, Fry JT. Moving toward a shared process: the impact of parent experiences on perinatal palliative care. Semin Perinatol. 2017;41:95–100.
Côté-Arsenault D, Denney-Koelsch E. ‘My baby is a person’: parents’ experiences with life-threatening fetal diagnosis. J Palliat Med. 2011;14:1302–8.
Walker LV, Miller VJ, Dalton VK. The health-care experiences of families given the prenatal diagnosis of trisomy 18. J Perinatol. 2008;28:12–9.
Balaguer A, Martín-Ancel A, Ortigoza-Escobar D, Escribano J, Argemi J. The model of palliative care in the perinatal setting: a review of the literature. BMC Pediatr. 2012;12:25.
Wool C. State of the science on perinatal palliative care. J Obstet Gynecol Neonatal Nurs. 2013;42:372–82.
Catania TR, Bernardes L, Guerra Benute GR, Gibeli MABC, do Nascimento NB, Barbosa TVA. et al. When one knows a fetus is expected to die: palliative care in the context of prenatal diagnosis of fetal malformations. J Palliat Med. 2017;20:1020–31.
American College of Obstetricians and Gynecologists. Perinatal palliative care: ACOG Committee Opinion Summary, Number 786. Obstet Gynecol. 2019;134:660–1.
Hancock HS, Pituch K, Uzark K, Bhat P, Fifer C, Silveira M, et al. A randomised trial of early palliative care for maternal stress in infants prenatally diagnosed with single-ventricle heart disease. Cardiol Young. 2018;28:561–70.
Feudtner C, Womer J, Augustin R, Remke S, Wolfe J, Friebert S, et al. Pediatric palliative care programs in children’s hospitals: a cross-sectional national survey. Pediatrics. 2013;132:1063–70.
Marc-Aurele KL, Hull AD, Jones MC, Pretorius DH. A fetal diagnostic center’s referral rate for perinatal palliative care. Ann Palliat Med. 2018;7:177–85.
Tosello B, Dany L, Bétrémieux P, Le Coz P, Auquier P, Gire C, et al. Barriers in referring neonatal patients to perinatal palliative care: a French multicenter survey. PLoS ONE. 2015;10:e0126861.
English NK, Hessler KL. Prenatal birth planning for families of the imperiled newborn. J Obstet Gynecol Neonatal Nurs. 2013;42:390–9.
Quinn M, Gephart S. Evidence for implementation strategies to provide palliative care in the neonatal intensive care unit. Adv Neonatal Care. 2016;16:430–8.
Mazwi ML, Henner N, Kirsch R. The role of palliative care in critical congenital heart disease. Semin Perinatol. 2017;41:128–32.
Bertaud S, Lloyd DFA, Laddie J, Razavi R. The importance of early involvement of paediatric palliative care for patients with severe congenital heart disease. Arch Dis Child. 2016;101:984–7.
Acknowledgements
The authors would like to acknowledge Malinda Hoyt, Allie Wayne, and Jill Curruth for their help with data support. We would also like to acknowledge the FHC staff, the Palliative Care Team members, and most importantly, the families served.
Author information
Authors and Affiliations
Contributions
MHT conceptualized and designed the study, acquired data, played an important role in interpreting the results, drafted the initial manuscript, reviewed and revised the manuscript, and approved the final version. KE conceptualized and designed the study, acquired data, played an important role in interpreting the results, reviewed and revised the manuscript, and approved the final version. JL conceptualized and designed the study, coordinated and supervised data collection, played an important role in interpreting the results, drafted the initial manuscript, reviewed and revised the manuscript, and approved the final version. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41372_2021_966_MOESM1_ESM.docx
Process Overview of the Palliative Care Team (PaCT) within the Fetal Health Center (FHC) at Children’s Mercy Kansas City
Rights and permissions
About this article
Cite this article
Tucker, M.H., Ellis, K. & Linebarger, J. Outcomes following perinatal palliative care consultation: a retrospective review. J Perinatol 41, 2196–2200 (2021). https://doi.org/10.1038/s41372-021-00966-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-00966-2
This article is cited by
-
Specialist perinatal palliative care: a retrospective review of antenatal referrals to a children’s palliative care service over 14 years
BMC Palliative Care (2023)
-
Fetal outcomes and continuity in perinatal palliative care patients at a quaternary care pediatric hospital
Journal of Perinatology (2023)