Abstract
Objective
To characterize literature that describes infant mode of death and to clarify how limitation of life-sustaining treatment (LST) is defined and rationalized.
Study design
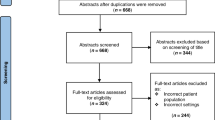
Eligible studies were peer-reviewed, English-language, and included number of infant deaths by mode out of all infant deaths in the NICU and/or delivery room.
Result
58 included studies were primarily published in the last two decades from North American and European centers. There was variation in rates of infant mode of death by study, with some showing an increase in deaths following limitation of LST over time. Limitation of LST was defined by the intervention withheld/withdrawn, the relationship between the two practices, and prior frameworks. Themes for limiting LST included diagnoses, low predicted survival and/or quality of life, futility, and suffering.
Conclusion
Limitation of LST is a common infant mode of death, although rates, study definitions, and clinical rationale for this practice are variable.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
CDC. Centers for Disease Control and Prevention National Center for Health Statistics. Leading causes of death and numbers of deaths, by age: United States, 1980 and 2017 https://www.cdc.gov/nchs/data/hus/2018/007.pdf: Centers for Disease Control and Prevention National Center for Health Statistics; 2018.
Hug L, Alexander M, You D, Alkema L. National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: a systematic analysis. Lancet Glob Health. 2019;7:e710–e20.
World Health O. World health statistics 2019: monitoring health for the SDGs, sustainable development goals. Geneva: World Health Organization; 2019; 2019.
Trowbridge A, Walter JK, McConathey E, Morrison W, Feudtner C. Modes of death within a children’s hospital. Pediatrics. 2018;142.
Wentlandt K, Toupin P, Novosedlik N, Le LW, Zimmermann C, Kaya E. Language used by health care professionals to describe dying at an acute care hospital. J Pain Symptom Manag. 2018;56:337–43.
Duff RS, Campbell AG. Moral and ethical dilemmas in the special-care nursery. N Engl J Med. 1973;289:890–4.
Singh J, Lantos J, Meadow W. End-of-life after birth: Death and dying in a neonatal intensive care unit. Pediatrics. (Evanst) 2004;114:1620–6.
Cook LA, Watchko JF. Decision making for the critically ill neonate near the end of life. J Perinatol. 1996;16:133–6.
Verhagen AAE, Dorscheidt J, Engels B, Hubben JH, Sauer PJ. End-of-life decisions in dutch neonatal intensive care units. Arch Pediatrics Adolesc Med 2009;163:895–901.
Fry JT, Matoba N, Datta A, DiGeronimo R, Coghill CH, Natarajan G, et al. Center, gestational age, and race impact end-of-life care practices at regional neonatal intensive care units. J Pediatr. 2020;217:86–91.e1.
Verhagen AA, Janvier A, Leuthner SR, Andrews B, Lagatta J, Bos AF, et al. Categorizing neonatal deaths: A cross-cultural study in the United States, Canada, and The Netherlands. J Pediatr. 2010;156:33–7.
Fajardo CA, Gonzalez S, Zambosco G, Cancela MJ, Forero LV, Venegas M, et al. End of life, death and dying in neonatal intensive care units in Latin America. Acta Paediatrica. 2012;101:609–13.
Baker JN, Levine DR, Hinds PS, Weaver MS, Cunningham MJ, Johnson L, et al. Research priorities in pediatric palliative care. J Pediatr. 2015;167:467–70 e3.
Youngblut JM, Brooten D. Perinatal and pediatric issues in palliative and end-of-life care from the 2011 Summit on the Science of Compassion. Nurs Outlook 2012;60:343–50.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169:467–73.
Peters M, Godfrey C, McInerney P, Munn Z, Tricco A, Khalil H. Chapter 11: Scoping Reviews. In: Z AEM, editor. JBI Manual for Evidence Synthesis 2020.
Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org.
Barney G, Glaser PD. The constant comparative method of qualitative analysis. The grounded theory review. 2008;7.
Rahman S, Al Rifai H, El Ansari W, Nimeri N, El Tinay S, Salameh K, et al. A PEARL study analysis of national neonatal, early neonatal, late neonatal, and corrected neonatal mortality rates in the state of qatar during 2011: A comparison with world health statistics 2011 and Qatar’s Historic Data over a Period of 36 Years (1975–2011). J Clin Neonatol. 2012;1:195–201.
Schulz-Baldes A, Huseman D, Loui A, Dudenhausen JW, Obladen M. Neonatal end-of-life practice in a German perinatal centre. Acta Paediatr. 2007;96:681–7.
Aladangady, N., et al., Short-term outcome of treatment limitation discussions for newborn infants, a multicentre prospective observational cohort study. Arch Dis Child Fetal Neonatal Ed., 2017;102:F104–F109.
Aghion A, Hussey-Gardner B, Davis NL, Falck AJ. Patient and provider factors impacting referral for neonatal organ donation. Pediatr Transplant. 2020;24:e13744. https://doi.org/10.1111/petr.13744.
Tudehope DI, Papadimos E, Gibbons K. A 12-year review of neonatal deaths in delivery room in a perinatal tertiary centre. J Paediatr Child Health. 2012;48:63.
Berger TM, Hofer A. Causes and circumstances of neonatal deaths in 108 consecutive cases over a 10-year period at the Children’s Hospital of Lucerne, Switzerland. Neonatology. 2009;95:157–63.
Eventov-Friedman S, Kanevsky H, Bar-Oz B. Neonatal end-of-life care: A single-center NICU experience in Israel over a decade. Pediatrics. 2013;131:e1889–96.
Dupont‐Thibodeau A, Barrington K, Taillefer C, Janvier A, Dupont-Thibodeau A. Changes in perinatal hospital deaths occurring outside the neonatal intensive care unit over a decade. Acta Paediatrica. 2017;106:1456–9.
Garten L, Daehmlow S, Reindl T, Wendt A, Munch A, Buhrer C. End-of-life opioid administration on neonatal and pediatric intensive care units: Nurses’ attitudes and practice. Eur J Pain. 2011;15:958–65.
Snoep M, Jansen N, Groenendaal F. Cause and course of neonatal deaths in a tertiary neonatal and paediatric intensive care. Eur J Pediatr. 2016;175:1856–7.
McHugh-Strong CM, Sanders MR. Experience with newborn intensive care deaths in a tertiary setting. Am J Perinatol. 2000;17:27–33.
Nishida H, Sakamoto S. Ethical problems in neonatal intensive care unit-medical decision making on the neonate with poor prognosis. Early Hum Dev. 1992;29:403–6.
Koper JF, Bos AF, Janvier A, Verhagen AA. Dutch neonatologists have adopted a more interventionist approach to neonatal care. Acta Paediatr. 2015;104:888–93.
Ramelet AS, Bergstraesser E, Grandjean C, Dorsaz A, Fahrni-Nater P, Cignacco E, et al. Comparison of end-of-life care practices between children with complex chronic conditions and neonates dying in an ICU versus Non-ICUs: A substudy of the pediatric end-of-life care needs in Switzerland (PELICAN) Project∗. Pediatr Crit Care Med. 2020:E236–46.
Kim M-J, Lee J-H, Lee H-D. Recent changes in end-of-life decisions for newborns in a Korean Hospital American. J Hosp Palliat Med. 2018;35:574–8.
Peng NH, Chen CH, Liu HL, Lee HY, Huang H, Chang YC, et al. To explore the neonatal clinicians’ beliefs and attitudes towards caring for dying neonates in Taiwan. Intensive Care Med. 2013;39:S143.
Verhagen AA, Spijkerman J, Muskiet FD, Sauer PJ. Physician end-of-life decision-making in newborns in a less developed health care setting: Insight in considerations and implementation. Acta Paediatr. 2007;96:1437–40.
Hagen CM, Hansen TW. Deaths in a neonatal intensive care unit: A 10-year perspective. Pediatric critical care medicine: A journal of the society of critical care medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2004;5:463–8.
Moura H, Costa V, Rodrigues M, Almeida F, Maia T, Guimaraes H. End of life in the neonatal intensive care unit. Clinics. 2011;66:1569–72.
Chan LC, Cheung HM, Poon TC, Ma TP, Lam HS, Ng PC. End-of-life decision-making for newborns: A 12-year experience in Hong Kong. Arch Dis Child Fetal Neonatal Ed. 2016;101:F37–42.
Younge N, Smith PB, Goldberg RN, Brandon DH, Simmons C, Cotten CM, et al. Impact of a palliative care program on end-of-life care in a neonatal intensive care unit. J Perinatol. 2015;35:218–22.
Weiner J, Sharma J, Lantos J, Kilbride H. How infants die in the neonatal intensive care unit: Trends From 1999 Through 2008. Arch Pediatrics Adolesc Med. 2011;165:630–4.
de Leeuw R, de Beaufort AJ, de Kleine MJ, van Harrewijn K, Kollée LA. Foregoing intensive care treatment in newborn infants with extremely poor prognoses. A study in four neonatal intensive care units in The Netherlands. J Pediatr. 1996;129:661–6.
Wilkinson DJ, Fitzsimons JJ, Dargaville PA, T Campbell N, Loughnan PM, McDougall PN, et al. Death in the neonatal intensive care unit: changing patterns of end of life care over two decades. Arch Dis Child-Fetal Neonatal Ed. 2006;91:F268–F71.
Marçola L, De Barbosa SMM, Zoboli I, Polastrini RTV, Ceccon MEJ. Analysis of death and palliative care in a neonatal intensive care unit. Rev Paul de Pediatr. 2017;35:125–9.
Ng SKF, Keenan N, Swart S, Berry MJ. Palliative care in a tertiary neonatal intensive care unit: a 10-year review [published online ahead of print, 2018 Nov 22]. BMJ Support Palliat Care. 2018;bmjspcare-2018-001538. p 1–5. https://doi.org/10.1136/bmjspcare-2018-001538.
Caniano DA, Hazebroek FW, DenBesten KE, Tibboel D. End-of-life decisions for surgical neonates: Experience in The Netherlands and United States. J Pediatr Surg. 1995;30:1420–4.
Arlettaz R, Mieth D, Bucher HU, Duc G, Fauchere JC. End-of-life decisions in delivery room and neonatal intensive care unit. Acta Paediatrica. 2005;94:1626–31.
Verhagen AA, van der Hoeven MA, van Meerveld RC, Sauer PJ. Physician medical decision-making at the end of life in newborns: insight into implementation at 2 Dutch centers. Pediatrics. 2007;120:e20–8.
Kelly NP, Rowley SR, Harding JE. Death in neonatal intensive-care. J Paediatr Child Health. 1994;30:419–22.
Barton L, Hodgman JE. The contribution of withholding or withdrawing care to newborn mortality. Pediatrics. 2005;116:1487–91.
da Costa DE, Ghazal H, Al Khusaiby S. Do not resuscitate orders and ethical decisions in a neonatal intensive care unit in a Muslim community. Neonatal Intensive Care. 2003;16:35–9.
Orfali K. Parental role in medical decision-making: fact or fiction? A comparative study of ethical dilemmas in French and American neonatal intensive care units. Soc Sci Med. (1982) 2004;58:2009–22.
Verhagen AA, Dorscheidt JH, Engels B, Hubben JH, Sauer PJ. Analgesics, sedatives and neuromuscular blockers as part of end-of-life decisions in Dutch NICUs. Arch Dis Child Fetal Neonatal Ed. 2009;94:F434–8.
Wall SN, Partridge JC. Death in the intensive care nursery: Physician practice of withdrawing and withholding life support. Pediatrics. 1997;99:64–70.
Whitelaw A. Death as an option in neonatal intensive care. Lancet. (Lond, Engl) 1986;2:328–31.
Pearson EB, Bose CL, Kraybill EN. Decisions about futile treatment in an intensive care nursery. North Carol Med J. 1995;56:462–6.
Berner ME, Rimensberger PC, Hüppi PS, Pfister RE. National ethical directives and practical aspects of forgoing life-sustaining treatment in newborn infants in a Swiss intensive care unit. Swiss Med Wkly. 2006;136:597–602.
Hellmann J, Knighton R, Lee SK, Shah PS, Andrews W, Payot A, et al. Neonatal deaths: Prospective exploration of the causes and process of end-of-life decisions. Arch Dis Child: Fetal Neonatal Ed. 2016;101:F102–F7.
Section On H, Palliative M, Committee On Hospital C. Pediatric palliative care and hospice care commitments, guidelines, and recommendations. Pediatrics. (Evanst) 2013;132:966–72.
Rogers M, Meier DE, Heitner R, Aldridge M, Hill Spragens L, Kelley A, et al. The National palliative care registry: A decade of supporting growth and sustainability of palliative care programs. J Palliat Med. 2019;22:126–1031.
Wang CH, Du LZ, Ma XL, Shi LP, Tong XM, Liu H, et al. Analysis of in-hospital neonatal death in the tertiary neonatal intensive care unit in China: A multicenter retrospective study. Chin Med J. (Engl) 2016;129:2652–8.
Beauchamp TL. Principles of biomedical ethics. Eighth edition. ed. Childress JF, editor. New York, NY: Oxford University Press; 2019.
Diekema DS, Mercurio MR, Adam MB. Clinical ethics in pediatrics: a case-based textbook. Cambridge: Cambridge University Press; 2011.
Wilkinson D, Savulescu J. A costly separation between withdrawing and withholding treatment in intensive care. Bioethics. 2014;28:127–37.
Weise KL, Okun AL, Carter BS, Christian CW. Guidance on forgoing life-sustaining medical treatment. Pediatrics. (Evanst) 2017;140:e20171905.
Feltman DM, Du H, Leuthner SR. Survey of neonatologists’ attitudes toward limiting life-sustaining treatments in the neonatal intensive care unit. J Perinatol. 2012;32:886–92.
Yotani N, Nabetani M, Feudtner C, Honda J, Kizawa Y, Iijima K. Withholding and withdrawal of life-sustaining treatments for neonate in Japan: Are hospital practices associated with physicians’ beliefs, practices, or perceived barriers. Early Hum Dev. 2020;141:104931.
Rebagliato M, Cuttini M, Broggin L, Berbik I, de Vonderweid U, Hansen G, et al. Neonatal end-of-life decision making: Physicians’ attitudes and relationship with self-reported practices in 10 European countries. JAMA: J Am Med Assoc. 2000;284:2451–9.
Lonergan B, Wright A, Markham R, Machin L. Time-limited trials: A qualitative study exploring the role of time in decision-making on the Intensive Care Unit. Clin Ethics. 2020;15:11–6.
Rysavy MA, Horbar JD, Bell EF, Li L, Greenberg LT, Tyson JE, et al. Assessment of an updated neonatal research network extremely preterm birth outcome model in the Vermont Oxford network. JAMA Pediatr. 2020;174:e196294–e.
Richardson DK, Corcoran JD, Escobar GJ, Lee SK. SNAP-II and SNAPPE-II: Simplified newborn illness severity and mortality risk scores. J Pediatr. 2001;138:92–100.
Kukora S, Gollehon N, Weiner G, Laventhal N. Prognostic accuracy of antenatal neonatology consultation. J Perinatol. 2017;37:27–31.
Meadow W, Lagatta J, Andrews B, Caldarelli L, Keiser A, Laporte J, et al. Just, in time: Ethical implications of serial predictions of death and morbidity for ventilated premature infants. Pediatrics (Evanst) 2008;121:732–40.
Stevens SM, Richardson DK, Gray JE, Goldman DA, McCormick MC. Estimating neonatal mortality risk: An analysis of clinicians’ judgments. Pediatrics. (Evanst) 1994;93:945–50.
Shapiro N, Wachtel EV, Bailey SM, Espiritu MM. Implicit physician biases in periviability counseling. J Pediatr. 2018;197:109–15.e1.
Haward MF, Murphy RO, Lorenz JM. Message framing and perinatal decisions. Pediatrics. (Evanst) 2008;122:109–18.
Boardman FK. Whose life is worth preserving? Disabled people and the expressivist objection to neonatology. Acta Paediatrica. 2021;110:391–3.
Adams SY, Tucker R, Clark MA, Lechner BE. “Quality of life”: Parent and neonatologist perspectives. J Perinatol. 2020;40:1809–20.
Saigal S, Stoskopf BL, Feeny D, Furlong W, Burrows E, Rosenbaum PL, et al. Differences in preferences for neonatal outcomes among health care professionals, parents, and adolescents. JAMA: J Am Med Assoc. 1999;281:1991–7.
Saigal S. Self-perceived health status and health-related quality of life of extremely low-birth-weight infants at adolescence. JAMA: J Am Med Assoc. 1996;276:453–9.
Lantos JD. Neonatal bioethics: the moral challenges of medical innovation. Meadow W, editor. Baltimore: Johns Hopkins University Press; 2006.
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA: J Am Med Assoc. 2015;314:1039–51.
Pyle AK, Fleischman AR, Hardart G, Mercurio MR. Management options and parental voice in the treatment of trisomy 13 and 18. J Perinatol. 2018;38:1135–43.
Frader J, Truog RD, Brett AS. The problem with futility. N. Engl J Med. 1992;326:1560–4.
Bosslet GT, Pope TM, Rubenfeld GD, Lo B, Truog RD, Rushton CH, et al. An Official ATS/AACN/ACCP/ESICM/SCCM policy statement: Responding to requests for potentially inappropriate treatments in intensive care units. Am J Resp Crit Care Med. 2015;191:1318–30.
Cassell EJ. The nature of suffering: and the goals of medicine. New York: Oxford University Press; 1991.
Salter EK. The new futility? The rhetoric and role of “suffering” in pediatric decision-making. Nurs Ethics. 2020;27:16–27.
Fortney CA, Baughcum AE, Moscato EL, Winning AM, Keim MC, Gerhardt CA. Bereaved parents’ perceptions of infant suffering in the NICU. J Pain Symptom Manag. 2020;59:1001–8.
Baughcum AE, Fortney CA, Winning AM, Dunnells ZDO, Humphrey LM, Gerhardt CA. Healthcare satisfaction and unmet needs among bereaved parents in the NICU. Adv Neonatal Care. 2020;20:118–26.
Clark, OE, et al., Parent Perceptions of Infant Symptoms and Suffering and Associations With Distress Among Bereaved Parents in the NICU. J Pain Symptom Manage. 2021;62:e20–e27.
James JMD, Munson DMD, DeMauro SBMDM, Langer JCMS, Dworetz ARMD, Natarajan GMD, et al. Outcomes of Preterm Infants following Discussions about Withdrawal or Withholding of Life Support. J Pediatr. 2017;190:118–23.e4.
Natarajan G, Mathur A, Zaniletti I, DiGeronimo R, Lee K-S, Rao R, et al. Withdrawal of Life-Support in Neonatal Hypoxic-Ischemic Encephalopathy. Pediatr Neurol. 2019;91:20–6.
Campbell AG, Lloyd DJ, Duffty P. Treatment dilemmas in neonatal care: who should survive and who should decide? Ann N. Y Acad Sci. 1988;530:92–103.
Airede KI. Should we resuscitate? Ethical dilemmas. Ann Trop Paediatr. 1991;11:169–74.
Ryan CA, Byrne P, Kuhn S, Tyebkhan J. No resuscitation and withdrawal of therapy in a neonatal and a pediatric intensive care unit in Canada. J Pediatr. 1993;123:534–8.
Moseley KL, Church A, Hempel B, Yuan H, Goold SD, Freed GL. End-of-life choices for African-American and white infants in a neonatal intensive-care unit: A pilot study. J Natl Med Assoc. 2004;96:933–7.
Roy R, Aladangady N, Costeloe K, Larcher V. Decision making and modes of death in a tertiary neonatal unit. Arch Dis Child Fetal Neonatal Ed. 2004;89:F527–30.
Simpson CDA, Ye XAY, Hellmann J, Tomlinson C. Trends in cause-specific mortality at a Canadian outborn NICU. Pediatrics. 2010;126:E1538–E44.
Fontana MS, Farrell C, Gauvin F, Lacroix J, Janvier A. Modes of death in pediatrics: Differences in the ethical approach in neonatal and pediatric patients. J Pediatr. 2013;162:1107–11.
Samsel C, Lechner BE. End-of-life care in a regional level IV neonatal intensive care unit after implementation of a palliative care initiative. J Perinatol. 2015;35:223–8.
Weiner J, Sharma J, Lantos J, Kilbride H. Does diagnosis influence end-of-life decisions in the neonatal intensive care unit? J Perinatol. 2015;35:151–4.
Lam V, Kain N, Joynt C, van Manen MA. A descriptive report of end-of-life care practices occurring in two neonatal intensive care units. Palliat Med. 2016;30:971–8.
Acknowledgements
We would like to thank Chloe Rotman, MLIS, Manager of Library Services at Boston Children’s Hospital, for her assistance with the early phases of this scoping review, including search strategy and Covidence.
Funding
Cummings is supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health under award number R01HD094794 (CC PI). This funder played no role in the study design, analysis, or preparation of this article. The other authors received no other external funding for this study.
Author information
Authors and Affiliations
Contributions
ML and RD conceptualized and designed the study, designed the data collection protocol, collected the data, carried out the qualitative analyses, drafted the initial manuscript, and reviewed and revised the manuscript. CC and JW conceptualized and designed the study, supervised the data collection and qualitative analyses, and critically reviewed the manuscript for intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lin, M., Deming, R., Wolfe, J. et al. Infant mode of death in the neonatal intensive care unit: A systematic scoping review. J Perinatol 42, 551–568 (2022). https://doi.org/10.1038/s41372-022-01319-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01319-3
This article is cited by
-
End of life care in a level IV outborn neonatal intensive care unit
Journal of Perinatology (2024)